
Maternal-Fetal Physiologic
What are the developmental stages of early pregnancy?
Fertilization and cleavage result in a zygote (an 8-cell mass) which then divides to form the morula (a 16-cell mass) 3 days after fertilization. A blastocyst develops and implantation occurs approximately 10 days after fertilization. An embryonic disk develops after the first week and a yolk sac after 5 weeks.
What are the placental membranes and uterine layers (fetal to maternal)?
Amnion
Chorion (with villi composed of syncytial trophoblasts and cytotrophoblasts)
Decidua parietalis (endometrium) Myometrium
Serosa (See Fig. 8.1)
Figure 8.1 Embryologic layers of the human fetus at 3 months.
How does the timing of division affect the development of monozygotic twins?
Division in less than 72 hours: two embryos, two amnions, two chorions (“di-di”)
Division between 4 and 7 days: two embryos, two amnions, one chorion (“mono-di”)
Division after 7 days: one shared amnion and chorion (“mono-mono”)
Division after the embryonic disk has developed: conjoined twins
What are the major shunts involved with fetal circulation?
Ductus venosus
Foramen ovale
Ductus arteriosus
What are the patterns of fetal blood flow (starting from the umbilical vein)?
1. Umbilical vein → ductus venosus and liver → inferior vena cava → right atrium → foramen ovale → left atrium → left ventricle → cephalic/systemic circulation → internal iliac artery → umbilical arteries → placenta
2. Superior vena cava → right atrium → right ventricle → pulmonary artery → ductus arteriosis (mostly) and fetal lungs (small amount) → descending aorta → hypogastric arteries → umbilical arteries (see Fig. 8.2)

Do each of the following vessels carry oxygenated or deoxygenated blood?
Umbilical artery:
Deoxygenated
Umbilical vein:
Oxygenated
What are the embryologic remnants associated with each of the following?
Umbilical vein:
Ligamentum hepatis
Ductus venosus:
Ligamentum venosum
Ductus arteriosus:
Ligamentum arteriosum
Umbilical arteries:
Medial umbilical ligaments
How does pregnancy affect cardiac output (CO), blood volume, and blood pressure (BP)?
CO increases up to 50% (1.8 L/min). Blood volume increases by 50%.
BP decreases.
These changes peak during the second trimester and remain relatively constant until delivery.
Pregnancy affects which components of CO?
Remember, CO = SV × HR. Both stroke volume (SV) and heart rate (HR) increase; however, SV increases more than HR.
How does pregnancy affect SV?
Preload is increased with an increase in blood volume; afterload is reduced by the low-resistance uteroplacental circulation and by peripheral vasodilatation.
What percentage of CO goes to the uterus during pregnancy?
Up to 20% at term (compared to < 1% in the nonpregnant state)
How does the cardiac examination change during pregnancy?
Heart sounds are louder and split Often a systolic murmur and an S3 Slight left axis deviation on EKG Mild cardiomegaly on chest x-ray (CXR) (A diastolic murmur is never normal and should be evaluated.)
Describe positional changes that affect CO in pregnancy:
In the supine position the inferior vena cava is compressed, which may decrease CO by up to 30%. Maximum venous return and CO is maintained in the left lateral decubitus (LLD) position.
Describe the hematologic changes of pregnancy:
Red blood cell mass increases by 15% to 30% (because of increased erythropoietin).
Plasma volume increases by 30% to 50% (because of increased aldosterone).
Hct and Hb decrease, causing the physiologic “anemia of pregnancy” (because of increased plasma volume).
Note: An Hb less than 11 is never normal and must be evaluated for iron/folate deficiency or a hemoglobinopathy.
When does the anemia of pregnancy reach its nadir?
Around 24 weeks
What is the effect of pregnancy on BP?
BP decreases in the first trimester, nadirs at approximately 24 weeks, and then almost normalizes by term. Diastolic is affected more than systolic.
How does pregnancy affect pulmonary function tests (PFTs)?
Tidal volume increases by 40%.
Minute ventilation increases by 50%.
Functional residual capacity decreases by 20%.
Total lung capacity slightly decreases.
Expiratory reserve volume and total lung capacity decrease.
Forced expiratory volume (FEV1) does not change.
Respiratory rate does not change.
What hormone mediates these effects?
Progesterone
How is the acid base equilibrium affected during pregnancy?
Respiratory alkalosis with metabolic compensation (pH between 7.40 and 7.45)
What is the effect of pregnancy on oxygen consumption?
Increases by over 20% owing to the placenta, fetus, and maternal organs
What is the effect of pregnancy on renal function?
Glomerular filtration rate (GFR) increases by 50% (because of the increase in glomerular plasma flow).
Renal blood flow increases.
Plasma creatinine, BUN, and uric acid levels decrease (because of the increased GFR).
Normal Cr, BUN, or UA may indicate underlying pathology (preeclampsia, renal insufficiency).
Why is the pregnant woman at increased risk for urinary tract infections?
Progesterone reduces ureteral tone and peristalsis, and relaxes the bladder wall allowing reflux through the incompetent vesico-ureteral valves. This results in stasis of urine, dilated ureters, increased pressure in the renal pelvis, and bacterial proliferation.
What are the common causes of bacteriuria in pregnancy?
Escherichia coli >> Klebsiella > Proteus > Group B streptococcus (GBS) > Enterococci > Staphylococci
Where does hydronephrosis in pregnancy most commonly occur?
On the right side (because of right uterine dextrorotation and right ureter compression)
What happens to plasma osmolality during pregnancy?
The increase in intravascular fluid decreases plasma osmolality.
What is the clinical affect of this change in plasma osmolality?
Pitting edema in gravity-dependent areas
What is the significance of trace protein or glucose in the second or third trimester?
It is normal, because of increased GFR.
When does morning sickness occur?
During the first trimester, as levels of hCG are rapidly rising. After hCG levels peak (~10 weeks), morning sickness decreases.
What is hyperemesis gravidarum?
An idiopathic, noninfectious, severe nausea and vomiting that causes dehydration, ketone formation, weight loss, hypokalemia, and metabolic alkalosis.
How does progesterone affect the GI tract?
Lower esophageal sphincter tone decreases (can lead to GERD)
Small bowel and colon transit decreases (can lead to bloating and constipation)
Venous congestion (can lead to hemorrhoids)
Biliary tract peristalsis decreases (increases risk of cholelithiasis and cholecystitis)
How do liver function tests (LFTs) change in pregnancy?
Alkaline phosphatase is increased (because of placental production). Other enzymes are within normal limits.
(Abnormalities may suggest pathology: hepatitis, HELLP, acute fatty liver of pregnancy, cholestasis of pregnancy, or other pathologies)
How does pregnancy affect the risk of pancreatitis?
Increases the risk (because of increased risks of cholelithiasis and hyperlipidemia)
Why is the mortality associated with appendicitis higher in pregnancy?
Because of the gravid uterus, the appendix is pushed higher leading to a delay in the diagnosis.
How is the coagulation system affected by pregnancy?
Decreased protein S
Resistance to protein C
Increased factor I (fibrinogen), II, V, VII, VIII, X, and XII
Because of these, pregnancy is a hypercoagulable state
What are the potential complications of this hypercoagulable state?
Venous thrombosis (occurs 0.7 per 1000 women in pregnancy) and subsequent pulmonary embolism. Both occur predominantly in the third trimester.
What is the effect of pregnancy on immunity?
Cell-mediated immunity is weakened but humoral immunity is strengthened.
What is hCG and where is it formed?
Human chorionic gonadotropin; in the syncytiotrophoblast of the placenta
hCG is structurally related to what other glycoprotein hormones?
Luteinizing hormone (LH), follicle-stimulating hormone (FSH), and thyroid-stimulating hormone (TSH) (they all have the same α subunit but different β subunits)
How does hCG promote pregnancy?
Maintains the corpus luteum for first trimester
Causes sexual differentiation in the male fetus
Ensures adequate T3 and T4 production
Increases relaxin secretion by the corpus luteum (leading to decreased vascular resistance)
What are the three major types of estrogen and where are they predominately produced?
1. Estrone: adrenals (dehydroepiandrosterone [DHEA] is the precursor)
2. Estriol (least bioactive): placenta
3. Estradiol (most bioactive): ovaries
What happens to the adrenal hormones during pregnancy?
Adrenocorticotropic hormone (ACTH), corticotropin-releasing hormone (CRH), and cortisol all increase
What is oxytocin?
A hormone produced by the hypothalamus and released by the posterior pituitary. Concentrations rise throughout gestation, during labor, and with lactation or nipple stimulation.
What are the major actions of oxytocin?
Contraction of uterine myometrium, ductal myoepithelial contraction (milk expression), orgasm, and bonding
What peptide is similar to oxytocin and what are the clinical consequences?
Antidiuretic hormone (ADH)
Induction/augmentation of labor with oxytocin may cause severe fluid retention and pulmonary edema.
What happens to thyroid hormone levels during pregnancy?
TBG increases
Total T3 and T4 levels increase but free T3 and T4 levels (and thus thyroid function) remain unchanged, TSH does not change.
What mediates these thyroid hormone changes?
hCG stimulates TSH to increase total T4 and T3 levels. Estrogen increases the hepatic production of TBG.
What is hPL and where is it formed?
Human placental lactogen; in the syncytiotrophoblast of the placenta
What is the function of hPL?
It antagonizes insulin and increases lypolysis to ensure adequate glucose delivery to the fetus
How does maternal glucose metabolism change during pregnancy?
hPL causes mild maternal insulin resistance and can lead to the development of gestational diabetes.
Why does gestational diabetes mellitus (GDM) occur?
There is insufficient maternal insulin to counter the hyperglycemic effects of placental hPL. It occurs most commonly in the third trimester, when hPL levels are highest.
