

NAME |
PAGE |
735 |
|
736 |
|
738 |
|
740 |
|
744 |
|
746 |
|
748 |
|
749 |
|
750 |
|
752 |
|
754 |
|
756 |
|
758 |
|
759 |
|
760 |
|
762 |
|
764 |
|
766 |
|
768 |
|
770 |
|
772 |
|
774 |
|
776 |
|
778 |
|
780 |
|
782 |
|
784 |
|
786 |
|
788 |
|
790 |
|
792 |
|
794 |
|
796 |
|
798 |
|
800 |
|
802 |
|
804 |

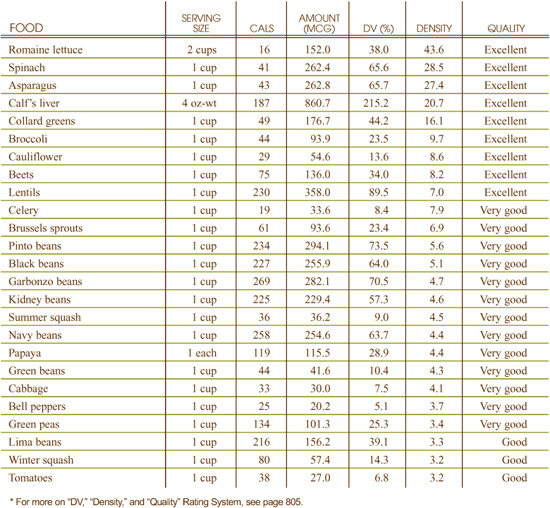
What makes the World’s Healthiest Foods so full of health-promoting potential is that they are nutrient-rich. What is so essential about these nutrients is that they are needed to sustain our body. An inadequate intake of these nutrients can cause a reduction in our physiological function, leading to poor health since the body doesn’t have what it needs to work properly.
We must therefore rely upon our food to provide us with these important nutrients. The more our foods concentrate these nutrients, the better they are because they can give our body an abundance of what it needs to achieve optimal health. This is why nutrient-rich foods—the World’s Healthiest Foods—form the foundation of our health.
The World’s Healthiest Foods provides an abundance of the wide variety of nutrients you need for optimal function. It is important to remember that these nutrients do not work alone but in concert (synergistically) with other nutrients. Some set the stage for the activity of others or work in unison with them, while some neutralize or balance the effects of others. This is why study after study has shown that diets containing nutrient-rich foods, like the World’s Healthiest Foods, are associated with better health.
The section on Health-Promoting Nutrients will give you detailed information about the function of an array of important nutrients and a list of the World’s Healthiest Foods that provides the best sources of these nutrients. It will provide you with a variety of information on over 30 nutrients and why we need to include foods rich in each nutrient in our “Healthiest Way of Eating.” It features the following information for each nutrient: the richest food sources of the nutrient; the nutrient’s function; the impact that cooking, storage and processing has on it; public health recommendations; how it promotes health; the causes and symptoms of deficiency; and, whether you need to be concerned about consuming too much of it.
Each chapter includes a Health-Promoting Nutrient chart for that particular nutrient. These charts can serve as valuable tools for helping you to make decisions as to which foods can help you to meet your personal health and nutrition needs. Whether you want to increase your calcium intake to help reduce your risk of osteoporosis or increase your folic acid intake to reduce your risk of cardiovascular disease, these charts will be helpful to you. If you’re looking to jump start your protective defenses during the winter season by consuming more vitamin C-rich foods or find easy ways to increase your content of dietary fiber, you can use the Health-Promoting Nutrient charts to see which foods are excellent, very good and good sources of the nutrient of interest.
Note: If you want help determining your nutritional status and information regarding health-promoting nutrients, which ones may be deficient in your diet, and which foods will help fulfill your nutritional needs, I suggest you go to the home page of the www.whfoods.org website and click on the Food Advisor. The Food Advisor is an interactive program that cannot be replicated in this book. Many thousands of people have been helped by this short, unique questionnaire. It only takes a few minutes to be on your way to vibrant health.
ANTIOXIDANTS ARE DIETARY COMPOUNDS—such as vitamins, minerals, amino acids and phytonutrients—that directly bind to and destroy damaging free radicals. As metabolites of oxidation reactions, free radicals can negatively impact the structure and function of the body in various ways, including: damaging our DNA (see page 75) and causing mutations, which may lead to cancer; oxidizing LDL cholesterol, which is the initiating step in the progression of atherosclerosis; and causing joint damage that can lead to arthritis. As research continues to support the role that free radicals play in the progression of both chronic diseases and other signs of aging, such as the loss of skin elasticity and cognitive function, antioxidants are gaining an ever more important place in health-promoting diets.
Many people are familiar with the vitamins and minerals that are renowned for their antioxidant activity. The ACE vitamins—vitamins A, C and E—as well as the minerals selenium, zinc, copper and manganese are just some of the traditional nutrients that are important when it comes to fighting the damage caused by free radicals. These nutrient antioxidants do not work alone but rather in synergy, each depending upon others to help support its optimal function. Their synergistic relationship is one of the reasons that it is so important to not focus on single nutrient intake, but on intake of an array of nutrients, as offered in the World’s Healthiest Foods.
In the past few years, there have been great contributions made to the arena of antioxidant nutrients, with researchers discovering special compounds in plants—known as phytonutrients—that have potent antioxidant potential. Their discovery of the wide array of phytonutrients, and the fact that so many of them have impressive abilities to prevent oxidative damage, has led researchers to suggest that the presence of these antioxidant phytonutrients may be one of the important reasons why diets rich in vegetables, fruits and other plant-based foods are consistently linked to promoting health and reducing risk of disease.
The wide spectrum of phytonutrients offered by plant-based foods such as fruits, vegetables, whole grains and legumes further supports the fact that these foods can make important contributions to our health. Some researchers estimate up to 40,000 phytonutrients will someday be fully catalogued and understood.
Plants are so rich in antioxidant phytonutrients for a reason: they provide plants with protection from the environmental challenges they face, such as damage from ultraviolet light, toxins, and pollution; when we consume plants rich in phytonutrients, they appear to provide humans with protection as well. Investigating the ways in which phytonutrients provide this protection is one of the most exciting areas in nutrition research today, and recent findings are providing science-based explanations as to how plant foods support our health and wellness.
Some of the major classes of phytonutrients that have antioxidant function include:
• Terpenoids: These include the basic terpenoids like limonene found in citrus foods and menthol, as well as the carotenoids (for more on Carotenoids, see page 740).
• Flavonoids: Flavonoids are the plant pigments that give plants their color. Flavonoids include the anthocyanins in blueberries and quercetin found in onions (for more on Flavonoids, see page 754).
• Isoflavonoids and lignans: Examples include genistein and daidzein found in soy foods, and the lignans in flaxseed and rye.
• Organic acids: Examples include ferulic acid, which is found in whole grains, and the coumarins, which are found in parsley and citrus fruits.
Since many phytonutrients are also responsible for the deep pigments that color our food, one way to look for foods rich in antioxidants is to choose foods that feature a palette of colors. For example, red signals lycopene; yellow/orange, betacarotene and beta-cryptoxanthin; blue/purple, anthocyanins; and green, chlorophyll. Enjoying a spectrum of different colored foods will allow you to enjoy the benefits of a spectrum of antioxidants.
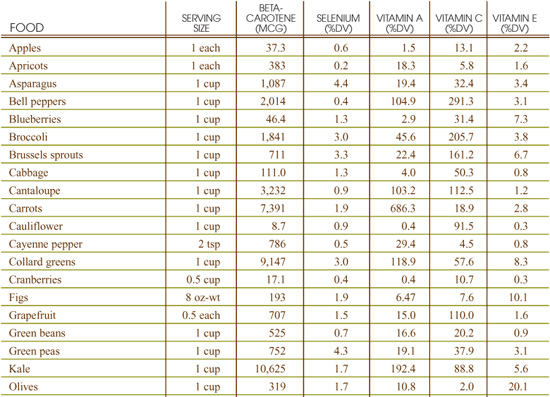
To find foods rich in antioxidants, you can also use the nutrient chapters featured in this section. Look at the chapters for antioxidants such as vitamins A, C, and E, the antioxidant minerals, and carotenoids and flavonoids, and you will find charts that detail the World’s Healthiest Foods that are the richest in those nutrients. In addition, I have also created a chart, located on page 804, which compiles the values of several antioxidant nutrients for some of World’s Healthiest Foods. While this is not an all-inclusive chart, it can give you an idea of the measurement of some antioxidant nutrients in some of your favorite foods.
With the growing interest in antioxidants, researchers are developing ways to measure the overall antioxidant capacity of foods. Instead of measuring specific nutrients, they measure just how powerful different foods (and their compendium of nutrients) are at exerting antioxidant activity. One of the most well known is ORAC, which stands for Oxygen Radical Absorbance Capacity. While ORAC values have oftentimes been cited as a measurement of a food’s inherent antioxidant potential, there are still very few studies published in Medline that review its use. Since I strongly believe that a food’s antioxidant value is not linked to just one nutrient, but a compendium of its entire matrix, I look forward to more research on ORAC and other measurements of total antioxidant potential of food.
Best World’s Healthiest Food Sources of Antioxidants
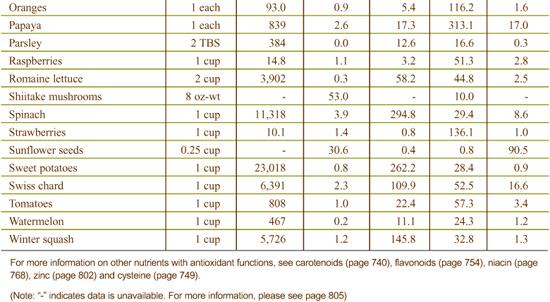
Best Sources of Biotin from the World’s Healthiest Foods
What can biotin-rich foods do for you?
• Support healthy skin through proper fat production
• Help your body make efficient use of sugar
• Maintain an energy supply in your nerve cells
What events can indicate a need for more biotin-rich foods?
• Depression
• Nervousness
• Memory problems
• Red or sore tongue
• Tingling or numbness in feet
• Heart palpitations
Biotin is relatively stable when exposed to heat, light, and oxygen. Strongly acidic conditions, however, can denature this vitamin. In raw eggs, biotin is typically bound to a sugar-protein molecule (the glycoprotein called avidin), and cannot be absorbed into the body unless the egg is cooked, allowing the biotin to separate from the avidin protein.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for biotin. The recommendations are as follows:
• 0–6 months: 5 mcg
• 6–12 months: 6 mcg
• 1–3 years: 8 mcg
• 4–8 years: 12 mcg
• 9–13 years: 20 mcg
• 14–18 years: 25 mcg
• 19 years and older: 30 mcg
• Pregnant females of any age: 30 mcg
• Lactating females of any age: 35 mcg
The FDA has set the Reference Value for Nutrition Labeling for biotin at 300 mcg. This is the recommended intake value used by the FDA to calculate the %Daily Value for biotin that may appear on food labels.
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for biotin.
Biotin plays an integral role in the metabolism of fats, sugars and amino acids. While bacteria in our digestive tract appear capable of making biotin, the extent and dependability of this process is still a matter of debate. For this reason, it’s very important for us to get biotin from our food.
Biotin was discovered in the late 1930s and early 1940s and was originally referred to as “vitamin H.” Egg yolks are one of the richest sources of biotin in the diet, but it is important to not eat whole eggs raw if you want to maximize your biotin consumption. That’s because raw egg whites contain avidin, a sugar and protein-containing molecule that binds together with biotin and prevents its absorption.
Many foods that concentrate biotin also feature vitamin B5 (pantothenic acid), a nutrient that participates in many of the same chemical reactions as biotin.
Biotin is involved in the metabolism of both sugar and fat. In sugar metabolism, biotin helps move sugar from its initial stages of processing to its conversion into usable chemical energy. For this reason, muscle cramps and pains related to physical exertion, which may be the result of the body’s inability to use sugar efficiently as fuel, may signal a biotin deficiency.
Many of the classic biotin deficiency symptoms involve skin-related problems, and the role of biotin in fat synthesis is often cited as a reason for this biotin-skin link. Biotin is required for the function of an enzyme in the body called acetyl Co-A car-boxylase. This enzyme puts together the building blocks for the production of fat in the body. Fat production is critical for all cells in the body since their membranes must contain the correct fat components in order to function properly.
Fat production is especially critical for skin cells since they die and must be replaced very rapidly, and also because they are in contact with the outside environment and must serve as a protective barrier. When cellular fat components cannot be made properly due to biotin deficiency, skin cells are among the first cells to develop problems. In infants, the most common biotin-deficiency symptom is cradle cap—a skin condition in which crusty yellowish/whitish patches appear around the infant’s scalp, head, eyebrows and the skin behind the ears. In adults, the equivalent skin condition is called seborrheic dermatitis, which is not limited to areas around the scalp but can occur in many different locations on the skin.
Because glucose and fat are used for energy within the nervous system, biotin also functions as a supportive vitamin in this area. Numerous nerve-related symptoms have been linked to biotin deficiency. These symptoms include seizures, lack of muscle coordination (ataxia), and lack of good muscle tone (hypotonia).
In addition to lack of biotin-containing foods in the diet, deficient dietary intake of pantothenic acid (vitamin B5) can contribute to a functional biotin deficiency since B5 works together with biotin in many metabolic situations.
Intestinal problems should also be considered as a possible reason for biotin deficiency. Under appropriate circumstances, bacteria in the large intestine can produce biotin, but when intestinal problems create bacterial imbalance, the body is deprived of this alternative source. Consumption of raw egg whites can also contribute to a deficiency since they contain the glycoprotein avidin, which can bind to biotin, preventing its absorption.
Additionally, as many as 50% of pregnant women may be deficient in biotin, a deficiency that may increase the risk of birth defects. Preliminary research has found laboratory evidence of biotin deficiency both in the early (first trimester) and late (third trimester) stages of pregnancy.
Skin-related problems, including cradle cap in infants and seborrheic dermatitis in adults, are the most common biotin deficiency-related symptoms. Hair loss can also be symptomatic of biotin deficiency.
Nervous system-related problems, such as seizures, ataxia, and hypotonia, provide the second most common set of biotin deficiency related symptoms. Additionally, muscle cramps and pains related to physical exertion can be symptomatic of a deficiency, reflecting the body’s inability to use sugar efficiently as a fuel.
Reports of biotin toxicity have not surfaced in the research literature, despite the use of biotin over extended periods of time in dietary supplement doses as high as 60 milligrams (one milligram equals 1,000 micrograms) per day. For this reason, in its 1998 recommendations for intake of B-complex vitamins, the Institute of Medicine chose not to set a Tolerable Upper Intake Level (UL) for biotin.
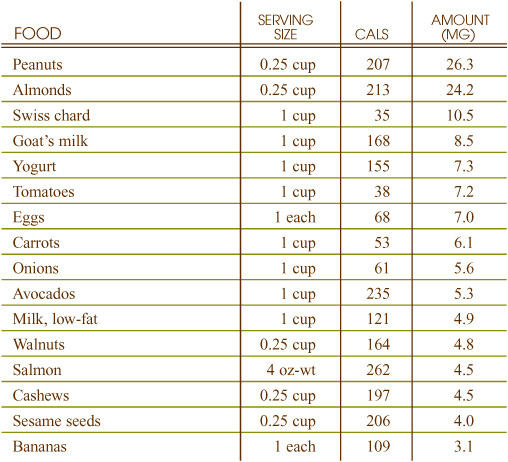
Best Sources of Calcium from the World’s Healthiest Foods
What can calcium-rich foods do for you?
• Maintain healthy, strong bones
• Support proper functioning of nerves and muscles
• Help your blood to clot
What events can indicate a need for more calcium-rich foods?
• Osteopenia (bone-thinning)
• Frequent bone fractures
• Muscle pain or spasms
• Tingling or numbness in your hands or feet
• Bone deformities and growth retardation in children
The amount of calcium in foods is not adversely impacted by cooking or long-term storage.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for calcium. The recommendations are as follows:
• 0–6 months: 210 mg
• 6–12 months: 270 mg
• 1–3 years: 500 mg
• 4–8 years: 800 mg
• 9–18 years: 1,300 mg
• 14–18 years: 1,300 mg
• 19–30 years: 1,000 mg
• 31–50 years: 1,000 mg
• 51+ years: 1,200 mg
• Postmenopausal women not taking hormone replacement therapy: 1,500 mg
• Pregnant and lactating women, younger than 18 years: 1,300 mg
• Pregnant and lactating women, older than 19 years: 1,000 mg
The FDA has set the Reference Value for Nutrition Labeling for calcium at 1,000 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for calcium that may appear on food labels.
The Institute of Medicine established the Tolerable Upper Intake Level (UL) for calcium at 2,500 mg.
Minerals, like calcium, cannot be made in the body, and therefore must be attained through the foods that we eat. Calcium is one of the most abundant minerals in the human body, accounting for approximately 1.5% of total body weight. While calcium has a lot of important functions, one of its most notable is to promote bone health and prevent osteoporosis. In fact, a calcium-deficient diet is one of the factors that has been linked to the development of osteoporosis.
Other nutrients—such as magnesium, phosphorus, and the trace minerals zinc, copper and boron—also play an important role in enhancing bone density and appear in many calcium-rich foods. Therefore, gaining calcium through your diet will not only provide you with a natural source of this important nutrient, but also of others that act synergistically to promote your health. Although dairy foods have been traditionally promoted as a concentrated source of calcium, many green vegetables provide more calcium per calorie than do milk or milk products.
Getting enough calcium from your diet is specifically important in these modern times when many people’s diets are filled with calcium-depleting factors. For example, sodium, caffeine, the phosphates in carbonated beverages, and excessive consumption of protein can cause an increase in calcium excretion.
Calcium is best known for its role in maintaining the strength and density of bones. In a process known as bone mineralization, calcium and phosphorus join to form calcium phosphate, a major component of the mineral complex hydroxyapatite that gives structure and strength to bones. If dietary calcium intake is too low to maintain normal blood levels to satisfy calcium’s other important functions, the body will draw on calcium stores in the bones to maintain normal blood concentrations, which, after many years, can lead to osteoporosis.
Calcium also plays a role in many other physiological activities including blood clotting, nerve conduction, muscle contraction, regulation of enzyme activity, and cell membrane function.
In addition to insufficient calcium intake, there are other factors that can cause calcium deficiency.
Lack of stomach acid impairs the absorption of calcium and may lead to poor calcium status. Hypochlorhydria, a condition characterized by insufficient secretion of stomach acid, affects many people and is especially common in older individuals.
Adequate intake of vitamin D is necessary for the absorption and utilization of calcium. As a result, vitamin D deficiency, or impaired conversion of the inactive to the active form of vitamin D (which takes place in the liver and kidneys), may also lead to a poor calcium status.
In children, calcium deficiency can cause improper bone mineralization, which leads to rickets, a condition characterized by bone deformities and growth retardation. In adults, calcium deficiency may result in osteomalacia, or “softening of the bone.” Calcium deficiency, along with other contributing factors, can also result in osteoporosis.
Low levels of calcium in the blood (especially one particular form of calcium, called free ionized calcium) may cause a condition called tetany, in which nerve activity becomes excessive. Symptoms of tetany include muscle pain and spasms, as well as tingling and/or numbness in the hands and feet.
Excessive intakes of calcium (more than 3,000 mg per day) may result in elevated blood calcium levels, a condition known as hypercalcemia. If blood levels of phosphorus are low at the same time as calcium levels are high, hypercalcemia can lead to the calcification of soft tissue. This condition involves the unwanted accumulation of calcium in cells other than bone. These negative impacts of excessively high calcium intake prompted the Institute of Medicine to establish a Tolerable Upper Intake Level (UL) of 2,500 milligrams for intake of calcium through either food and/or dietary supplements.
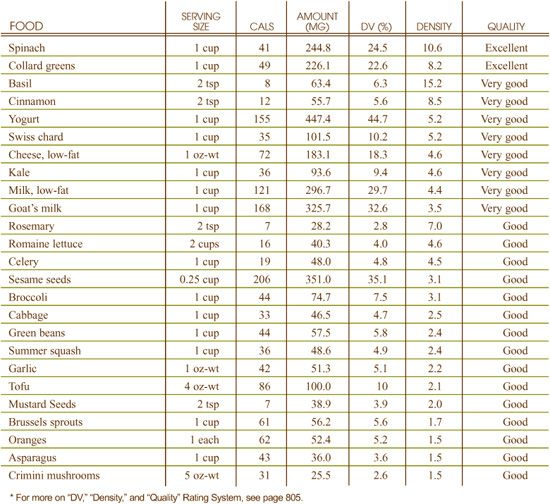
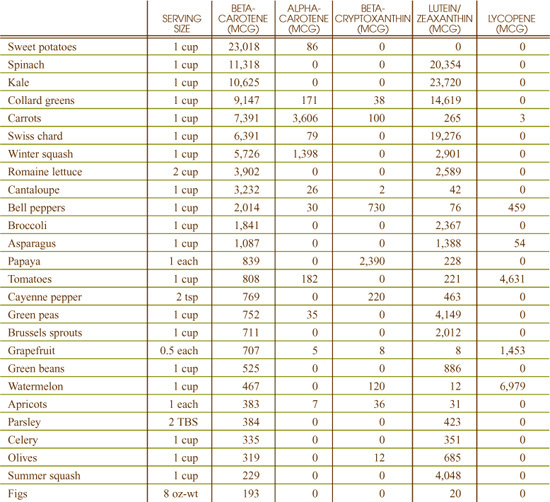
Best Sources of Carotenoids from the World’s Healthiest Foods (betacarotene, alpha-carotene, beta-cryptoxanthin, lutein/zeaxanthin, lycopene)
What can carotenoid-rich foods do for you?
• Protect your cells from the damaging effects of free radicals
• Provide a source of vitamin A
• Enhance the functioning of your immune system
• Promote eye health
• Promote lung health
What events can indicate a need for more carotenoid-rich foods?
• Low intake of fruits and vegetables
• Smoking
• Regular alcohol consumption
In certain cases, cooking can improve the availability of alpha- and betacarotene in foods. Lightly steaming carrots and spinach improves your body’s ability to absorb carotenoids in these foods. It is important to note, however, that in most cases, prolonged cooking of vegetables decreases the availability of these carotenoids by changing the shape of the carotenoid from its natural trans-configuration to a cis-configuration. For example, fresh carrots contain 100% all-trans betacarotene, while canned carrots contain only 73% all-trans betacarotene.
