Ankle & hindfoot
Normal anatomy
Lateral view—bones and joints
The lateral and medial malleoli can be identified. Helpful hints to aid identification:
The posterior lip (or tubercle) of the tibia, conventionally and inaccurately referred to as the posterior malleolus, is well shown.
The calcaneum and its sustentaculum tali are demonstrated. Bohler's angle can be assessed for normality.
The base of the 5th metatarsal is often included.

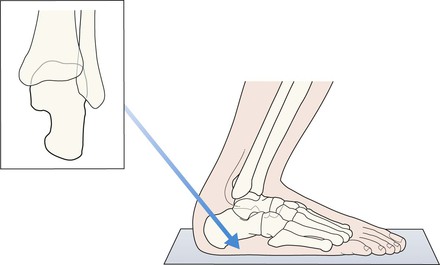
AP mortice
The mortice projection is obtained with slight (20°) internal rotation so that the fibula does not overlap the talus.
The joint space should be of uniform width all the way around. This space is well seen medially, it continues over the superior aspect of the dome of the talus, on to the lateral side of the joint.
The width of the joint space measures approximately 4 mm2.
The surface of the talar dome should be smooth, smooth, smooth. No irregularity, no notching, no defect.
The lateral process (also known as the lateral tubercle) of the talus is an important structure. The talocalcaneal ligament attaches to this part of the bone.
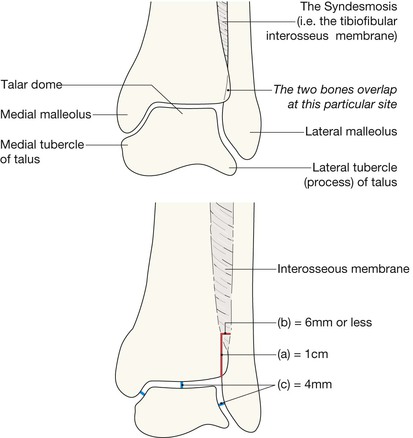
A useful rule: the bones of the tibia and fibula should always overlap on the mortice view. Any clear separation between these two bones should lead you to question whether the interosseous membrane is torn.
Analysis: the checklists1,3,4
AP mortice
Check the:
▪ Malleoli—fracture or … fractures?
▪ Tibiofibular interosseous membrane—any suggestion of a rupture?
□ If normal, the tibia and fibula should show some degree of overlap.
□ A measurement: the width of the space between the distal tibia and fibula at a point 1.0 cm proximal to the tibial articular surface should not exceed 6 mm5.
□ Medial and lateral processes (ie the tubercles, p. 268)—any fragmentation?
▪ Joint width—does any part exceed the normal 4 mm3?
▪ Epiphyses and growth plates in children—normal? (see pp. 15 and 280).
Common fractures/torn ligaments
The malleoli3,6
▪ Most ankle fractures involve one or both malleoli. These fractures are often easy to diagnose because you will know precisely which bones are tender.
▪ The direction of the applied forces will determine the particular fracture (or fractures) and any associated ligamentous damage:
Base of the 5th metatarsal
An avulsion fracture. This common injury results from avulsion of the metatarsal tuberosity at the insertion of the peroneus brevis tendon. The fracture occurs as a consequence of forced inversion.
The calcaneum
The calcaneum is the most commonly injured bone of the hindfoot. Types of calcaneal fracture are shown on pp. 278–279. See also infrequent calcaneal injuries on p. 288.
Growth plate (Salter–Harris) fractures
▪ Relatively common in children. A distal growth plate injury of the tibia is second in frequency to an injury of the distal growth plate of the radius.
▪ Growth plate fractures are described in detail on pp. 14–17.
▪ The most common growth plate fractures (types 1–4) are shown below.
Ligamentous injuries
Torn medial or lateral ligaments
If there is widening of one side of the mortice joint space then there is commonly an associated fracture elsewhere. Suspect widening if the joint space is wider than 4 mm medially or laterally3. Caution: the radiographs may appear normal even when there is severe ligamentous damage. Sometimes stress views will be required.
Tear of the interosseous membrane
This injury is very easy to overlook1,5,9,10. The AP radiograph will often provide evidence of a tear/rupture. Look for widening of the space between the distal tibia and the fibula. A useful rule of thumb: suspect a tear of the tough tibiofibular syndesmosis whenever the distal tibia and fibula do not overlap slightly on the AP mortice view.