What are striae distensae or striae gravidarum?
Stretch marks; caused from a diminution of elastin fibers and fibrillin microfibrils
What other skin changes occur during pregnancy?
Chloasma or melasma (hyperpigmentation of the face)
Linea nigra (darkening of the linea alba from the pubic symphysis to the xiphoid process)
Hyperpigmentation of the axilla, genitalia, perineum, anus, inner thighs, neck, scars, nevi, and lentigo
Palmar erythema and telangiectasias Hirsutism and acne
What is Chadwick sign?
Bluish color of vulvar and vaginal membranes because of venous congestion; a normal finding in pregnancy
What other vaginal changes occur in pregnancy?
Increased vascularity and distensibility; increased vaginal discharge (because of increased capillary permeability and desquamation)
What changes occur to the cervix and uterus during pregnancy?
Hegar sign (softening of the lower uterine segment that occurs in early pregnancy)
Increased eversion of the cervical columnar epithelium
What breast changes occur in pregnancy?
Enlargement, increase in cystic components, darkening of areolae, hypertrophy of sebaceous glands, colostrum production (in late pregnancy)
When should prenatal care begin?
Preconception or as soon as pregnancy is suspected.
What are the major goals of preconceptive counseling?
Minimize unplanned pregnancies Optimize chronic medical disorders (diabetes mellitus [DM], epilepsy, hypothyroid, cardiovascular disorders)
Promote healthy behaviors
Counsel regarding adequate diet, exercise, and nutritional supplements (folic acid and iron)
Offer appropriate vaccinations (rubella, diphtheria, hepatitis B virus)
Screen for genetic or chromosomal abnormalities
Improve patient’s readiness for pregnancy and parenting
What does folic acid supplementation help prevent?
Neural tube (NT) defects
Who should take folic acid supplementation?
All women of reproductive age; the NT closes 26 days after fertilization (often before a woman is aware of pregnancy) therefore they need to begin supplementation before becoming pregnant.
How much folic acid should healthy women of reproductive age consume?
A balanced diet plus 0.4 mg daily
What are the early signs and symptoms of pregnancy?
Amenorrhea or irregular bleeding
Nausea/vomiting
Breast tenderness
Urinary frequency
How is pregnancy diagnosed?
β-hCG
When does β-hCG become positive?
Serum tests become positive following implantation (about 10 days after fertilization).
Urine tests become positive 2 to 3 weeks after fertilization or around on the first day of a missed period.
Where is hCG formed?
In the placental trophoblasts
What is the primary function of hCG?
To maintain the corpus luteum and to produce progesterone.
Why is the β subunit of hCG measured?
β subunit of hCG differentiates it from LH, FSH, and TSH, which all share the same β subunit.
What are some reasons that β-hCG may be abnormally elevated?
Multiple gestations
Trophoblastic disease
Molar pregnancy
Choriocarcinoma
At what rate does serum β-hCG increase?
Serum concentrations double every 48 hours during the first trimester and peak at 100,000 IU/L; levels then regress to 30,000 IU/L from the 20th week until term
A woman with a positive pregnancy test presents to the ER with vaginal bleeding. She has been trying to become pregnant and cannot remember her last menstrual period (LMP). Her serum β-hCG is 200 IU/L and no gestational sac is visualized on transvaginal ultrasound. What is your next step in management?
Ask the patient to return in 2 days to recheck the β-hCG. If it is not doubling appropriately she may have an ectopic pregnancy or a spontaneous abortion. A gestational sac should be visualized with a β-hCG greater than 1500 IU/L.
What is the estimated gestational age (EGA)?
Duration of the pregnancy dated from first day of the LMP. The EGA of a normal pregnancy at term is 40 weeks.
What is the developmental age (DA) of a pregnancy?
Duration of the pregnancy dated from fertilization; typically 14 days less than the EGA (such that the DA of a normal pregnancy at term is 38 weeks)
What is the estimated date of confinement (EDC)?
The “due date” when the pregnancy is full term
What is Naegele rule?
For women with a regular 28-day menstrual cycle:
EDC = LMP − 3 months + 7 days + 1 year
What gestational ages are defined by the following terms?
First trimester: less than 14 weeks
Second trimester: 14 to 28 weeks
Third trimester: more than 28 weeks
Viability: 24 weeks
Prematurity: 24 to 36 weeks
Term: 37 to 42 weeks
Post dates: more than 40 weeks
Post term: more than 42 weeks (increased risk of perinatal morbidity and mortality)
What ages are defined by the following terms?
Neonate: birth to 28 days of life
Infant: birth until 1 year of life
What are the patient’s Gs and Ps?
Gravidity: total number of pregnancies
Parity: all viable and nonviable pregnancies, including spontaneous, therapeutic, and voluntary abortions
What are the four numbers that follow parity?
1. T (term): deliveries more than 37 weeks EGA
2. P (preterm): deliveries between 20 and 37 weeks
3. A (abortuses): deliveries prior to 20 weeks (such as abortions or ectopic pregnancies)
4. L (living): living children (including twins or adoptions)
What are the Gs and Ps for a mother of three with a history of an normal spontaneous vaginal delivery (NSVD) at term, preterm twins, a fetal demise at 23 weeks, and an ectopic pregnancy at 6 weeks?
G4 P1213
How is pregnancy dating confirmed?
Ultrasound (most accurate in the first trimester) and fundal height on physical examination
What size-date discrepancy* would require further evaluation?
1. Ultrasound should be within 1 week of the EGA during the first trimester, within 10 days during the second trimester, and within 3 weeks in the third trimester.
2. FH should be within 3 weeks of the EGA (determined by LMP).
*A size-date discrepancy suggests either underlying pathology or an error in dating (requiring the EDC to be changed).
In what circumstances is fundal height greater than dates?
Twins, polyhydramnios, macrosomia, fibroids, hydatidiform mole (molar pregnancy)
To what EGA does each fundal height correspond?
12 weeks EGA
Symphysis pubis:
20 weeks EGA
Umbilicus:
Fundal height in centimeters above the symphysis pubis corresponds to EGA after 20 weeks
With each of the following tools, when can fetal cardiac activity be detected?
Transvaginal ultrasound:
6 weeks EGA
Abdominal ultrasound:
10 weeks EGA
Doppler fetal heart monitor:
12 weeks EGA
Ascultation:
20 weeks EGA
What fetal parameters are measured on ultrasound to assess EGA?
First trimester: crown-rump length
Second/third trimesters: femur length, abdominal circumference, biparietal diameter, and head circumference
Why is dating important?
Monitoring growth, appropriate timing of screening markers (quad screen, gestational diabetes mellitus [GDM]), delivery planning (fetal lung maturity, postdates)
A woman presents to the emergency room with abdominal pain. Her period is 1 week late and her serum β-hCG measures 2000 IU/L. Transvaginal ultrasound (TVUS) visualizes thickened endometrial tissue and fluid in the cul-de-sac. What is the greatest concern?
Ruptured ectopic pregnancy. TVUS can visualize a gestational sac at 5 weeks EGA, which corresponds to a serum β-hCG level of 1500 to 2000 IU/L.
What are relevant aspects of a patient’s past obstetrical history (ObHx)?
For each prior pregnancy:
Date of delivery
Mode of delivery or outcome
Gestational age and weight at delivery
Anesthesia complications
Any history of infertility
Type of uterine incision with prior C-sections
Year and EGA of all abortions and procedures
What are relevant aspects of a patient’s past gynecologic history (GynHx)?
Gyn triad: age of menarche/cycle length/duration of menstruation
History of cysts, fibroids, abnormal Pap smears, gyn surgeries
STIs
Prior use of contraception
What are relevant aspects of a patient’s genetic & family history (FHx)?
Relatives with pregnancy-related disorders (eg, pregnancy losses)
Family history of chronic medical conditions (diabetes, thyroid disorders, hemoglobinopathies)
Consanguinity
Twins
Congenital, chromosomal, or metabolic abnormalities (blood disorders, mental retardation) Ethnicity of the mother and father (for possible screening tests)
How much weight should a woman be advised to gain in pregnancy?
Average women should gain between 25 and 35 lbs (underweight women should gain more and overweight women should gain less).
When does a fetus experience the most rapid weight gain?
In the third trimester; the fetus gains approximately ½ lb/wk
What is the recommended daily nutritional intake during pregnancy?
Calories: an additional 300 kcal/d for each fetus
Protein: increase daily intake by 5 to 6 g
Iron: requirements double to 30 mg/d
Calcium: increases by 1000 mg in the third trimester during fetal bone calcification
Daily intakes of copper (2 mg), folate (0.4 mg), vitamin C (50 mg), vitamin D (10 mcg or 400 IU), and vitamin B12 (2 mcg) should continue
Which substances and foods should be limited or avoided?
Tobacco, alcohol, street drugs
Herbal medications
Caffeine more than 500 mg or more than 4 cups a day (can cause SAB or growth restriction)
Iodine (can cause fetal goiter)
Large amounts of vitamins A, D, E, and K
Unpasteurized dairy
Methylmercury (in raw fish, shark, swordfish, king mackerel, and tilefish)
Should exercise change during pregnancy?
Activity can be maintained at the same intensity prior to pregnancy, in the absence of obstetric or medical complications. If a patient does not, she should be encouraged to begin light exercise.
How often are prenatal care visits scheduled?
Every 4 weeks during the first and second trimesters
Every 2 weeks in the third trimester (28-36 weeks)
Once a week near term (36-40 weeks)
Postdates will require more involved monitoring.
(Adequate prenatal care requires more than nine visits, with the first visit during the first trimester)
What are the four cardinal questions asked during each prenatal care visit?