Lutein appears to be sensitive to cooking and storage. Prolonged cooking of green, leafy vegetables is suggested to reduce their lutein content. Additionally, the lutein content of wheat seeds has been found to decline with longer storage times.
Vine-ripened tomatoes have a higher lycopene content than tomatoes ripened off the vine. Although not all scientists agree, it is generally accepted that the availability of lycopene from tomato products is increased when these foods are processed at high temperatures or packaged with oil. If actually true, this means that your body absorbs the lycopene in canned, pasteurized tomato juice and tomato products that contain oil more easily than the lycopene found in a fresh, raw tomato.
While it appears that more research is necessary in this area, a recent study that explored the interrelationship of carotenoid (alpha-carotene, betacarotene and lycopene) absorption with dietary fat consumption seems to be supportive of the oil-carotenoid connection. This study found that the absorption of carotenoids from salad vegetables such as spinach, romaine lettuce, cherry tomatoes, and carrots was much greater with a full-fat dressing than a reduced-fat dressing. This interrelationship makes sense since carotenoids are fat-soluble compounds.
There is minimal research specifically focusing upon the effects of cooking, storage or processing upon beta-cryptox-anthin and zeaxanthin.
In an effort to set public health recommendations, the Institute of Medicine at the National Academy of Sciences reviewed the existing scientific research on carotenoids in 2000. Despite the large body of population-based research that links high consumption of carotenoid-containing foods with a reduced risk of several chronic diseases, the Institute of Medicine concluded that this evidence was not strong enough to support a required carotenoid intake level because it is not yet known if the health benefits associated with carotenoid-containing foods are due to the carotenoids or to some other substance in the food. Therefore, to date, no recommended dietary intake levels have been established for carotenoids.
However, the National Academy of Sciences does support the recommendations of various health agencies, which encourage individuals to consume five or more servings of carotenoid-rich fruits and vegetables every day.
Carotenoids are a phytonutrient family that represents one of the most widespread groups of naturally occurring plant pigments. Alpha-carotene, betacarotene, beta-cryptoxanthin, lutein/zeaxanthin and lycopene are among the most abundant carotenoids in the North American diet.
Alpha-carotene, betacarotene and beta-cryptoxanthin are considered “pro-vitamin A” compounds since they can be converted in the body into retinol, the active form of vitamin A. Among these, betacarotene has the greatest vitamin A activity with the other two having about half that of betacarotene.
Lutein/zeaxanthin and lycopene do share an important characteristic with these “provitamin A” carotenoids—they all have very impressive antioxidant activity. (Although separate molecules, lutein and zeaxanthin are often referred to collectively since they are usually measured together.)
Carotenoids are a great example of why whole foods (rather than dietary supplements) may be the best source of attaining nutrients for most people. While study after study shows carotenoid-rich foods to be of significant importance to preventing chronic disease, the same cannot be said of isolated carotenoid dietary supplements. This fact was brought to public attention when studies suggested that betacarotene supplements were associated with greater risk of developing lung cancer in smokers. While it may be argued that the culprit was that the synthetic carotenoids were in a form not readily acceptable to the body, what cannot be argued is that populations who eat carotenoid-rich foods seem to enjoy better health.
Eating foods rich in carotenoids enhances your body’s usage of these important nutrients since these foods naturally contain other nutrients that act in synergy with carotenoids, supporting their physiological function in your body and therefore contributing to your optimal health. Also, there are probably many other health-promoting carotenoids and phytonutrients contained in whole foods, which science has not yet identified.
Carotenoids are powerful antioxidants, protecting the cells of the body from damage caused by free radicals. While they work in concert, different carotenoids have been found to have unique features. For example, lutein/zeaxanthin are especially active in the eye, protecting the retina and lens from oxidative damage, and therefore protecting against the development of cataracts and age-related macular degeneration. Lycopene is especially effective at quenching a free radical called singlet oxygen and is known for being especially effective at protecting membrane lipids from oxidation, which may be the reason that lycopene intake has been linked with reducing the risk of such health conditions as cardiovascular disease and prostate cancer.
Alpha-carotene, betacarotene and beta-cryptoxanthin are three of the most commonly consumed “provitamin A” carotenoids in the North American diet. Since the body can convert them into retinol, an active form of vitamin A, they can help prevent deficiency of this important nutrient. Among its other functions, vitamin A is important to maintaining a healthy immune system.
Lycopene is also believed to play a role in the prevention of heart disease by inhibiting free radical damage to LDL cholesterol. Before cholesterol can be deposited in the plaques that harden and narrow arteries, it must be oxidized by free radicals. With its powerful antioxidant activity, lycopene can prevent LDL cholesterol from being oxidized. Numerous research studies have also found that diets rich in carotenoid-containing foods are associated with a reduced risk of heart disease.
Carotenoids are found throughout the eyes, with lutein and zeaxanthin being concentrated in the retina and lens. Observational studies have noted that higher dietary intake of lutein and zeaxanthin is related to reduced risk of cataracts and age-related macular degeneration, two eye conditions for which there are minimal options when it comes to effective prevention. Researchers speculate that these carotenoids may promote eye health through their ability to protect the eyes from light-induced oxidative damage and aging through both their antioxidant actions as well as their ability to filter out UV light.
Research suggests that beta-cryptoxanthin may promote the health of the respiratory tract. Serum concentrations of this carotenoid have been found to be associated with improved lung function; individuals who smoke as well as those who inhale second hand smoke have been found to have lower levels of this carotenoid. In addition, the other provitamin A carotenoids—alpha-carotene and betacarotene—may also play a role in promoting lung health since vitamin A itself is known to be necessary for proper growth and development of lung tissue.
Consumption of lycopene-rich foods is associated with a reduced risk of prostate cancer. Recent research has also suggested that lycopene can boost sperm concentrations in infertile men. In one study, a lycopene-supplemented diet resulted in a statistically significant improvement in sperm concentration and motility amongst the 30 infertile men being studied with six pregnancies following as a result of the trial.
Increased intake of beta-cryptoxanthin has been found to be associated with reduced risk of esophageal and lung cancer while intake of lycopene is associated with reduced risk of prostate cancer. One reason that carotenoids may support optimal health is because they have the ability to stimulate cell-to-cell communication, which, if not functioning properly, may contribute to the overgrowth of cells, a condition that eventually leads to cancer.
Carotenoids are fat-soluble substances, and as such require the presence of dietary fat for proper absorption through the digestive tract. Consequently, your carotenoid status may be impaired by a diet that is extremely low in fat or if you have a medical condition that causes a reduction in the ability to absorb dietary fat; these conditions include pancreatic enzyme deficiency, Crohn’s disease, celiac sprue, cystic fibrosis, surgical removal of part or all of the stomach, gall bladder disease, and liver disease.
Due to low consumption of fruits and vegetables, many adolescents and young adults do not take in enough carotenoids. Smokers and drinkers have been found to eat fewer foods that contain carotenoids, while researchers also suspect that cigarette smoke destroys carotenoids.
A low dietary intake of carotenoids is not known to directly cause any diseases or health conditions, at least in the short term. However, if your intake of vitamin A is also low, a dietary deficiency of alpha-carotene, betacarotene, beta-cryptoxan-thin and/or other “provitamin A” carotenoids can cause the symptoms associated with vitamin A deficiency.
Yet, long-term inadequate intake of carotenoids is associated with chronic diseases, including heart disease and various cancers. One important mechanism for this carotenoid-disease relationship appears to be free radicals. Research indicates that diets low in carotenoids can increase the body’s susceptibility to damage from free radicals. As a result, over the long term, carotenoid deficient diets may increase tissue damage from free radical activity, and increase risk of chronic diseases like heart disease and cancers.
High intake of carotenoid-containing foods is not associated with any toxic side effects. As a result, the Institute of Medicine at the National Academy of Sciences did not establish a Tolerable Upper Intake Level (UL) for carotenoids when it reviewed these nutrients in 2000.
Excessive consumption of betacarotene can lead to a yellowish discoloration of the skin called carotenodermia, while excessive lycopene can lead to a deep orange discoloration called lycopenodermia. Both are harmless and reversible.
While there hasn’t been concern about the safety of carotenoids in foods, there has been some concern raised over the safety of carotenoid dietary supplements as reflected in studies that have shown increased risk of lung cancer in smokers taking betacarotene supplements.
Researchers traditionally have attributed the health-promoting effects of plant foods to their comprehensive array of vitamins, minerals and fiber. More recently, however, research studies are uncovering a new story. Plant foods contain thousands of other compounds in addition to macronutrients (carbohydrates, proteins, fats and fiber) and micronutrients (vitamins and minerals). These other compounds are collectively known as phytonutrients (phyto=plant). Simply put, phytonutrients are active compounds in plants that have been shown to provide benefit to humans when consumed.
Like us, plants are exposed to damaging radiation, toxins and pollution, and this toxic exposure results in the generation of free radicals within their cells. Free radicals are reactive molecules that can bind and damage proteins, cell membranes and DNA. Since plants can’t move away from these insults, nature has provided them with a means of protection: they can make a variety of types of protective compounds—the phytonutrients. When we consume plants rich in phytonutrients, they appear to provide humans with protection as well. Investigating the ways in which phytonutrients provide this protection is one of the most exciting areas in nutrition research today, and recent findings are providing science-based explanations as to how plant foods support our health and wellness.
Most plants use sunlight as an energy source. Although to the eye sunlight appears as a single, clear, bright force, it is actually made up of many different wavelengths, some of which plants capture for the generation of energy. Others, however, are wavelengths from which plants need protection. Each plant contains literally thousands of different phytonutrients that can act as antioxidants, providing protection from potentially damaging free radicals. Many of these compounds also provide the plants with color, with their different colors each reflecting a different variety of protection they provide.
If a plant were only one color, with no shades or variations in that color, it would only be able to receive and protect against one specific wavelength of light. A plant with several different colors is like a television set with an antenna, and a plant with many different colors is like a television with a satellite dish. Most plants have a satellite dish’s worth of colors—even ones that look very green to us when we eat them. Like the primer used beneath a coat of paint, these other colors are simply overshadowed by the primary color that we see.
Some researchers estimate up to 40,000 phytonutrients will someday be fully catalogued and understood. In just the last 30 years, many hundreds of these compounds have been identified and are currently being investigated for their health-promoting qualities. At research organizations like the National Institute of Cancer, and at many universities around the world, different individual phytonutrients are being studied to identify their specific health benefits.
While phytonutrients are classified by their chemical structure, because there are so many compounds, phytonutrients are also lumped together in families depending on the similarities in their structures. Names such as terpenes are used to decribe carotenoids, some of which are precursors to vitamin A and which provide the orange, red and pink colors in foods such as carrots, tomatoes and pink shellfish; limonoids, which are found in citrus fruits and provide them with their distinctive smell; and coumarins, natural blood thinners found in parsley, licorice and citrus fruits.
The phenols, or polyphenols (poly=many), is another family of phytonutrients that has received much research attention and discussion in the scientific literature. In fact, some of the most talked about phytonutrients are in this family. They include the anthocyanidins, which give blueberries and grapes their dark blue and purple color, and the catechins, found in tea and wine, which provide the bitter taste as well as the tawny coloring in these foods. Anthocyanidins have been found to provide unique antioxidant protection from free radical damage in both water-soluble and fat-soluble environments. And, their free radical scavenging capabilities are thought to be more potent than many of the currently well-known vitamin antioxidants; anthocyanidins are estimated to have fifty times the antioxidant activity of both vitamin C and vitamin E. Flavonoids are also commonly considered phenols, although the term “flavonoids” can refer to many phytonutrients.
Lastly, the isoflavones are usually categorized as members of this phenol family. Isoflavones, which are found in soy, kudzu, red clover and rye, have been researched extensively for their ability to protect against hormone-dependent cancers, such as breast cancer.
Other phytonutrients include the organosulfur compounds, such as the glucosinolates and indoles from Brassica vegetables like broccoli, and the allylic sulfides from garlic and onions, all of which have been found to support our ability to detoxify noxious foreign compounds like pesticides and other environmental toxins. Organic acids are another common family of phytonutrients and include some powerful antioxidants, like ferulic acid, which are found in whole grains.
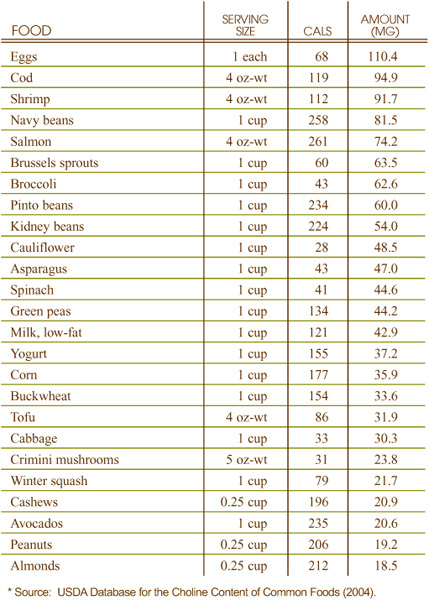
Best Sources of Choline from the World’s Healthiest Foods
What can choline-rich foods do for you?
• Promote proper cell membrane function
• Assist nerve-muscle communication
• Prevent the build-up of homocysteine
What events can indicate a need for more choline-rich foods?
• Fatigue
• Insomnia
• Accumulation of fats in the blood
• Nerve-muscle problems
• Poor ability of the kidneys to concentrate urine
Consistent information is not available on the effects of cooking, storage, and processing on the choline content of food. Like other B complex vitamins, choline can be damaged by overexposure to heat and oxygen, and for this reason overcooking of foods high in choline is not recommended.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for choline. The recommendations are as follows:
• 0–6 months: 125 mg
• 6–12 months: 150 mg
• 1–3 years: 200 mg
• 4–8 years: 250 mg
• 9–13 years: 375 mg
• Males 14 years and older: 550 mg
• Females 9–13 years: 375 mg
• Females 14–18 years: 400 mg
• Females 19 years and older: 425 mg
• Pregnant females: 450 mg
• Lactating females: 550 mg
The FDA has not set a Reference Value for Nutrition Labeling for choline.
Details on choline’s Tolerable Upper Intake Level (UL) are provided under heading “Can You Consume Too Much Choline?”
Even though choline has only recently been officially adopted into the B family of vitamins, it has been the subject of nutritional investigations for almost 150 years. Key research discoveries about choline came in the late 1930s, when scientists discovered that tissue from the pancreas contained a substance that could help prevent fatty build-up in the liver. This substance was named choline after the Greek word chole, which means bile. Since the 1930s, research has shown that choline is found not only in the pancreas and liver, but is also a component of every human cell. In addition to its uniqueness as a fat-modifying substance, choline is chemically unique since it is a trimethylated molecule (a compound that has three methyl groups).
Eating foods rich in choline enhances your body’s usage of this important nutrient since these foods naturally contain other nutrients that act in synergy with choline, supporting its physiological function in your body and therefore best contributing to your optimal health.
Choline is a key component of many fat-containing structures in cell membranes. Since cell membranes are almost entirely composed of fats, the membranes’ flexibility and integrity, key elements of cellular health, depend on adequate supplies of choline. Membrane structures that require choline include phosphatidylcholine and sphingomyelin, which are highly represented in the brain; choline, therefore, is particularly important for brain health.
Choline’s chemical uniqueness as a trimethylated molecule makes it highly important in methyl group metabolism. Many important chemical events in the body are made possible by the transfer of methyl groups from one place to another. For example, genes in the body can be switched on or turned off in this way, and cells can use methylation to send messages back and forth. Choline is also important in the metabolic cycle that keeps levels of homocysteine balanced.
Choline is a key component of acetylcholine, a messenger molecule found in the nervous system that sends messages between nerves and muscles. The neurotransmitter acetylcholine is the body’s primary chemical means of sending messages between nerves and muscles.
In addition to poor dietary intake of choline itself, poor intake of other nutrients can result in choline deficiency. These include vitamin B3 (niacin), folic acid, and the amino acid methionine; all three nutrients are needed in order for choline to obtain the three methyl groups that compose its chemical structure. Additionally, problems including liver cirrhosis are common contributing factors to choline deficiency.
Of special importance in the relationship between choline and health is the impact of choline deficiency on the risk of coronary heart disease and other cardiovascular problems since choline deficiency can lead to homocysteine build-up. Mild choline deficiency has also been linked to fatigue, insomnia, poor ability of the kidneys to concentrate urine, problems with memory, and nerve-muscle imbalances. Choline deficiency can also cause deficiency of folic acid, another B vitamin critically important for health.
The consequences of choline deficiency are particularly visible in the liver since a lack of choline changes the way in which the liver packages and transports fat. The primary symptom of this change in fat packaging is a decrease in the blood level of VLDL (very low-density lipoprotein, a complex fat-containing molecule that the liver uses to transport fat). As part of this same unnatural pattern, levels of blood triglycerides can also become greatly increased as a result of choline deficiency.
Doses of choline in the 5–10 gram/day range have been associated with reductions in blood pressure and in some subjects, feelings of faintness or dizziness. These amounts are typically much higher than the choline content of the foods in the average diet.
In 1998, the Institute of Medicine set the following Tolerable Upper Intake Level (UL) for choline: for those 1–8 years it is 1 gram; 9–13 years old, 2 grams; 14–18 years old, 3 grams; and, 19 years and older, 3.5 grams.
Best Sources of Chromium from the World’s Healthiest Foods
What can chromium-rich foods do for you?
• Help maintain normal blood sugar and insulin levels
• Support normal cholesterol levels
What events can indicate a need for more chromium-rich foods?
• Hyperinsulinemia; insulin resistance
• High blood sugar levels
• Type 2 diabetes
• High blood pressure
• High triglyceride and total cholesterol levels
• Low HDL cholesterol
Under most circumstances, food processing methods decrease the chromium content of foods. For example, when whole grains are milled to make flour, the chromium-containing germ and bran are removed, and consequently, most of the chromium is lost. On the other hand, acidic foods cooked in stainless steel cookware can accumulate small amounts of chromium by leaching the mineral from the cookware.
In 2001, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for chromium. The recommendations are as follows:
• 0–6 months: 0.2 mcg
• 7–12 months: 5.5 mcg
• 1–3 years: 11 mcg
• 4–8 years: 15 mcg
• Males 9–13 years: 25 mcg
• Males 14–50 years: 35 mcg
• Males 51+ years: 30 mcg
• Females 9–13 years: 21 mcg
• Females 14–18 years: 24 mcg
• Females 19–50 years: 25 mcg
• Females 51+ years: 20 mcg
• Pregnant females 14–18 years: 29 mcg
• Pregnant females 19–50 years: 30 mcg
• Lactating females 14–18 years: 44 mcg
• Lactating females 19–50 years: 45 mcg
The FDA has set the Reference Value for Nutrition Labeling for chromium at 120 mcg. This is the recommended intake value used by the FDA to calculate the %Daily Value for chromium that may appear on food labels.
Details on Chromium’s Tolerable Upper Intake Levels (UL) are provided under the heading “Can You Consume Too Much Chromium?”
This essential mineral, required by the body in trace amounts, was first discovered in 1797 by a chemist in France named Louis-Nicolas Vaquelin. Many years later, a physician and research scientist in the U.S. named Walter Mertz discovered that chromium played a key role in carbohydrate metabolism, possibly by participating in formation of a special compound which he named “glucose tolerance factor,” or GTF. Researchers are still not clear whether GTF is an actual chemical compound or not. But they are clear that the nutrients related to GTF—even though they may not be assembled into a single chemical structure—play an important role in blood sugar balance.
Eating foods rich in chromium enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with chromium, supporting its physiological function in your body and therefore contributing to your optimal health.
It is important to eat natural, whole foods since the refinement process strips away naturally occurring chromium. People who consume diets high in simple sugars should be especially careful about consuming enough chromium-rich foods since refined sugars rob the body of chromium by increasing its excretion. Vitamin C increases the absorption of chromium, and many chromium-rich foods come naturally packaged with this important mineral.
As the active component of GTF, chromium plays a fundamental role in controlling blood sugar levels. The primary function of GTF is to increase the cells’ ability to regulate insulin, the hormone responsible for carrying sugar (glucose) into the cells where it can be used for energy.
After a meal, blood glucose levels begin to rise, and, in response, the pancreas secretes insulin, which lowers blood glucose levels by increasing the rate at which glucose enters the cells. To accomplish this, insulin must be able to attach to receptors on the surface of cells. GTF initiates the attachment of insulin to the insulin receptors.
Chromium may also participate in cholesterol metabolism, suggesting a role for this mineral in maintaining normal blood cholesterol levels. In addition, chromium is involved in the metabolism of nucleic acids, which are the building blocks of DNA, the genetic material found in every cell.
If you have diabetes or heart disease, the amount of chromium your body needs may be increased. You may also need extra chromium if you experience physical injury, trauma or mental stress. All of these conditions increase the excretion of chromium. In addition, in the case of stress, the need for increased chromium may be also related directly to blood sugar imbalance. Under severe stress, the body increases its output of certain hormones. These hormonal changes alter blood sugarbalance, and this altered blood sugar balance can create a need for more chromium.
Dietary deficiency of chromium is believed to be widespread in the United States since food processing methods remove most of the naturally occurring chromium from commonly consumed foods. Chromium deficiency leads to insulin resistance, a condition in which the cells of the body do not respond to the presence of insulin. Insulin resistance can lead to elevated blood levels of insulin (hyperinsulinemia) and elevated blood levels of glucose, which can ultimately cause heart disease and/or diabetes. In fact, even mild dietary deficiency of chromium is associated with Syndrome X. This medical condition features a constellation of symptoms, including hyperinsulinemia, high blood pressure, high triglyc-eride levels, high blood sugar levels, and low HDL cholesterol levels, all of which increase one’s risk for heart disease.
Due to the limited nature of existing research studies, the Institute of Medicine at the National Academy of Sciences did not establish set a Tolerable Upper Intake Level (UL) for chromium. However, in 2001, this organization did make a recommendation that individuals with pre-existing liver or kidney disease be particularly careful to limit their chromium intake.
According to the Encyclopedia of Natural Medicine (Pizzorno and Murray, 1998), more than half of the carbohydrates consumed by people in the United States are added to foods as sweetening agents. Simply put, most of the carbohydrates we eat in this country are in the form of highly processed sugars. The typical American diet consists largely of processed foods that are loaded with refined sweeteners, with names like sucrose (table sugar), maltodextrin, fructose, lactose, and high fructose corn syrup. These sweeteners have the same amount of calories per gram as other, more healthful sources of carbohydrates such as whole grains. But, unlike whole grains, refined sweeteners are called “empty calories” because they do not contain any of the essential nutrients, such as fiber, vitamins, and minerals. Eating too much refined sugar is associated with a variety of health conditions including diabetes, hypoglycemia, obesity, poor immune function, mood fluctuations, dental caries, and premenstrual syndrome.
