

Anything that causes inflammation will, in turn, cause insulin resistance. And anything that causes insulin resistance will cause inflammation. This dangerous spiral is at the root of so many of our twenty-first-century chronic maladies.
Inflammation is something we are all familiar with—from a sore throat, an allergic reaction with hives, or a cut that gets infected and swollen, red, hot, and tender. But the inflammation that drives obesity and chronic disease is invisible and doesn’t hurt. It is a hidden, smoldering fire created by your immune system as it tries to fight off bad food (sugar, processed foods, inflammatory fats), stress, toxins, food allergens, an overgrowth of bad bugs in your gut, and even low-grade infections.
These triggers all cause an increase in the inflammatory molecules of your immune system called cytokines. They are important in fighting off infection and cancer, helping your body distinguish between friend and foe. But when inflammatory cytokines get out of control, chronic diseases of every stripe result.
One of the most significant medical discoveries of the twenty-first century is that inflammation is the common thread connecting not just the obvious autoimmune and allergic diseases but most chronic disease, including heart disease, obesity, diabetes, cancer, dementia, and depression. In fact, out-of-control inflammation causes insulin resistance, which, as we now know, is the main factor in all these diseases apart from autoimmunity and allergy. The insulin resistance then creates even more inflammation, and the whole biological house burns down.
Anything that triggers cytokines will make your cells more insulin-resistant, which will in turn make your pancreas pump out more insulin in order to get glucose inside your cells to burn for energy. But since your cells are resistant to the insulin, you require even more of it. Insulin resistance is a state of starving in the midst of plenty.
As we said earlier, insulin is a fat storage hormone that makes you eat more and gain more weight. We now know that fat cells (or adipocytes) also produce their very own highly inflammatory cytokines called adipocytokines (or adipokines for short).1 These adipokines (IL-1, IL-6, and tumor necrosis factor alpha) worsen insulin resistance, obesity, and diabetes, and inflame many other chronic diseases.
What triggers this inflammation? A number of recent studies have pointed to a few basic causes that we can identify and treat directly.
Sugar, refined carbohydrates, trans fats, too many inflammatory omega-6 fats from processed plant oils (such as soybean or corn oil), artificial sweeteners, hidden food allergies and sensitivities, chronic infections, imbalances in gut bacteria, environmental toxins, stress, and a sedentary lifestyle all promote inflammation. Of course, which of these factors is the source of inflammation for you is a key question, and the answer is different for everyone. You must locate all the sources of inflammation in your life and eliminate them if you want to overcome diabesity. The Blood Sugar Solution will help you do that.
Depression and obesity are two problems that often go together. That was true for J.P., an eighteen-year-old who came for help with fatigue, depression, anxiety, and a 27-pound weight gain. When he first saw me, he weighed 201 pounds. He had severe pre-diabetes and didn’t know it.
We found many clues in his story and on his tests that all pointed to inflammation driving his obesity and depression. He had canker sores (gluten problem2); cracking at the corners of his mouth (B vitamin deficiencies); acne on his face, chest, back, and shoulders (dairy or sugar intake and gut inflammation); and seasonal allergies. He also was cold and tired (thyroid problems), especially in the mornings. He had trouble falling asleep, and had been on Paxil for four years to treat his anxiety and depression. He had other telltale symptoms of inflammation and immune dysfunction, including itchy ears (allergies or fungus) and white spots on his nails (zinc deficiency).
He had horrible eating habits: no breakfast, fast food for lunch and dinner, and diet and regular sodas throughout the day. He hated seafood (omega-3 fat deficiency). He did, at least, exercise for 25 minutes a day on the treadmill and 1–2 times a week with a trainer. And he slept 10 hours a night.
His lab tests showed omega-3 fat,3 vitamin D,4,5,6 B6,7 and B128 deficiencies, all associated with pre-diabetes and depression. He had autoimmune thyroid antibodies with otherwise “normal” thyroid function.9 He also had high cholesterol, low HDL, and high triglycerides, all of which are classic for pre-diabetes. He had a normal blood sugar but a sky-high insulin level after a sugar drink (linked to acne,10 depression,11 weight gain, and carbohydrate cravings).
We also found antibodies to gluten (linked to fatigue, depression,12 hypothyroidism,13 and acne) and many other foods,14 indicating a “leaky gut” (see Chapter 11), which also causes diabesity.