1. Do you have any contractions?
2. Do you have any leakage of fluid?
3. Do you have any vaginal bleeding?
4. Do you feel fetal movement (after 20 weeks)?
What are important parameters in evaluating the pelvic shape?
Pelvic inlet (diagonal conjugate = distance from the pubic symphysis to the sacral promontory)
Prominence of ischial spines
Pelvic sidewalls (convergent vs parallel)
Shape of sacrum
What measurements are taken during each standard prenatal care visit?
Weight
Blood pressure
Urine dip (protein, glucose, leukocytes)
Fundal height
Abdominal doppler fetal heart rate (after 12 weeks)
Which vaccines should be offered to pregnant women?
Any required inactivated vaccines and the influenza vaccine (in the second or third trimester)
Do not give vaccines that contain active viral components (measles, mumps, oral polio vaccine, or rubella)
What is advanced maternal age (AMA)?
More than 35 years of age at the time of delivery
What symptoms must a patient be educated about? What do each signify?
Vaginal bleeding (SAB in first trimester, placental abruption or placenta previa in second or third trimester)
Edema, headache, blurry vision, right upper quadrant pain, epigastric pain (preeclampsia)
Dysuria, fever, chills (pylonephritis)
What are the signs and symptoms of preterm labor?
Any of the following symptoms between 20 and 37 weeks EGA:
Abdominal, vaginal, or lower back pain or pressure that does not improve after hydration/rest
Uterine contractions every 10 minutes for more than 1 hour
A sudden thinning or increase in vaginal discharge
Bleeding from the vagina
What is round ligament pain?
As the gravid uterus increases rapidly during the second and third trimester, tension on the round ligament may cause sharp shooting inguinal and groin pain. Rest, warm compresses, and acetaminophen may relieve the pain.
What is the prevalence of domestic violence (DV) among pregnant women?
DV affects approximately 1 in 6 women (more prevalent among pregnant than nonpregnant women).
What are routine intake prenatal labs?
Hematology: blood type and screen (T&S), hemoglobin and hematocrit
Rubella status (immune or nonimmune)
HIV
HBV (HBsAg)
Syphilis (RPR or VDRL)
Chlamydia and gonorrhea cervical cultures
Tuberculosis (PPD)
Urine culture
Pap smear
What are some appropriate screening tests for the following groups?
Mediterranean or Asian descent Hgb electrophoresis for thalassemia
African descent Hgb electrophoresis for sickle cell and thalassemia
Ashkenazi Jews descent Hexosaminidase A leukocyte assay for Tay-Sachs
DNA analysis for: Canavan disease, Bloom syndrome, cystic fibrosis, familial dysautonomia, Fanconi anemia, Gaucher disease, mucolipidosis Type IV, Niemann Pick disease, or Tay-Sachs disease
Caucasian descent Delta F 508 mutations for cystic fibrosis (autosomal recessive)
Serum phenylalanine level for phenylketonuria
In an Rh(−) pregnant woman with an Rh(+) father of the baby, would her first or second child be at greatest risk?
Her second child, because of isoimmunization and the development of anti-Rh antibodies. The first Rh(+) fetus will only be mildly affected, if at all.
What is the major complication associated with isoimmunization?
Hemolytic disease of the newborn (with possible hydrops, anasarca, or death)
How is Rh isoimmunization prevented?
With Rh immune globulin (RhoGAM)—an antibody to the D antigen
Who is given RhoGAM?
All Rh(−) mothers with a possible Rh(+) fetus
When is RhoGAM given?
At 28 weeks EGA
At delivery
with in 72 hours of an abortion or vaginal bleeding at any gestational age
Following all invasive procedures (CVS or amniocentesis)
Name some additional screening and diagnostic tests. At what EGA are these routinely completed:
Genetic Screening
First trimester: nuchal translucency screen (with serum free β-hCG and PAPP-A) is done between 11 and 13 weeks.
Second trimester: quad or triple screen is done between 15 and 18 weeks.
Anatomic survey with ultrasound (to assess for fetal anomalies): 18 to 20 weeks.
Glucose challenge test (GCT): 24 to 28 weeks.
Streptococcus group B (perineal and rectal culture): 36 weeks.
Repeat Hgb, Hct, and syphilis: third trimester.
In sexually high risk women, what tests should be repeated? At what EGA?
Gonorrhea, Chlamydia, and HIV after 28 weeks (third trimester)
What is the nuchal translucency?
A cystic space dorsal to the cervical spine measured by ultrasound at 11 to 13 weeks
It is a sensitive indicator of chromosomal abnormalities—a large diameter signifies a greater risk of aneuploidy and poor fetal outcome.
What other tests enhance the sensitivity of a nuchal translucency?
Maternal serum free β-hCG and plasma protein A (PAPP-A) measurements
What is measured in the triple screen?
α-fetoprotein (AFP)
β-hCG
Estriol (E3)
In the quad screen?
Quad screen: all of above plus inhibin A
When are these tests employed and what do they assess?
Between 16 and 20 weeks
Abnormal values correlate with various chromosomal, genetic, and developmental disorders
How should an abnormal triple/quad screen be followed-up?
With a detailed ultrasound and possibly an amniocentesis
What do the following triple screen results suggest?
↓ AFP, ↑ hCG, ↓ E3:
Trisomy 21
↓ AFP, ↓ hCG, ↓ E3:
Trisomy 18
An elevated AFP may indicate what fetal conditions?
Neural tube defects
Gastroschisis/Omphalocele (abdominal wall defects)
Fetal death
Placental abnormalities
A decreased AFP may indicate what fetal condition?
Down syndrome
What are the most common neural tube defects (NTDs)?
Anencephaly and spina bifida
What is a glucose challenge test (GCT)?
A screening test for gestational diabetes. The patient drinks 50 g of glucose and her blood sugar is tested 1 hour later.
What is the cutoff for the GCT?
Serum glucose greater than 130 to 140 mg/dL
What should be done if a patient has an abnormal GCT?
A diagnostic test called the glucose tolerance test (GTT)
What is a Glucose tolerance test (GTT)?
After an overnight fast, blood sugar is tested. 100 g glucose is then given and blood sugar is checked every hour for 3 hours.
What are the normal values for a GTT?
Fasting < 95 mg/dL
1 hour < 180 mg/dL
2 hours < 155 mg/dL
3 hours < 140 mg/dL
When is gestational diabetes diagnosed?
If there are two or more abnormal values on the GTT
An ultrasound done routinely on women between 18 and 22 weeks gestation that looks at the following:
1. Estimated gestational age of fetus
2. Size of fetus
3. Number of fetuses
4. Location of the placenta
5. Fetal cardiac activity
6. Amount of amniotic fluid
7. Basic anatomical structures (including the brain, spine, stomach, kidneys, bladder, and the four chambers of the heart)
What is a level II ultrasound?
A more detailed and targeted ultrasound done for high-risk women or women with a suspected fetal anomaly on their level I ultrasound.
What is chorionic villus sampling (CVS)?
A diagnostic procedure for genetic anomalies that involves transvaginal or transabdominal aspiration of placental cells at 10 to 13 weeks EGA.
What is the risk of CVS?
There is a 1/200 risk of adverse fetal outcome (such as limb deformaties) or demise. This is minimally higher than an amniocentesis.
What is an amniocentesis?
A diagnostic procedure done after 14 weeks EGA that can detect chromosomal/genetic abnormalities, amniotic infection, inflammation, and fetal lung maturity. It involves transabdominal aspiration of the amniotic fluid from the uterine cavity.
What is the risk of amniocentesis?
There is less than 1/300 risk of adverse fetal outcome (chorioamnionitis, preterm labor, ruptured membranes) or fetal demise.
What is quickening and when does it occur?
The mother’s first perception of fetal movement (FM); it usually occurs between 16 and 20 weeks (may be earlier in a multipara).
After 26 to 32 weeks, fetal well-being can be assessed by asking the mother to count FM, “kick counts,” which should occur at least eight times every 2 hours.
What are the commonly used tests of fetal well-being and when are they used?
Nonstress test (NST).
Biophysical profile (BPP).
Modified biophysical profile.
They are used most commonly for reassurance in high risk pregnancies or in the complaint of decreased fetal movement.
What is an NST?
Placement of an external fetal monitor to trace the fetal heart rate for 20 minutes. A tocodynamometer monitor is also placed to assess for uterine contractions (see Fig. 8.3).
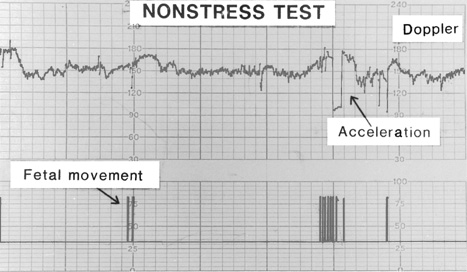
Figure 8.3 Reactive nonstress test. (Reproduced with permission, from Cunningham FG et al. Williams Obstetrics. 22nd ed. New York, NY: McGraw-Hill; 2005:279.)
What is a reactive NST?
Two accelerations above the baseline of 15 beats per minute (bpm) for 15 seconds within 20 minutes
What does a reactive NST indicate?
Reassuring fetal status
What is fetal tachycardia?
A baseline FHR more than 160 bpm
What is the most common cause of fetal tachycardia?
Maternal tachycardia
What are some other causes of fetal tachycardia?
Maternal fever
Anemia
Asphyxia
Infection
Autoimmune disorders
Adrenergic medications
Cardiac anomalies (eg, SVT)
What is fetal bradycardia?
A baseline FHR less than 110 bpm
What are some causes of fetal bradycardia?
Physiologic (short episodes because of transient compression of the fetal head/umbilical cord)
Maternal hypotension
Local anesthesia (eg, paracervical block)
Uteroplacental insufficiency (eg, placental abruption, uterine rupture, cord prolapse)
Cardiac anomalies
How is fetal heart rate variability assessed?
10 minutes of fetal heart tracing is reviewed to assess peak-to-trough differences in heart rate. Variability may be:
Absent
Minimal (< 5 bpm)
Moderate (normal = 6-25 bpm)
Marked (> 25 bpm)
What is suggested by a sinusoidal pattern on EFM?
Severe fetal anemia, hypoxia, or exposure to sedative hypnotics
What are the five components of the biophysical profile (BPP)?
1. Breathing: 30 seconds after 30 minutes of observation (seen as rhythmic deflection of fetal chest wall and diaphragm).
2. Movement: three gross body movements in 30 minutes.
3. Tone: extension and flexion of an extremity.
4. Amniotic fluid: vertical pocket is more than 2 cm or normal amniotic fluid index (AFI).
5. Reactive NST.
Each is worth 2 points for 10 possible points. The fetus is given 30 minutes to demonstrate each variable.
What do each of the following BPP scores signify?
8 to 10: reassuring fetal status with an intact CNS
6: equivocal test; repeat within 24 hours
4: high risk of fetal hypoxia; consider delivery
0 to 2: fetal hypoxia; delivery immediately regardless of EGA
Other than fetal hypoxia, what are some other causes of a low BPP?
Fetal sleep cycle
Transplacental sedatives
Corticosteroids
Which of the BPP elements are lost first as the fetus becomes progressively more hypoxic?
Breathing is lost early, then FHR accelerations, movement, tone, and finally amniotic fluid
How is chronic fetal stress manifested?
Oligohydramnios (AFI < 5 cm or vertical pocket < 2 cm), because of several days of decreased renal perfusion.
During hypoxic stress, where is fetal blood preferentially shunted?
Brain, heart, and adrenals
What are umbilical artery Dopplers?
A measurement of the ratio of systolic to diastolic flow (S/D) through the umbilical artery.
What is a normal S/D ratio?
Less than 3.0 in the third trimester because of low placental resistance; this ratio is dependent on gestational age
When should umbilical artery dopplers be done?
Only in cases of intrauterine growth restriction
Before the development of NST/BPP, what test was performed to assess uteroplacental insufficiency?
A contraction stress test (CST). Nipple stimulation or oxytocin was administered to induce three contractions (ctx) every 10 minutes with concurrent FHM. A normal test has no late decelerations. This is rarely performed today.
What are the three types of decelerations?
1. Early
2. Late
3. Variable
Describe early decelerations:
A gradual decrease from baseline that mirrors a contraction
What do early decelerations signify?
A vagal response from compression of the fetal head during uterine ctx; they are normal.
Describe variable decelerations:
A rapid decline of more than 15 beats from the baseline that is unrelated to uterine ctx.
What do variable decelerations signify?
Usually cord compression (can be relieved by changing the mother’s position)
Describe late decelerations:
A gradual decrease from baseline that starts after the ctx starts, peaks after the ctx peaks, and returns to baseline after the contraction has finished.
What do late decelerations signify?
Uteroplacental insufficiency
Fetal metabolic acidosis and hypoxia are suggested by what findings on a fetal heart tracing?
Recurrent, prolonged, and late decelerations
Minimal (> 5 bpm), decreased or absent long-term variability
Tachycardia (> 160 bpm), which may also be associated with infection or maternal fever
What is the significance of irregular contractions in the third trimester?
If the fetal status is reassuring, there is no cervical change, and ctxs are less than 4 per hour they are likely insignificant Braxton Hicks contractions.
If the contractions are painful, the patient may be in latent labor.
What is fetal fibronectin?
A glycoprotein that is normally present in maternal circulation and amniotic fluid. If it is present in the cervicovaginal secretions, it suggests that the cervix is undergoing structural change and the patient may go into labor in the next 2 weeks.
How is fetal fibronectin used clinically?
It has a high negative predictive value, so it is used to rule out preterm labor.
How is labor defined?
Regular uterine contractions that result in cervical effacement and dilation
How is labor diagnosed?
With tocodynamometry and serial cervical examinations
What are some of the signs of labor?
Painful contractions
Bloody show
Spontaneous rupture of membranes (SROM)
What is bloody show?
Vaginal passage of blood-tinged mucus
What are the four characteristics of cervical change?
Change in consistency (from firm to soft)
Change in position (from posterior to anterior)
Progressive effacement (cervix becomes shorter and thinner)
Dilation of the internal os (from 0-10 cm)
The following terms refer to rupture of fetal membranes (ROM) under what conditions?
SROM: spontaneous rupture of membranes (at ≥ 37 weeks)
PPROM: preterm, premature rupture of membranes (EGA < 37 weeks with rupture)
Prolonged PROM: rupture of membranes more than 18 hours without the onset of labor
What are the four signs and symptoms of spontaneous rupture of membranes?
Initial gush with continued loss of fluid
Pooling of vaginal fluid on sterile speculum examination
Positive nitrazine blue test (indicating that the vaginal fluid is alkaline, with a pH > 6)
Ferning of dried fluid under low power magnification (because of fetal urine salt crystals in the amniotic fluid)
What can cause a false-positive nitrazine blue test?
Anything that causes the vagina to become more alkaline, such as:
Sperm
Blood
Infection
Douching
What is the pH of amniotic fluid?
7.0
Describe the following terms:
Nulligravida: a woman who never conceived
Nullipara: a woman who never carried a fetus to viability
Primipara: a woman who has delivered a viable fetus in the past, regardless of the outcome of the fetus
Multigravida: a woman who has carried more than one fetus to viability, regardless of the outcome of the fetus
Grand multiparity: given birth five or more times
What is the term for a difficult delivery, protracted labor, or arrest of labor?
Labor dystocia
How does labor affect the shape of the fetal head (in cephalic presentation)?
The fetal calvarium undergoes molding, where the bones of the skull shift to minimize the diameter that must pass through the bony pelvis
On vaginal examination, the presenting fetal vertex is noted to be soft without any identifiable sutures or fontaneles. What is the term for this fetal finding (which often occurs in prolonged labors with slow cervical dilation)?
Caput succedaneum. the tissues overlying the fetal calvarium become edematous and swollen
Why are women in labor predisposed to gastric aspiration?
Increased intraabdominal pressure
Relaxation of the lower esophageal sphincter
Recumbent laboring position
What are some of the consequences of gastric aspiration?
Pneumonia
Bronchospasm
Adult respiratory distress syndrome (ARDS)
What precaution is taken in labor to minimize this risk?
Oral intake is restricted to clear liquids
What is a pudendal block?
A method of administering local anesthesia to the pudendal nerve (sacral nerve roots 2, 3, and 4), with subsequent decreased vulvar sensation.
How is a pudendal block administered?
Transvaginally. The anesthetic is injected medial and inferior to the ischial spines through the sacrospinous ligaments bilaterally.
When can an epidural be placed?
At any point in labor once the patient begins experiencing painful contractions
Where is an epidural catheter placed?
A guide needle is used at the interspinous space between the fourth and fifth lumbar vertebra. The ligamentum flavum is penetrated and the catheter is threaded into the potential epidural space, which consists of lymphatics and venous plexuses. An epidural injection enters the extradural or peridural space—it does not penetrate the dura mater.
Where is a spinal block placed?
It enters the dura and then the subarachnoid space, bathed by cerebral spinal fluid. Only the pia mater separates the cord from the injected substance.
What are the risks associated with epidurals and spinal blocks?
Spinal headache
Hypotension
Infection
Hematoma
High spinal blockade (leads to apnea)
Cord compression (a surgical emergency)
What advantages does a spinal block offer?
A faster onset and requires a lower dose of anesthetics
What risks are increased with a spinal block?
Hypotension
Nausea
Compromised placental perfusion
Ascending respiratory paralysis (because of anesthesia reaching the cervical nerve roots 3, 4, and 5)
Does regional, local, or general anesthesia increase the rate of cesarean delivery?
No
What is the fetal lie?
The crown-rump axis of the fetus in relation to the longitudinal axis of the uterus
What types of fetal lie are there?
Longitudinal
Transverse
Oblique
What is the fetal presentation?
The fetal part closest to the cervix and pelvic inlet
What is the most common fetal presentation?
Cephalic, followed by breech
What are the other types of fetal presentation? Describe them:
Types of cephalic presentation:
Vertex
Brow
Mentum
Face (depending on which part is leading through the cervix)
Types of breech presentation (See Fig. 8.4):
Frank breech (flexed hips and extended knees)
Complete breech (flexed hips and knees)
Footling breech (one knee flexed, one knee extended)
Other:
Hand
Shoulder
Funic (cord)
Compound (involves more than one fetal part leading)
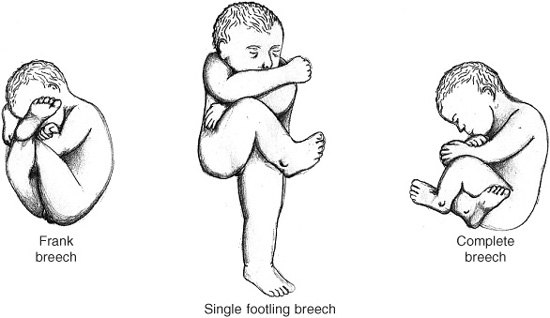
Figure 8.4 Breech presentation.
What is the incidence of mal-presentation (any presentation not cephalic) at the onset of labor?
Less than 4%
Fetal attitude or posture describes what characteristic?
The degree of flexion of the fetal neck, back, and joints of the limbs
Describe the fetal postures from most flexed to most extended:
Vertex → Military → Brow (forehead) → Face
What are the risks associated with an extended neck?
The fetus requires a larger leading diameter and thus has less ability to negotiate the birth canal. This can lead to labor dystocia.
What are the shapes of the two fetal fontanels and when do they close?
1. The anterior fontanel is diamond shaped and closes late in infancy (near 13 months).
2. The posterior or occipital fontanel is triangle shaped and closes early in infancy (near 2 months).
During labor how are the fetal fontanels examined? What is the significance of this examination?
The fetal scalp is examined on sterile vaginal examination (SVE). The location of the posterior fontanel is noted with regard to maternal left/right and anterior/posterior/transverse orientation. This describes the specific position of the presenting fetal head. (See Fig. 8.5)
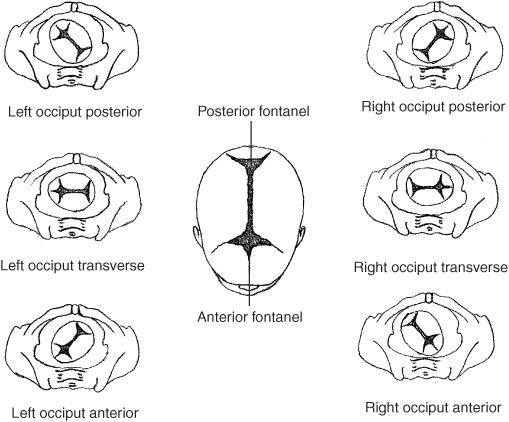
Figure 8.5 Vertex presentations.
Why does the occiput posterior (OP) position frequently cause labor dystocia?
Because the fetal head must be more flexed and rotate more extensively (135° instead of 90°) to pass under the symphysis pubis. Additionally, this position is often associated with brow or face presentations.
What is a normal synclitism?
When the leading sagittal suture is parallel to the pelvic outlet
What is anterior asynclitism?
When the sagittal suture is deflected toward the sacrum, allowing more of the parietal bone to be palpated anteriorly
What is posterior asynclitism?
Deflection of the fetal sagittal suture toward the maternal symphysis pubis. It is normal unless the tilt is severe.
How is the position of a fetus described in a face or breech presentation?
The relationship of the fetal mentum (chin) or sacrum are described in relation to maternal right, left, anterior, and posterior.
Leopold maneuvers convey what information about the fetus?
Estimated fetal weight (EFW)
Fetal presenting part
Fetal lie
Engagement
What are the four Leopold maneuvers?
First position: hands are placed at the cephalic margins of the fundus to determine the nonpresenting part that occupies the fundus and the fetal lie.
Second position: hands are placed at the right and left margins of the fundus to feel for small fetal parts and to confirm fetal position.
Third position: thumb and finger are placed just above the symphysis pubis to assess engagement of the presenting part.
Fourth position: facing the patient’s feet, the examiner’s fingers trace the fundus toward the pelvic inlet to identify the anterior shoulder with cephalic presentation and to assess the degree of descent of the presenting part (see Fig. 8.6).
Figure 8.6 Leopold maneuvers. (Reproduced with permission, from Cunningham FG et al. William Obstetrics. 22nd ed. New York, NY: McGraw-Hill: 2005:416.)
When is an SVE indicated?
During PNC visits at term
Upon presentation to labor and delivery with symptoms of labor
Periodically throughout the course of labor to assess progress
When should a manual pelvic examination not be performed?
When there is bright red blood per vagina. An ultrasound should be performed first to confirm no placenta previa.
When the membranes are ruptured, SVEs should be minimized (to reduce risk of infection).
What information is gathered during a manual pelvic examination?
Fetal position
Cervical dilation/cervicaleffacement/station of the presenting fetus
Cervical consistency (firm, soft)
Cervical position (posterior, anterior)
Clinical pelvimetry (diagonal conjugate, pelvic sidewalls, interspinous diameter, and a wide pubic arch)
What is the interspinous diameter and what is its significance?
The distance between the ischial spines Used to estimate the station of the presenting fetal part
What station is associated with each of the following positions?
A leading edge that is −3 cm above the ischial spines:
−3 station
A leading edge that is at the level of the spines:
0 station
A leading edge that is 3 cm past the spines:
+3 station
What is zero station (determined on SVE)?
When the leading fetal edge is at the level of the maternal ischial spines.
What is its obstetrical significance of zero station?
It represents the most narrow sagittal obstetric diameter and so signifies that the largest fetal diameter has engaged the bony pelvis.
What is the significance of pelvic classification and clinical pelvimetry?
Clinical pelvimetry seeks to describe the pelvic inlets, angles, and diameters. However, pelvic type and pelvimetry are not reliable predictors of vaginal delivery, labor dystocia, or cesarean section and so they are rarely employed in contemporary obstetrics.
What is the best indicator of pelvic adequacy?
Prior vaginal delivery, prior progress of labor, or family history ofcephalopelvic disproportion (CPD)
What defines the first stage of labor?
The onset of consistent painful contractions until the cervix is completely dilated (10 cm) and 100% effaced.
How is the first stage of labor further subdivided?
Into latent and active phase (See Fig. 8.7)

Figure 8.7 Schematic illustration of progress of cervical dilation against time in the successive stages of labor.
Regular painful contractions that result in cervical dilation up to 3 to 5 cm
Describe the active phase:
A faster rate of cervical dilation which typically begins after approximately 4 cm dilation and/or full effacement in the presence of regular uterine contractions that continues through full cervical dilation of 10 cm
What are minimum adequate rates of cervical dilation during the active phase?
For multiparas: at least 1.5 cm/h
For nulliparas: at least 1.2 cm/h
What are some conditions that slow the active phase?
Uterine dysfunction
Fetal malposition
CPD
How is the active phase of the first stage of labor further subdivided?
Acceleration phase: an increasing rate of dilation from 3 to 5 cm cervical dilatation to 8 cm
Deceleration phase: a slower rate of cervical dilation after 8 cm until full dilation
How is arrest of dilation defined?
More than 2 hours with no cervical change in the presence of adequate contractions
What is the second stage of labor?
From a fully dilated and fully effaced cervix until delivery of the fetus
What is a protracted labor?
When there continues to be some cervical change or descent of the fetus, however it is progressing slower than would be expected
Define protraction of the second stage in terms of fetal descent:
In nulliparas: fetal head descent less than 1 cm/h
In multiparas: fetal head descent less than 2 cm/h
Define protraction of the second stage in terms of length of labor (with and without an epidural):
In nulliparas:
2 hours without an epidural
3 hours with an epidural
In multiparas:
1 hour without an epidural
2 hours with an epidural
Complete cessation of dilation (no change for 2 hours) or descent (no change for 1 hour) despite adequate contractions
What are the causes of secondary arrest of labor?
Problems with the three “P”s:
Power (inadequate uterine contractions)
Passage (pelvic disproportion)
Passenger (malpresentation, macrosomia)
Define arrest of descent:
More than 2 hours in a nullipara or more than 1 hour in a multipara with no descent of the fetus despite adequate contractions.
If the patient has had an epidural or regional anesthesia she is given 1 additional hour.
When should a woman begin pushing to aid in the descent and delivery of the fetus?
During the second stage (after full cervical dilatation)
Why is pushing avoided in the first stage of labor?
To prevent cervical lacerations and maternal exhaustion
A nulliparous patient at term has dilated from 6 to 7 cm over 2 hours. Is this adequate change, protracted dilation, or arrest of dilation?
Protracted dilation (a nullipara should dilate at least 1.2 cm/h during the active phase of labor)
In the above patient, what should be done?
Her contraction pattern should be evaluated (possibly with an IUPC) and her labor can be augmented if her contractions do not appear to be adequate.
A rate of cervical dilation less than 5 cm/h in a nulliparous or 10 cm/h in a multiparous patient is considered what type of labor?
Precipitous labor
What risks are associated with precipitous labor?
An increased risk of fetal hypoxia, brain injury, and maternal morbidity such as hemorrhage and vaginal/cervical lacerations
How is the third stage of labor defined?
It begins after delivery of the fetus and continues until the placenta is delivered.
What is the acceptable duration of the third stage of labor?
Less than 30 minutes (although some clinicians will wait up to 60 minutes)
What are the three Gs that indicate the placenta has separated and is ready to be delivered?
1. Globular uterus
2. Growing cord
3. Gush of blood
What is the fourth stage of labor?
The acute maternal hemodynamic adjustment to the fluid shifts associated with labor that lasts 1 to 2 hours after delivery of the placenta
Why is the woman at increased risk for in the fourth stage of labor?
Postpartum hemorrhage
What are the seven cardinal movements of labor?
The positions that describe the behavior of the fetal head during the second stage of labor.
They include:
1. Engagement
2. Descent
3. Flexion
4. Internal rotation
5. Extension
6. External rotation (or restitution)
7. Expulsion (See Fig. 8.8)
Define fetal engagement in cephalic presentation:
When the biparietal diameter of the fetal head reaches the pelvic inlet or zero station (when the leading fetal edge has reached the ischial spines)
Why does a fetus flex and rotate during labor?
To negotiate the 90° concave curvature of the pelvic passage
The fetus presents the smallest diameter of its head (suboccipito-bregmatic diameter) by engaging what position?
Tight anterior flexion of the head (the inability to flex the head may lead to a dystocia)
How does the fetal head undergo internal rotation?
The fetus rotates so as to turn the saggital suture from a transverse to an anteroposterior position, it is a passive movement.
When does the fetal head undergo extension?
As the fetus is crowning at the introitus and the head has passed under the symphysis pubis
Figure 8.8 Cardinal movements of labor. (Reproduced with permission, from Cunningham FG et al. Williams Obstetrics. 22nd ed. New York, NY: McGraw-Hill: 2005:418.)
What cardinal movements occur while the fetal head is at the introitus?
Extension and external rotation
After the fetal head is delivered what subsequent steps should the clinician take?
1. Check for nuchal cord (umbilical cord around the neck).
2. Apply gentle downward pressure to assist the delivery of the anterior shoulder.
3. Gentle upward pressure for the posterior shoulder.
4. Support the subsequent delivery of the fetus’s body.
What are some indications for induction of labor (IOL)?
Prolonged pregnancy (postterm)
Diabetes mellitus
Rh alloimmunization
Preeclampsia
ROM at term
Placental insufficiency
Nonreassuring fetal status
Oligohydramnios
Intrauterine growth restriction
What are some contraindications to IOL?
Previous cesarean with a vertical uterine incision
Prior myomectomy entering the endometrial cavity
Malpresentation (breech)
Active genital herpes
Placenta or vasa previa
What is the Bishop score?
A rating system that evaluates a woman’s cervix to predict the likelihood that she will be able to deliver vaginally following IOL.
A score of 5 or greater is favorable.
What are the five cervical components of the Bishop score?
Consistency: firm = 0, medium = 1, soft = 2
Position: posterior = 0, middle = 1, anterior = 2
Effacement: 0%-30% = 0, 40%-50% = 1, 60%-70% = 2, ≥ 80% = 3
Dilation: closed = 0, 1-2 cm = 1, 3-4 cm = 2, 5-6 cm = 3
Station: −3 = 0, −2 = 1, −1 or 0 = 2, +1 or +2 = 3
Mnemonic: “see peds” (C PEDS)
What is the probability of a failed induction of labor with each of the following Bishop scores?
0-4: less than 50%
5-9: less than 10%
10-13: less than 1%
Preinduction cervical ripening can be achieved with what medications?
Prostaglandin PGE1: misoprostol (cytotec)
PGE2 or dinoprostone: prepidil (cervical gel) and cervadil (vaginal insert)
What mechanical techniques are used to ripen the cervix for IOL?
Hygroscopic cervical dilators (laminaria)—seaweed sticks that absorb water and expand
Balloon tipped transcervical catheter or Foley bulb
Membrane stripping or rupture to increase endogenous prostaglandins
What techniques can be used to count the number of contractions?
Palpation
External tocodynamometry
Intrauterine pressure catheter (IUPC)
Which of these devices is able to assess the force of the contractions?
Only IUPC
What are Montevideo units?
Quantifications of intrauterine pressure as determined by IUPC. They are calculated by multiplying the average peak strength of the contraction by the number of contractions over 10 minutes.
At what target MU are contractions considered adequate?
More than 200
What is uterine tachysystole?
More than five contractions in 10 minutes, averaged over a 30-minute window
What is a tonic contraction?
A contraction that lasts more than 3 minutes (usually in the context of a nonreassuring fetal tracing or fetal decelerations).
Why does uterine hyperstimulation/tonic contraction compromise placental blood flow?
The pressure in the placental sinuses exceeds maternal systolic BP, resulting in insufficient perfusion and fetal hypoxia
What aspects of the fetus can impact labor (passenger)?
Size (macrosomic > 4000 g)
Lie, presentation, attitude, position, asynclitism
Number of fetuses
Anatomic anomalies (sacrococcygeal teratoma)
Fetal scalp electrode (FSE) monitoring offers what benefits to electronic fetal monitoring (EFM)?
Continuous monitoring of the fetal heart rate in an obese patient or difficult to monitor fetus
How is the FSE applied?
Placental membranes must be ruptured and the electrode is adhered to the fetal calvarium
In what clinical setting is fetal blood sampling (fetal scalp pH) performed?
To acutely assess hypoxemia in the setting of nonreassuring FHR tracing, meconium, or other signs of fetal distress
What is suggested by the following range of fetal scalp pHs?
pH greater than 7.25: reassuring; a low probability of hypoxic-ischemic encephalopathy
pH 7.20 to 7.24: indeterminate; should be repeated in 30 minutes
pH greater than 7.20: a nonreassuring pH; delivery should be expedited with operative intervention
What other clinical information can be utilized to improve the predictive value of a low scalp pH?
FHR variability
What can be used to augment latent labor or prolonged early labor?
Cervical ripening agents (prostaglandins)
Intravenous oxytocin
An amniotomy
What is the effect of oxytocin (Pitocin) on labor?
It increases the frequency and force of uterine contractions.
What is the half-life of oxytocin?
3 to 5 minutes
A nulliparous patient is receiving 15 mU/min of intravenous oxytocin to augment her labor. Mother and fetus are tolerating labor well. There is no evidence of CPD, and an IUPC indicates 140 MU over a 10 minute interval. What is the next step in management?
Increase the oxytocin; the goal is to achieve more than 200 MU.
What are the risks involved with prolonged high-dose oxytocin administration?
Maternal SIADH and excessive fluid retention (pulmonary edema)
Hyperstimulation of the uterus
Postpartum atony and hemorrhage
Hyperbilirubinemia of the infant
Why is an amniotomy or assisted rupture of membranes (AROM) performed?
To induce or augment labor
To assess for meconium in the amniotic fluid
To place an IUPC or FSE
If the fetal head is not engaged in the pelvis or well applied to the cervix why is an amniotomy contraindicated?
Because of the risk of umbilical cord prolapse, compression by the presenting fetal part, and subsequent fetal hypoxia
A woman at 37 weeks EGA presents with painful uterine contractions, reassuring fetal status, no signs or symptoms of ROM, and an unchanged SVE after 3 hours. The cervix remains long, closed, and high. Irregular contractions occur at 15 to 20 minute intervals. What is your diagnosis?
Braxton Hicks contractions (prodromal or false labor)
How should the above woman be managed?
She should be hydrated, scheduled for close clinical follow-up, and advised to go home with labor precautions.
In the presence of a nonreassuring fetal heart rate what initial interventions should be tried?
Position the mother in left lateral decubitus position with flexed knees
Supplemental oxygen with a face mask Refrain from active pushing
Turn off the oxytocin and consider tocolytics (if tachysystole)
What is tocolysis?
Relaxation of the uterine smooth muscle
What substances are commonly used for uterine relaxation during tachysystole?
Terbutaline (or less often nitrous oxide)
What are the risks of applying traction on the cord during the third stage of labor?
Avulsion of the cord or uterine inversion
How can this risk be reduced?
By applying suprapubic pressure when applying gentle traction to the cord (fundal pressure should not be applied).
The placenta and uterus should be examined to ensure that no membranes or accessory lobes are retained.
After delivery of the placenta what is given to prevent postpartum hemorrhage?
20 units of oxytocin in 1 L of lactated ringers
What are the four classifications of vaginal and perineal lacerations?
First degree limited to vaginal mucosa and skin of the introitus
Second degree extends to the fascia and muscles of the perineal body.
Third degree trauma involves the anal sphincter.
Fourth degree extends into the rectal lumen, through the rectal mucosa.
What are the indications for an episiotomy?
To expedite delivery in the setting of nonreassuring fetal heart tracing or maternal exhaustion
Why is an episiotomy only performed with clear indication?
Third and fourth degree lacerations and anal incontinence of stool or flatus are more common with an episiotomy than with a spontaneous laceration.
What are advantages of midline episiotomies when compared with mediolateral episiotomies?
They are associated with fewer infections, faster healing, less pain, less blood loss, less dyspareunia, and better anatomical results.
What is the one advantage of the mediolateral episiotomy?
Decreased risk of extension to a third or fourth degree laceration
What muscles are affected by second degree lacerations?
Bulbocavernous and ischiocavernous laterally superficial transverse perineal muscle
What are the two major types of operative vaginal delivery?
1. Forceps
2. Vacuum
What is required for operative vaginal delivery?
Fully dilated cervix
Ruptured membranes
Engaged fetal head (at or below zero station)
Known absence of CPD
Known position of the fetal head
Experienced operator
The capability to perform an emergency cesarean delivery if necessary
What are the various types of forceps deliveries?
Outlet: fetal scalp is visible at the introitus and rotation does not exceed 45°.
Low: +2 station and may require more than 45° of rotation to AP orientation.
Mid-pelvic: head is engaged at or below 0 station (but above +2 station), rotation is often required to mimic the cardinal movements of labor.
High: above 0 station.
Operative vaginal delivery is appropriate or indicated in what context?
Fetal distress
Maternal exhaustion
Arrest of descent or prolonged 2nd stage
Contraindications to pushing
What are the most common maternal morbidities involved with forceps delivery?
Increased perineal trauma (third and fourth degree extensions)
Increased need for blood transfusion (these risks are increased with more rotation or at a higher station).
Vacuum delivery confers what advantages over forceps?
Can be achieved with minimal analgesia
What are some contraindications to vacuum-assisted delivery?
Low birth weight fetus (estimated fetal weight < 2500 g)
Prematurity less than 34 weeks
Suspected fetal coagulopathy
Recent scalp blood sampling
Face or breech presentation
An inability for the mother to engage in expulsive efforts
Cessation of contractions (vacuum traction must be coordinated with maternal effort)
What are the fetal morbidities involved with forceps and vacuum delivery?
Scalp lacerations, bruising, subgaleal hematomas, cephalohematomas, intracranial hemorrhage, neonatal jaundice, subconjunctival hemorrhage, clavicular fracture, shoulder dystocia, facial nerve injury, Erb palsy, retinal hemorrhage, and fetal death
Which operative vaginal delivery is associated with more trauma to the fetus?
Vacuum delivery—there is an increased risk of cephalohematoma and retinal hemorrhage when compared with forceps delivery.
Which operative vaginal delivery method is associated with more maternal trauma to the perineum?
Forceps
What are some indications for scheduled cesarean delivery?
Previous classical uterine incision
Prior myomectomy that entered the endometrial cavity
EFW is more than 5000 g (or > 4500 g in a diabetic)
Severe fetal hydrocephalus
Malpresentation (breech)
Active genital herpes
Placenta previa
What percentage of deliveries in the United States are cesarean deliveries?
Over 20%
What is the risk of a trial of labor in a woman with a prior classical uterine incision?
A 12% risk of uterine rupture, which is associated with fetal compromise, maternal shock, and a 10% maternal mortality rate.
What is the risk of uterine rupture in a laboring patient with a prior lower uterine segment incision?
Less than 1%
What are the signs and symptoms of uterine rupture?
Severe abdominal pain/uterine tenderness
Nonreassuring fetal heart rate tracing
Loss of fetal station
At what EGA is a cesarean section scheduled?
After 39 weeks in a patient with accurate dating of her pregnancy.
Fetal lung maturity tests should be performed if delivery is planned earlier or if the dating method is not adequate.
What is the lower uterine segment and what are the advantages of using this in a C-section?
The region of the uterus just superior to the cervix. The myometrium is significantly thinner than the uterine fundus (especially during labor) and is associated with a lower risk of uterine rupture in a future pregnancy.
What are the layers (from exterior to interior) that are incised with a Pfannenstiel or low transverse abdominal incision?
Skin → subcutaneous fat → superficial fascia (Camper’s and Scarpa’s) → anterior rectus sheath (fascia) → rectus abdominus muscle → preperitoneal fat → parietal peritoneum → visceral (vesico-uterine) peritoneum → uterus
What percentage of VBACs (vaginal births after cesarean) are successful?
60% to 80% are successful (depending on the indication for prior cesarean)
What term describes a pathologically thin lower uterine segment through which fetal membranes or fetal parts can be visualized prior to uterine incision?
A uterine window
What are some indications for a vertical lower uterine incision?
Premature breech fetus
Poorly developed lower uterine segment
Extensive fibrosis of lower uterine segment (following multiple cesareans)
Can the type of previous uterine incision be determined from the skin incision?
No
What is the duration of the postpartum period, also known as the puerperium?
6 to 8 weeks following delivery, when maternal physiology returns to the pre-pregnancy state
What is uterine involution?
The uterus returning to its pre-pregnancy size via contraction of the myometrium with subsequent atrophy. This constricts vessels and prevents hemorrhage
When is a pregnant woman at highest risk of developing venous thrombosis?
During the immediate puerperium period because of vessel trauma, immobility, increased fibrinogen, factor VII, VIII, IX, X, and platelets
Approximately 0.7 per 1000 women experience a venous thrombosis during pregnancy or postpartum.
During delivery, which nerve can be injured that leads to urinary retention?
The pudendal nerve; the neuropathy normally resolves within 2 months
Following a 300-minute second stage of labor, a G1P1 is unable to flex her hips against tension and has difficulty walking. What type of neuropathy is likely responsible?
Femoral nerve compression, secondary to hyperflexion of the hips during a prolonged second stage
Which episiotomy is associated with perineal or pelvic hematoma?
Mediolateral episiotomies
How soon should an Rh(D-) mother be given Rhogam (anti-D immune globulin), following delivery of an Rh+ fetus?
with in 72 hours of delivery
Where is the fundus during the postpartum period?
Immediately after delivery: near the umbilicus
After 24 hours: below the umbilicus
1 week: near the symphysis pubis
2 weeks: in the pelvis
6 to 8 weeks: it has assumed its nonpregnant size
What is lochia?
A combination of blood, serous exudate, erythrocytes, leukocytes, necrotic decidua, epithelial cells, and bacteria
What is the progression of the various types of lochia?
Lochia rubra (red): blood from the placental bed, mixed with tissue, lasting 3 to 5 days.
Lochia serosa (brown): older blood mixed with serous drainage, leukocytes, and cervical mucus, ending by the 10th day after delivery.
Lochia alba (yellow-white): lasts from the second to sixth week after delivery and has a small amount of blood, combined with leukocytes, epithelial cells, cholesterol, fat, and mucus.
How long does a woman shed lochia?
4 to 6 weeks; however, it should not be red for more than 2 weeks
What is suggested if a woman continues to have lochia rubra for over 2 weeks?
Retained products of conception (POC) must be considered
Her uterus, cervix, and vagina should be examined with possible dilation and curettage.
How much lochia is shed during the puerperium?
Initially it may be as heavy as a period and should gradually subside daily
The total amount lost is approximately 500 mL.
What is the management of a vaginal wound dehiscence?
Dehiscence of a vaginal laceration repair should be evaluated for infection, irrigated, and debrided of necrotic tissue. Sitz baths should be used liberally.
If discovered in the first 2 to 3 days after delivery, the wound can be resutured; however, if the tissue is friable or has evidence of infection, a secondary repair should be delayed for 6 to 8 weeks.
Antibiotics should be utilized if infection is noted.
What are some signs and symptoms of endometritis?
Elevated temperature (> 100.4°F or > 38°C)
Uterine tenderness
Purulent vaginal discharge
Leukocytosis
When does endometritis usually occur?
Usually within the first 3 to 5 days after delivery
It occurs in 4% of all vaginal deliveries and up to 10% of cesarean deliveries.
What are risk factors for the development of endometritis?
Prolonged ROM
Prolonged labor
Multiple internal examinations
Internal monitoring (FSE or IUPC)
Retained POC
Lower socioeconomic status
Poor nutrition
Concurrent genital tract infection
What is the treatment for endometritis?
It is a polymicrobial infection, with a mixture of aerobic and anerobic bacteria found. Treatment usually consists of gentamicin and clindamycin until the patient is afebrile for 24 to 36 hours.
What are other common causes of puerperal fever (postpartum or postcesarean-section fever)?
Wind (atelectasis or aspiration PNA)
Water (cystitis or UTI)
Wound (surgical site infection or laceration)
Walking (PE or a DVT)
Wonder drugs (medication side effect or adverse reaction)
Womb (endometritis)
Wet nurse (engorgement or mastitis: infection often with S. aureus or Streptococcus)
Phlebitis or septic pelvic thrombophlebitis
What are the five components of the Apgar score at 1, 5, and 10 minutes?
Appearance (blue, acrocyanosis, pink) Pulse (absent, < 100, > 100)
Grimace (none, present, vigorous)
Activity (flaccid, flexed, moving)
Respirations (absent, slow, crying)
Each component is given 0, 1, or 2 points
Silver nitrate, erythromycin, or tetracycline ointments are applied to the newborn’s eyes to prevent what ocular infection?
Chlamydia and gonorrhea
How does an infant benefit from skin-to-skin contact at birth?
Better temperature and glucose control, as well as an increased likelihood of maternal breastfeeding
Which vitamin is absent from human breast milk?
Vitamin K.
Infants are given a vitamin K shot at birth to prevent hemorrhagic disease of the newborn.
How does prolactin impact breastfeeding?
Stimulates milk production by the terminal exocrine glands
Nipple stimulation also increases oxytocin release from the posterior pituitary. How does this impact breastfeeding?
It causes contraction of the myoepithelial cells of the lactiferous ducts, allowing milk letdown.
How does breastfeeding prevent ovulation?
Prolactin inhibits the pulsatile gonadotropin releasing hormone from the hypothalamus.
What is colostrum?
Thick yellow breast secretions that contain plasma exudates, immunoglobulins (IgA), lactoferrin, albumin, and electrolytes. It is secreted during the first 2 days postpartum.
Why is an ELISA or Western blot repeated at 6 months and 1 year following delivery of an infant to an HIV+ mother?
Maternal transplacental IgG persists for several months in the infant’s serum.
The above tests check for antibodies to HIV, not the actual virus.
When does a breastfeeding woman’s milk “come in”?
3 to 5 days postpartum
Are mothers who are seropositive for the following conditions advised to breastfeed?
Hepatitis A: yes
Hepatitis B: yes, with vaccination and hepatitis B IgG administration to the infant at birth
Hepatitis C: yes
HIV: no
Are mothers who are exposed to the following substances advised to breastfeed?
Alcohol:
No
Street drugs:
No
Tobacco:
Yes
Hepatitis B vaccination:
Yes
Rubella vaccination:
Yes
Tetracyclines:
No
Sulfa drugs:
No, because they displace bilirubin and increase risk of kernicterus
Quinolones:
No
Chemotherapy:
No
Radiation:
No
Lithium or heavy metals:
No
Is previous mammoplasty (reduction or implantation) a contraindication to breastfeeding?
No. If the integrity of the nipple ducts are preserved, a woman can breastfeed; however, the surgical technique and subsequent scarring may make this difficult.
What is the caloric demand of lactation?
640 kcal/d
How much should breastfeeding women increase their daily caloric intake?
300 to 500 kcal
How much calcium should a breastfeeding woman consume?
1200 mg/d of calcium
A mother does not want to breastfeed although her breasts are extremely tender 5 days postpartum. What is appropriate management?
Tight-fitting bras, avoidance of nipple stimulation, cool compresses, acetaminophen or ibuprofen
How is cardiac output (CO) affected during the first day postpartum?
A 60% to 80% increase in CO occurs with the autotransfusion of uteroplacental blood to the intravascular space and decompression of the vena cava.
A leukocytosis less than 25,000 and low-grade fevers less than 101 are considered normal or abnormal 24 hours postpartum?
Normal
Over what time period does the CO and systemic vascular resistance gradually return to nonpregnant levels?
3 to 4 months, with concurrent reduction in left ventricular size and contractility
How does a prepartum cervix (cx) differ from a parous cx?
The prepartum cervical os can be described as a “pinpoint.”
Over several weeks following delivery, the cx slowly contracts, with the cervical os appearing as a transverse, stellate slit.
Why is a woman who has delivered vaginally at risk for pelvic relaxation, cytocele, rectocele, or incontinence?
Connective tissue and fascial stretching may not return to the pregravid state, resulting in persistent trauma or changes.
What is a persistent defect of the abdominal wall musculature caused by the gravid uterus known as?
Diastasis recti
How much weight is lost following delivery?
Almost half of the gestational weight gain is lost following delivery (13 lbs), with the additional weight loss occurring over the next 6 months (15 lbs).
Do women typically gain weight following pregnancy?
Most women maintain 10% of their gestational weight following the postpartum period
Why do some women note increased alopecia postpartum?
Scalp hair shifts from the predominant anagen phase (growing) during pregnancy to a predominant telogen phase (resting). This telogen effluvium typically resolves within 5 months.
What is the condition in which a woman displays hypopituitarism following a delivery with postpartum hemorrhage?
Sheehan’s syndrome, because of infarction and necrosis of the pituitary
When does serum human chorionic gonadotropin (HCG) return to normal (nondetectable levels)?
Within 4 to 6 weeks of delivery or abortion
What is suggested by a rising HCG postpartum?
Gestational trophoblastic disease
Why do some women note vaginal atrophy in the puerperium?
Prolactin inhibition of systemic estrogens
How is the thyroid affected postpartum?
Hormone levels are within normal limits by 4 weeks and the thyroid gland decreases to prepregnancy size over 3 months
When does ovulation and menstruation begin in a postpartum nonlactating woman?
Ovulation typically resumes within 45 days to 4 weeks.
Average duration to menstruation is 8 weeks postpartum.
When does ovulation and menstruation begin in a postpartum breastfeeding woman?
A woman who is breastfeeding more than 5 times a day can remain anovulatory for the duration of breastfeeding.
How long should the woman maintain “pelvic rest,” by refraining from coitus or inserting anything in the vagina?
6 weeks postpartum, so as to decrease the risk of an infection ascending through the patent cervical os, and to reduce the risk of infection or trauma to healing lacerations
What type of birth control will not affect breastfeeding?
IUD
Barrier methods
Progestin only pills (mini pill)
Depo-Provera
Why do oral contraceptive pills (OCPs) and Norplant affect breastfeeding?
Estrogen decreases breast milk production. It can be safely started 6 weeks after delivery if milk production is adequate.
Why do some clinicians recommend that women obtain an IUD 6 weeks postpartum instead of insertion at the time of delivery?
Decreased risk of expulsion because of patent os and uterine cramping
A 28-year-old G1P0 at 39 weeks gestation presents to L&D after leakage of fluid. She is ruled in for SROM with positive ferning, pooling, and nitrazine. She is contracting every 4 to 5 minutes and is admitted in latent labor. On the monitor, the fetal heart tones are 140 bpm with moderate variability, positive accelerations, but frequent brief spiky decelerations unrelated to contractions. What is the etiology of the variable decelerations?
a. Oligohydramnios
b. Uteroplacental insufficiency
c. Umbilical cord compression
d. Fetal head compression
Answer: c
What is being described are variable decelerations. These are thought to be caused by cord compression and do not signify fetal distress. Oligohydramnios increases the risk of cord compression, however it does not cause compression. Uteroplacental insufficiency leads to late decelerations which follow the onset of contractions and return to baseline after the contraction is complete. Fetal head compression leads to early decelerations, which begin and end with the contraction due to fetal vagal nerve stimulation.
A 32-year-old G2P1 at 30 weeks gestation presents to the hospital with left sided pelvic pain. It is cramping in nature but does not radiate. There are no associated fevers, no dysuria, and no hematuria. On examination she has no costovertebral angle tenderness. Her WBC is 10,000/mL. Her UA is negative for infection or blood. A renal US is performed with the finding of mild right hydronephrosis. What is the likely etiology of this finding?
a. Ureterolithiasis
b. Pyelonephritis
c. Compression of the right ureter by the uterus and right ovarian vein
d. Progesterone-related smooth muscle relaxation
e. c and d
Answer: e
Without evidence of stone on US, ureterolithiasis is unlikely. While pyelonephritis is more common in pregnancy, without a fever, CVAT, or infection on the UA this diagnosis is effectively excluded. Mild to moderate hydronephrosis in pregnancy is common, especially on the right, as a result of compression by the uterus and ovarian vein as well as by progesterone-mediated smooth muscle relaxation.
A 26-year-old G5P3013 at 12 weeks gestation calls with symptoms of shakiness, vomiting, and a 5 lb weight loss over the past 2 weeks. These symptoms developed 8 weeks ago, but have worsened. You call her in to your office and draw labs. Which of the following would you expect to see on TFTs?
a. Increased total thyroxine
b. Normal total thyroxine
c. Decreased total thyroxine
d. Decreased free thyroxine
e. Decreased thyronine binding globulin (TBG)
Answer: a
This patient has symptoms of hyperthyroidism. Total thyroxine (T4) is increased in this patient as a result of this condition. Furthermore, in pregnancy TBG levels are increased. This leads to an increase in total thyroxine.
A 42-year-old G1P0 at 14 weeks gestation presents to your office for routine obstetrical care. She has no medical history and no notable family history. She asks about risk of genetic abnormalities. You discuss amniocentesis, however she does not want such an invasive test. Which of the following tests would be indicated?
a. Maternal alpha fetoprotein (AFP)
b. Fetal nuchal translucency
c. Fetal nuchal translucency with maternal serum PAPP-A and β-hCG
d. Maternal serum AFP, hCG, estriol, and inhibin-A
If this patient declines diagnostic genetic testing (amniocentesis or CVS), genetic screening should be offered. The most sensitive test is an integrated or sequential test, which includes early nuchal translucency combined with maternal serum testing in the first and second trimesters. However this patient is presented too late for that option. In the second trimester, the triple or quad screen (answer d) is the only available tests.
A 27-year-old G1P0 at 41 weeks gestational age presents to L&D with painful contractions. Her cervix changes from 2/2/-2 to 5/0.5/-1 over 2 hours and she is admitted in labor. Fetal heart tones are reactive and she is contracting every 1 to 2 minutes. As an IV is being placed there is a large gush of blood and followed by difficulty in tracing the fetal heart tones. Her heart rate is 82 bpm and her BP is 108/64. What is the immediate next step in management?
a. Emergency cesarean section
b. Type, cross and transfuse two units of packed red blood cells
c. Place an intrauterine pressure catheter (IUPC)
d. Place an internal fetal scalp electrode (FSE)
Answer: d
A gush of blood may be indicative of placental abruption and thus continuous fetal monitoring is imperative. When fetal heart tones are difficult to trace externally, an internal monitor (FSE) can be quickly placed to monitor the fetal heart rate. There is no need for emergent delivery until fetal distress or significant maternal hemorrhage is evident. She is hemodynamically stable and does not need a transfusion. An IUPC is used to monitor contraction intensity and is not indicated.
A 28-year-old G3P2 presents to L&D at 38 weeks gestational age in active labor. She began contracting 5 hours ago and her cervical examination on admission was 8 cm dilated. She is expectantly managed for 2 hours when the nurse calls to ask you to evaluate the fetal heart rate tracing. The baseline is 130 bpm with moderate variability and decelerations that begin and end with each contraction. What is the physiologic etiology of this fetal heart rate pattern?
a. Oligohydramnios
b. Uteroplacental insufficiency
c. Umbilical cord compression
d. Fetal head compression
Answer: d
This patient is in active labor and is likely completely dilated. Decelerations and begin and end with a contraction are early decelerations and are a consequence of fetal head compression. Oligohydramnios in and of itself does not cause decelerations. Umbilical cord compression leads to variable decelerations which appear as decelerations unrelated to contractions (variable in morphology and timing).
A 19-year-old G1P0 presents to L&D at 38 weeks gestational age with painful contractions. She was 2 cm dilated and progressed to 5 cm within 2 hours. She is admitted to L&D and expectantly managed, contracting every 3 to 4 minutes. Four hours later, spontaneous rupture of membranes occurs and she is found to have an unchanged examination. The estimated fetal weight by Leopolds is 7 lbs and clinical pelvimetry deems her to have an adequate pelvis. Fetal heart tones are reassuring and contractions are occurring every 4 to 5 minutes. What is the next step in management?
a. Cesarean delivery
b. Ambulation and reexamination in 2 to 4 hours
c. Begin labor augmentation with oxytocin
d. Discharge the patient home
Answer: c
This patient is in arrested active labor. Arrested labor is defined as no cervical change, whereas protracted labor is defined as cervical change of less than 1.5 cm/h in a multiparous patient or less than 1.2 cm/h in a nulliparous patient. Either can be initially managed with oxytocin augmentation. Cesarean delivery is not indicated at this time. Expectant management does not facilitate delivery and may increase the risk of chorioamnionitis in this patient who has ruptured membranes. Rupture of membranes requires delivery, and thus discharging this patient would not be indicated.
A 34-year-old G2P1 presents for routine prenatal care. Her prior OB history is notable for a low transverse cesarean section for arrest of descent. She delivered a healthy 3800 g infant. She wants to avoid another cesarean section and asks about TOLAC (trial of labor after cesarean). Which of the following statements is true?
a. She should be induced at 37 weeks to minimize the risk of cephalo-pelvic disproportion.
b. The risk of uterine rupture is under 1%.
c. Current guidelines recommend a repeat cesarean section.
d. Her risk of repeat cesarean is decreased because of her prior cesarean indication.
Answer: b
TOLAC is an option for women with one or two prior low transverse cesarean sections. Risks include uterine rupture which occurs in less than 1% of cases. If this occurs, there is an approximately 10% risk of a severe adverse neonatal outcome. Induction increases the risk of uterine rupture and thus spontaneous labor is desired. Women that have a history of a nonrecurring indication for cesarean (such as placenta previa or breech presentation) are more likely to have a lower risk of a repeat cesarean.