Clearing Airway Obstructions
Active babies and toddlers are very impulsive creatures, with little awareness of danger. The sobering truth is that accidents are the leading cause of death and disabilities for young children. Most parents with new babies don’t spend a lot of time thinking about how to protect them from accidents. But as your baby grows and her body skills develop, you’ll soon discover yourself stocking up on babyproofing products such as outlet covers, pads for table corners, and safety gates in an attempt to protect your active and curious toddler from household hazards.
It’s almost inevitable that at some point during your baby’s first year, you’ll have a moment of total terror when your baby chokes, swallows an object, or falls and gets a nasty-looking bruise or cut. More often than not, you’ll be spared the worstcase scenario, but it always pays to be prepared.
All healthy children get their share of cuts, bruises, and scrapes as they develop their body skills, but sometimes serious accidents that can be life-threatening do occur. Nearly one-fourth of all children suffer an injury severe enough to require medical attention. In fact, accidents are the leading cause of death in children and young adults ages one to twenty-one. And, no matter how watchful and careful you are, your baby can get hurt before you can intervene— even if you’re only a few feet away.
Most of the emergencies covered here can be avoided by thinking ahead. Accidents occur most often in an atmosphere of stress—when you’re overly tired, when you and your baby are hungry, when parents are fighting with each other, or when you and your baby are in a new and unfamiliar situation, such as visiting neighbors or relatives.
Exploring babies need to be constantly monitored when they are awake. Hazardous products—such as adult medications, cleaning supplies, and sharp objects—have to be stored completely out of the reach of a crawling and roaming toddler.
As your baby’s world expands, she will be exposed to new adventures but also to new risks. A toddler has to learn the meaning of “no” when it comes to touching hot stoves, approaching unknown animals, racing out into the street, or exploring bodies of water. But it’s a hard lesson to teach because babies are so taken with the world and its distractions. Even with the greatest of care, it’s going to be virtually impossible to eliminate all risks. But, thinking in advance about how you will handle an emergency can help a lot. It also helps to have emergency medical supplies on hand and to rehearse what you would do if something unexpected were to happen.
| TYPE OF INJURY | PREVENTION | FIRST STEP | SECOND STEP | WHEN TO SEEK MEDICAL HELP |
| Abrasions (such as skinned knees, elbows, or forehead) | Don’t allow your tot to play on concrete, asphalt, or hard dirt surfaces. | Rinse the area to remove all dirt, gravel, or sand; then wash with soap and running water without rubbing. | Dry thoroughly and apply an antibiotic ointment. Cover with an adhesive bandage or gauze pad on elbows and knees. Change dressing frequently until the wound begins to heal. | Call your health-care provider when the wound covers a large surface, such as the back or abdomen; when it is on the face, especially near the eye; when it’s embedded with dirt, stones, or gravel that are not easily removed (they may cause scarring); and when there are signs of infection, such as increased warmth, redness, swelling, or pus-like drainage. |
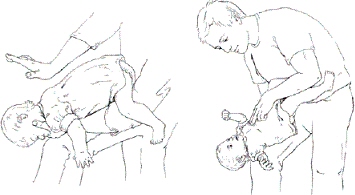
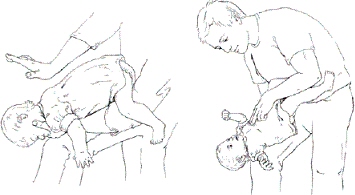
| Airway obstruction (choking, suffocation, and strangulation that prevents oxygen from getting to the lungs and brain) | Keep the baby safe from ingesting small objects, getting entangled in sheets or cords, and suffocating in blankets, waterbeds, or beanbag chairs. Keep the baby away from common offenders like deflated balloons and pieces of meat. Have every adult in the family learn CPR. | Try to clear the obstruction. (See illustrated instructions in Clearing Airway Obstruction on page chapter in this chapter .) | Perform infant CPR while someone calls 911. | Call 911 and/or go to the emergency room if the baby is having any kind of breathing problem. |