So, take a step towards better health and try these suggestions for eliminating refined sugar from your diet.
• Eat more fruit: Fruit is rich in naturally occurring sugar that can satisfy your craving for sweets. More importantly, most fruits contain fiber and several vitamins and minerals.
• Cut out the soda: If you are a soda drinker, you are getting too much sugar in your diet, plus a lot of other things that aren’t good for you! Also, don’t think you are doing yourself a favor by drinking fruit beverages. The number one ingredient in many of the fruit drinks sold in supermarkets is high fructose corn syrup. If you want to enjoy a fruit juice, choose a product that contains 100% fruit juice.
• Leave out the spoonful of sugar: Many of us add table sugar to hot and cold beverages. To break this habit, start by cutting the amount of sugar you add to your beverages in half, then slowly eliminate the sugar completely.
• Bake and cook with alternatives: If you like to make cookies and other baked goods, you probably use a lot of white and brown sugar. Try substituting a more natural sugar, such as dried organic cane juice, honey or molasses in your favorite cookie and dessert recipes. In addition, puréed fruits (such as dates, bananas and apples) or 100% fruit juice concentrate can be used in place of white and brown sugar in many recipes.
• Use the World’s Healthiest Foods as the foundation of your diet: The foods featured in this book are whole, unprocessed, and nutrient-rich foods. By incorporating more of these foods into your diet, you will automatically reduce your consumption of refined sweeteners.
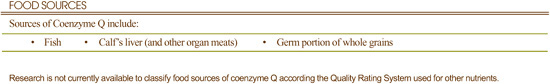
What can coenzyme Q-rich foods do for you?
• Help prevent cardiovascular disease
• Improve energy levels
• Stabilize blood sugar
• Restore the power of vitamin E
What events can indicate a need for more coenzyme Q-rich foods?
• Heart problems like angina, arrhythmia, or high blood pressure
• Problems with the gums
• Stomach ulcers
• High blood sugar
• Muscle weakness and fatigue
No research is currently available about the impact of cooking, storage or processing on this nutrient.
The Institute of Medicine at the National Academy of Sciences has not established a Dietary Reference Intake (DRI) nor Tolerable Upper Intake Level (UL) for coenzyme Q.
Coenzyme Q is extremely important to our health, especially the health of our heart and blood vessels. Its chemical structure was discovered in 1957, and since that time, nearly 5,000 research studies on coenzyme Q have been published.
In many living creatures, the same chemical pathways that make vitamin E, vitamin K, and folic acid also make coenzyme Q. While the human body cannot make these other vitamins, it appears that it can make coenzyme Q.
Coenzyme Q, also called ubiquinone since it is ubiquitiously present in all our cells, is often designated as coenzyme Q10. The number “10” following its name refers to a specific part of its chemical structure.
Coenzyme Q lies at the heart of our cells’ energy producing process. Special organelles (tiny organs) inside our cells, called mitochondria, take fat, carbohydrate and protein, and convert them into usable energy. This process always requires coenzyme Q. In some cells, like heart cells, this energy conversion process can be the difference between life and death, one of the reasons why coenzyme Q is so vital to health.
Coenzyme Q is a well-established antioxidant used by the body to protect cells from oxygen damage. The exact mechanism for this protective effect is not clear. However, in at least one study, up to 95% less damage to cell membranes has been demonstrated following supplementation with coenzyme Q.
Deficiency symptoms for coenzyme Q are not well-studied. However, deficiency of this nutrient has been clearly associated with a variety of heart problems including arrhythmia, angina, heart attack, mitral valve prolapse, high blood pressure, coronary artery disease, atherosclerosis, and congestive heart failure. Problems in regulating blood sugar have also been linked to coenzyme Q deficiency, as have problems with the gums and stomach ulcers.
Certain medications, such as statin drugs or beta blockers, can induce a deficiency of coenzyme Q.
From food sources alone, it would be impossible to obtain the hundred milligram level doses that are thought to be the starting point for toxicity. The Institute of Medicine has not established a Tolerable Upper Intake Level (UL) for coenzyme Q.
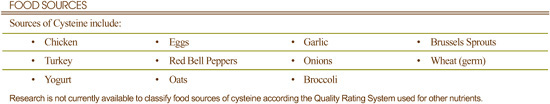
What can cysteine-rich foods do for you?
• Protect cells from free radical damage
• Help your body detoxify chemicals and heavy metals
• Help break down extra mucous in your lungs
What events can indicate a need for more cysteine-rich foods?
• Frequent colds
• COPD (Chronic Obstructive Pulmonary Disease)
No research is currently available about the impact of cooking, storage or processing on cysteine.
In 2002, the Institute of Medicine at the National Academy of Sciences set recommended protein digestibility amino acid standards for 9 amino acids or amino acid combinations. A standard of 25 milligrams per kilogram (one kilogram equals approximately 2.2 pounds) of body weight was set for intake of cysteine-plus-methionine combined. This standard applies to all individuals 1 year of age and older. For example, an individual weighing 70 pounds (31.75 kilograms) would require about 800 milligrams of cysteine-plus-methionine, whereas someone weighing 160 pounds (72.5 kilograms) would need about 1,800 milligrams.
Cysteine is an amino acid that occurs naturally in foods and which, with the help of other nutrient cofactors, can also be manufactured in the body from the amino acid methionine. Cysteine has unique functions since it is only one of two amino acids (the other is methionione) that contains sulfur. Cysteine is an important component of the antioxidant glutathione and can also be converted into the amino acid taurine.
Eating foods rich in cysteine enhances your body’s usage of this important nutrient since these foods naturally contain other nutrients that act in synergy with cysteine, supporting its physiological function in your body and therefore contributing to your optimal health.
As a key constituent of glutathione, cysteine has many important physiological functions. Glutathione, formed from cysteine, glutamic acid, and glycine, is found in all human tissues, with the highest concentrations found in the liver and eyes. Glutathione is a potent antioxidant, protecting fatty tissues from the damaging effects of free radicals. The antioxidant activity of glutathione is attributed specifically to the cysteine that it contains.
As mentioned above, cysteine is a key constituent of glutathione, a compound that also plays a vital role in the detoxification of harmful substances by the liver, which can also chelate (attach to and remove from the body) heavy metals such as lead, mercury, and cadmium. It is also believed that glutathione carries nutrients to lymphocytes and phagocytes, important immune system cells. Cysteine also has the ability to break down proteins found in mucous that settles in the lungs.
The production of cysteine in the body involves several nutrients. As a result, dietary deficiency of methionine, vitamin B-6, vitamin B12, s-adenosyl methionine or folic acid may decrease the production of cysteine.
Cysteine deficiency is relatively uncommon but may be seen in vegetarians with low intake of the plant foods containing methionine and cysteine. There is no known medical condition directly caused by cysteine deficiency, but low cysteine levels may reduce one’s ability to prevent free radical damage and may result in impaired function of the immune system.
The Institute of Medicine at the National Academy of Sciences did not establish a Tolerable Upper Intake Level (UL) for cysteine or other amino acids.
Best Sources of Copper from the World’s Healthiest Foods
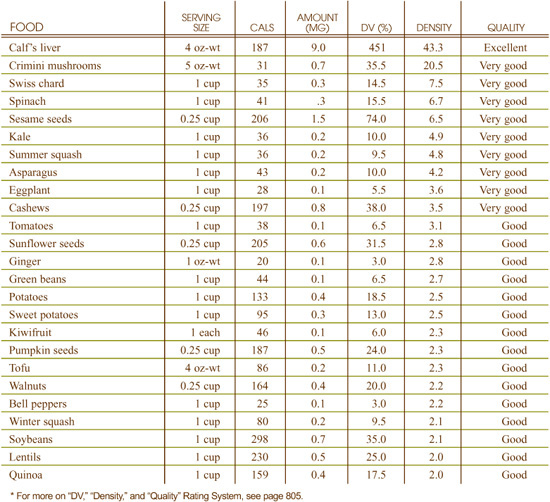
What can copper-rich foods do for you?
• Reduce tissue damage caused by free radicals
• Maintain the health of your bones and connective tissues
• Keep your thyroid gland functioning normally
• Help your body utilize iron
• Preserve your nerves’ myelin sheath
What events can indicate a need for more copper-rich foods?
• Blood vessels that rupture easily
• Bone and joint problems
• Elevated LDL and reduced HDL levels
• Frequent infections
• Iron deficiency anemia
• Loss of hair or skin color
Foods that require long-term cooking can have their copper content substantially reduced; for example, cooking beans may result in them losing one-half of their copper content. The processing of whole grains can also dramatically reduce copper content. In wheat, for example, the refining of the whole grain into 66% extraction wheat flour results in a drop of about 70% in the original copper that was present. Cooking with copper cookware increases the copper content of foods.
In 2000, the Institute of Medicine issued new Adequate Intake (AI) levels for copper for infants up to 1 year old and Recommended Dietary Allowances (RDAs) for all people older than 1 year old. The recommendations are as follows:
• 7–12 months: 220 mcg
• 1–3 years: 340 mcg
• 4–8 years: 440 mcg
• 9–13 years: 700 mcg
• 14–18 years: 890 mcg
• 19+ years: 900 mcg
• Pregnant females 14–50 years: 1 mg
• Lactating females 14–50 years: 1.3 mg
The FDA has set the Reference Value for Nutrition Labeling for copper at 2 mg (one mg equals 1,000 mcg). This is the recommended intake value used by the FDA to calculate the %Daily Value for copper that may appear on food labels.
The Institute of Medicine established a Tolerable Upper Intake Level (UL) for copper that varies by age group: for those 1–8 years it is 1,000 mcg; 9–13 years, 5,000 mcg; 14–18 years, 8,000 mcg; and, 19 years and older, 10,000 mcg.
Copper is an essential trace mineral that is vitally important to health since it is involved in several important enzymatic reactions in the body. It plays such varied roles as promoting collagen maintenance, proper iron absorption and antioxidant activity. Copper is the third most abundant trace mineral in the body. Since many whole, natural foods contain ample amounts of copper, eating a diet rich in the World’s Healthiest Foods can help you to fulfill your daily needs for this important nutrient.
Eating foods rich in copper enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with copper, supporting its physiological function in your body and therefore contributing to your vibrant health.
Superoxide dismutase (SOD) is a copper-dependent enzyme that catalyzes the removal of superoxide radicals from the body. If not eliminated quickly, superoxide radicals cause damage to cell membranes. When copper is not present in sufficient quantities, the activity of SOD is diminished, and the damage to cell membranes caused by superoxide radicals is increased. When functioning in this enzyme, copper works together with the mineral zinc, and it is actually the ratio of copper to zinc, rather than the absolute amount of either mineral alone, that helps this enzyme to function.
Copper also plays a role in many other physiological activities including iron utilization, bone and connective tissue development, energy production, blood clotting, thyroid hormone production, and neurotransmitter synthesis. It also plays a role in maintaining the integrity of the myelin sheath, a covering that protects nerves.
Certain medical conditions including chronic diarrhea, celiac sprue, and Crohn’s disease result in decreased absorption of copper and may increase the risk of developing a copper deficiency. In addition, copper requires sufficient stomach acid for absorption, so if you consume antacids regularly, you may increase your risk of developing a copper deficiency. Inadequate copper status is also observed in children with low protein status and infants fed only cow’s milk without supplemental copper.
Because copper is involved in many functions of the body, copper deficiency produces an extensive range of symptoms. These symptoms include iron deficiency anemia, ruptured blood vessels, osteoporosis, joint problems, brain disturbances, elevated LDL cholesterol, reduced HDL cholesterol, increased susceptibility to infection due to poor immune function, loss of pigment in the hair and skin, weakness, fatigue, breathing difficulties, skin sores, poor thyroid function, and irregular heart beat.
In recent years, nutritionists have been more concerned about copper toxicity than copper deficiency. One partial explanation for this involves the increase in the amount of copper found in drinking water due to the switch in most areas of the country from galvanized (steel) water pipes to copper water pipes. Excessive intake of copper can cause abdominal pain and cramps, nausea, diarrhea, vomiting, and liver damage.
Postpartum depression has also been linked to high levels of copper. This is because copper concentrations increase throughout pregnancy to approximately twice the normal values, and it may take up to three months after delivery for copper concentrations to normalize.
The toxic effects of high tissue levels of copper are seen in patients with Wilson’s disease, a genetic disorder characterized by copper accumulation in various organs. The treatment of Wilson’s disease involves avoidance of foods and supplements rich in copper and drug treatment with chelating agents that remove the excess copper from the body.
The Tolerable Upper Intake Level (UL) for copper varies by age group: for those 1–8 years it is 1,000 mcg; 9–13 years, 5,000 mcg; 14–18 years, 8,000 mcg; and,19 years and older, 10,000 mcg.
Best Sources of Dietary Fiber from the World’s Healthiest Foods
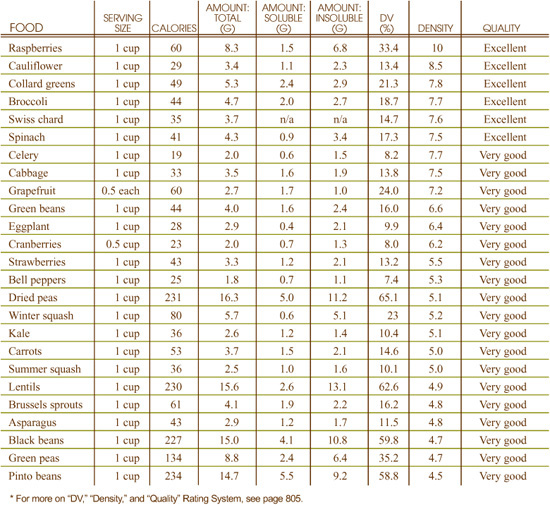
What can fiber-rich foods do for you?
• Support bowel regularity
• Help maintain normal cholesterol levels
• Help maintain normal blood sugar levels
• Help keep unwanted pounds off
What events can indicate a need for more fiber-rich foods?
• Constipation
• Hemorrhoids
• High blood sugar levels
• High cholesterol levels
Many whole foods contain five or more grams of fiber per serving, and in their whole, unprocessed form, would be highly supportive of health. When foods are processed, however, most or all of this fiber is usually lost. For example, most breads sold in the United States use an extraction process whereby the grain’s germ and bran, the components that contain most of its fiber, are discarded. While fruits and vegetables in their natural state are rich in fiber, the juicing process creates a food product with virtually no fiber. Cooking does not affect the dietary fiber content of the food.
In 2002, the Institute of Medicine at the National Academy of Sciences issued Adequate Intake (AI) levels for dietary fiber. The recommendations are as follows:
• 1–3 years: 19 g
• 4–8 years: 25 g
• Males 9–13 years: 31 g
• Males 51+ years: 30 g
• Females 9–13 years: 26 g
• Females 14–18 years: 26 g
• Females 19–50 years: 25 g
• Females 51+ years: 21 g
• Pregnant women: 28 g
• Lactating women: 29 g
The FDA has set the Reference Value for Nutrition Labeling for dietary fiber at 25 g. This is the recommended intake value used by the FDA to calculate the %Daily Value for dietary fiber that may appear on food labels.
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for dietary fiber.
Dietary fiber is undoubtedly one of the most talked about nutrients for health promotion and disease prevention. Promoting digestive health, keeping cholesterol levels in check, and filling you up to prevent your waistline from filling out are just some of its numerous benefits.
Processed refined foods are lacking in fiber, and therefore those who follow the average American diet receive less than the amount recommended to promote optimal health and ward off diseases. Yet, whole unrefined plant-based foods are naturally rich in fiber—yet another way eating the World’s Healthiest Foods helps to keep you healthy.
Fiber has been generally classified as soluble (the type found concentrated in oat bran and barley, which is known to reduce blood cholesterol levels and reduce blood sugar) and insoluble (found in wheat, and legumes, whose function includes promoting bowel regularity). Most whole foods contain both types of fiber; however, there may be a much greater amount of one than the other. Recently, medical and nutrition experts proposed that instead of soluble and insoluble, fiber should be classified according to whether it is viscous or fermentable, as they contend that the original terms do not adequately describe the physiological effects of all the different types of fiber. Categories of fiber include: celluloses, hemicelluloses, polyfructoses, gums, mucilages, pectins, lignins and resistant starches.
Certain types of fiber are referred to as insoluble fibers because the “friendly” bacteria that live in the large intestine can ferment them. The fermentation of dietary fiber in the large intestine (colon) produces a short-chain fatty acid called butyric acid, which serves as the primary fuel for the cells of the large intestines and helps maintain the health and integrity of the colon.
In addition to producing necessary short-chain fatty acids, these bacteria play an important role in the immune system by preventing pathogenic (disease-causing) bacteria from surviving in the intestinal tract. As is the case with insoluble fiber, fibers that are not fermentable in the large intestine help maintain bowel regularity by increasing the bulk of the feces and decreasing the transit time of fecal matter through the intestines. Bowel regularity is associated with a decreased risk for colon cancer and hemorrhoids.
Two other short-chain fatty acids produced during fiber fermentation, propionic and acetic acid, are used as fuel by the cells of the liver and muscles. In addition, propionic acid may be responsible, at least in part, for the cholesterol-lowering properties of fiber.
Soluble fibers lower serum cholesterol by reducing the absorption of dietary cholesterol. In addition, they combine with bile acids, which are made from cholesterol, and remove them from circulation. As a result, the liver must use additional cholesterol to manufacture new bile acids. Soluble fiber may also reduce the amount of cholesterol manufactured by the liver.
Soluble fibers also help normalize blood glucose levels by slowing the rate at which food leaves the stomach and by delaying the absorption of glucose following a meal. They also enhance insulin sensitivity. As a result, high intake of soluble fiber plays a role in the prevention and treatment of Type 2 diabetes. In addition, by slowing the rate at which food leaves the stomach, they promote a sense of satiety, or fullness, after a meal, which can help to prevent overeating and weight gain.
Inadequate chewing can prevent the health benefits of fiber from being realized, since insolube fibers, such as lignins, celluloses, and some hemicelluloses, require extra chewing in order to participate in biochemical processes.
There is no identifiable, isolated deficiency disease caused by lack of fiber in the diet. However, research clearly indicates that low intake of dietary fiber (less than 20 grams per day) over the course of a lifetime is associated with development of numerous health problems including constipation, hemorrhoids, colon cancer, obesity and elevated cholesterol levels.
Intake of dietary fiber in excess of 50 grams per day may cause an intestinal obstruction in susceptible individuals. In most individuals, however, this amount of fiber will improve, rather than compromise, bowel health. Excessive intake of fiber can also cause a fluid imbalance, leading to dehydration. Individuals who decide to suddenly double or triple their fiber intake are often advised to double or triple their water intake for this reason. But an even better approach is to increase fiber intake more gradually, in the range of 50% increases over a period of time long enough for the body to naturally adjust. In addition, excessive intake of soluble fiber, typically in supplemental form, may lead to mineral deficiencies by reducing the absorption or increasing the excretion of minerals.
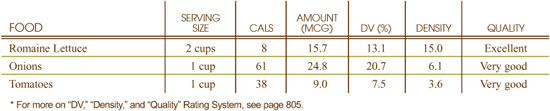
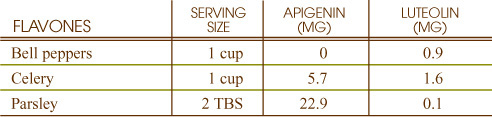
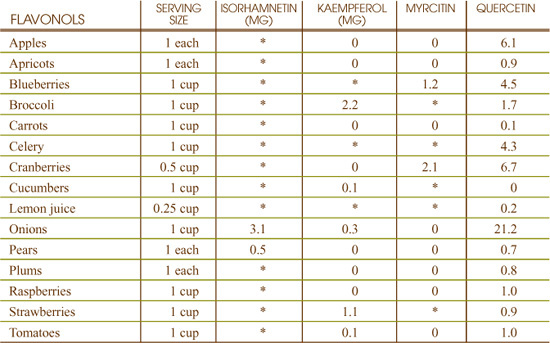
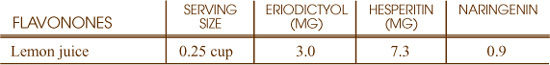
Best Sources of Flavonoids from the World’s Healthiest Foods

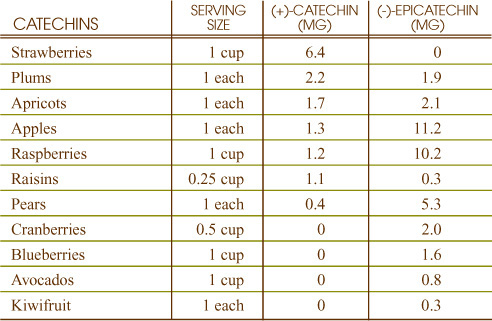
What can flavonoid-rich foods do for you?
• Help protect integrity of your blood vessels
• Protect cells from free radical damage
• Prevent excessive inflammation throughout your body
• Enhance the power of your vitamin C
What events can indicate a need for more flavonoid-rich foods?
• Easy bruising
• Excessive swelling after injury
• Frequent colds or infections
• Frequent nose bleeds
• Low intake of fruits and vegetables
Heat, degree of acidity (pH), and degree of processing can have a dramatic impact on the flavonoid content of food. Overcooking of vegetables has particularly problematic effects on this category of nutrients. For example, in fresh cut spinach, boiling extracts 50% of the total flavonoid content. With onions, boiling removes about 30% of the flavonoids.
In addition to the heat, the amount of cooking water may also play a role in flavonoid loss. A study found that zucchini, beans and carrots cooked with less water had higher polyphenolic flavonoid content than those cooked with larger volumes of water. Therefore, quick cooking methods that use little water such as steaming may be of benefit to conserving maximum amounts of flavonoids.
While flavonoids have been gaining recent attention for their health-promoting properties, currently no public health recommendations, such as Daily Reference Intakes or Daily Values, have been established for these phytonutrients.
Flavonoids, an amazing array of over 6,000 different substances found in virtually all plants, are responsible for many of the plant colors that dazzle us with their brilliant shades of yellow, orange, and red. Classified as plant pigments, flavonoids were discovered in 1938 when a Hungarian scientist named Albert Szent-Gyorgyi used the term “vitamin P” to describe them.