By removing the food allergens from his diet, getting him on a whole-foods, low-sugar, and unprocessed diet, cleaning up his gut with antifungals and giving him a probiotic, supporting his thyroid function, and fixing his nutritional deficiencies, all his symptoms cleared up. We didn’t need to treat all his individual “diseases.” We helped his system get back in balance and his symptoms went away as a side effect of getting healthy. In the first two months he lost 20 pounds and his cravings stopped. He had many causes of inflammation and we had to address them all.
Mounting evidence underscores the critical role that inflammation plays in the development and continuation of diabesity. In fact, those who have a high C-reactive protein (a marker of systemic inflammation) blood level have a 1,700 percent increased probability of developing diabetes.15 In medicine, 20 or 30 percent increases are considered significant; a seventeenfold increase should be headline news.
The increased rate of chronic illness we see in our society is a direct outcome of increased rates of inflammation. There is no longer any debate about this in the world of medicine. The important questions are, “What’s causing the inflammation, and how do we treat it most effectively?”
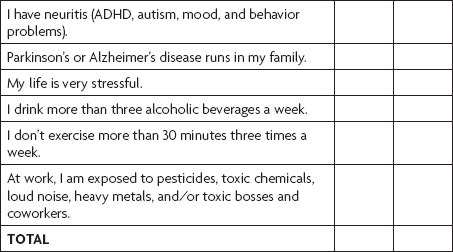
I can assure you the answer is not simply to take more aspirin or Advil. That’s like taking painkillers while a horse is standing on your foot. The treatment is getting the horse off your foot—and that means finding the underlying causes of inflammation and eliminating them. I will explain the primary causes in a moment, but first take the quiz below to find out how inflamed you are. Remember to take this quiz before you start the program and again after the six weeks are over to measure the “before and after” change in your health. You may need extra individualized support based on your scores; I explain this in Week 6 of the plan.
Hidden inflammation makes you fat and diabetic and causes many other chronic diseases including heart disease, cancer, and dementia. For any symptom you have experienced in the last month, place a check in the “Before” box. Then find out how severe your problem is by using the scoring key below. Place a check in the “After” box after you’ve completed the six-week program to see how much you’ve improved.
My guess is that most of you found you are inflamed. Let’s review the top seven causes of inflammation in our society. In Part IV, I will show you how to correct these problems.
Dietary sugars and refined flours are the biggest triggers of inflammation. They cause insulin levels to spike and start a cascade of biochemical reactions that turn on genes and lead to chronic and persistent inflammation. This begins a downward spiral into more inflammation, more insulin resistance, poorer blood sugar control, and more disease.
However, it is not just sugar, but also artificial sweeteners that drive inflammation, as we learned in Chapter 4. Diet drinks and artificial sweeteners of all stripes likely increase insulin resistance.
Lack of fiber, too many inflammatory omega-6 fats (soybean and corn oil), and not enough anti-inflammatory omega-3 fats (fish oil, flaxseeds) also contribute to the development of systemic inflammation, and that leads to worsening insulin resistance.
Food sensitivities and allergens also may play a role in the development of insulin resistance and diabesity. The allergies I am talking about here are not the typical hypersensitivity or acute allergies we are most familiar with, such as peanut or bee sting allergies. These are known as immediate-acting “IgE-mediated responses,” and while they can be deadly, they are not a major contributor to insulin resistance.
Delayed, or hidden, allergies (known as “IgG-mediated responses”) do, however, play a significant role. Some people suffer from allergic responses to inputs—like certain foods—which cause a broad array of subtle symptoms. These sensitivities don’t cause your throat to swell shut like IgE-mediated allergies do, but they do create systemic low-grade inflammation in the body that can manifest itself in any number of ways. Recent research indicates that these sensitivities may contribute to insulin resistance.
In fact, in a study that compared obese children to normal-weight children, the obese children had threefold higher levels of C-reactive protein and a two-and-a-half-fold higher level of IgG antibodies for the 277 different foods tested.16 In addition, these obese children had thicker carotid arteries, an indication of cholesterol-laden plaque lining the arteries and a strong predictor of heart disease and stroke. Plaque results from inflammation that starts in the gut but spreads throughout the body as food particles “leak” across a damaged gut barrier and trigger the production of cytokines such as IL-1, IL-6, and TNF (tumor necrosis factor) alpha.
This highly significant study points to the previously unrecognized connection between food allergies, weight gain, and insulin resistance. Diets eliminating common food sensitivities can help treat diabesity. For patients who have trouble losing weight, I often recommend a six-week elimination of dairy and gluten, the most common culprits, as a critical part of The Blood Sugar Solution. In fact, this is the single most important part of the program for many people, resulting in the greatest weight loss and reversal of diabesity.