Also … apply the 6 mm rule (see p. 270).
Infrequent but important injuries
Fractures of the talus
Talar fractures are rare. Many result from a high energy injury, often a road traffic accident or a fall from a height.
Neck of the talus4,11
An important injury because of the high risk of subsequent avascular necrosis (AVN) and secondary degenerative arthritis. AVN is caused by disruption of the blood supply to the body of the talus. Displacement of the fracture increases the probability of AVN. A displaced fracture is easy to detect. An undisplaced fracture is easy to overlook.
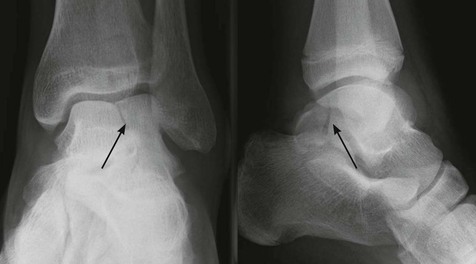
Talar dome–osteochondral fracture
A small but clinically important impaction fracture, usually consequent on an inversion injury1,12. The term osteochondritis dissecans was used in early descriptions of this lesion when it was assumed that the pathology was a spontaneous necrosis of bone in the dome of the talus. It is now generally accepted that most of these lesions are actually osteochondral fractures resulting from trauma.
In many cases the talar lesion is not an acute injury but has resulted from an earlier shearing or compression force.
Maisonneuve fracture
The ankle joint is in effect a bone ring and this particular ring extends as high as the knee because of the strong tibiofibular interosseous membrane. On occasion an external rotation injury of the ankle may cause an ankle injury but in addition the forces/energy acting within the interosseous membrane (the tibiofibular syndesmosis) may extend to the upper leg and cause a fracture of the proximal fibula13. The high fibular fracture may be overlooked because the main symptoms are around the ankle joint.
This combination injury is known as a Maisonneuve fracture. Suspect this injury whenever clinical examination of the upper leg is painful.
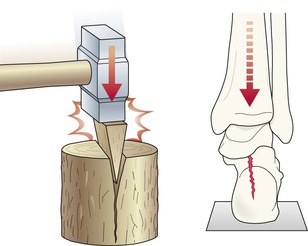
Distal tibial fractures involving the articular surface
These fractures are rare, accounting for less than 1% of fractures of the lower limb14.
The usual cause: a high energy fall or RTA producing a compression fracture, often with comminution. Compression fractures of the tibia are rare because it is usually the calcaneum that received and accepts the major vertical force and is fractured.
Complex Salter–Harris fractures
These two fractures are rare but need to be recognised early, as accurate reduction is essential in order to ensure normal growth and to avoid subsequent ankle deformity.
Triplane fracture3,15,16
This Salter–Harris type 4 fracture is a complex multi-directional fracture of the tibial epiphysis. It is a three plane fracture. As follows:
▪ Sagittal plane: vertical fracture through the epiphysis.
▪ Horizontal plane: transverse fracture through the growth plate.
Always suspect this complex fracture whenever the AP view shows a vertical fracture through the tibial epiphysis. Suspicion necessitates CT for full evaluation.
Pitfall: the full extent of the injury is often not evident on plain radiography.
Tillaux fracture3,16
This Salter–Harris type 3 fracture is an avulsion fracture through the tibial epiphysis. The fracture involves a partially closed epiphysis (age 11–15 years). It occurs in adolescents in whom the medial part of the growth plate has fused, but the normal fusion has not yet reached the lateral aspect. It is a two plane fracture. As follows:
▪ Vertical plane: through the epiphysis.
▪ Horizontal plane: through the lateral part of the growth plate.
Pitfall. This fracture can sometimes be confused with a Triplane fracture on plain radiography. CT will distinguish.
Talar dislocations—Infrequent but important
The subtalar joint has two parts and either part can dislocate as a result of a high energy force.
Pitfalls
Calcaneum: the apophysis
Normal accessory ossicles
Small bones lying adjacent to the tips of the medial and lateral malleoli are very common. They may be misread as avulsed fracture fragments. Occasionally an ossicle will be difficult to distinguish from a fracture and clinical correlation is important. Fractures are tender, accessory ossicles are not. Also:
▪ An accessory ossicle has a well defined (ie corticated) outline.
▪ An acute fracture fragment is ill defined (ie not corticated) on one of its sides.