| Animal bites | Keep your curious baby away from animals, and especially guard your baby in others’ homes and yards. | If the skin is broken, wash thoroughly with soap and running water and dab hydrogen peroxide in the wound. Cover the wound with sterile gauze or a bandage. | Infection is a danger whether the bite is from a playmate, a wild or stray animal, or a family pet. Seek medical care, and try to have the animal confined for rabies testing. A rabies vaccination may be needed. | Any child who has a bite wound with broken skin should have medical treatment. Call your doctor’s office or go to the emergency room for care. (And remember to notify your child’s health-insurance carrier of your visit within 24 hours.) |
| Cuts or scrapes | Remove squarecornered coffee tables from your living area (or cover the corners with corner guards). Remove sharp-edged or glasstopped tables and other furniture as well. Don’t allow your newly walking baby to play on gravel or asphalt surfaces, or where there could be broken glass. | Wash your hands with soap and water, and then gently wash the baby’s wound. Pat the area dry with a sterile gauze pad, applying pressure to help stop the bleeding, if needed. | Spread just the wounded area with antibacterial ointment. Wash your hands again to get the grease off your fingers, then cover the wound with a bandage. Newer, waterproof bandages work best. Change the bandage daily, inspecting for redness or pus, the signs of infection. | Seek medical attention if your baby’s wound is jagged, deep, longer than 1 inch, or if it keeps bleeding for longer than 5 minutes; if your baby’s been bitten by an animal (or human); if the sore is contaminated with gravel or dirt; or if it’s a puncture wound from a nail or other rusty object, such as barbed wire. |
| Head injuries, concussion | Don’t let your baby climb on furniture. Use screw-mounted safety gates at the tops of staircases. Never leave your baby to nap or allow rough play in an adult bed, unless it’s a mattress on the floor. Exercise caution with children’s climbing equipment, especially if the surface underneath isn’t wellpadded. | Soothe the baby; examine the injury for cuts. | Monitor baby for signs of concussion (loss of consciousness, headache, dizziness, confusion, nausea, or vomiting). | If after a fall the baby loses consciousness, has more than one bout of vomiting, or is unusually sluggish, call your pediatrician or go to an emergency room. |
| Heatstroke | Keep your baby out of hot cars and direct sunlight, and undress her down to her diaper on hot days. Make sure her room is well-ventilated. If you don’t have air-conditioning, use small, out-of-reach fans in her room. Don’t overdress your baby in the winter, especially if she has a cold or fever. (Babies can’t “sweat out” a cold.) | Watch for the symptoms of overheating: hot, dry (or sometimes moist) skin, extremely high fever, possible convulsions, and loss of consciousness. | Be sure that your baby gets plenty of breastfeeding or formula during hot months. | Heatstroke can be fatal. Contact your baby’s doctor immediately, or take your baby to an emergency room if she has been exposed to extreme heat or overdressing and spikes a high fever or has a seizure. |
| Insect bites and stings | Keep your child away from areas where bees, wasps, hornets, or yellow jackets congregate, or when you are clearing ground. Note that insect repellants may be toxic to babies and young children. (Always read the label.) | Try to identify the insect. Most bite reactions are temporary and heal on their own. Remove the stinger from a bee with a scrape of your fingernail or a charge card. | Aloe vera gel from the plant can be soothing for minor bites. | Seek immediate medical attention if your child develops breathing problems or shows other signs of shock. |
| Mild burns from hot liquids or surfaces | Set your water heater to 120° F or cooler. Never drink hot beverages near your baby. Keep cups and bowls containing hot liquids and pots and appliances (irons, hair wands, coffeemakers) and cords away from counter and table edges. When there is a hot oven, keep your baby out of the kitchen with a gate or play yard. Shield heaters, woodstoves, and fireplace openings. | Your baby will scream and the burn will quickly turn red. Run cool water over the burn as quickly as possible to cool down the area. | Apply aloe vera gel or cream, but don’t put butter, ice, or other home remedies on the burn. They may actually make it worse. Your baby’s health-care provider may recommend an antibiotic ointment applied several times a day to keep mild burns from becoming infected. | Seek help immediately if your baby has suffered a serious burn, such as an electrical burn, a large burn over her body, or she stops breathing. Call your pediatrician if the burn begins to blister, looks chalky, covers a large area of skin, or is on the baby’s face, hands, feet, or genitals. |