Well-known flavonoids include the flavonols, quercetin, myricitin and kaempferol and the flavones, apigenin and luteolin. Flavonoids may also be named directly after the unique plant that contains them. Ginkgetin is a flavonoid from the ginkgo tree, and tangeretin is a flavonoid from the tangerine.
Flavonoid-rich foods are oftentimes foods that are also rich in vitamin C, which is important since these nutrients need each other to perform effectively. Recent findings that foods as diverse as apples, onions, berries, thyme, berries, tea and red wine had immense health-promoting activities led researchers to discover that many of their benefits may come from their flavonoids.
Most flavonoids function in the human body as antioxidants. In this capacity, they help neutralize overly reactive oxygen-containing molecules and prevent them from damaging parts of cells. Particularly in traditional Chinese medicine, plant flavonoids have been used for centuries in conjunction with their antioxidant, protective properties. While flavonoids may exert their cell structure protection through a variety of mechanisms, as suggested by various research studies, one of their potent effects may be through their ability to increase levels of the powerful antioxidant glutathione.
Inflammation—the body’s natural response to danger or damage—must always be carefully regulated to prevent overactivation of the immune system and unwanted immune response. Many types of cells involved with the immune system have been shown to alter their behavior in the presence of flavonoids. Prevention of excessive inflammation appears to be a key role that many different chemical categories of flavonoids play.
Present-day research has clearly documented the synergistic (mutually beneficial) relationship between flavonoids and vitamin C. Many of the vitamin-related functions of vitamin C also appear to require the presence of flavonoids, as each substance improves the antioxidant activity of the other.
Test tube studies have found that several flavonoids have antimicrobial activity. For example, myricitin has been found to stop the growth of certain strains of Staphylococcus and Klebsiella bacterium while procyanin C-1 has been found to inhibit the growth of HSV-1 (herpes simplex virus).
Poor intake of fruits and vegetables—or routine intake of highly processed fruits and vegetables, whether they be overcooked or juiced—are common contributing factors to flavonoid deficiency.
Potential indicators of flavonoid deficiency include excessive bruising, nosebleeds, swelling after injury, and hemorrhoids. Generally weakened immune function, as evidenced by frequent colds or infections, can also be a sign of inadequate dietary intake of flavonoids.
Even in very high amounts (for example, 140 grams per day), flavonoids do not appear to cause unwanted side effects. Even when raised to the level of 10% of total caloric intake, flavonoid supplementation has been shown to be non-toxic. Studies during pregnancy have also failed to show problems with high-level intake of dietary flavonoids.
Best Sources of Folate from the World’s Healthiest Foods
What can folate-rich foods do for you?
• Support red blood cell production and help prevent anemia
• Help prevent homocysteine build-up
• Support cell production, especially skin cells
• Allow nerves to function properly
What events can indicate a need for more folate-rich foods?
• Depression; irritability
• Mental fatigue, forgetfulness, or confusion
• Insomnia
• General or muscular fatigue
• Gingivitis or periodontal disease
Folate contained in animal products appears to be relatively stable to cooking, unlike folate in plant products, up to 40% of which can be lost from cooking. (In general, however, animal products only tend to average about 10 micrograms of folate per 6-ounce serving. Calf’s liver is an important exception, with over 1,000 micrograms in 6 ounces). Processed grains and flours may have lost up to 70% of their folate; although some manufacturers add folate back to their processed grain product, this is a voluntary procedure, and there are no standards for this process.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Recommended Dietary Allowances (RDAs) for folate. The recommendations are as follows:
• 6–12 months: 80 mcg
• 1–3 years: 150 mcg
• 4–8 years: 200 mcg
• 9–13 years: 300 mcg
• 14+ years: 400 mcg
• Pregnant females: 600 mcg
• Lactating females: 500 mcg
The FDA has set the Reference Value for Nutrition Labeling for folate at 400 mcg. This is the recommended intake value used by the FDA to calculate the %Daily Value for folate that may appear on food labels.
Details of folate’s Tolerable Upper Intake Levels (UL) are provided under the heading “Can You Consume Too Much Folate?”
Folate is a B-complex vitamin most publicized for its importance in pregnancy and prevention of birth defects. The term “folic acid” is sometimes used interchangeably with the term “folate.” Folic acid is the form of folate that is generally available in supplements and fortified foods. In food, as well as in the body, this vitamin is usually found in its folate form.’ In the past few years, it has also gained recognition for the important role it plays in promoting heart health. Its name is derived from the Latin word for “foliage,” reflecting its concentration in many leafy green vegetables.
Folate has a chemically complicated structure and is equally as complicated in its interaction with the human body. For example, many foods contain folate in several different forms, and some of these forms require breakdown by intestinal enzymes for their absorption. Even when the body is operating at full efficiency, only about 50% of ingested food folate is absorbed. Because of this and the popularity of folate-depleted processed foods, folate deficiency is one of the most widespread. That’s one of the many reasons that it is so important to eat the World’s Healthiest Foods since they are concentrated sources of this important nutrient. What’s also great about these folate-rich foods is that they are also rich sources of other B-vitamins, such as B1, B2 and niacin, which are needed in adequate amounts in the body in order for folate to have optimal functioning.
Folate helps maintain healthy circulation of the blood throughout the body by preventing build-up of homocysteine. A high serum homocysteine level is associated with increased risk of cardiovascular disease, and low intake of folate is a key risk factor for elevated homocysteine levels. Increased intake of folic acid, particularly by men, has repeatedly been suggested as a simple way to lower risk of cardiovascular disease by preventing build-up of homocysteine in the blood. Preliminary research also suggests that high homocysteine levels can lead to the deterioration of dopamine-producing brain cells and may therefore contribute to the development of Parkinson’s disease. Therefore, folate deficiency may have an important relationship to neurological health.
One of folate’s key functions as a vitamin is to allow for complete development of red blood cells, which help carry oxygen around the body. When folic acid is deficient, red blood cells cannot form properly and continue to grow without dividing. This condition is called macrocytic anemia, and one of its most common causes is folic acid deficiency.
Cells with very short life spans (like skin cells, intestinal cells, and most cells that line the body’s exposed surfaces or cavities) are also highly dependent on folic acid for their creation. For this reason, folic acid deficiency has repeatedly been linked to problems in these types of tissue, including gingivitis, periodontal disease, seborrheic dermatitis, and vitiligo (loss of skin pigment).
Prevention of neural tube defects in newborn infants is only one of the nervous system-related functions of folic acid. Deficiency of folate has been linked to a wide variety of nervous system problems including general mental fatigue, non-senile dementia, depression, restless leg syndrome, nerve problems in the hands and feet, irritability, forgetfulness, confusion, and insomnia. The link between folate and many of these conditions may involve the role of folate in maintaining a proper balance in the nervous system’s message-carrying molecules.
In addition to poor dietary intake of folate, deficient intake of other B vitamins can contribute to folate deficiency. These vitamins include B1, B2, and B3, which are all involved in folate recycling. Poor protein intake can cause deficiency of folate binding protein that is needed for optimal absorption of folate from the intestines, and can also be related to an insufficient supply of certain amino acids that directly participate in metabolic recycling of folate. Excessive intake of alcohol, smoking, and heavy coffee drinking can also contribute to folate deficiency.
Because of its link with the nervous system, folate deficiency can be associated with irritability, mental fatigue, forgetfulness, confusion, depression, and insomnia. The connections between folate, circulation, and red blood cell status make folate deficiency a possible cause of general or muscular fatigue. Its role in protecting the lining of body cavities means that folate deficiency can also result in intestinal tract symptoms (like diarrhea) or mouth-related symptoms like gingivitis or periodontal disease.
At very high doses greater than 1,000-2,000 mcg, folate intake can trigger the same kinds of nervous system-related symptoms—insomnia, malaise, irritability, intestinal dysfunction—that it is ordinarily used to prevent. Primarily for these reasons, the Institute of Medicine set a Tolerable Upper Intake Level (UL) in 1998 of 1,000 mcg for men and women, 19 years and older. This UL was only designed to apply to “synthetic folate,” defined as the forms obtained from supplements and/or fortified foods.
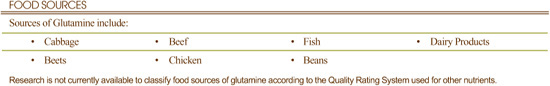
What can glutamine-rich foods do for you?
• Maintain the health of your intestinal tract
• Help your body produce glutathione, a key antioxidant nutrient
• Ensure proper acid-base balance in your body
• Help maintain your muscle mass
What events can indicate a need for more glutamine-rich foods?
• Regular high-intensity exercise
• Intestinal dysbiosis, including irritable bowel syndrome
• Frequent colds or flu
• Severe burns
• Low muscle mass or muscle wasting
No research shows problematic effects of cooking, storage, or processing on glutamine levels in food.
The Institute of Medicine at the National Academy of Sciences has not established a Dietary Reference Intake (DRI) or Tolerable Upper Intake Level (UL) for glutamine.
Glutamine is an amino acid synthesized by the body from another amino acid, called glutamic acid or glutamate. Glutamine is referred to as a conditionally essential amino acid because under certain circumstances the body is unable to produce enough glutamine to meet its needs, so it becomes “essential” during these times to obtain glutamine from the diet. Glutamine is the most abundant amino acid in the blood and muscle tissue and is especially important in maintaining the health of the gastrointestinal tract and the immune system. In recent years, glutamine has become increasingly popular among athletes, as it is believed that glutamine helps prevent infections following athletic events and speeds post-exercise recovery.
Glutamine is the preferred fuel source for the cells lining the small intestine. By nourishing these cells, glutamine helps maintain the health and integrity of the gastrointestinal (GI) tract, which is vital to preserving overall well-being. Glutamine also serves as a source of fuel for muscle and immune cells.
Glutamine plays a role in maintaining the proper acid-base balance in the body. Glutamine also serves as precursor to the antioxidant glutathione, participates in glycogen synthesis (the storage form of carbohydrate), and provides nitrogen compounds for the manufacture of nucleotides that are used to make DNA and RNA.
Because glutamine can be synthesized by the body from the amino acid glutamate, glutamine deficiency is not very common. Nevertheless, muscle and blood concentrations of glutamine are rapidly depleted when the body is confronted with any type of physical stress, such as high-intensity exercise, injury, surgery, burns, infections, and malnutrition, which cause the body to use up its stores of glutamine; during these stressful times, the body is unable to synthesize glutamine quickly enough to meet its needs for this amino acid. Consequently, people under physical stress may be at risk for glutamine deficiency.
Also, the principle site for glutamine synthesis is muscle tissue. As a result, people with low muscle mass, such as the elderly, or those with muscle wasting diseases may be at risk for glutamine deficiency.
Consumption of glutamine from food sources alone is not known to cause any harmful effects. To date, a Tolerable Upper Intake Level (UL) has not been established for glutamine.
One common way of making glutamine inside the body is by converting an amino acid called glutamic acid into glutamine. In order for this conversion to take place, a form of vitamin B-3 is required. Glutamic acid is itself often synthesized though a complicated conversion reaction involving three additional molecules. This complex reaction requires vitamin B-6 in order to occur. For these reasons, vitamins B-3 and B-6 can be regarded as helper nutrients when it comes to glutamine sufficiency in the body.
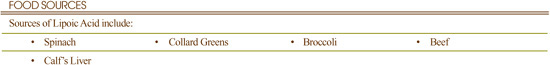
What can lipoic acid-rich foods do for you?
• Maintain your antioxidant defense system
• Help regulate your blood sugar
• Help regenerate vitamin C and E supplies
What events can indicate a need for more lipoic acid-rich foods?
• High blood sugar
• Frequent colds or infections
• Eye problems like cataracts or glaucoma
At present, there are no studies showing the impact of cooking, storage or processing on levels of lipoic acid in foods.
The Institute of Medicine at the National Academy of Sciences has not established a Dietary Reference Intake (DRI) nor Tolerable Upper Intake Level (UL) for lipoic acid.
Our bodies cannot be maximally efficient in producing energy from carbohydrates or fats without the help of lipoic acid. It is also classified as an antioxidant, and it plays a direct role in protecting our cells from oxygen damage in both water-and fat-based environments. In addition, our supplies of several different antioxidants, including vitamins E and C, cannot be successfully maintained in the absence of lipoic acid.
The antioxidant function of lipoic acid has been extensively studied, and its ability to help prevent oxygen-based damage to cells is well established. The antioxidant role of lipoic acid may be the key factor in explaining its success in preventing cataract formation in animal studies. Prevention of oxygen-based damage to nerves is also a key area of clinical research on the possible use of lipoic acid.
Because of its two-fold interactions with both water-soluble (vitamin C) and fat-soluble (vitamin E) substances, lipoic acid has been shown to prevent deficiency of both vitamins in human and animal studies. Other antioxidants seem to benefit equally from the presence of lipoic acid. These antioxidants include coenzyme Q, glutathione, and NADH (a form of niacin).
Since lipoic acid is found in the mitochondria (energy production units) of animal cells, individuals who eat none of the animal foods rich in lipoic acid may be at higher risk for lipoic acid deficiency than individuals who do. Similarly, vegetarians who eat no green leafy vegetables may also be at special risk, since the chloroplasts in these leaves house most of the plants’ lipoic acid. Individuals with poor protein intake, and particularly those with poor intake of the amino acids methionine, cysteine, and taurine may also be at higher risk of lipoic acid deficiency.
Since lipoic acid protects proteins during aging, older individuals may be at greater risk of deficiency. Similarly, because lipoic acid is used to help regulate blood sugar, individuals with diabetes may be at special risk of deficiency. As lipoic acid is absorbed primarily through the stomach, individuals with stomach disorders such as low stomach acid may also be at increased risk of deficiency.
Because lipoic acid works so closely with many other antioxidant nutrients, deficiency symptoms for lipoic acid alone are difficult to pinpoint. Lipoic acid is required for the maintenance of vitamin C supplies, so symptoms of lipoic acid deficiency can imitate symptoms of vitamin C deficiency. These symptoms can include weakened immune function and increased susceptibility to colds and other infections.
Toxicity symptoms from excessive intake of lipoic acid have not been adequately studied. While there have been a few reports of adverse effects, these were from supplementation and were at dosages that are higher than can be obtained through food sources alone.
Best Sources of Iodine from the World’s Healthiest Foods
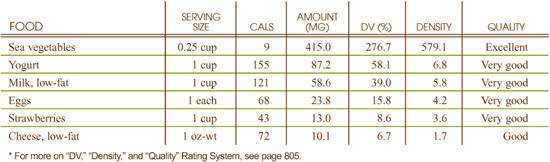
What can iodine-rich foods do for you?
• Help ensure proper thyroid gland functioning
What events can indicate a need for more iodine-rich foods?
• Goiter (enlargement of the thyroid gland)
• Depression
• Fatigue
• Weakness
• Weight gain
Food processing practices often increase the amount of iodine in foods. For example, the addition of potassium iodide to table salt to produce “iodized” salt has dramatically increased the iodine intake of people in developed countries. In addition, iodine-based dough conditioners are commonly used in commercial bread making, which increases the iodine content of the bread.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for iodine for infants up to 1 year old and Recommended Dietary Allowances (RDAs) for all people older than 1 year old. The recommendations are as follows:
• 0–6 months: 110 mcg
• 7–12 months: 130 mcg
• 1–8 years: 90 mcg
• 9–13 years: 120 mcg
• 14+ years: 150 mcg
• Pregnant females: 220 mcg
• Lactating females: 290 mcg
The FDA has set the Reference Value for Nutrition Labeling for iodine at 150 mcg. This is the recommended intake value used by the FDA to calculate the %Daily Value for iodine that may appear on food labels.
Details on iodine’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Iodine?”
Iodine is a trace mineral that is essential for health. We need to receive iodine from our food since this mineral has so many important functions, the most well known being its pivotal role in manufacturing the thyroid hormones, thyroxine and triiodothyronine. Thyroxine is also known as T4, as it contains four iodine atoms while triiodothyronine is known as T3 and contains three iodine atoms. Since thyroid hormones are intricately connected to so many body functions, their importance, and therefore the importance of iodine-containing foods, cannot be stressed enough.
Eating foods rich in iodine enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with iodine, supporting its physiological function in your body and therefore contributing to your optimal health.
As a component of the thyroid hormones thyroxine (T4) and triiodothyronine (T3), iodine is essential to human life. Without sufficient iodine, your body is unable to synthesize these hormones, and because the thyroid hormones regulate metabolism in every cell of the body and play a role in virtually all physiological functions, an iodine deficiency can have a widespread adverse impact on your health and well-being.
Several other physiological functions for iodine have been suggested. Iodine may help inactivate bacteria, hence its use as a skin disinfectant and in water purification. By modulating the effect of the hormone estrogen on breast tissue, iodine may also play a role in the prevention of fibrocystic breast disease, a condition characterized by painful swelling in the breasts. Finally, researchers hypothesize that iodine deficiency impairs the function of the immune system and that adequate iodine is necessary to prevent miscarriages.
The absorption and/or utilization of iodine are inhibited by components of certain foods. These food components, called goitrogenic compounds, are found primarily in cruciferous vegetables (for example, cabbage, broccoli and kale), soybean products, cassava root, peanuts, and millet. While overconsumption of these foods may reduce the amount of available iodine for the manufacture of thyroid hormones, cooking may partly offset this effect. For example, as much as 1/3 of the goitrogenic substances in broccoli (like isothiocyanates) may be deactivated when broccoli is simmered in water. In the early part of the 20th century, iodine deficiency was quite common in the United States and Canada. However, this problem has since been almost completely resolved by the use of iodized salt. In addition, iodine is now added to animal feed, which has increased the iodine content of commonly consumed foods, including cow’s milk, which helps, but does not eliminate, the possibility of iodine deficiency.
Goiter, or enlargement of the thyroid gland, is usually the earliest symptom of iodine deficiency. Goiter is more common in certain geographical areas of the world and is attributed to lack of iodine in the diet as well as to the consumption of goitrogenic foods.
Iodine deficiency may eventually lead to hypothyroidism, which causes a variety of symptoms including fatigue, weight gain, weakness and/or depression. Interestingly, iodine deficiency can also cause hyperthyroidism, a condition characterized by weight loss, rapid heart beat, and appetite fluctuations.
It is difficult to take in too much iodine from food sources alone. In general, even high intakes of iodine from food are well-tolerated by most people. However, in certain circumstances, excessive consumption of iodine can actually inhibit the synthesis of thyroid hormones, thereby leading to the development of goiter and hypothyroidism. Excessive iodine intake may also cause hyperthyroidism, thyroid papillary cancer, and/or iodermia (a serious skin reaction). Individuals with autoimmune thyroid disease (for example, Grave’s disease or Hashimoto’s disease) or those who have experienced an iodine deficiency at some point in their life may be more susceptible to the dangers of excessive iodine consumption.
In an attempt to prevent these symptoms of iodine toxicity, the Institute of Medicine established Tolerable Upper Intake Levels (UL) for iodine. They are as follows: for those 1–3 years it is 900 mcg; 4–8 years, 300 mcg; 9–13 years, 600 mcg; 14–18 years, 900 mcg; 19 years and older, 1,100 mcg; pregnant and lactating women 14–18 years, 900 mcg; and, pregnant and lactating women 19 years and older, 1,100 mcg.
Although iodized salt has been the primary source of iodine in many meal plans for the past fifty years, excessive use of salt has also been a problem in the U.S. In many coastal communities around the world, and particularly in Asia, the primary sources of iodine in meal plans are sea vegetables. Outside of iodized salt, eggs, milk and cheese are the primary sources of iodine in the U.S. diet, and consequently, individuals who do not consume eggs or cow’s milk products may especially benefit from inclusion of sea vegetables in their meal plan.
Eating sea vegetables as part of a healthy diet is nothing new. In fact, archaeological evidence suggests that Japanese cultures have been consuming sea vegetables for more than 10,000 years. While very popular in Asian cuisines, most regions and countries located by waters, including Scotland, Ireland, Norway, Iceland, New Zealand, the Pacific Islands and coastal South American countries, have been consuming sea vegetables since ancient times.
Here is some quantitative information on sea vegetables’ iodine content: one gram of kelp contains between 100 and 200 mcg of iodine, one gram of wakame about 79 mcg, and one gram of dulse between 150 and 500 mcg. The variation in iodine content is related to the circumstances in which they grow.
From a nutrition perspective what’s great about sea vegetables is not just that they are rich in iodine but that they also contain a host of other nutrients. Not only do they feature an array of trace minerals, but they also contain unique phytonutrients known as sulfated polysaccharides (also called fucans) that have been studied for their anti-inflammatory properties.
Best Sources of Iron from the World’s Healthiest Foods
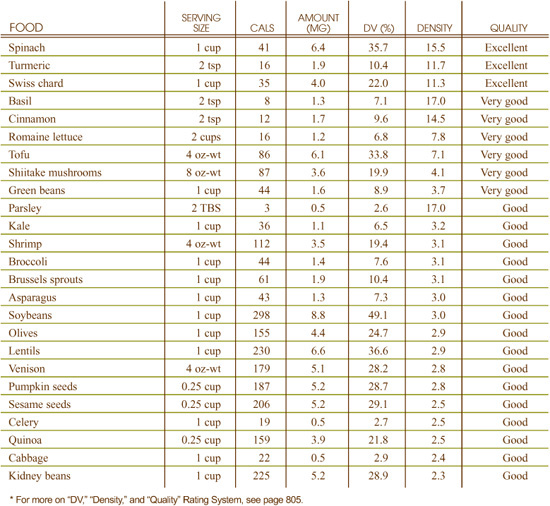
What can iron-rich foods do for you?
• Enhance oxygen distribution in your body
• Keep your immune system healthy
• Help your body produce energy
What events can indicate a need for more iron-rich foods?
• Fatigue and weakness
• Decreased ability to concentrate
• Increased susceptibility to infections
• Depression
• Hair loss; brittle nails
• Headaches; dizziness
Much of the iron in whole grains is found in the bran and germ. As a result, the milling of grain, which removes the bran and germ, eliminates about 75% of the naturally occurring iron in whole grains. Refined grains are often fortified with iron, but the added iron is less absorbable than the iron that naturally occurs in the grain.