In my practice, using IgG food sensitivities as a guide to treatment has been one of the most powerful interventions to treat and reverse a whole host of chronic ailments. In my book The UltraSimple Diet (www.bloodsugarsolution.com/ultrasimple-diet), I provide a comprehensive elimination diet to test for these hidden sensitivities. I have seen dramatic effects in weight loss, inflammatory conditions like autoimmune disease, and even mood and behavioral disorders (which I explain in my book The UltraMind Solution— www.bloodsugarsolution.com/ultramind-solution). But most physicians, especially allergists, do not accept or believe in these food reactions. That is unfortunate because there is solid evidence for the benefits of an elimination diet, including a remarkable study, published in one of the world’s most prestigious journals, the Lancet, showing that attention deficit hyperactivity disorder (ADHD) improved dramatically through an elimination diet based on IgG food-sensitivity testing.17 Interestingly, ADHD and childhood obesity often show up together and may be caused by similar factors.18
In medical school, we were trained to think that people with celiac disease were skinny kids with diarrhea, bloated bellies, and abdominal pain. Today we know differently; you can be fat, old, and constipated (or have no digestive symptoms) and still have celiac disease.
That was the case for Ron, who was a hefty 350 pounds when he came to see me. He was a weight loss expert, having tried every program from very low-calorie diets to no-carb diets to liquid diets. He could never maintain the weight loss.
He had many symptoms, including joint pain, a chronic cough, postnasal drip, and asthma, all of which were clues that inflammation might be driving his weight. He went from 180 pounds in high school to over 300 during graduate school. Cravings were his constant companion. He was a self-proclaimed carb addict. Exhausted all the time, he propped himself up with diet sodas and fast food. Since he was so big, he couldn’t sleep lying down and spent every night sleeping in a chair. He was a heavy snorer and likely had sleep apnea. His doctor put him on a statin and aspirin, but that didn’t make him feel better or address the underlying causes of his symptoms.
When we tested him, we found he had very high levels of inflammation with a C-reactive protein of 8.5 (normal is less than 1.0); his insulin was 183 after a sugar drink (normal is less than 25); and he had high uric acid and lots of dangerous small LDL particles (statins lower the total amount of LDL but don’t affect particle size or the quality of your cholesterol). All these indicated severe pre-diabetes. But most important, we found very high levels of anti-gliadin (AGA) and tissue transglutaminase (TTG) antibodies, which indicate an autoimmune reaction to gluten. He had celiac disease, which explained all his health problems, including obesity, pre-diabetes, asthma, joint pain, and fatigue.
Six weeks after being on a gluten-free diet, not only did he lose three notches on his belt, but his knees didn’t hurt, his asthma was gone, he wasn’t hungry, his energy was back, and he didn’t need a nap every day. And he could finally sleep in his bed. Anytime I see anyone with serious health problems, I always check for gluten sensitivity.
Gluten-free is hot these days. There are books and websites, restaurants with gluten-free menus, and grocery stores with hundreds of new gluten-free products on the shelves. Is this a fad, or a reflection of response to a real problem?
Sadly, chronic illness is increasingly caused by eating our beloved diet staple, bread, the staff of life, and all the wheat products hidden in everything from soups to vodka to salad dressing to lipstick to envelope adhesive. In a moment I will explain why gluten sensitivity and celiac disease have been increasing and now affect at least 20 million Americans. Unfortunately, 99 percent of the people who have problems with gluten or wheat are not currently diagnosed.
We know that gluten, a protein found in wheat, barley, rye, spelt, and oats, triggers obesity and diabetes in patients with gluten sensitivity all the way to full-blown celiac disease, an autoimmune disorder that triggers body-wide inflammation.
Ninety-eight percent of the people with celiac have a genetic predisposition (which occurs in 30 percent of the population). But even though our genes haven’t changed, we have seen a dramatic increase in celiac disease in the last 50 years, likely because of environmental triggers—namely, the hybridization of wheat grown in this country, which has changed the quality and type of proteins and starches in wheat, creating much higher gluten content. Our bread is not what it used to be. It is more of a Frankenfood, a by-product of industrial agriculture or “super-starch and super-gluten.” Combine that with the damage our guts have suffered from our diet, environment, lifestyle, and overuse of antibiotics, acid blockers, and anti-inflammatories, and you have the perfect storm for gluten intolerance.
In a study comparing blood samples taken 50 years ago from 10,000 young Air Force recruits to recent samples from 10,000 people, researchers found it remarkable that there has been a 400 percent increase in celiac disease over the last 50 years.19 And that’s just the full-blown disease, which affects about 1 in 100 people, or about 3 million Americans.
Gluten also causes inflammation through a low-grade autoimmune reaction. In other words, your immune system creates low-level antibodies to gluten but not full-blown celiac disease. In fact, 7 percent of the population (21 million) have these anti-gliadin antibodies. They have also been found in 18 percent of the people with autism and 20 percent of those with schizophrenia.
In a major study in the Journal of the American Medical Association, hidden gluten sensitivity was shown to increase risk of death by 35–75 percent, mostly by causing heart disease and cancer.20 By just this mechanism alone, more than 20 million Americans are at risk for heart attack, obesity, cancer, and death.
Most of the increased risk occurs when gluten damages the gut lining. All the bugs and partially digested food particles inside your intestine leak across the gut barrier and are exposed to your immune system, 60 percent of which lies right under the surface of the layer of cells lining your gut. Your immune system attacks these foreign proteins, and this leads to systemic inflammation.
There is also some striking new research showing that adverse immune reactions to gluten may result from problems in very different parts of the immune system than those implicated in celiac disease. Most doctors dismiss gluten sensitivity if you don’t have a diagnosis of celiac disease, but this new research proves them wrong. Celiac disease results when the body creates antibodies against the wheat (adaptive immunity), but another kind of gluten sensitivity results from a generalized activated immune system (innate immunity). This means that people can be gluten-sensitive without having celiac disease or gluten antibodies and still have inflammation and many other symptoms.21
Too many people, trying to eat healthy, are eating too much gluten-free junk food like cookies, cakes, and processed food. Just because a food is gluten-free doesn’t mean it’s healthy. Gluten-free cookies and cake are still cookies and cake! Vegetables, fruits, beans, nuts and seeds, and lean animal protein are all gluten-free—stick with those.
In the past, doctors would only diagnose celiac disease based on positive intestinal biopsy. But Dr. Alessio Fasano of the University of Maryland School of Medicine suggests a more inclusive way to diagnose celiac disease and gluten intolerance or sensitivity. He suggests that any four out of the five factors below are diagnostic.22 I would agree for full-blown celiac, but except for only a positive gene test, I think any of these factors warrants a trial of a strict 100 percent gluten elimination diet for six weeks.
And I believe if you have just three out of five criteria, you should be gluten-free for life.
You have symptoms of celiac (any digestive, allergic, autoimmune, or inflammatory disease including diabesity).
You get better on a gluten-free diet.
You have elevated antibodies to gluten (anti-gliadin [AGA] or tissue transglutaminase [TTG] antibodies).
You have a positive small intestinal biopsy.
You have the genes that predispose you to gluten sensitivity (HLA DQ2/8).
Chronic infections can also trigger inflammation. New studies show that infections such as adenovirus (the kind of virus that causes upper respiratory infections or infectious pinkeye) may be linked to obesity and insulin resistance.23 These can be identified and treated by experienced practitioners in functional medicine. You can also boost your immune system in order to suppress and control these latent infections.
To learn more about what tests to get in order to check for latent infections, see How to Work with Your Doctor to Get What You Need at www.bloodsugarsolution.com.
Toxins also play a large role in inflammation and can lead to diabesity. The increasing load of persistent organic pollutants (such as PCBs and pesticides) and heavy metals (such as arsenic, mercury, and lead) has been linked to both diabetes and insulin resistance.24 The link between toxins, inflammation, and diabesity25 will be discussed further in Chapter 12, “Step 5: Maximize Detoxification.”
Chronic stress is yet another cause of inflammation in the body.26 That’s one more reason for you to relax and learn how to calm your mind. I discussed this in the last chapter and we will go into greater detail about the impacts of stress in Chapter 14, “Step 7: Soothe Your Mind,” where I explain how chronic stress and the resultant high levels of cortisol increase insulin and weight gain around the middle.
It’s hard to imagine that doing nothing can make you inflamed, but that is exactly what happens. Lack of regular exercise creates low-grade inflammation in the body. And regular exercise dramatically reduces inflammation,27 which is why exercise is so critical to the reversal and treatment of diabesity.
Studies show that deficiencies in basic nutrients such as vitamin D, omega-3 fats, and antioxidants promote inflammation, and that simply taking a multivitamin and mineral supplement is as effective for lowering inflammation as taking a statin medication, with a lot less expense and fewer side effects.28 In Part IV, I will guide you in how to choose and take the best nutrients to correct inflammation and diabesity.
Locating and addressing each of the causes of inflammation in your life is essential not only for overcoming diabesity but also for addressing virtually every other health-related issue. There is no doubt about it: Inflammation is one of the common pathways to illness. Cooling off the fires is essential if you want to heal.