| Snake bites | Keep your baby away from wood and mulch piles, rocks, the edges of streams, and other areas where snakes have been reported. | Try to identify the snake, but do not pursue it or try to capture it. Your child’s reaction, whether mild or severe, depends upon the snake and the amount of venom. Symptoms may include swelling at the wound site, shortness of breath, and shock. | Don’t try to suck the venom, apply a tourniquet, or cut the wound, which may only cause more tissue damage or introduce infection. | Seek immediate medical attention. |
| Splinters and embedded shards | Keep shoes on your toddling baby’s feet if there is rough wooden flooring inside, or if you are going outdoors. Don’t let your baby climb on woodpiles; keep wood furniture and windowsills sanded and stained. Clean up all glass splinters and safely dispose in a thick paper bag. Keep cacti well out of reach. | Wash your hands and the splinter area with warm, soapy water. Use tweezers and pull out the splinter at the same angle it went in. | Apply antibiotic ointment, and bandage the area. | Call the doctor if your child is in pain, or if you’re having trouble removing the splinter; if it is a deep puncture from a needle or toothpick; if the splinter is rusty metal, such as a nail; if it’s a fish hook with a barb; if it’s a pellet from a BB gun; if it is a shard of clear plastic or glass that’s hard to remove; or if it is a piece of imbedded pencil lead that could cause a permanent tattoo under the skin. (Note: Pencil “lead” is graphite and not lead, so it’s not toxic.) |
| Sunburn | Keep your baby out of direct sun entirely until 6 months of age, and then use babysafe sunscreens (30 SPF and above) on exposed skin when you’re going to be outdoors for more than a few minutes. | Apply aloe vera lotion and/or cool compresses of water and baking soda. | Give the baby plenty of fluids (breastmilk, formula, or, if your baby’s older than 6 months, water). | Call your pediatrician if your baby has a fever and/or blistered skin. |
| Ticks | Inspect pets that go outdoors daily for ticks during warm months, and give them tick-repellent medications. Look for ticks on your child after walks, and dress her in long pants tucked into socks to prevent ticks from jumping on her skin. | Ticks usually burrow next to the scalp or in warm places on the skin. Do NOT try to pull the tick off with your fingers. Grasp the head as close to the skin as possible with a pair of tweezers. Pull slowly and firmly. | Once the tick is removed, wash the wound with soap and water, then wipe it down with rubbing alcohol or hydrogen peroxide to disinfect it. Apply an antibiotic ointment and cover with an adhesive bandage. | Notify your baby’s doctor if the bite site becomes infected or develops a rash or red ring around it, which could signal Lyme disease. |
Dealing with an emergency
Tens of thousands of babies are rushed to emergency rooms in the United States each year as the result of accidents and severe illnesses. Emergency rooms can be chaotic, crowded (and sometimes unhealthy) places. They can also be downright frightening, especially when your vulnerable baby is concerned. With large hospitals located in major urban areas, you and your baby may end up spending long periods of time sitting with a lot of other people in an impersonal waiting room, being required to undergo a preadmission interview, and then sitting some more while you wait for your baby to be seen.
Ultimately you’re going to have to turn your baby over to the ER staff for treatment, and hopefully, she will get swift, kind, and careful care. Doing some advance footwork can help you to make rapid decisions about where to go for emergency care if you need to.
Here are our tips for making it through the experience:
• Check out your options in advance. We suggest investigating local hospitals and walk-in centers to weigh your options before your baby ever needs emergency care. Contact the ERs in your area to ask questions about the emergency services that are offered and how the admission procedure works. When emergency rooms are crowded, babies who show the symptoms of the flu or who are deemed to have less-than-life-threatening injuries may be diverted to a different treatment area in the hospital to make room for more serious cases. While you’re researching options, you may want to check on your hospital’s score from the Joint Commission on Accreditation of Healthcare Organizations (www.jcaho.org; 630-792-5800).