Cooking with iron cookware will add iron to food, a practice that can eventually lead to iron toxicity.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for iron for infants up to 6 months old and Recommended Dietary Allowances (RDAs) for all people older than 6 months. The recommendations are as follows:
• 0–6 months: 0.27 mg
• 1–3 years: 7 mg
• 4–8 years: 10 mg
• 9–13 years: 8 mg
• Males 14–18 years: 11 mg
• Male 19+ years: 8 mg
• Females 19–50 years: 18 mg
• Females 51+ years: 8 mg
• Pregnant females 4–50 years: 27 mg
• Lactating females 14–18 years: 10 mg
• Lactating females 19–50 years: 9 mg
The FDA has set the Reference Value for Nutrition Labeling for iron at 18 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for iron that may appear on food labels.
Details on iron’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Iron?”
Iron is vital to the health of the human body, and is found in every human cell, primarily linked with protein to form the oxygen-carrying molecule hemoglobin. The iron in food comes in two forms: heme iron and non-heme iron. Heme iron is found only in animal flesh, as it is derived from the hemoglobin and myoglobin in animal tissues. Non-heme iron is found in plant foods and dairy products.
It is important to eat foods that are rich in iron since several nutrients in these foods increase your body’s ability to absorb iron. Mother nature is very intelligent and packaged these nutrients together in iron-rich foods. For example, iron-rich green vegetables are also concentrated sources of vitamin C, copper, and manganese, nutrients that aid iron absorption. Additionally, amino acids improve iron absorption by stimulating hydrochloric acid secretion in the stomach. Foods such as shrimp, venison, beef and calf’s liver are concentrated sources of both iron and its absorption-boosting amino acids.
Iron serves as the core of the hemoglobin molecule, which is the oxygen-carrying component of the red blood cell. Red blood cells pick up oxygen from the lungs and distribute it to tissues throughout the body. The ability of red blood cells to carry oxygen is attributed to the presence of iron in the hemoglobin molecule.
If we lack iron, we will produce less hemoglobin, and therefore supply less oxygen to our tissues. Iron is also an important constituent of another protein called myoglobin. Myoglobin, like hemoglobin, is an oxygen-carrying molecule that distributes oxygen to muscle cells, especially to skeletal muscles and to the heart.
Iron also plays a vital role in the production of energy as a constituent of several enzymes, including iron catalase, iron peroxidase, and the cytochrome enzymes. It is also involved in the production of carnitine, a nonessential amino acid important for the proper utilization of fat. The function of the immune system is also dependent on sufficient iron.
Iron absorption is decreased in people with low stomach acid (hypochlorhydria), a condition that is common in the elderly and those who use antacids frequently. In addition, iron absorption is decreased by caffeine and tannic acid found in coffee and tea and by phosphates found in carbonated soft drinks. Phytates, found in whole grains, and oxalates, found in spinach and chocolate, may also decrease iron absorption by forming complexes with the mineral, which cannot be absorbed through the digestive tract.
Although the human body conserves iron very well by reusing iron from old red blood cells to make hemoglobin for new red blood cells, iron deficiency is one of the most common nutrient deficiencies in the United States and around the world. Poor iron status may be caused by inadequate dietary intake, poor absorption, parasitic infection, and/or medical conditions that cause internal bleeding.
People who donate blood regularly, women with excessive menstrual bleeding, those who use medications (for example, antacids) that interfere with the absorption of iron, and pregnant and lactating women may be at risk for iron deficiency. In addition, the elderly, vegetarians, and children often have inadequate intake of this mineral.
Iron deficiency causes microcytic and hypochromic anemia, a condition characterized by underdeveloped red blood cells that lack hemoglobin, thereby reducing their oxygen-carrying capacity. But even before iron deficiency anemia develops, people with poor iron status may experience a variety of symptoms including fatigue, weakness, loss of stamina, decreased ability to concentrate, increased susceptibility to infections, hair loss, dizziness, headaches, brittle nails, apathy, and depression. In children, iron deficiency is associated with learning disabilities and a lower IQ.
Although iron overload is not likely to develop from food sources alone, men, because they do not experience the regular iron losses associated with the menstrual cycle in women, may be at greater risk for the problems associated with excessive iron. In recent years, excess iron intake and storage, especially in men, has been implicated as a cause of heart disease and cancer. In addition, iron has been found in increased levels in the joints of people with rheumatoid arthritis.
The Institute of Medicine set the following Tolerable Upper Intake Levels (UL) for iron: 7 months to 13 years, 40 mg; 14 years and older, 45 mg; and, pregnant or lactating women, 45 mg.
Best Sources of Magnesium from the World’s Healthiest Foods
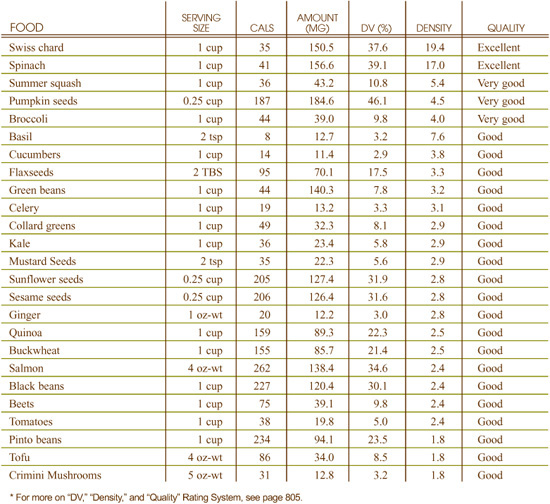
What can magnesium-rich foods do for you?
• Relax nerves and muscles
• Build and strengthen bones
• Keep your blood circulating smoothly
What events can indicate a need for more magnesium-rich foods?
• Muscle weakness, tremor, or spasm
• Elevated blood pressure
• Imbalanced blood sugar levels
• Headaches
The impact of cooking and processing on magnesium can vary greatly. Since a greater percent of magnesium is found in water-soluble form, blanching, steaming, or boiling can result in a substantial loss of magnesium. For example, about one-third of the magnesium in spinach is lost after blanching, while cooking beans may result in 65% loss. In other foods, like almonds or peanuts, very little loss of magnesium results either from roasting or from processing into nut butter.
In 1997, the Institute of Medicine at the National Academy of Sciences issued Recommended Dietary Allowances (RDAs) for magnesium. The recommendations are as follows:
• 1–3 years: 80 mg
• 4–8 years: 130 mg
• 9–13 years: 240 mg
• Males 14–18 years: 410 mg
• Males 19–30 years: 400 mg
• Females 14–18 years: 360 mg
• Females 19–30 years: 310 mg
• Females 31+ years: 320 mg
• Pregnant females up to 18 years: 400 mg
• Pregnant females 19–30 years: 350 mg
• Pregnant females 31–50 years: 360 mg
• Lactating females up to 18 years: 360 mg
• Lactating females 19–30 years: 310 mg
• Lactating females 31–50 years: 320 mg
The FDA has set the Reference Value for Nutrition Labeling for magnesium at 400 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for magnesium that may appear on food labels.
Details on magnesium’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Magnesium?”
Magnesium is usually referred to as a “macromineral,” which means that our food must provide us with hundreds of milligrams of magnesium every day. Inside our bodies, magnesium is found mostly in our bones (60–65%), but is also concentrated in our muscles (25%), and in other cell types and body fluids. Like all minerals, magnesium cannot be made in our body and must therefore be plentiful in our diet in order for us to remain healthy. Magnesium is sometimes regarded as a “calming” mineral, since it has the ability to relax our muscles.
Eating foods rich in magnesium enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with magnesium, supporting its physiological function in your body and therefore contributing to your optimal health.
Magnesium acts together with calcium to help regulate the body’s nerve and muscle tone. In many nerve cells, magnesium serves as a chemical gate blocker—as long as there is enough magnesium around, calcium can’t rush into nerve cells and activate the nerve. This helps keep the nerve relaxed. If our diet provides us with too little magnesium, this gate blocking can fail, and the nerve cells can become overly activated, sending too many messages to the muscles and causing them to overcontract. This chain of events helps explain how magnesium deficiency can trigger muscle tension, soreness, spasms, cramps, and fatigue.
Magnesium plays a role in maintaining bone health with about two-thirds of all magnesium in our body found in our bones. The magnesium found in bone has two very different roles to play in our health. Some of it helps give bones their physical structure by being part of the bone’s crystal lattice scaffolding, together with the minerals phosphorus and calcium. Bone’s other reservoir of magnesium is found on its surface, and while it does not appear to be involved in the bone’s structure, it does act as a storage site for magnesium that the body can draw upon in times of poor dietary supply.
Over 300 different enzymes, body proteins that trigger chemical reactions, require magnesium in order to function. For this reason, the functions of this mineral are especially diverse. It is involved in the metabolism of proteins, carbohydrates, and fats and also helps genes function properly. Some fuels cannot be stored in our muscle cells unless adequate supplies of magnesium are available. The metabolic roles of magnesium are so diverse that it is difficult to find a body system that is not affected by magnesium deficiency.
In addition to poor dietary intake, problems in the digestive tract are the most common cause of magnesium deficiency. These digestive tract problems include malabsorption, diarrhea, and ulcerative colitis. Many kinds of physical stresses can contribute to magnesium deficiency, including cold, stress, physical trauma, and surgery.
Because magnesium plays such a wide variety of roles in the body, the symptoms of magnesium deficiency can also vary widely. Many symptoms involve changes in nerve and muscle function, including muscle weakness, tremor, and spasm. In the heart muscle, magnesium deficiency can result in arrhythmia, irregular contraction, and increased heart rate. Because of magnesium’s role in bone structure, the softening and weakening of bone can also be a symptom of magnesium deficiency. Other symptoms can include: imbalanced blood sugar levels; headaches; elevated blood pressure; depression; and lack of appetite.
There do not seem to be any toxicity symptoms associated with the intake of high amounts of magnesium from food, which is why the Institute of Medicine did not set a Tolerable Upper Intake Level (UL) for dietary magnesium. Alternatively, symptoms associated with high levels of magnesium from dietary supplements have been reported; the most common toxicity symptom associated with high levels of magnesium intake is diarrhea. The UL for magnesium from dietary supplements is 350 milligrams.
Best Sources of Manganese from the World’s Healthiest Foods
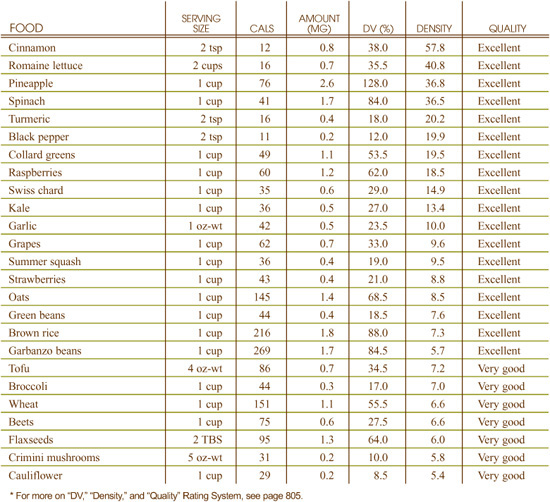
What can manganese-rich foods do for you?
• Protect your cells from free radical damage
• Keep your bones strong and healthy
• Maintain normal blood sugar levels
• Promote optimal function of your thyroid gland
• Maintain the health of your nerves
• Help your body synthesize cholesterol
What events can indicate a need for more manganese-rich foods?
• High blood sugar levels
• Excessive bone loss
• Low cholesterol levels
• Loss of hair color
• Skin rash
• Reproductive system difficulties
Significant amounts of manganese can be lost in food processing, especially in the milling of whole grains to produce flour, and in the cooking of beans. For example, three and one-half ounces of raw navy beans start out with about one milligram of manganese, which drops by 60% to 0.4 milligrams after cooking.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for manganese. The recommendations are as follows:
• 7–12 months: 600 mcg
• 1–3 years: 1.2 mg
• 4–8 years: 1.5 mg
• Males 9–13 years: 1.9 mg
• Males 14–18 years: 2.2 mg
• Males 19+ years: 2.3 mg
• Females 9–18 years: 1.6 mg
• Females 19+ years: 1.8 mg
• Pregnant or lactating females: 2 mg
The FDA has set the Reference Value for Nutrition Labeling for manganese at 2.0 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for manganese that may appear on food labels.
Details on manganese’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Manganese?”
Manganese, a trace mineral that participates in many enzyme systems in the body, was first considered an essential nutrient in 1931. Researchers discovered that experimental animals fed a diet deficient in manganese demonstrated poor growth and impaired reproduction. Manganese is found widely in nature, but occurs only in trace amounts in human tissues. Yet, while there may only be a relatively small amount in our bodies, manganese plays a vitally big role in maintaining our health through being a necessary cofactor of very important enzymes. Like other minerals, the body cannot make manganese, and so we must obtain this important mineral from our food.
Eating foods rich in manganese enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with manganese, supporting its physiological function in your body and therefore best contributing to your optimal health.
Manganese activates the enzymes responsible for the utilization of several key nutrients, including biotin, vitamin B1, vitamin C, and choline. It is a catalyst in the synthesis of fatty acids and cholesterol, facilitates protein and carbohydrate metabolism, and may also participate in the production of sex hormones and the maintenance of reproductive health.
In addition, manganese activates the enzymes that are important in the formation of bone. It has also been theorized that manganese is involved in the production of the thyroid hormone known as thyroxine and in maintaining the health of nerve tissue. Manganese is also a component of a variety of enzymes, playing a role in other physiological functions including blood sugar regulation.
Additionally, manganese-dependent superoxide dismutase (SOD) is an enzyme that has antioxidant activity and protects tissues from the damaging effects of free radicals. This enzyme is found exclusively inside the body’s mitochondria (oxygen-based energy factories inside most of our cells).
Poor dietary intake of manganese appears to be the most common cause of manganese deficiency. However, other factors can contribute to a need for more manganese. Like zinc, manganese is a mineral that can be excreted in significant amounts through sweat, and individuals who go through periods of excessive sweating may be at increased risk for deficiency.
Proper formation of bile in the liver and proper circulation of bile through the body are also required for manganese transport. As a result, individuals with chronic liver or gallbladder disorders may need more dietary manganese.
Because manganese plays a role in a variety of enzyme systems, dietary deficiency of manganese can impact many physiological processes. In humans, manganese deficiency is associated with poor glucose tolerance (high blood sugar levels), skin rash, loss of hair color, excessive bone loss, low cholesterol levels, and compromised function of the reproductive system. It is important to emphasize, however, that manganese deficiency is very rare in humans, and does not usually develop.
Although symptoms of manganese toxicity do not typically appear even at high levels of dietary intake, in severe cases of excessive manganese consumption, individuals can develop a syndrome called “manganese madness,” characterized by hallucinations, violent acts, and irritability. overconsumption of manganese is also associated with impotency. Manganese toxicity is most likely to occur in people with chronic liver disease, as the liver plays an important role in eliminating excess manganese from the body.
The Institute of Medicine established Tolerable Upper Intake Levels (UL) for manganese. They are as follows: for those 1–3 years it is 2 mg; 4–8 years, 3 mg; 9–13 years, 6 mg; 14–18 years, including pregnant and lactating women, 9 mg; and, those older than 19 years, including pregnant and lactating women, 11 mg. It would be very unlikely for a meal plan to exceed these levels.
Best Sources of Niacin from the World’s Healthiest Foods
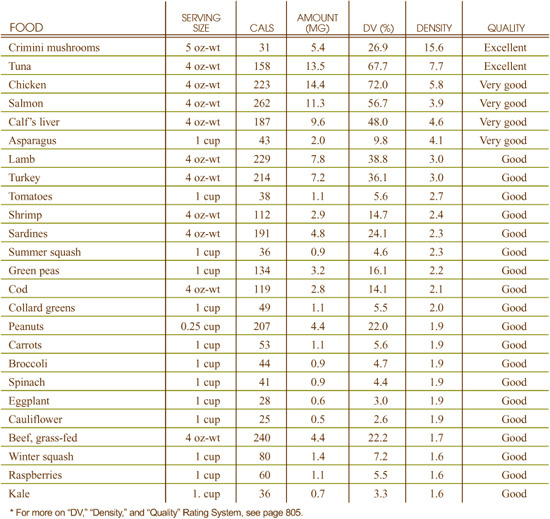
What can niacin-rich foods do for you?
• Stabilize your blood sugar
• Support genetic processes in your cells
• Help lower cholesterol levels
• Help your body process fats
What events can indicate a need for more niacin-rich foods?
• Generalized or muscular weakness
• Digestive problems
• Skin infections
• Lack of appetite
Niacin is one of the more stable water-soluble vitamins and is minimally susceptible to damage by air, light, and heat.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Recommended Dietary Allowances (RDAs) for niacin. The recommendations are as follows:
• 0–6 months: 2 mg
• 6–12 months: 4 mg
• 1–3 years: 6 mg
• 4–8 years: 8 mg
• 9–13 years: 12 mg
• Males 14+ years: 16 mg
• Females 14+ years: 14 mg
• Pregnant females: 18 mg
• Lactating females: 17 mg
The FDA has set the Reference Value for Nutrition Labeling for niacin at 20 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for niacin that may appear on food labels.
Details on niacin’s Tolerable Upper Intake Levels (UL) are provided under the heading “Can You Consume Too Much Niacin?”
Niacin is a member of the B-complex vitamin family. The term “niacin” that is used interchangeably with vitamin B3 is actually a non-technical term that refers to several different chemical forms of the vitamin. These forms include nicotinic acid and nicotinamide (niacinamide).
Although niacin can be made in the body from the amino acid tryptophan, inadequate intake of many nutrients, including protein, iron, vitamins B1, B2, B6, and C, inhibits this conversion; therefore, it is recommended that people also ensure that they obtain adequate niacin from their diet. This is not difficult to do since many niacin-rich foods also contain the other nutrients necessary for niacin’s production from tryptophan. Another reason getting your niacin from food is important is that most of these foods also contain vitamin B12, and a deficiency of this B vitamin can lead to increased excretion of niacin.
Like its fellow B-complex vitamins, niacin is important in energy production. Two unique forms of niacin (called nicotinamide adenine dinucleotide, or NAD, and nicotinamide adenine dinucleotide phosphate, or NADP) are essential for conversion of the body’s proteins, fats, and carbohydrates into usable energy. Niacin is also used to synthesize starch that can be stored in the body’s muscles and liver for eventual use as an energy source.
Niacin plays a critical role in the chemical processing of fats in the body. The building blocks for fat-containing structures in the body (like cell membranes) typically require the presence of niacin for their synthesis, as do many fat-based steroid hormones.
Components of DNA, the primary genetic material in our cells, require niacin for their production; deficiency of niacin, like deficiency of other B-complex vitamins, has been directly linked to genetic (DNA) damage. The relationship between niacin and DNA damage appears to be particularly important in relationship to cancer and its prevention.
Although experts cannot agree on the precise mechanism though which niacin affects blood sugar regulation and function of the hormone insulin, the vitamin has repeatedly been shown to be involved in insulin metabolism and blood sugar regulation. Researchers continue to investigate the exact relationship between niacin, insulin, and blood sugar levels.
Intestinal problems, including chronic diarrhea, inflammatory bowel disease, and irritable bowel disease can all trigger niacin deficiency. Because part of the body’s supply comes from conversion of the amino acid tryptophan, deficiency of tryptophan can also increase risk of niacin deficiency. (Tryptophan deficiency is likely to occur in individuals with poor overall protein intake.) Physical trauma, all types of stress, long-term fever, and excessive consumption of alcohol have also been associated with increased risk of niacin deficiency.
Because of its unique relationship with energy production, niacin deficiency is often associated with general weakness, muscular weakness, and lack of appetite. Skin infections and digestive problems can also be associated with niacin deficiency.
In the amounts provided by food, no symptoms of toxicity have been reported in the scientific literature. The Institute of Medicine has set a Tolerable Upper Intake Level (UL) for niacin of 35 milligrams. This UL applies to men and women 19 years or older, and is limited to niacin that is obtained from supplements and/or fortified foods.
Q I heard that anything fortified or enriched is bad for you. Is this true?
A Enriched foods are not necessarily bad for you although some enriched foods are less than ideal. For example, let’s look at white bread. It is made from wheat that is refined, stripped of many of its nutrients, and then has nutrients added back to it. I would much rather have bread made from whole wheat, where the nutrients you enjoy are those that are the original ones that were included in the wheat itself. Enrichment or fortification may not necessarily be bad, but philosophically I like to enjoy foods that just feature their natural compendium of nutrients, rather than those that feature nutrients that were either added back after they were removed, or added to a food but not naturally there in the first place.
Best Sources of Omega-3 Fatty Acids from the World’s Healthiest Foods Seafood sources (contain the omega-3 fatty acids EPA, DHA, and DPA in addition to ALA)
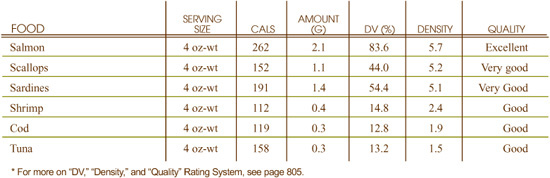
Best Sources of Omega-3 Fatty Acids from the World’s Healthiest Foods Plant food sources (contain the omega-3 fatty acid ALA)
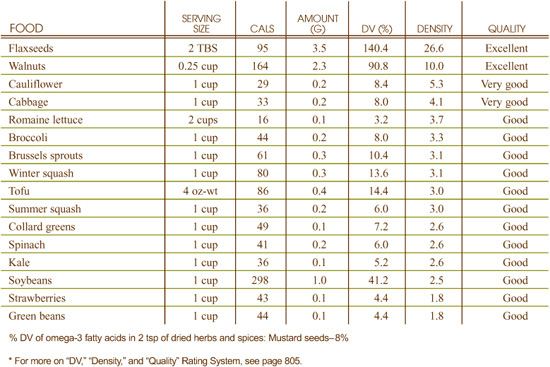
What can omega-3 fatty acid-rich foods do for you?
• Reduce inflammation throughout your body
• Keep your blood from clotting excessively
• Maintain the fluidity of your cell membranes
What events can indicate a need for more omega-3 fatty acid-rich foods?
• Depression
• Fatigue; inability to concentrate
• Dry, itchy skin; brittle hair and nails
• Joint pain
Omega-3 fatty acids are susceptible to damage from heat, light, and oxygen. When exposed to these elements for too long, they can become oxidized or rancid, which not only alters the flavor and smell of the oil, but also diminishes its nutritional value. In addition, the oxidation of fatty acids produces free radicals, which are believed to play a role in the development of cancer and other degenerative diseases.
In 2002, the Institute of Medicine at the National Academy of Sciences issued Adequate Intake (AI) levels for linolenic acid, the initial building block for all omega-3 fatty acids found in the body. For male teenagers and adult men, 1.6 grams per day were recommended. For female teenagers and adult women, the recommended amount was 1.1 grams per day. These guidelines do not seem as well-matched to the existing health research on omega-3 fatty acids as guidelines issued by the “Workshop on the Essentiality of and Recommended Dietary Intakes (RDI) for Omega-6 and Omega-3 Fatty Acids” in 1999 sponsored by the National Institutes of Health (NIH). This panel of experts recommended that people consume at least 1.2% of their total daily calories as omega-3 fats. To meet this recommendation, a person consuming 1,800 calories per day should eat sufficient omega-3-rich foods to provide at least 2.5 grams of omega-3 fatty acids.
Omega-3 fatty acids are a type of polyunsaturated fat whose importance in health promotion and disease prevention cannot be overstated. The three most nutritionally important omega-3 fatty acids are alpha-linolenic acid, (ALA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
ALA is classified as “essential” because the body is unable to manufacture it on its own and because it plays a fundamental role in several physiological functions. The body can convert ALA into EPA and DHA; however, this conversion can be limited, with less than one-third of the ALA being converted into the EPA and DHA forms. For this reason vegans and vegetarians relying on ALA as their only source of omega-3 fatty acids should increase their consumption of ALA-rich foods accordingly to ensure sufficient production of its important derivatives, EPA and DHA.
EPA and DHA can also be derived directly from certain foods, most notably cold-water fish including salmon, tuna and sardines. In addition, certain types of algae contain DHA. Omega-3 fatty acids are believed to play a role in the prevention of cardiovascular disease, while DHA, in particular, is necessary for proper brain and nerve development.
By getting your omega-3 fatty acids from whole food sources, you will gain the benefit of nature’s wisdom. Most omega-3 rich foods also contain vitamin E, which serves to protect the fats from oxidation, a chemical process that produces free radicals.
Diets rich in omega-3 fats produce cell membranes with a high degree of fluidity, therefore promoting optimal functioning of the cells. In addition to their ability to receive nutrients and effectively remove wastes, a healthy membrane promotes the ability of a cell to communicate with other cells. Researchers believe that loss of cell-to-cell communication is one of the physiological events that leads to growth of cancerous tumors. Recent in vitro (test tube) evidence suggests that when omega-3 fatty acids are incorporated into cell membranes, they may help to protect against cancer, notably of the breast.
Omega-3 fats play an important role in the production of prostaglandins, powerful hormone-like substances that regulate many important physiological functions, including blood pressure, blood clotting, nerve transmission, the inflammatory and allergic responses, the functions of the kidneys and gastrointestinal tract, and the production of other hormones.
For example, EPA and DHA serve as direct precursors for series-3 prostaglandins, which have been called “good” or “beneficial” because they reduce platelet aggregation, reduce inflammation and improve blood flow. The role of EPA and DHA in the prevention of cardiovascular disease can be explained in large part by the ability of these fats to increase the production of favorable prostaglandins.
Recent statistics indicate that nearly 99% of people in the United States do not eat enough omega-3 fatty acids. In addition, in some people, the enzymes that convert ALA to EPA and DHA are underactive, so they are not able to optimally convert ALA to EPA and DHA. To increase the efficacy of this conversion, be sure that your diet includes a sufficient amounts of vitamin B6, vitamin B3, vitamin C, magnesium and zinc, cofactors of conversion enzymes. In addition, limit your intake of saturated fat and partially hydrogenated fat, as these compounds are known to decrease the activity of the conversion enzymes.
Since the symptoms of omega-3 fatty acid deficiency are very vague and can often be attributed to some other health condition or nutrient deficiencies, few people (or their physicians, for that matter) realize that they are not consuming enough omega-3 fatty acids. The symptoms of omega-3 fatty acid deficiency include fatigue, dry and/or itchy skin, brittle hair and nails, constipation, frequent colds, depression, poor concentration, lack of physical endurance, and/or joint pain.
In its 2002 guidelines for omega-3 fatty acid intake, the Institute of Medicine at the National Academy of Sciences declined to establish a Tolerable Upper Intake Level (UL) for omega-3s. However, research was cited showing increased risk of bleeding and hemorrhagic stroke in a few studies following supplementation with omega-3s.
Excessive consumption of omega-3 fatty acids from food sources has not known to cause any health problems.
Best Sources of Pantothenic Acid from the World’s Healthiest Foods
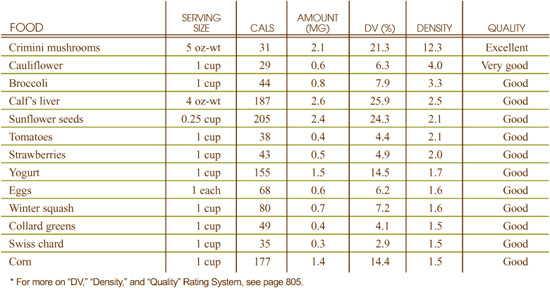
What can pantothenic acid-rich foods do for you?
• Help turn carbohydrates and fats into usable energy
• Improve your ability to respond to stress by supporting your adrenal glands
• Assure adequate production of healthy fats in your cells
What events can indicate a need for more pantothenic acid-rich foods?
• Fatigue, listlessness
• Sensations of weakness
• Numbness, tingling, and burning/shooting pain in the feet
Pantothenic acid is relatively unstable in food, and significant amounts of this vitamin can be lost through cooking, freezing, and commercial processing. For example, research on frozen foods has shown a loss of 21–70% for pantothenic acid in meats and similar losses for processed cereal grains and canned vegetables. Fruits and fruit juices lose 7–50% of their pantothenic acid during processing and packaging.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for pantothenic acid. The recommendations are as follows:
• 0–6 months: 1.7 mg
• 6–12 months: 1.8 mg
• 1–3 years: 2 mg
• 4–8 years: 3 mg
• Males 9–13 years: 4 mg
• Males 14+ years: 5 mg
• Females 9–13 years: 4 mg
• Females 14+ years: 5 mg
• Pregnant females: 6 mg
• Lactating females: 7 mg
The FDA has set the Reference Value for Nutrition Labeling for panthothenic acid at 10 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for panthothenic acid that may appear on food labels.
Details on pantothenic acid’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Pantothenic Acid?”
Pantothenic acid, also known as vitamin B5, is a member of the B-complex family of vitamins first researched in the 1930–1940s. The name of the vitamin comes from the Greek word pantos, meaning “everywhere.” The vitamin’s name reflects its almost universal presence in nature; it is found in virtually all types of food.
Nutrients such as folate, biotin, and vitamin B12 are required for proper use of pantothenic acid in the body’s metabolic pathways, while vitamin C is necessary for preventing B5 deficiency. Foods that feature pantothenic acid also feature these important vitamins as well.
In its metabolically active form, pantothenic acid gets combined with another small, sulfur-containing molecule to form coenzyme A (or simply, CoA). This conversion allows pantothenic acid to participate in a wide variety of chemical reactions.
Eating foods rich in panthothenic acid enhances your body’s usage of this important vitamin since these foods naturally contain other nutrients that act in synergy with pantothenic acid, supporting its physiological function in your body and therefore contributing to your optimal health.
When found in its CoA form, pantothenic acid plays a pivotal role in helping release energy from sugars, starches, and fats. Most of this energy release occurs in the energy production factories found in every cell called the mitochondria. Increased levels of pantothenic acid in the blood of marathon runners, for example, has led to interest in this vitamin as a potential aid in physical training, where sustained energy release from the mitochondria is critical.
While the CoA form of pantothenic acid is important for releasing energy stored as fat, it is equally important for the creation of important fat-containing molecules. Two basic types of fats—fatty acids and cholesterol—both require the CoA form of pantothenic acid for their synthesis. Sphingosine, a fat-like molecule that is constantly involved in the delivery of chemical messages inside our cells, also requires pantothenic acid for its synthesis.
Sometimes it is important for the body to make small chemical changes in the shape of cell proteins. For example, if a cell does not want its proteins to be chemically broken down into other substances, it may want to modify their structure in order to prevent this chemical breakdown. One way for cells to accomplish this task is to attach acetyl chemical groups to proteins. Pantothenic acid in the form of CoA, can be used to help acetylate proteins, thereby protecting them from chemical breakdown. Additionally, sometimes this chemical process can dramatically change the function of a protein. For example, sometimes the acetylation of a protein can pave the way for its conversion into a hormone. This process is especially well researched in relationship to the body’s adrenal glands, where stress-related hormone production requires participation of pantothenic acid.
In addition to poor dietary intake, digestive problems are the most common contributing factor to pantothenic acid deficiency. The reason for this connection between poor digestion and pantothenic acid deficiency involves the CoA form of pantothenic acid which is typically found in food. Proper digestion is required to release pantothenic acid from this CoA form and allow it to be absorbed into the body from the small intestine.
Because pantothenic acid is needed to release energy from carbohydrates and fats, its deficiency is often related to low energy-related symptoms. These symptoms include fatigue, listlessness, and sensations of weakness. One rare symptom of pantothenic acid deficiency is called “burning foot syndrome.” In this condition, numbness and tingling, together with burning and shooting pain, in the feet occurs.
The amount of pantothenic acid available in food is not likely to be associated with any adverse events. In addition, because no other toxicity symptoms have been reported in the research literature, no Tolerable Upper Intake Level (UL) was established by the Institute of Medicine for pantothenic acid in its 1998 report on this vitamin.
Q Are there foods that are bad for my immune system?
A Your immune system is not just involved in fighting invaders like bacteria, but also becomes activated when you eat foods to which you are intolerant or allergic. Reactions to allergic foods can be quick, like the anaphylactic reaction often seen with peanut or shellfish allergies, but food allergy reactions can also be delayed and cause a number of symptoms like headaches, fatigue, muscle aches, rashes and other systemic (whole body) effects. The most common allergenic foods include peanuts, shellfish, cow’s milk, wheat, and soy; however, everyone is unique in their food intolerances and allergies.
Processed foods and foods produced with pesticides or not grown organically may also be problematic for your immune function. Toxic metals such as cadmium, lead and mercury are immunosuppressive. Some pesticides and preservatives can negatively affect the gastrointestinal lining. Excess sugar can also cause stress on the immune system.
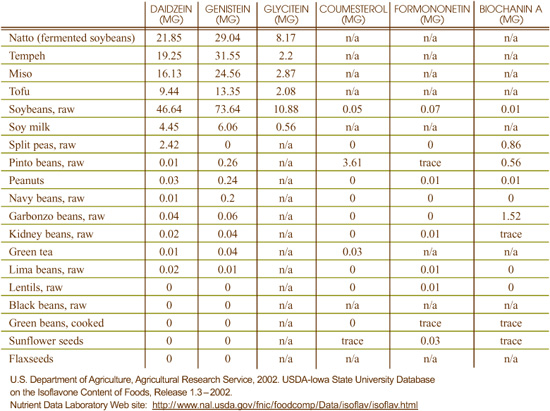
The diets of many traditional cultures throughout the world, including those of Asia and the Mediterranean region, feature plant-based foods rich in unique nutrients known as phytoestrogens. Isoflavones and lignans are the two best-studied groups of phytoestrogenic phytonutrients.
In Asia, the prominent phytoestrogens are the isoflavones found in soy foods such as soybeans, tofu, tempeh and miso as well as the lignans found in the sea vegetables. In the Mediterranean region, these isoflavone and lignan phytoestrogens are supplied by numerous foods including the legumes, seeds and vegetables that make up a significant portion of the traditional diet. Researchers suggest that phytoestrogenic nutrients help to explain part of the reason that these diets are associated with a reduced risk of certain diseases.
The term phytoestrogen reflects the ability of these plant (“phyto”) compounds to act as weak estrogenic compounds, helping to balance hormonal levels in the body. Phytoestrogens are structurally similar to the mammalian estrogen hormone, estradiol, and can bind to estrogen receptors in the body; yet, they are thought of as having weak estrogenic activity, exhibiting only a fraction of that of estradiol. Phytoestrogens may help to balance estrogen levels, with the ability to either exert estrogenic activity if body levels of estrogen are low or anti-estrogenic activity if body levels are high.
Dietary phytoestrogen intake has been associated with reduced risk of various diseases including breast and prostate cancer. They are also suggested to be of benefit to women during times when they are experiencing fluctuating estrogen levels, such as during menopause.
Like all foods, those containing phytoestrogens are not “magic bullets” and need to be incorporated into a person’s overall meal plan in a balanced and logical way. I believe that they need to be eaten in moderation like all foods.
While both isoflavones and lignans act as phytoestrogens, they each have unique properties and for most people, a healthy diet should include food sources of both. How much a person should eat would depend upon their unique health needs, but if we look at the research we can find some general recommendations.
Currently, no public health organizations in the U.S. have issued recommended daily intake levels for phytoestrogens or lignans. In Japan, a culture where the benefits of soyfoods, the most concentrated dietary source of isoflavones, have been well studied, the average intake was 50–70 total grams per day in 1995. This would translate into 2 ounces per day, an amount that is by no means daunting (the soyfoods need not be eaten every day to gain benefit as you could use 14 ounces per week as a dietary goal as well). While studies have shown therapeutic benefits of flaxseeds at ranges from 10–50 grams, most healthcare practitioners recommend 1–2 tablespoons of ground flaxseed daily for general wellness.
In addition to food sources of phytoestrogens, there are herbs that are concentrated in these important phytonutrients, and which are used by many women while they move through menopause. These herbs include red clover and black cohosh*.
The chart on the previous page reflects the World’s Healthiest Foods most concentrated in isoflavones. Daidzein and genistein are the most studied in terms of their phytoestrogenic properties. Glycetein, coumesterol, formononetin and biochanin A are also important isoflavones with health-promoting properties.
The chart on this page reflects the World’s Healthiest Foods most concentrated in phytoestrogenic lignans. These lignans include secoisolariciresinol, maitiresinol and pinoresinol. They are converted in the body into the enterolignans-enterolactone and enterodiol, which act as weak estrogens to help balance the body’s hormonal level (enterolignans are also known as mammalian lignans). Currently, the most thorough examination of the lignan content of foods has been to measure the amount of enterolignans into which they are converted.
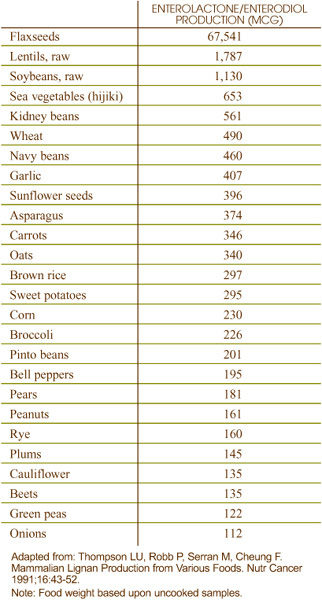
Best Sources of Potassium from the World’s Healthiest Foods
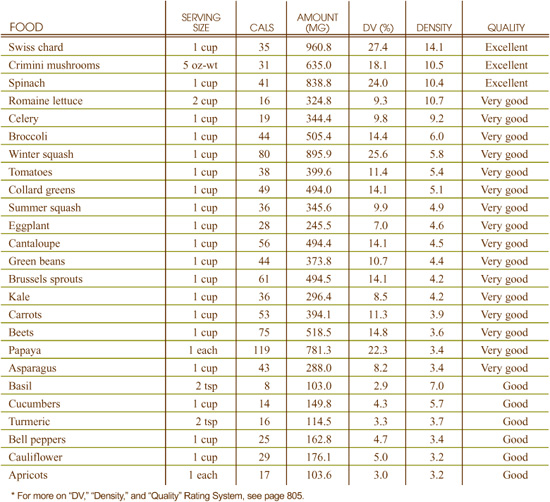
What can potassium-rich foods do for you?
• Help your muscles and nerves function properly
• Help lower your risk of high blood pressure
• Maintain the proper electrolyte and acid-base balance in your body
• Help maintain calcium levels
What events can indicate a need for more potassium-rich foods?
• Muscle weakness
• Confusion
• Irritability
• Fatigue
• Heart problems
• Chronic diarrhea
• Regular, intense exercise
• Use of certain diuretics
Potassium losses from cooking of high-potassium foods can be significant. In the case of spinach, for example, potassium levels have been shown to drop 56% after blanching for several minutes.
Sometimes this passage of potassium out of foods can be nutritionally beneficial. For example, parsley tea often contains significant amounts of potassium because this mineral is leached out of the parsley leaves and into the hot tea water.
In 2004, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for potassium. The recommendations are as follows:
• 0–6 months: 400 mg
• 6–12 months: 700 mg
• 1–3 years: 3,500 mg
• 4–8 years: 3,800 mg
• 9–18 years: 4,500 mg
• 14–18 years: 4,700 mg
• 19+ years: 4,700 mg
• Pregnant women: 4,700 mg
• Lactating women: 5,100 mg
The FDA has set the Reference Value for Nutrition Labeling for potassium at 3,500 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for potassium that may appear on food labels.
Details on potassium’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Potassium?”
Potassium plays a critically important role in health. It is an electrolyte, which means that it conducts electricity when dissolved in water. Since the body is mostly water and many physiological functions are “sparked” by this energy potential, potassium fulfills many important roles. The balance between potassium and another electrolyte, sodium, is extremely important for maintaining cellular health. The overconsumption of sodium in our diets is just another reason supporting the need to consume potassium-rich foods, an easy recommendation to follow if your diet is rich in the World’s Healthiest Foods since fruits and vegetables are very concentrated sources of potassium.
Potassium is especially important in the activity of muscles and nerves. The degree to which our muscles contract and our nerves become excitable both depend heavily on the presence of potassium in the right amount.
Potassium’s ability to decrease calcium excretion is yet another reason for the importance of potassium-rich foods. Since many factors in the modern diet (including excess protein and caffeine consumption) increase calcium excretion, consuming potassium-rich fruits and vegetables may be helpful in maintaining the density and strength of your bones.
Eating foods rich in potassium enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with potassium, supporting its physiological function in your body and therefore contributing to your optimal health.
Potassium plays an important role in muscle contraction and nerve transmission. Many of our muscle and nerve cells have specialized channels for moving potassium in and out of the cell. Sometimes potassium moves freely in and out, and sometimes a special energy-driven pump is required. When the movement of potassium is blocked, or when potassium is deficient in the diet, activity of both muscles and nerves can become compromised.
Potassium is involved in the storage of carbohydrates for use by muscles as fuel. It is also important in maintaining the body’s proper electrolyte and acid-base (pH) balance. Potassium may also counteract the increased urinary calcium loss caused by the high-salt diets typical of many people, thus helping to prevent bones from thinning out at an increased rate.
In addition to poor dietary intake, overuse of muscles, as might occur in excessive physical activity, is a factor that can increase a person’s need for potassium. Any events that draw excessive fluid out of the body—including excessive sweating, diarrhea, overuse of diuretics (including caffeine-containing beverages), poor water intake, or adherence to a ketogenic diet—can increase the need for potassium.
Since potassium functions in close cooperation with sodium, imbalanced intake of salt (sodium chloride) can also increase a person’s need for potassium. Higher amounts of potassium are also needed by persons with high blood pressure.
Since potassium occurs naturally in a wide variety of foods, dietary deficiency of potassium is uncommon. However, if you experience excessive fluid loss through vomiting, diarrhea or sweating, or if you take certain medications, you may be at risk for potassium deficiency.
In addition, a diet that is high in sodium and low in potassium can negatively impact potassium status. The typical American diet, which is high in sodium-containing processed foods and low in fruits and vegetables, contains about two times more sodium than potassium; many health experts recommend taking in at least five times more potassium than sodium.
The symptoms of potassium deficiency include muscle weakness, confusion, irritability, fatigue, and heart disturbances. Athletes with low potassium stores may tire more easily during exercise, as potassium deficiency causes a decrease in the storage of glycogen, the fuel used by exercising muscles.
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for potassium. They noted that there have been no documented adverse effects of excessive consumption of potassium from food sources alone. They did note, however, that adverse effects have been documented for excess potassium from dietary supplements and salt substitutes, notably for those with kidney disease or diabetes.
Best Sources of Protein from the World’s Healthiest Foods
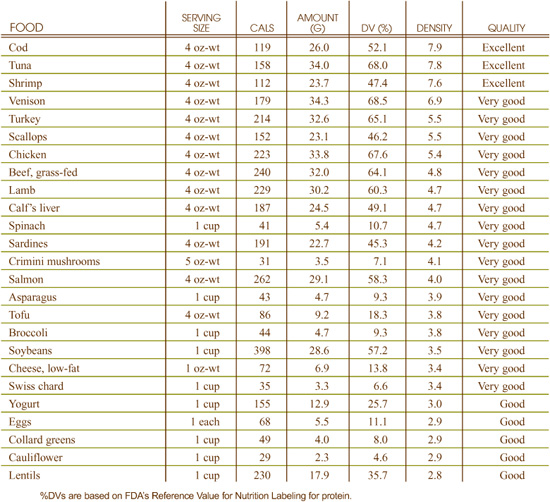
What can protein-rich foods do for you?
• Keep your immune system functioning properly
• Maintain healthy skin, hair and nails
• Help your body produce enzymes
What events can indicate a need for more protein-rich foods?
• Weight loss; muscle wasting
• Fatigue and weakness
• Frequent infections
• Slow growth and development in children
Overcooking foods containing protein can destroy heat sensitive amino acids (for example, lysine) or make the protein resistant to digestive enzymes.
In 2002, the Institute of Medicine at the National Academy of Sciences set Adequate Intake (AI) levels for infants 0–6 months of age and Recommended Dietary Allowances (RDAs) for protein for all age groups 7 months and older. The recommendations are as follows:
• 0–6 months: 9.1 g
• 6 months to 1 year: 13.5 g
• 1–3 years: 13 g
• 4–8 years: 19 g
• 9–13 years: 34 g
• Males 14–18 years: 52 g
• Males 19+ years: 56 g
• Females 14+ years: 46 g
• Pregnant and lactating women: 71 g
The FDA has set the Reference Value for Nutrition Labeling for protein at 50 g. This is the recommended intake value used by the FDA to calculate the %Daily Value for protein that may appear on food labels.
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for protein.
Protein was the first substance to be recognized as a vital part of living tissue. In fact, the word protein comes from the Greek word proteos, which means “primary” or “taking first place,” indicating the importance of this nutrient in the function of the body. Accounting for 20 percent of our body weight, proteins perform a wide variety of functions throughout the body as vital components of body tissues, enzymes, and immune cells.
Proteins are complex molecules comprised of a combination of different amino acids, which are compounds that contain carbon, oxygen, hydrogen, nitrogen and sometimes sulfur. Amino acids link together in specific numbers and unique combinations to make each different protein. Protein is an essential component of the diet because it provides the amino acids that the body needs to synthesize its own proteins.
Proteins can carry certain nutrients (such as iron and vitamin A); therefore, inadequate protein intakemay impair the function of many nutrients.
There are nine essential amino acids that we must receive from our food as our bodies cannot synthesize them on their own. Individual foods were not meant to provide us with a complete set of these essential amino acids, rather they were meant to be combined into diets and cuisines that functioned as a whole to provide all essential amino acids. Therefore, it’s important to eat a wide array of protein-containing foods to ensure you meet the spectrum of your amino acid needs
Protein, providing four calories per gram, is an important source of energy for the body when carbohydrates and fats are not available. The body also uses the amino acids contained in proteins to manufacture its own proteins, including several structural proteins. Examples include myosin, actin, collagen, elastin and keratin: proteins that maintain the strength and integrity of muscles, connective tissues (ligaments and tendons), hair, skin, and nails.
In addition to using protein to generate energy for cellular function whenever necessary and to create structural proteins, the body uses the amino acids contained in proteins to manufacture various other protein-containing molecules that have a wide variety of important functions in the body. These include: enzymes that catalyze chemical reactions in the body; hormones involved in blood sugar regulation and thyroid hormone synthesis; transport proteins such as hemoglobin (carries oxygen) and transferrin (carries iron); lipoproteins that participate in the transportation of fat and cholesterol; antibodies, which play an important role in the immune system; and compounds that participate in the maintenance of proper fluid balance and acid-base balance.
Protein digestion and metabolism involves hydrochloric acid secreted by the stomach and enzymes synthesized by the pancreas. Additionally, the liver controls amino acid metabolism. Therefore any condition that compromises the function of any of these three organs can negatively impact protein status. In addition, the ability of the body to manufacture non-essential amino acids may be hampered with inadequate intake of vitamin B6.
Both adults and children can live healthfully on a low intake of protein, assuming they eat a sufficient amount of calories and all of the essential amino acids are present in the diet. For example, it would be possible to consume less than the RDA amount of protein while getting sufficient levels of amino acids if an excellent balance of high-quality, protein-containing foods was consumed. This type of balance would usually contain fish, nuts, seeds, and legumes. Protein intake as much as 25% under the RDA (in the vicinity of 40 grams per day) might be healthy if an optimal intake of amino acids was maintained and there were no existing health problems. Because affluent cultures often have protein intake above the RDAs, symptoms of protein deficiency are most often seen in impoverished people who have limited access to food. Protein-energy malnutrition, caused by low intake of both protein and calories, is especially common in children in underdeveloped nations, with symptoms including growth retardation and increased susceptibility to infections.
In developed countries, protein-energy malnutrition is most likely to affect people who have suffered severe physical trauma, which increases protein needs (for example, extensive skin burns) or those who have a medical condition or psychological problem that impacts their desire or ability to eat. The elderly are also at risk for protein-energy malnutrition.
Because meat and dairy foods are primary sources of protein in the American diet, many nutritionists caution that those following a vegetarian or vegan diet may be at risk for protein deficiency. However, vegetarians and vegans who eat a variety of vegetables, grains and legumes can easily meet or exceed current protein requirements.
In the case of some chronic health problems, where protein supplies have become overtaxed and depleted, as much as 100 grams of protein per day may be needed to help restore body functions. But in general, excessive intake of protein is ill-advised. Excessive intake of protein over many years may lead to kidney problems and/or accelerated bone loss eventually leading to osteoporosis. Due to a lack of doseresponse relationships at higher levels of protein intake, however, the National Academy of Sciences decided not to set a Tolerable Upper Intake Level (UL) for protein when setting protein standards in 2002.
Best Sources of Selenium from the World’s Healthiest Foods
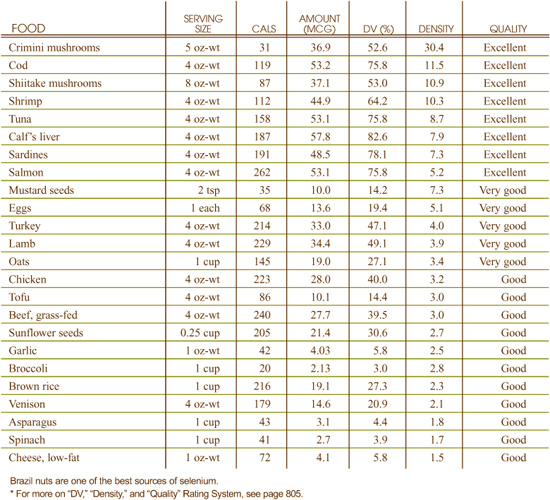
What can selenium-rich foods do for you?
• Protect cells from free radical damage
• Enable thyroid hormone production
• Help lower your risk of joint inflammation
What events can indicate a need for more selenium-rich foods?
• Weakness or pain in the muscles
• Discoloration of the hair or skin
• Whitening of the fingernail beds
Like most minerals, selenium is present in many different forms in food and can vary greatly in its response to cooking and processing. High losses can occur in foods where it is found in water-soluble form and where contact with water during cooking is great. For example, when beans are cooked, 50% of the original selenium may be lost.
Additionally, in 60% extraction wheat, almost 75% of the original selenium is lost. In the case of animal foods, loss of selenium from cooking appears minimal. When a four ounce serving of beef is broiled, for example, virtually none of the selenium is lost.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for selenium for infants up to 1 year old and Recommended Dietary Allowances (RDAs) for all people older than 1 year. The recommendations are as follows:
• 6 months–3 years: 20 mcg
• 4–8 years: 30 mcg
• 9–13 years: 40 mcg
• 14+ years: 55 mcg
• Pregnant females: 60 mcg
• Lactating females: 70 mcg
The FDA has set the Reference Value for Nutrition Labeling for selenium at 70 mcg. This is the recommended intake value used by the FDA to calculate the %Daily Value for selenium that may appear on food labels.
Details on selenium’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Selenium?”
While selenium is considered a micromineral, meaning that it needs to be consumed daily in small amounts, its contribution to health is anything but small. Since it has been found to greatly promote the body’s antioxidant potential, nutrition researchers have been suggesting strong links between this mineral and the prevention of numerous chronic diseases including cancer, heart disease, rheumatoid arthritis and asthma. Therefore, eating selenium-rich foods is an important part of a diet geared at overall wellness promotion.
Eating foods rich in selenium enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with selenium, supporting its physiological function in your body and therefore best contributing to your optimal health.
When oxygen-containing molecules in the body become too reactive, they can start damaging the cell structures around them. In chemistry, this imbalanced situation involving oxygen is called oxidative stress. Selenium helps prevent oxidative stress by working together with a group of nutrients—vitamin B3, vitamin E, vitamin C, and glutathione—to prevent oxygen molecules from becoming too reactive.
In many instances of heart disease, for example, where oxidative stress has been shown to be the source of blood vessel damage, low intake of selenium has been identified as a contributing factor to the disease. Similarly, in rheumatoid arthritis, where oxidative stress damages the area inside and around the joints, dietary deficiency of selenium has been shown to be a contributing cause.
In addition to iodine, selenium is a critical mineral for maintaining proper function of the thyroid gland. In order for the thyroid to produce the most active form of its hormone (triiodothyronine, or T3), selenium is not only essential, but also helps regulate the amount of hormone that is produced.
Accumulated evidence from prospective studies, intervention trials and studies on animal models of cancer has suggested a strong inverse correlation between selenium intake and cancer incidence. Several mechanisms have been suggested to explain the cancer-preventive activities of selenium. Selenium has been shown to induce DNA repair and synthesis in damaged cells, inhibit the proliferation of cancer cells, and induce their apoptosis, the self-destruct sequence the body uses to eliminate worn out or abnormal cells. In addition, selenium is incorporated at the active site of many proteins, including glutathione peroxidase, which is particularly important for cancer protection.
Research suggests that selenium may neutralize mercury toxicity in the body. This potential benefit may be derived by two possible mechanisms: some selenium-containing compounds may directly bind with mercury while others, such as glutathione peroxidase, may combat the oxidative stress created by mercury.
Dietary deficiency is the most common cause of selenium deficiency. Because plant content of selenium is so heavily dependent on the selenium content of the soil, researchers have been able to identify different areas of the world where selenium deficiency is particularly common. In the United States, parts of the Pacific Northwest, parts of the Great Lakes region moving eastward toward the New England states, and parts of the Atlantic Coast have been identified as selenium-deficient regions. Eating foods grown in these areas could contribute to risk of selenium deficiency.
Deficiency symptoms for selenium are difficult to determine and controversial in the research literature. Intake of selenium that is borderline or only mildly deficient has not been connected with specific symptoms in the research literature. With prolonged and severe deficiency, symptoms clearly center around two areas of the body where oxidative stress is known to take its toll: the heart and the joints.
Nausea, vomiting, hair loss, skin lesions, abnormalities in the beds of the fingernail, and fingernail loss can all be symptomatic of selenium toxicity. Levels of selenium necessary to trigger these toxicity symptoms aren’t usually obtained from food, since selenium-rich foods contain about 30–50 micrograms of selenium per serving. (Brazil nuts would be one exception here, since they average about 70–90 micrograms per nut.) Selenium supplementation would be a more likely cause of selenium toxicity than food ingestion.
In light of potential toxicity risks, in 2000 the National Institute of Medicine set the Tolerable Upper Intake Levels (UL) for selenium of 400 mcg per day for men and women 19 years and older.
Best Sources of Tryptophan from the World’s Healthiest Foods
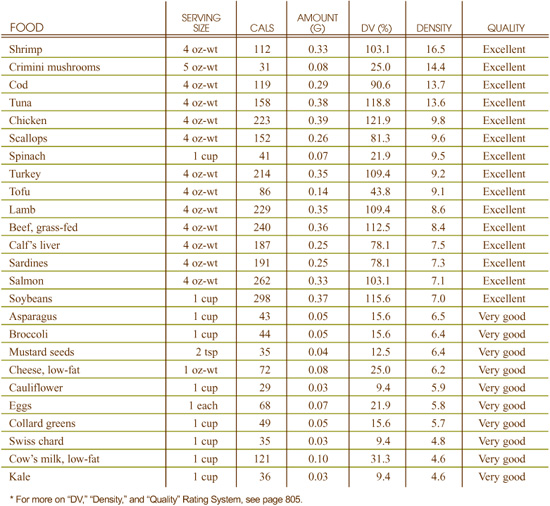
What can tryptophan-rich foods do for you?
• Help regulate your appetite
• Elevate your mood
• Promote better sleep
What events can indicate a need for more tryptophan-rich foods?
• Depression, anxiety
• Impulsiveness
• Inability to concentrate
• Weight gain or unexpected weight loss
• Slow growth in children
• Overeating or carbohydrate cravings
• Poor dream recall
• Insomnia
There is no research showing problematic effects of cooking, storage, or processing on tryptophan levels in food.
In 2002, the Institute of Medicine at the National Academy of Sciences established recommended amino acid patterns for all individuals 1 year of age and older. Tryptophan was recommended at 7 milligrams per gram of protein consumed each day. Since the recommended Daily Value for protein is 50 grams per day, 350 milligrams of tryptophan would represent the current Institute of Medicine’s recommendation when placed in the context of Daily Values. An alternative set of recommendations, based on milligrams of tryptophan consumed per kilogram of body weight, has been developed by the World Health Organization and is structured as follows:
• Infants up to two years: 17 mg/kg
• Children 2–10 years: 12.5 mg/kg
• Children and teens 10–18 years: 3.3 mg/kg
• Adults over 18 years of age: 3.5 mg/kg
Tryptophan is one of the essential amino acids that the body uses to synthesize the proteins it needs. An essential amino acid is one that our bodies cannot manufacture and which we must therefore get from our diets. Tryptophan works in concert with many other nutrients that are necessary for its metabolism, including vitamin B6, vitamin C, folic acid and magnesium. For this reason, it is best to get your daily supply of tryptophan from foods since tryptophan-containing foods typically include these other nutrients as well.
Tryptophan serves as a precursor for serotonin, a neurotransmitter that helps the body regulate appetite, sleep patterns, and mood. Because of its ability to raise serotonin levels, supplemental tryptophan has been used therapeutically in the treatment of a variety of conditions, most notably insomnia, depression, and anxiety.
A small amount of the tryptophan we get in our diet (about 3%) is converted into niacin (vitamin B3) by the liver. This conversion can help prevent the symptoms associated with niacin deficiency when dietary intake of this vitamin is low.
Low dietary intake of tryptophan is the most common cause of deficiency. Dietary deficiency of tryptophan may lead to low levels of serotonin. Low serotonin levels are associated with depression, anxiety, irritability, impatience, impulsiveness, inability to concentrate, weight gain, overeating, carbohydrate cravings, poor dream recall, and insomnia. Additionally, factors such as vitamin B6 deficiency, cigarette smoking, high sugar intake, alcohol abuse, excessive protein consumption, low blood sugar, and diabetes can lead to reduced conversion of tryptophan to serotonin.
Because tryptophan is an essential amino acid, its dietary deficiency may cause the symptoms characteristic of protein deficiency, which include weight loss and impaired growth in infants and children. When accompanied by dietary niacin deficiency, lack of tryptophan in the diet may also cause pellagra, the classic niacin deficiency disease that is characterized by the “4 Ds”—dermatitis, diarrhea, dementia, and death. This condition is very rare in the United States, however, and cannot occur simply because of a tryptophan deficiency.
High dietary intake of tryptophan from food sources is not known to cause any symptoms of toxicity.
Best Sources of Vitamin A from the World’s Healthiest Foods
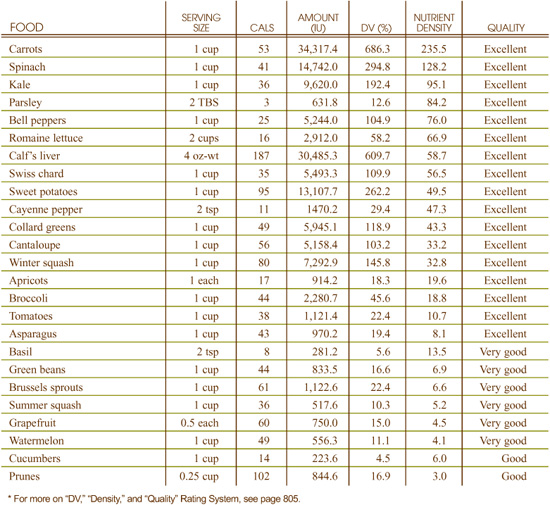
What can vitamin A-rich foods do for you?
• Preserve and improve your eyesight
• Help you fight off viral infections
What events can indicate a need for more vitamin A-rich foods?
• Night blindness
• Frequent viral infections
• Goosebump-like appearance of the skin
Neither cooking nor storage significantly affects the amount or availability of preformed vitamin A in foods.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for vitamin A for infants up to 1 year old, Recommended Dietary Allowances (RDAs) for people older than 1 year old and Estimated Average Requirements (EARs) for pregnant and lactating women. The recommendations are as follows and are given in both International Units (IU) and Retinol Equivalents (RE):
• 0–6 months: 1,333 IU (400 mcg RE)
• 7–12 months: 1,666 IU (500 mcg RE)
• 1–3 years: 1,000 IU (300 mcg RE)
• 4–8 years: 1,333 IU (400 mcg RE)
• 9–13 years: 2,000 IU (600 mcg RE)
• Males 14+ years: 3,000 IU (900 mcg RE)
• Females 14+ years: 2,333 IU (700 mcg RE)
• Pregnant women 18 years or younger: 2,500 IU (750 mcg RE)
• Pregnant women 19 years and older: 2,567 IU (750 mcg RE)
• Lactating women 18 years or younger: 4,000 IU (1,200 mcg RE)
• Lactating women 19 years or older: 4,333 IU (1,300 mcg RE)
The FDA has set the Reference Value for Nutrition Labeling for vitamin A at 5,000 IU. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin A that may appear on food labels.
Details on vitamin A’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Vitamin A?”
Vitamin A, identified in 1913, was the first fat-soluble vitamin to be discovered. Vitamin A is also known as retinol, a name given in reference to the participation of this compound in the functions of the retina of the eye. Vitamin A has also been called the “anti-infective” vitamin due to its role in supporting the activities of the immune system. While retinol, or preformed vitamin A, occurs only in foods of animal origin, some fruits and vegetables contain certain carotenoid phytonutrients—betacarotene, alpha-carotene, and beta-cryptoxan-thin—that the body can convert into vitamin A. These carotenoids are sometimes referred to as “provitamin A,” while retinol is called “preformed vitamin A.” As nutrition researchers continue to forge the strong link between free radicals and disease development, it becomes increasingly important for people wanting to promote optimal health to ensure they consume adequate amounts of vitamin A-rich foods.
Eating foods rich in vitamin A enhances your body’s usage of this important vitamin since these foods naturally contain other nutrients that act in synergy with vitamin A, supporting its physiological function in your body and therefore contributing to your optimal health.
Vitamin A stimulates several immune system activities, possibly by promoting the growth and preventing the shrinkage of the thymus gland. It is known to enhance the function of white blood cells, increase the response of antibodies to antigens, and to have anti-viral activity.
In addition, retinoic acid, one of vitamin A’s metabolically active forms, is needed to maintain the normal structure and function of epithelial and mucosal tissues, which are found in the lungs, trachea, skin, oral cavity, and gastrointestinal tract. These tissues, when healthy and intact, serve as the first line of defense for the immune system, providing a protective barrier that disease-causing microorganisms cannot penetrate.
Vitamin A participates in the synthesis of rhodopsin, a photopigment found in the eye. Rhodopsin plays a fundamental role in the adaptation of the eye to low-light conditions and night vision.
Vitamin A is necessary for normal cell growth and development. Vitamin A is also essential for reproductive processes in both males and females and plays a role in normal bone metabolism. In addition, some of the most cutting-edge research in the field of genetics has been examining the role of vitamin A in regulating genetic events.
Since vitamin A is a fat-soluble vitamin, vitamin A deficiency may be caused by a diet that is extremely low in fat and/or the presence of certain medical conditions. In addition, chronic diarrhea caused by gastrointestinal infections and/or intestinal parasites may contribute to vitamin A deficiency. In addition, exposure to certain toxic chemicals (for example, polybrominated biphenyls and dioxin) enhances the breakdown of vitamin A by the liver. Inadequate intake of protein contributes to vitamin A deficiency.
Vitamin A deficiency primarily affects the health of the skin, hair, eyes, and immune system, although loss of appetite, bone abnormalities, and growth retardation are also associated with inadequate intake of this vitamin. A tell-tale sign of vitamin A deficiency is hyperkeratosis, a goosebump-like appearance of the skin caused by excessive production of keratin (a protein found in skin) that blocks hair follicles. In its initial stages, hyperkeratosis is found on the forearms and thighs, where the skin becomes dry, scaly, and rough. In its advances stages, hyperkeratosis affects the whole body, causing hair loss. Prolonged vitamin A deficiency can lead to night blindness, due to impaired production of rhodopsin, the compound in the retina responsible for detecting small amounts of light.
Toxicity can occur with excessive intakes of preformed vitamin A (not necessarily with carotenoid intake). The dosage needed to attain toxicity is such that it is difficult to attain this level from preformed vitamin A from food alone; rather, toxicity is more likely associated with prolonged intake of high levels of vitamin A supplements or accidental ingestion of extremely high dosages. Those with poor liver function are more likely to experience adverse events from excessive vitamin A intake. The Tolerable Upper Intake Level (UL) for vitamin A established by the Institute of Medicine varies by age group: for those 3 years and younger it is 2,000 IU; 4–8 years, 3,000 IU; 9–14 years, 5,666 IU;15–18 years, 9,332 IU; 19 years and older, 10,000 IU; pregnant or lactating women 18 years or younger, 9,332 IU; and pregnant or lactating women 19 years and older, 10,000 IU.
Best Sources of Vitamin B1 from the World’s Healthiest Foods
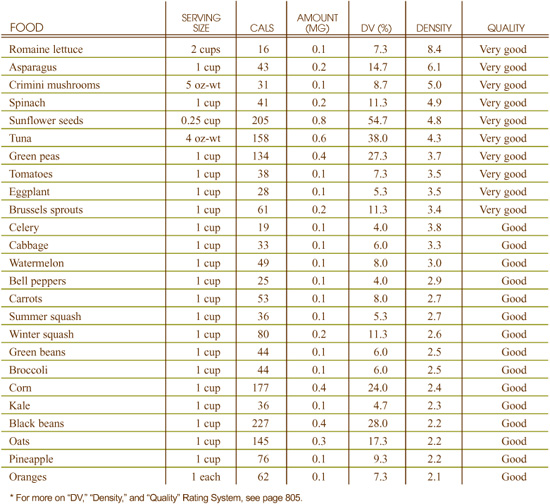
What can vitamin B1-rich foods do for you?
• Maintain your energy supplies
• Coordinate the activity of nerves and muscles
• Support proper heart function
What events can indicate a need for more vitamin B1-rich foods?
• “Pins and needles” sensations
• Feeling of numbness, especially in the legs
• Muscle tenderness, particularly in the calf muscles
• Loss of appetite
Vitamin B1 is highly unstable and easily damaged by heat, pH, and by other chemical substances. Both sulfites and nitrites can inactivate vitamin B1. Processing of grains for use in cereals, and, in particular, heating of processed grain components, can result in the loss of more than half of the grains’ vitamin B1 content.
Long-term (for example, 12 months) refrigeration of vitamin B1-containing foods can also result in substantial loss, on an average of 20-60%.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Recommended Dietary Allowances (RDAs) for vitamin B1 for all individuals 1 year and older. Adequate Intake (AI) levels were established for infants under 1 year of age. These 1998 recommendations are as follows:
• 0–6 months: 200 mcg
• 1–3 years: 500 mcg
• 4–8 years: 600 mcg
• 9–13 years: 900 mcg
• Males 14+ years: 1.2 mg
• Females 14+ years: 1.1 mg
• Pregnant females: 1.4 mg
• Lactating females: 1.5 mg
The FDA has set the Reference Value for Nutrition Labeling for vitamin B1 at 1.5 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin B1 that may appear on food labels.
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for vitamin B1.
Although some vitamin B1 is stored in the body, we need to get a regular supply of it from our diet. No B-complex vitamin is more dependent on its fellow B vitamins than thiamin. Its absorption into the body requires adequate supplies of vitamins B6, B12, and folic acid, which is not a problem since many thiamin-rich foods also contain adequate amounts of these other B vitamins.
Vitamin B1 is traditionally well known for its role in the nutritional deficiency disease, beriberi. Sailing voyages were a common backdrop for the appearance of beriberi, and the addition of whole grains to ships’ rations was found to prevent its occurrence. By 1926, researchers discovered that the preventive substance in whole grains that could also remedy the energy deprivation in the ships’ crews was vitamin B1. Although beriberi is extremely rare in the United States, our understanding of vitamin B1 and its relationship to energy deprivation has carried over into our approach to other health problems in which vitamin B1 deficiency plays a critical role.
Most cells in the body depend on sugar as an energy source. When oxygen is used to help convert sugar into usable energy, the process of energy generation is called aerobic energy production. This process cannot take place without adequate supplies of vitamin B1 since B1 is part of an enzyme system that enables oxygen-based processing of sugar. Because vitamin B1 is so important in energy production, and because food energy is usually measured in terms of calories, vitamin B1 is often prescribed in relationship to caloric intake. For example, recommendations sometimes suggest intake of 0.5 milligrams of vitamin B1 for every 1,000 calories consumed.
Vitamin B1 plays a key role in supporting the nervous system, where it permits healthy development of the fat-like coverings (myelin sheaths) which surround most nerves. In the absence of vitamin B1, these coverings can degenerate or become damaged.
A second type of connection between vitamin B1 and the nervous system involves its role in the production of the messenger molecule acetylcholine. This molecule, called a neurotransmitter, is used by the nervous system to relay messages between the nerves and muscles. Acetylcholine cannot be produced without adequate supplies of vitamin B1. Because acetylcholine is used by the nervous system to ensure proper muscle tone in the heart, deficiency of B1 can also result in compromised heart function.
The leading risk factor for vitamin B1 deficiency in the United States is alcoholism. Heavy users of coffee and tea may also have increased risk of vitamin B1 deficiency since these beverages act as diuretics and remove both water and water-soluble vitamins (like vitamin B1) from the body. Our need for vitamin B1 is also increased by chronic stress, chronic diarrhea, chronic fever, and smoking.
Because of its ability to disrupt the body’s energy production, one of the first symptoms of vitamin B1 deficiency is loss of appetite that reflects the body’s listlessness and malaise. Symptoms related to nerve dysfunction are commonly associated with vitamin B1 deficiency since the myelin sheaths that surround the nerves will not be formed properly without adequate supplies of this nutrient.
These nerve-related symptoms include “pins and needles” sensations or numbness, especially in the legs. Additionally, inability of the nervous system to ensure proper muscle tone in the gastrointestinal tract can lead to indigestion or constipation, and muscle tenderness, particularly in the calf muscles.
Even at extremely high doses, vitamin B1 intake does not appear to carry a risk of toxicity. The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for intake of vitamin B1.
Best Sources of Vitamin B2 from the World’s Healthiest Foods
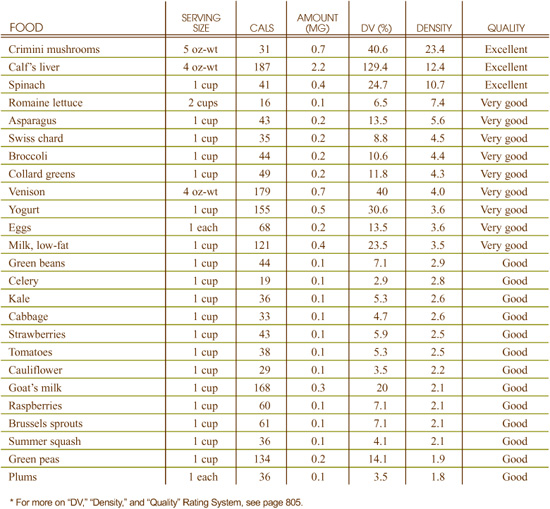
What can vitamin B2-rich foods do for you?
• Help protect cells from oxygen damage
• Support cellular energy production
• Maintain your supply of other B vitamins
What events can indicate a need for more vitamin B2-rich foods?
• Sensitivity to light
• Tearing, burning and itching of the eyes
• Soreness around the lips, mouth, and tongue
• Cracking of the skin at the corners of the mouth
Heat and air do very little damage to vitamin B2, but light is a primary damaging factor for this vitamin. In studies involving the boiling of macaroni noodles, for example, prolonged exposure to light was the critical factor related to loss of vitamin B2. Due to this nutrient’s sensitivity to light, high-vitamin B2-rich foods should be cooked in covered pots whenever possible and stored in opaque containers. Without prolonged exposure to light, loss of vitamin B2 from cooking and storing is typically less than 25%.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Recommended Dietary Allowances (RDAs) for vitamin B2 for all individuals 1 year of age and older. Adequate Intake (AI) levels were established for infants under 1 year of age. The recommendations are as follows:
• 0–6 months: 300 mcg
• 6–12 months: 400 mcg
• 4–8 years: 600 mcg
• 9–13 years: 900 mcg
• Males 14+ years: 1.3 mg
• Females 14–18 years: 1.0 mg
• Females 19+ years: 1.1 mg
• Pregnant females: 1.4 mg
• Lactating females: 1.6 mg
The FDA has set the Reference Value for Nutrition Labeling for vitamin B2 at 1.7 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin B2 that may appear on food labels.
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for vitamin B2 in its 1998 recommendations.
Vitamin B2, also commonly called riboflavin, gets its name from its color. The root of this word is the Latin word flavus meaning “yellow.” When a person’s urine becomes bright yellow following high level supplementation with B-complex vitamins, excess riboflavin excreted in the urine is often responsible for this change in color. Because riboflavin is a component of enzymes that are necessary for everything from energy production to antioxidant status, getting enough from the foods in your diet is important for maintaining optimal health.
Eating foods rich in vitamin B2 enhances your body’s usage of this important vitamin since these foods naturally contain other nutrients that act in synergy with vitamin B2, supporting its physiological function in your body and therefore best contributing to your optimal health.
Vitamin B2, through its conversion to FAD, is involved in the breakdown of homocysteine. Since homocysteine excess is associated with increased risk of cardiovascular disease, maintaining adequate levels of vitamin B2 can be of benefit to heart health.
Glutathione is a protein-like molecule that is responsible for preventing oxygen-based damage to cell membranes, blood vessel linings and joint tissue. Like many antioxidant molecules, glutathione must be constantly recycled. Through its role as a cofactor in the enzyme glutathione reductase, vitamin B2 plays an important role in recycling glutathione back into its active antioxidant form.
Vitamin B2 plays an important role in maintaining supplies of its fellow B vitamins. One of the pathways used in the body to create vitamin B3 (niacin) is by conversion of the amino acid tryptophan. This conversion process is accomplished with the help of an enzyme that requires vitamin B2 to function.
Like vitamin B1, vitamin B2 plays a critical role in the body’s energy production. When active in the body’s energy production pathways, riboflavin typically takes the form of flavin adenine dinucleotide (FAD) or flavin mononucleotide (FMN). When riboflavin is converted into these FAD and FMN forms, it can attach to protein enzymes and allow oxygen-based energy production to occur. Proteins with FAD or FMN attached to them are often referred to as flavoproteins. Flavoproteins are found throughout the body, and particularly in locations where oxygen-based energy production is constantly needed. These locations include the heart and skeletal muscles.
Although not as dramatic as its impact on vitamin B1, alcoholism clearly decreases the availability of vitamin B2 in the body. Heavy exercise has also been shown to increase the need for vitamin B2. Particularly in women training for athletic events, up to 10–15 times the ordinary amount of vitamin B2 may be needed to sustain optimal health. Due to the enrichment of processed grain products, wheat flour remains the primary source of vitamin B2 in the U.S. diet; individuals on specialty diets where carbohydrates like breads, grains, and pastas are avoided may be at special risk for riboflavin deficiency.
Many of the early-stage deficiency symptoms for riboflavin involve eye-related problems. These problems include excessive sensitivity to light, tearing, burning and itching in and around the eyes, and loss of clear vision. Soreness around the lips, mouth, and tongue, and cracking of the skin at the corners of the mouth are symptoms that can also be characteristic of riboflavin deficiency. Peeling of the skin, particularly around the nose, can also indicate lack of vitamin B2.
Toxic side effects from supplemental intake of vitamin B2 (which would be at much higher doses than that found naturally in food) have not been documented in the research literature. Consequently, the Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for vitamin B2.
Best Sources of Vitamin B6 from the World’s Healthiest Foods
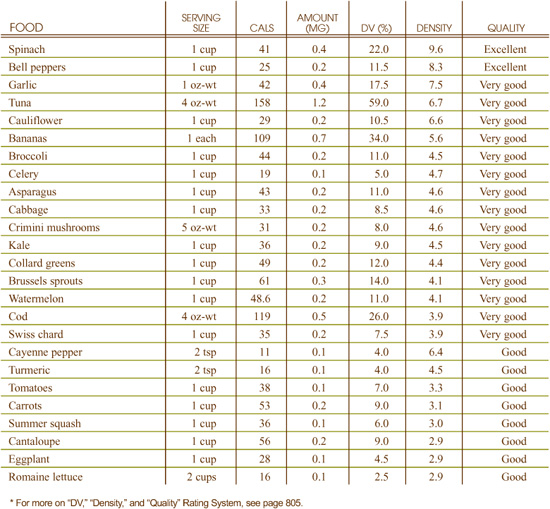
What can vitamin B6-rich foods do for you?
• Support nervous system health
• Promote proper breakdown of sugars and starches
• Help prevent homocysteine build-up in your blood
What events can indicate a need for more vitamin B6-rich foods?
• Fatigue or malaise
• Anemia
• Skin disorders including eczema and seborrheic dermatitis
Large amounts of vitamin B6 are lost during most forms of cooking and processing. Loss of vitamin B6 from canning of vegetables is approximately 60–80%; from canning of fruits, about 38%; from freezing of fruits, about 15%; from conversion of grains to grain products, between 50–95%; and from conversion of fresh meat to meat by-products, 50–75%. When food is heated, the more acidic the food, the poorer the vitamin B6 retention.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Recommended Dietary Allowances (RDAs) for vitamin B6. The recommendations are as follows:
• 0–6 months: 100 mcg
• 6–12 months: 300 mcg
• 1–3 years: 500 mcg
• 4–8 years: 600 mcg
• 9–13 years: 1.0 mg
• Females 14–50 years: 1.2 mg
• Males 51 years and older: 1.7 mg
• Females 51 years and older: 1.5 mg
• Pregnant females: 1.9 mg
• Lactating females: 2.0 mg
The FDA has set the Reference Value for Nutrition Labeling for vitamin B6 at 2.0 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin B6 that may appear on food labels.
Details on vitamin B6’s Tolerable Upper Intake Level (UL) are provided under the heading “Can You Consume Too Much Vitamin B6?”
Vitamin B6 is one of the best studied of all B vitamins and has one of the greatest varieties of chemical forms. The forms of this vitamin all begin with the letters “pyr,” and include pyridoxine, pyridoxal, pyridoxamine, pyridoxine phosphate, pyridoxal phosphate, and pyridoxamine phosphate. The vitamin was not originally given this name, however, but was referred to as “antidermatitis factor” since skin inflammation (dermatitis) seemed to increase when foods with B6 were eliminated from the diet. Yet, the importance of vitamin B6 in the diet extends to much more than just its benefits upon the skin; it is involved in numerous physiological functions throughout the body, making it vitally important to optimal health.
Many foods that contain vitamin B6 also contain other B vitamins, which is important since vitamin B6 has key interactions with these other nutrients. For example, vitamins B2 and B3 are both needed to convert B6 into its various chemical forms. Vitamin B6 deficiency can also reduce the body’s absorption of vitamin B12.
The role of vitamin B6 in our nervous system is very broad and involves many aspects of neurological activity. One aspect focuses on the creation of an important group of neurotransmitter messaging molecules called amines, compounds that the nervous system relies on for transmission of messages from one nerve to the next. Amines are often made from protein building blocks called amino acids, and the key nutrient for making this process occur is vitamin B6. Some of the amine-derived neurotransmitters that require vitamin B6 for their production include serotonin, melatonin, epinephrine, norepinephrine, and GABA.
Nucleic acids, which are used in the creation of our DNA genetic material and many amino acids, the building blocks of proteins, require adequate supplies of vitamin B6 for their synthesis. Therefore, it is difficult to find a chemical category of molecules in the body that does not depend in some way on vitamin B6 for its production.
The processing of carbohydrates (sugar and starch) in our body depends on the availability of vitamin B6. This vitamin is particularly important in facilitating the breakdown of glycogen, a special form of starch stored in our muscle cells and to a lesser extent in our liver. Because carbohydrate processing plays such a key role in certain types of athletic events, researchers have looked closely at the role vitamin B6 plays in carbohydrate processing during physical performance.
Through the role it plays in the metabolism of sulfur-containing molecules, vitamin B6 is critical for maintaining hormonal balance and eliminating toxic substances through the liver. It plays a similar role with respect to methyl-containing molecules. Many important chemical events are made possible by methyl group transfer. For example, genes in the body can be switched on and turned off in this way, and cells can use the process to send messages back and forth. Through its involvement with the metabolism of chemical molecules called methyl groups, vitamin B6 also plays a role in ensuring that substances like homocysteine, which can build up excessively in the blood and increase risk of cardiovascular disease, are kept within a healthy range.
In addition to dietary insufficiency, smoking and the use of many prescription medications (including oral contraceptives) can contribute to vitamin B6 deficiency.
Because of its key role in the formation of new cells, vitamin B6 is especially important for healthy function of body tissue that regenerates itself quickly. The skin is exactly this type of tissue, and it is one of the first to show problems when vitamin B6 is deficient. Many skin disorders have been associated with vitamin B6 deficiency, including eczema and seborrheic dermatitis. The critical role of vitamin B6 in the formation of red blood cells means that vitamin B6 deficiency can also result in symptoms of anemia, malaise, and fatigue. The key role of vitamin B6 in the nervous system also results in many nerve-related symptoms when vitamin B6 is deficient. These symptoms can include convulsions and seizures in the case of severe deficiency.
Imbalances in nervous system activity have been shown to result from high levels of supplemental vitamin B6 intake, but not from food intake since the dosages that have been associated with these adverse events are so much higher than can be reached with food sources alone. The Tolerable Upper Intake Level (UL) for vitamin B6 is 100 mg for adults 19 years and older.
Best Sources of Vitamin B12 from the World’s Healthiest Foods
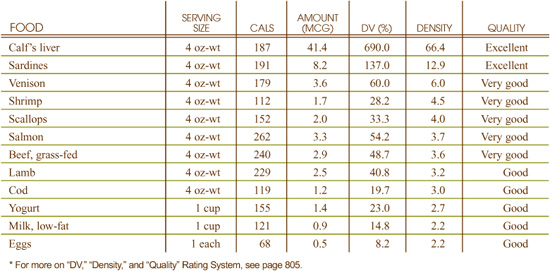
What can vitamin B12-rich foods do for you?
• Support production of red blood cells and prevent anemia
• Allow nerve cells to develop properly
• Help your cells metabolize protein, carbohydrate, and fat
What events can indicate a need for more vitamin B-12-rich foods?
• Depression
• Nervousness
• Memory problems
• Red or sore tongue
• Tingling or numbness in feet
• Heart palpitations
When derived from animal foods, vitamin B12 is fairly well preserved under most cooking conditions. For example, about 70% of the vitamin B12 present in beef is retained after broiling for 45 minutes at 350°F. Similarly, about 70% of vitamin B12 is still present after cow’s milk is boiled for 2–5 minutes. Retention of vitamin B12 in plant-based foods like tempeh, a fermented food made from soy, has not been well researched.
In 1998, the Institute of Medicine at the National Academy of Sciences issued new Recommended Dietary Allowances (RDAs) for vitamin B12 for all individuals 1 year of age and older. Adequate Intake (AI) levels were set for infants under the age of 1 year. The recommendations are as follows:
• 0–6 months: 400 nanograms
• 7–12 months: 500 nanograms
• 1–3 years: 900 nanograms
• 4–8 years: 1.2 mcg
• 9–13 years: 1.8 mcg
• 14+ years: 2.4 mcg
• Pregnant females of any age: 2.6 mcg
• Lactating females of any age: 2.8 mcg
The FDA has set the Reference Value for Nutrition Labeling for vitamin B12 at 6 mcg. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin B12 that may appear on food labels.
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for vitamin B12 when it set its most recent RDAs in 1998.
Vitamin B12 is unusual with respect to its origins. While most vitamins can be made by a wide variety of plants and specific animals, no plant or animal has been shown capable of producing B12, and the exclusive source of this vitamin appears to be tiny microorganisms like bacteria, yeasts, molds, and algae. While its origins may be unusual, vitamin B12’s importance is widespread since this nutrient is so vital to our health, affecting our blood, nervous system, energy level and overall feeling of wellness.
Like most vitamins, B12 can occur in a variety of forms and can take on a variety of names. Names for vitamin B12 include cobamide, cobalamin, hydroxcobalamin, aquocobalamin, nitrotocobalamin, and cyanocobalamin. Each of these designations contains a form of the word “cobalt,” since cobalt is the mineral found in the center of the vitamin.
Eating foods rich in vitamin B12 enhances your body’s usage of this important vitamin since these foods naturally contain other nutrients that act in synergy with vitamin B12, supporting its physiological function in your body and therefore best contributing to your optimal health.
Perhaps the most well known function of vitamin B12 involves its role in the development of red blood cells. As these cells mature, they require information provided by molecules of DNA, the substance in our cells that contains genetic information. Without B12, synthesis of DNA becomes defective, and so does the information needed for red blood cell formation. The cells become oversized and poorly shaped, and begin to function ineffectively, a condition called pernicious anemia. More often than not, pernicious anemia isn’t caused by a lack of vitamin B12 itself, but by a lack of intrinsic factor, a unique protein made in the stomach, upon which vitamin B12 is dependent for its absorption.
A second major function of B12 involves its participation in the development of nerve cells. The myelin sheath—a coating that encloses the nerves—does not form properly whenever B12 is deficient. Additionally, protein, carbohydrates and fats all depend upon vitamin B12 for their proper cycling and movement throughout the body.
Stomach problems can contribute to a vitamin B12 deficiency in two ways. First, irritation and inflammation of the stomach can prevent the stomach cells from functioning properly, which may stop them from producing intrinsic factor. Lack of stomach acids can also lead to B12 deficiency since it is needed to release B12 from protein in food to which it is usually attached.
The ability of a strict vegetarian diet to supply adequate amounts of vitamin B12 remains controversial, despite increasing evidence in support of vegetarianism and its nutritional adequacy. The controversy is fueled by two somewhat divergent schools of thought. One emphasizes the fact that most animals, including humans, are capable of storing long-term supplies of B12, and therefore a daily requirement would be regarded as highly unlikely. The other school of thought, however, points to the unreliability of plants as sources of vitamin B12. Since no plant is capable of making this nutrient, the amount of B12 in plant food depends upon the relationship of the plant to soil and root-level microorganisms that make the vitamin.
Cultured and fermented bean products like tofu, tempeh, miso, and tamari (soy sauce) may or may not contain significant amounts of B12, depending upon the microorganisms used to produce them. The B12 content of sea vegetables also varies according to the distribution of microorganisms in the surrounding sea environment.
Although vitamin B12 is not the only nutrient deficiency that can contribute to occurrence of the following symptoms, its deficiency should be considered as a possible underlying factor whenever any of the symptoms listed below are present: dandruff, nervousness, decreased blood clotting, paleness, depression, fatigue, memory problems, weak pulse, and menstrual problems.
Excessive intake of folic acid can mask B12 deficiency, so individuals at risk for vitamin B12 deficiency who are also taking folic acid in supplement form should consult with their healthcare practitioner.
No toxicity levels have been reported for vitamin B12, and no toxicity symptoms have been identified in scientific research studies. The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for this nutrient.
Q How can you get vitamin B12 without eating meat or other animal products?
A It is definitely more difficult to get vitamin B12 from non-animal sources than many other nutrients. Vegans must pay attention to their intake of vitamin B12 since this vitamin occurs primarily in animal foods, and its deficiency can cause a variety of irreversible neurological problems. A study published in 1999 in the American Journal of Clinical Nutrition involving 245 Australian Seventh-day Adventist ministers evaluated the vitamin B12 status of lacto-ovo vegetarians and vegans who were not taking vitamin B12 supplements. Seventy three percent of the participants had low serum vitamin B12 concentrations.
Interestingly, vitamin B12 cannot be made by animals or plants, but only by microorganisms, like bacteria. When plant foods are fermented with the use of B12-producing bacteria, they end up containing B12. Otherwise, they usually don’t. Sea plants are an exception to the fermented plant rule since they can contain small amounts of B12 from contact with microorganisms in the ocean. Yet, while sea vegetables, algae and fermented foods like tempeh may contain some vitamin B12, they don’t necessarily contain an adequate amount. Therefore, to ensure adequate intake, many people who do not consume any animal-derived foods either look for vitamin B12-fortified foods and/or take vitamin B12 supplements.
Best Sources of Vitamin C from the World’s Healthiest Foods
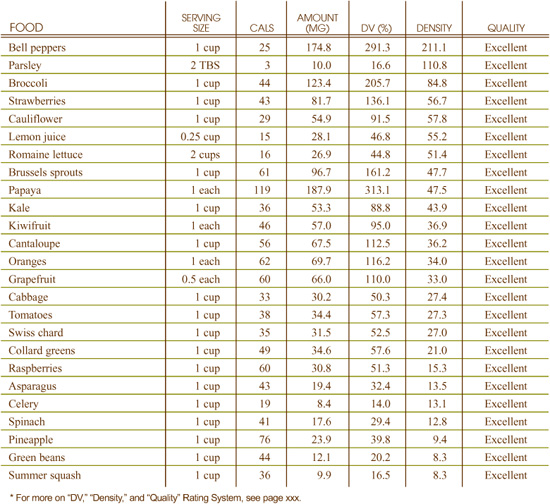
What can vitamin C-rich foods do for you?
• Help protect cells from free radical damage
• Regenerate your vitamin E supplies
• Improve iron absorption
• Lower your cancer risk
What events can indicate a need for more vitamin C-rich foods?
• Poor wound healing
• