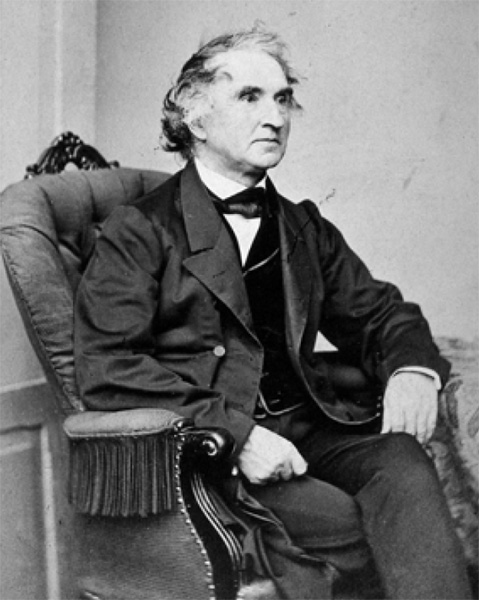
Justus von Liebig. Photograph by F. Hanfstaengl. Wellcome Collection
Opium and morphine were natural products, made from a plant. So was almost every other drug available to physicians in the mid-nineteenth century (along with a few non-plant substances like mercury). They were all refined from nature.
But that was about to change. Science in its modern sense—that is, based entirely on observation, experimentation, publication, and replication—was just beginning to make a mark on the world of drugs. The old structures built to explain health and the natural world—a tangle of ancient theories from Rome and Greece, leavened with some Arabic insights, and shoehorned into a Christian framework—had already given way. Now the new sciences were about to release a flood of new drugs.
No scientific discipline in the mid-nineteenth century was as dynamic, as revolutionary, or as important to medicine as chemistry. At a very simple level, chemistry is about how atoms join together to make molecules, and how those molecules behave with one another. It was here, at the level of molecules, that chemists in the 1800s crashed headlong into religion.
It had to do with the definition of life. In the West, the dividing line between life and death had long been set by Christianity. The difference between the two was the presence of a holy force, a God-given spark that separated dead rocks from living creatures. This was not only a religious idea; many scientists around 1800, for instance, believed that the chemicals found in living things—organic chemicals—were fundamentally different from other chemicals. There was some good evidence to back them up: While chemical reactions in a lab, for instance, could in most cases be reversed, with reactants changing to products and products changing back to reactants, reactions using chemicals made in living bodies, it was thought at the time, could not. You could not turn wine back into grape juice or unfry an egg. The organic chemicals involved in the processes of life, it was thought, must have something in them that was different from other chemicals. Their actions could not be treated or studied the same way, and thus were lumped together as the new field of organic chemistry. There was something unique about them; they operated by a different set of rules, were touched by something else—perhaps that vital spark.
This idea of vitalism permeated chemistry in the 1700s and early 1800s. Chemists took sides: Some believed that all chemicals were the same, and that eventually organic chemicals would be seen to conform to the same rules that governed the rest of chemistry. There was no vital spark, no mystical something that separated life from death. Others argued that there was certainly something different, more special, perhaps divine about chemicals involved in living organisms.
Most healers of the day continued to believe that life was permeated with a special spirit, and that a balance and flow of vital forces in the body guided health. These “special forces” ideas ruled Western medicine for centuries under the general heading of the four humors, while in China it was seen as the flow of chi. Today, it lives in the alternative healer’s belief in subtle energies.
But not in chemistry. The idea of this hard-and-fast dividing line between the quick and the dead took a literary blow in 1818 with the publication of Mary Shelley’s novel Frankenstein; or, The Modern Prometheus, with its doctor-protagonist playing God by restoring life to dead tissue, and then a more scientifically important punch in 1832, when the German chemist Friedrich Wöhler showed that he could synthesize one of the substances thought to be made only in living bodies, the molecule urea, entirely in his laboratory from the combination of two dead chemicals. This seems like a small thing now. But at the time it was a big deal. Science, with its ever-more-powerful array of facts and techniques, was blurring the line between life and death. Scientists were crossing a threshold.
Wöhler’s great friend—and arguably even greater chemist—Justus von Liebig took the next steps. Liebig was a phenomenon of science, a true genius, a great teacher, who was passionate about applying chemistry to everything—especially living processes. This German chemist was fascinated with the ways in which living organisms interacted with the nonliving world, especially the chemistry of that interaction. He was the first to show, for instance, that growing plants required certain mineral elements—nitrogen, phosphorus, potassium, and so forth—in order to thrive. In other words, he figured out how fertilizers work. He was the father of agricultural chemistry. And this difficult, demanding, opinionated man also had a lifelong interest in drugs. He became doubly famous as the father of clinical chemistry, the use of chemistry in medicine.
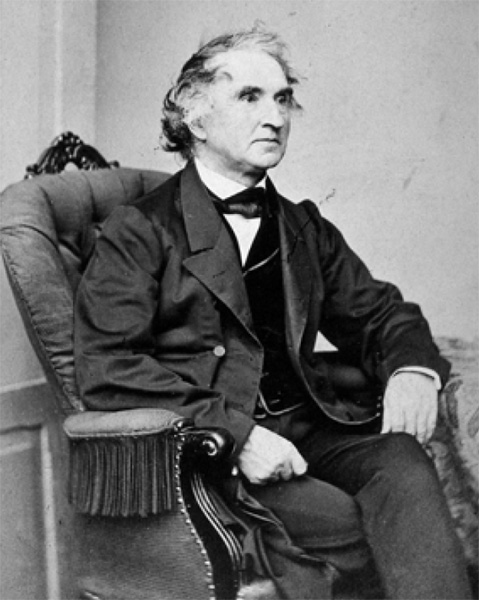
Justus von Liebig. Photograph by F. Hanfstaengl. Wellcome Collection
In fact, what Liebig was doing was demonstrating that nutrition, growth, the processes of life itself did not come from God alone, but from chemical changes. He summarized his ideas in his 1842 book, Animal Chemistry.
After Liebig, most scientists considered that living processes could effectively be reduced to a series of chemical reactions. The body could be picked apart in finer and finer detail, reduced all the way down to the level of molecules. This reductionist approach has guided much of the study of life ever since. God no longer sets the terms of the argument.
Along the way, Liebig made a lot of interesting new chemicals. One of them, chloral hydrate, first emerged from his lab in 1832. This entirely synthetic chemical could not be found in the body; it had never existed on earth, as far as anyone knew, until Liebig made it. And yet it was destined to be used as a medicine.
Liebig didn’t know that. He never thought of using it as a medicine. He was tinkering, playing with molecules, learning what transformed one into another. He found, for instance, that he could turn chloral hydrate into a heavy, sweet-smelling liquid called chloroform, the fumes from which could knock a person unconscious. By the 1850s, chloroform was being tested as a way to put patients to sleep before surgery. But it was too hard to handle, too dangerous—it was easy for patients to breathe in too much, and accidental deaths happened on the operating table—so researchers set it aside and started looking for alternatives. Liebig had shown that he could transform chloral hydrate into chloroform in his lab, so might the same thing happen in the body? Could chloral hydrate be a safer alternative to chloroform? They started testing it on animals.
Chloral hydrate is a solid at room temperature, but it can be made into a more easily administered liquid by simply mixing it with alcohol. In either form, solid or liquid, it was found in the 1860s to be great at putting humans to sleep. It had been around too long to be patented—its medicinal use didn’t start until decades after Liebig first made it—but it was made by a number of firms and widely used.
Although natural drugs like opium could make users sleepy, they also had other effects. This made chloral hydrate, in the eyes of many historians, the first true sleeping pill, a class of drugs physicians called “hypnotics.” A little chloral could calm patients down, a bit more could help ease them to sleep, a lot could knock them out. By 1869 it was being sold as a sleeping aid and a way to soothe patients before surgery. More than being the first hypnotic, chloral was the first widely used, totally synthetic drug.
Within a few years it grew into an international fad. Like morphine, it was taken both as a medicine and as a recreational drug. Nervous Victorians used it to tranquilize themselves. Insomniacs devoured it before bedtime. Partygoers played with its effects. As the New York Times reported from London in 1874: “Chloral is the now-fashionable hypnotic, the means by which balmy sleep, nature’s sweet restorer, is wooed.”
It was also dangerous. As use spread, so did reports of accidental overdoses and use in suicide. And worse.
In the fall of 1900, a seventeen-year-old girl named Jennie Bosschieter took an evening walk from her family’s working-class apartment in Paterson, New Jersey, to get baby powder for her niece. She never came home. The next morning a milkman found her body on the shores of the Passaic River. She’d been raped. And poisoned. An autopsy showed that she’d overdosed on chloral hydrate.
The story that emerged became a Gilded Age cause célèbre. A few days after Bosschieter’s body was found, the driver of a horse-drawn hack admitted that he’d picked her up at a saloon the night before, when she was carried into his carriage by four men who brought her out of the saloon’s side door. She was unconscious but alive. The men directed the driver to an isolated spot out in the country, where, he told police, they spread a blanket and repeatedly assaulted the girl. The only time they paused was when she vomited. When they got her back into the carriage, she was limp and unresponsive. Her attackers got worried. These four young men seemed well-connected; they directed the carriage driver to the home of a leading local physician who was a family friend of one of the girl’s attackers. But it was too late. The girl was dead. They carried her body back to the carriage, ordered the driver to the river, dumped the body, and gave the driver $10 to keep his mouth shut.
It wasn’t enough. A few days later the driver went to the police, the police went to the doctor, and the doctor gave up the young men. They were all from respectable, wealthy local families. One of them was the brother of a judge.
The four men blamed the victim, saying that she’d joined them voluntarily, flirted with them, was drunk and throwing her arms around them. They bought her absinthe and champagne, they testified, but knew nothing about any chloral. They simply took her for a carriage drive, got worried when she passed out, then panicked when she died. They couldn’t explain why her underwear was missing. Or how a bottle with chloral in it was found near the body.
The better elements in town chose to believe the young men, and rumors began flying about this loose factory girl, a working-class teenage strumpet who had cast a spell over their favorite sons. A socialist newspaper came to Bosschieter’s defense, framing her death as an attack on the working class by upper-class degenerates. The newspapers loved it.
The eventual trial was a public spectacle, the courtroom packed and buzzing. Hundreds who’d been turned away milled about outside, yelling at witnesses as they arrived.
Under cross-examination the four young men, counseled by some of the area’s best attorneys, stuck to their story. But the evidence was too damning. After three days, they were all convicted of second-degree murder. Three of them were given thirty-year sentences. The fourth finally confessed to the crime, provided details, and was given fifteen years. All of them were released after serving little more than half their sentences, thanks to years of what one newspaper called “relentless pleas for clemency on their behalf by Paterson’s influential class.”
Jennie Bosschieter had died from a mixture of chloral hydrate and alcohol commonly called “knockout drops.” It was the original date-rape drug. And it found other uses as well.
There was Mickey Finn, for instance. Now more a phrase than a figure, Finn was likely a real person, the bartender and manager of a saloon that operated around the turn of the century on the South Side of Chicago. In 1903, a prostitute named “Gold Tooth” Mary Thornton testified that one Michael Finn, manager of the Lone Star Saloon, was poisoning his customers and robbing them. The simple system worked like this: Finn or one of his workers, a waiter or a “house girl,” would slip chloral hydrate into a likely customer’s drink; when the drug took effect, the semiconscious customer was escorted (or carried) into a back room, robbed, and dumped in an alley. Later the victim couldn’t remember much.
Finn was caught and his bar shut down, but the idea of “slipping somebody a Mickey” was just getting started. Knockout drops would become part of the criminal fabric of America.
Chloral’s legitimate uses, most of them in mental hospitals, were even more important. Sometimes mental patients were out of control, manic, thrashing—a danger to themselves and those around them. In the old days, attendants had used force and restraints like straitjackets to manage them, and opium, morphine, even cannabis to calm them. But chloral was better, faster, less liable to cause hallucinations, and a more controllable way to knock patients out. In smaller doses it could calm agitated patients and ensure a quiet night of sleep for patients and attendants alike. It’s no wonder that for three decades around the turn of the century, you could tell you were in a mental hospital even if you were blindfolded. It was the smell—the pear-like smell of chloral from the breath of patients. The mental wards reeked of it.
The chloral era lasted until around 1905, when chemists came up with even better synthetic drugs, barbiturates, followed in the 1950s and 1960s by early forms of today’s tranquilizers, and the more powerful antipsychotics (see the chapter on chlorpromazine, this page).
We now have hundreds of types of improved sleeping pills, better relaxants, and more varied drugs for criminals to lace into their victims’ drinks. Chloral still gets prescribed and used (it was, among other things, in the cocktails of drugs that killed Marilyn Monroe and Anna Nicole Smith), although it’s now a minor player.
But it earned its place in history. Chloral, the first widely used, totally synthetic drug, broke new ground. It proved that scientists working with test tubes in laboratories could make medicines that could match or exceed the power of those made by nature. Its eager adoption by mental health experts, its enthusiastic use by sleepless members of the public, even the subsequent press attention to its lurid criminal use all pointed toward profits that could be made by exploring other laboratory-made drugs.
Liebig’s and Wöhler’s scientific heirs, the generations of organic chemists who came of age in the late 1800s and early 1900s, became masters at tinkering with molecules that had an effect on the body, adding a few atoms here, taking away a few there, tailoring them for specific purposes. The more new chemicals they made and tested on animals and humans, the more they learned about what worked to promote health and what didn’t. Along with the blooming of chemical industries in general, a few chemists began devoting themselves to finding new synthetic drugs.
Knockout drops helped give birth to the behemoth we now call Big Pharma.