• Always keep a “loaded” cell phone in the car. Keep a cell phone with a car charger available in the car at all times so you will always have a device for summoning help. Load the phone with your pediatrician’s number, 911, the numbers of key relatives, the customer service number for your health insurance, and the hospital’s emergency number so you’ll have rapid access to whomever you need. Summon your baby’s pediatrician on the way to the hospital. He or she can give the hospital the heads up that you’re on the way and any details about your baby’s condition, and he may be able to meet you there. Knowing that your doctor’s on the way may improve the efficiency of your care.
• Create an emergency information packet for each person in your family. It should include your child’s full name, sex, Social Security number, a photocopy of the front and back of her health insurance card, a recent picture, her address, telephone number, date of birth, weight, height, blood type (if you know it), the name and telephone number of her doctor, a list of relatives to contact, a list of any medications she is taking (including vitamins), and a detailed description of any preexisting conditions she has. Fold the information into a self-sealing, transparent sandwich bag, write “IN CASE OF EMERGENCY” and your child’s name on it, and duct tape it onto the inside of your refrigerator door, where you or emergency personnel can grab it in a hurry (rescue squads are trained to always check inside the refrigerator door for medications and emergency information). That will save you having to divert your attention from your baby when rescue squad members require critical information before they transport your baby to a hospital.
• Plan backup support. Rehearse with your partner, your next of kin, and your neighbor about what you will do if you have a family emergency and you need someone to be with you at the hospital, and someone else to care for your children should something unexpected happen.
• Get preapproval from your health insurance company. If there’s time, contact your health insurance company on the way to the hospital or shortly after you arrive or ask a family member to do that for you. Most health insurance companies require immediate notification when a patient is receiving emergency medical care. Informing them may help to smooth out problems with billing and paperwork later.
• Consider summoning the rescue squad. If you deem your baby’s emergency to be serious, it may make more sense to have the rescue squad come to you rather than trying to drive your baby to the hospital yourself. That way, your baby will have professional care and attention all the way to the hospital and she will also get a more rapid response once she arrives there. Ambulance services are expensive, but the few minutes that it takes the rescue squad to arrive may make a huge difference in the speed and quality of intervention your baby receives.
• Be aggressive. You are your baby’s primary source for security, safety, and protection, so it’s important to be firm and insistent when it comes to going along with your baby rather than allowing the staff to whisk her away without you. Explain that you will remain quiet but that as your baby’s guardian, you must insist that you stay with her. If you are a breastfeeding mother, explain that your baby is being breastfed and you are her sole source for nourishment, which is another reason why you need to go along for the ride.
• Keep records. Keep a record of the staff members who treated your child in the emergency room in case your insurer needs further proof that your baby’s visit was warranted. Calling the insurer may help to reverse coverage if it was denied.
WARNING! Strangulation Dangers
Seventy-five percent of the 5,000 children who are treated in emergency rooms every year from airway obstruction from toys and toy parts are ages four and under, and nearly 100 babies die each year in crib-and bed-related accidents. If any toy can fit through the cardboard tube of a roll of toilet paper, it’s too small. If a can of soda can fit between the bars of a cradle, a crib, or a playpen; through the space between a headboard and a mattress; or between a guardrail and a mattress—then that space poses an entrapment danger for a baby. Among children of all ages, balloons are the most common cause of toy-related choking death. (For more information about choosing safe toys, see page 344 in 4. Gear Guide.)
• Ask for copies of your baby’s records. When you’re getting ready to check your baby out, ask for a copy of her X-rays and lab results. It’s much easier to take them as you are leaving than it is to ask the hospital for them weeks later. Having them in hand will help when you go for a follow-up appointment with your baby’s doctor.
Serious versus life-threatening situations
Some emergency situations can be dangerous, but not necessarily life threatening. For example, your toddler could fall and incur a head injury, have bleeding, or a severe illness—all of which are serious—but she most likely will survive.
In these situations, your baby will be breathing regularly and have a steady pulse (although it may be faster or slower than normal). She may be screaming or uncomfortable, but conscious, or able to be awakened from sleep. In this case, your first priority will be to call 911, or to take your baby to a hospital emergency room as quickly and calmly as possible.
An emergency is termed “life threatening” when a baby’s critical body functions, such as breathing or circulation, start to fail. When this happens, your baby might be in danger of dying, which requires an immediate response, even before you summon help. Some life-threatening accidents include: poisoning, drowning, electric shock, an obstructed airway, serious burns, and heavy bleeding from a wound.
An accident is “life endangering” when a baby is unconscious and her body is going into shock. The term “shock” refers to the way a body reacts when the blood supply to vital organs, including the brain, heart, liver, and kidneys has been threatened. It can be caused by significant loss of blood or bodily fluids, but it can also be the result of an allergic reaction to drugs or insect bites.
A baby in shock will have rapidly falling blood pressure and will seem to get progressively worse. Hypovolemic shock occurs when there is a rapid loss of blood or other body fluids. It can happen after any serious injury, a burn, or as the result of a bleeding wound. It can also be caused by severe dehydration when a baby isn’t getting enough fluids or is ill and vomits a lot, has prolonged diarrhea, or is suffering from heat exhaustion.
Clearing Airway Obstructions
If your baby is going into shock, she will appear pale; have cold, clammy skin; a rapid but weak pulse; shallow breathing; and she will seem extremely irritable and uncomfortable. Alternatively, she could be extremely sluggish and hard to wake up. Your baby may also have nausea and vomiting and appear extremely thirsty.
Airway obstruction
Airway obstruction is the leading cause of unintentional injury-related death among children under age one. It includes choking, suffocation, and strangulation, all of which prevent oxygen from entering the lungs and brain. Depriving the brain of oxygen for more than 4 minutes may cause lasting brain damage or death.
Here are the ways that babies die from airway obstruction and what you can do to protect your baby:
• Neck compression from entrapment. A baby’s throat is made of soft tissue and it can become compressed under the lid of a toy box or when the baby’s airway becomes compressed by the edge of a mattress because it doesn’t fit flush against the side a bassinet, crib, or play yard. A baby’s body can slip out through the leg hole of a stroller or under the tray of a highchair, leaving the head stuck behind. A baby’s neck can also be captured in the spaces between the guardrails and frames of toddler and adult-sized beds.
Prevention: Make sure the spaces between guardrails and bed frames, and between the headboards and footboards of beds, are less than 3.5 inches. Buy certified high chairs that have a center post to prevent “submarining” under the tray; close up the leg holes of full-sized strollers when they’re completely reclined, and remain in the same room when your baby is napping in one. Don’t use a toy box, or use one with a special, baby-safe hinge.
• Choking on swallowed objects. An object, such as a piece of a hot dog, a chunk of carrot, a nut or piece of hard candy, a small toy or marble, the mouthpiece of a pacifier, or a piece of rubber from a deflated balloon can become jammed in the baby’s throat, blocking her airway. Also, a baby may choke on her bottle because she is drinking without adult supervision.
Prevention: Keep foods, small objects and toys, and rubber balloons—all of which are choking hazards—away from children under age four. Cut chunky foods into small pieces. Inspect pacifiers for structural integrity. Follow manufacturers’ age guidelines for toy use. Don’t let your tot run, play, or walk with a bottle, sippy cup, or food in her mouth. Always hold your baby for bottle feedings and supervise other eating experiences.
• Suffocation. A soft surface—such as the vinyl covering of a beanbag chair, a waterbed mattress, or an indented couch cushion—can cover a baby’s nose and mouth, cutting off her air supply, and her neck and head muscles aren’t strong enough to allow her to change positions. Sixty percent of suffocations occur where babies sleep.
Prevention: Place your baby to sleep on her back on a firm, flat, crib mattress, in a crib that meets national safety standards. Keep pillows, comforters and quilts, soft toys, and other objects out of your baby’s crib.
FLASH FACT: Trauma and Children’s Deaths
These are the leading causes of children’s deaths from trauma (in order of frequency):
• Motor-vehicle accidents
• Drowning
• Fires/burns
• Suffocation and choking
• Firearms
• Falls
• Poisonings
• Life-threatening emergencies
• Strangulation. A baby can become entangled in the noose of a window-blind or drapery cord, or the cord tie on a hood. A piece of the baby’s clothing can get caught on a sliding board or other piece of play-yard equipment, her nightgown could catch on the protruding post of a crib, or her neck could get caught in a long string from a wall hanging.
Prevention: Remove drawstrings from the outerwear of clothing for young children. Tie up or cut all window-blind and drapery cords so there is no noose.
Severe bleeding
Your baby’s body doesn’t contain very much blood. A 25-pound toddler’s body holds only about a quart. Spurting or steady bleeding may indicate that an artery or a vein has been punctured. Blood from an artery that carries oxygenated blood from the heart to the rest of the body will be bright red in color. Blood that is being carried back to the heart by a vein will be dark, bluish-red. In a serious bleeding situation, your baby’s body and brain can be seriously compromised unless immediate action is taken. Here are the steps to take if your baby has been seriously injured and is bleeding:
• 911. Get someone else to make the emergency call while you stay with your baby. If emergency help is delayed, have someone else drive you to the emergency room while you stay close to the baby.
• Stop the bleeding. Use a piece of cloth or a shirt to apply steady pressure to the wound to stop the flow of blood. Put more cloth over the old pad when it becomes soaked, rather than changing dressings, since that might dislodge early clotting.
• Raise the wounded limb. If you’re sure that your baby’s spine has not been injured, raise the arm or leg above the heart to help slow down the loss of blood. (Your baby’s limbs may be limp and numb if there has been a spinal injury.)
• A tourniquet. A tourniquet is tying a bandage around the wound so tightly that blood flow is cut off. It is a dangerous and drastic measure because it cuts off the blood supply to the rest of the limb, which may cause the limb to die. A tourniquet should be applied only if a limb has been severed or death is imminent.
Once your child arrives at the hospital, she may require stitches (sutures) or surgery to repair the wound. You will be given instructions about what to do for you child once the bleeding has been stemmed and the wound dressed.
Emergency baby life support
Basic baby life support is designed to keep your baby alive and breathing until help comes. It is very rare for a baby to need emergency resuscitation, but it’s important to take a course in life support or CPR (cardiopulmonary resuscitation) through your local American Red Cross chapter or the American Heart Association. In the meantime, here are some basic instructions to rehearse:
1. Make sure your baby isn’t breathing or moving. Mucus, blood, vomit, a solid piece of food or candy, or the tongue can easily obstruct a baby’s small airways, causing her to become unconscious.
2. Shout for help.
3. Have a second person call 911.
4. If there’s been an accident, try to see how seriously your baby is injured and whether she is unconscious: Your baby will not respond to gentle motions or to tapping her feet.
5. If you suspect that your baby has a head or neck injury, don’t move her body, which could make the spinal cord vulnerable.
6. Look, listen, and feel your baby’s chest to see if she is breathing. If there is no one to help you, and your baby is obviously not breathing, or turning blue, perform CPR for one minute before calling for help. Remember, a baby’s lungs are tiny, and so are her air passages.
Just because a product appears to be designed for use by babies, there’s no guarantee it’s going to be safe. Every year baby products injure tens of thousands of babies seriously enough to require hospital emergency-room treatment. The three biggest causes of baby-product-related injuries are poor design, misuse, and product deterioration after use. (For information on how to buy safe baby products and toys, see in 4. Gear Guide.)
The competition among baby-product manufacturers is fierce. When an innovative product design makes a big profit in the marketplace, other manufacturers quickly follow with nearly identical clones. The only problem is that fatal flaws also get copied and mass-reproduced.
Over the decades, products that once might have appeared to be wonderful contraptions for babies have later been discovered to have serious, baby-threatening flaws.
Safety awareness
Sometimes parents misuse baby products by relying on them to serve as babysitters. Many babies have died when they were left alone in a device and got into trouble with no one to there to help them. They’ve fallen over in suctioned bathtub seats and drowned; gotten strangled in frame strollers when they were supposed to be napping; or strangled when their necks got captured on the partially collapsed side of a playpen while their parents were somewhere else in the house.
Parents often fail to follow manufacturers’ age and weight guidelines, unintentionally putting their babies at risk. A baby too big for her car seat could overload it, causing her to be injured or killed when the seat frame or straps fail to withstand crash pressures; a toy meant for an older child could have small parts that a baby could chew off and choke on; a curious toddler could open the battery compartment of a kid’s toy and choke.
All baby products eventually break down from the wear and tear that parents and babies give them. Wheels fall off of strollers, safety latches get bent and stop holding, seat belts fray, buckles break—and sometimes these product failures can be a life-threatening hazard for a baby. The worst offenders are old, malfunctioning cribs with missing bars or broken hardware. They are responsible for the deaths of nearly a hundred babies every year in the United States.
How to Do Baby CPR
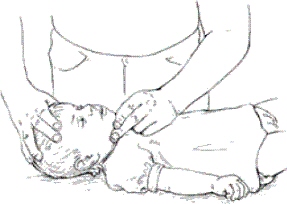
1. Place your baby on her back and try to open the airway by tilting her head back and lifting her chin.
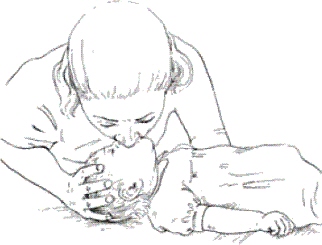
2. Place your mouth over the baby’s mouth and nose and give two slow, gentle breaths. If breathing doesn’t start, try 2 more slow breaths, 1 breath every 2 to 3 seconds with 1 to 1½ seconds per breath (about 20 breaths per minute). Pause in between to take air.

3. Check pulse (inner side of upper arm).
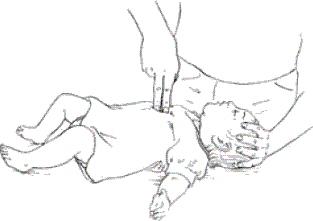
4. If your baby is still not breathing, and there are no signs of movement, place two fingers between her ribs on the lowest place on her chest (the sternum). Press down in cycles of 5 compressions followed by one slow breath in the baby’s mouth and nose with your mouth. Continue with 5 compressions and one slow breath until your baby revives or help arrives.
Seven ways to protect your baby from baby-product dangers
Here are our suggestions for how to protect your baby from getting hurt or killed by a baby product:
1. Shop carefully. Make sure the product is right for your baby. Check out the manufacturers’ recommended age and weight recommendations, and read all the warnings before you buy.
2. Follow the directions. There you’ll find the information that’s critical for your baby’s safety, and whom to contact when there’s a problem. Put all your baby-product receipts and literature in a single file so you can find them when you need them.
3. Mail the registration card. Even though it may make you a target for junk mail, it’s also the primary way that manufacturers locate customers who have bought bad products to inform them there’s been a recall.
4. Keep up with recalls. Periodically check the Web sites of the Consumer Product Safety Commission and other federal agencies that regulate baby products to see if you own recalled products. (See How to Do Baby CPR.)
5. Use straps. The seat straps in strollers, car seats, high chairs, booster seats, swings, and changing tables are there for an important reason: They protect babies from falling out or getting strangled. Use the straps every time you put your baby in one of these products.
6. Stay nearby. Stay in the same room if your baby is in a holding device, such as a stroller, high chair, play yard, car seat, or stroller. Feed your baby in your arms instead of using a bottle-propper, and always hold your baby during bathing instead of using a dangerous suctioned bath seat that could topple over and drown your baby in only a matter of minutes.
7. Keep baby away from product dangers. Keep your baby out of range when you’re installing, opening, closing, assembling, or doing other things with baby products. You can get distracted, and sharp corners, hinges, and edges could cause injuries.
The Leading Baby-Product Dangers
It’s easy to believe that baby products are safe. After all, they were made for babies, right? The real truth is that baby products harm tens of thousands of babies every year. Here’s a summary of how baby products hurt babies:
| PRODUCT CATEGORY | DANGERS | WHAT HAPPENS |
| Baby toys | Small parts, such as eyes, buttons, or wheels come loose; sharp points and edges injure; loose fur or hair gets chewed off; balloons pop and catch in the throat. | Small parts come loose and are swallowed and get stuck in babies’ throats, cutting off the air supply. Sharp points injure during falls. Fur and hair gets caught in the throat. Pieces of latex from popped balloons are inhaled and shut off the baby’s air supply. |
| Bedding and crib quilts | Puffy, soft surfaces on quilts, loose sheets, and stuffed crib toys. | Babies suffocate in soft surfaces when placed face downward or when their necks get wrapped up in loose sheets. |
| Buckets with water, and water-filled diaper pails | Toddlers drop a toy into the water and then reach down to try to retrieve it. | The baby’s heavy head causes her to fall in headfirst and drown. |
| Car seats | Parents fail to follow directions. They place seats in the front seat of the car in front of killer air bags; seats are installed incorrectly; children aren’t safely secured in the seat; or the child is put in the wrong seat for her weight. | Front seat air bags deploy during a crash, killing the small occupant in front. The seat isn’t fastened down, the baby isn’t correctly strapped into the seat, or the baby is too large for the seat, leading to serious injuries during a crash. |
| Cribs | Hardware bends and breaks. Bars work loose. Decorative posts capture baby’s clothing. | Babies’ vulnerable necks get caught in gaps between the mattress support and the crib, or between the bars when their bodies slide out. Clothing forms a noose and strangles. |
| Portable play yards | Sidebars don’t click into place when they’re set up, forming a loose, V shape. | Toddlers attempt to climb out and strangle when they get their necks captured in the V. |
| “Safety” gates | Accordion-style gates have X-shaped joints that work like scissors when they close. Other models have holes in center mesh panels used for climbing. Stoppers on the side of the gate fail to hold. | Babies get their hands or fingers crushed when the gate opens. Toddlers use holes in the gate panel to climb over and fall down stairs on the other side. Stoppers on pressure-mounted gates don’t hold, causing the gate to fall down stairs with the baby. |
| Strollers | Large leg holes or gaps in the frame allow the baby to slide out. Sharp hardware captures small hands and fingers, especially when the frame accidentally collapses. | Napping babies are left unattended. Strangulation occurs when the baby’s body slides through leg holes or out of gaps, leaving the head behind. Frames fail to lock in the open position, capturing children’s fingers and hands in sharp hinges. |
| Suctioned bath seats | Suction cups on the base of self-standing tub seats don’t hold. | Parents leave the baby unattended and the seat falls over, pressing the baby’s face into the water. The baby drowns within several minutes. |
| Wheeled walkers | These small seats on wheels move faster than parents anticipate. | Walkers tumble down open staircases, causing severe head trauma. They propel babies into hot stoves, fireplaces, and into outdoor swimming pools where they drown. |
Product Recall Reconnaissance
Federal agencies have the power to recall baby products that pose dangers, and literally millions of baby products have been banned, pulled off shelves, or undergone “corrective actions” that retrofit the unsafe parts of a product.
In spite of federal actions, product-related accidents and injuries continue to happen, killing hundreds of babies every year and rushing over 10,000 babies to emergency rooms for treatment. New products introduce new baby dangers into the marketplace; old and worn-out products fail; and, greedy importers ignore federal regulations by selling shoddy goods that fail federal standards.
Keep on top of recalls and report baby-product problems by frequently accessing these federal sites:
| AGENCY | WHAT IT DOES | CONTACT |
| U.S. Consumer Product Safety Commission (CPSC) | Regulates the safety of most baby products, clothing, bedding, and toys. (Carseat recalls generally come from the National Highway Traffic Safety Administration— see below.) |
4330 East West Highway Bethesda, MD 20814 Toll-free consumer hotline: 800-638-2772 Web site: www.cpsc.gov |
| National Highway Traffic Safety Administration (NHTSA) | Regulates and recalls children’s car seats and rates their installation instructions. |
400 Seventh Street, SW Washington, D.C. 20590 Toll-free Auto Safety Hotline: 888-327-4236 Web site: www.nhtsa.dot.gov |
| U.S. Food and Drug Administration (FDA) | Regulates baby food, medicines, and cosmetics, such as bathing products and diaper rash creams. |
5600 Fishers Lane Rockville, Maryland 20857-0001 General information number: 888-INFOFDA (888-463-6332) Web site: www.fda.gov |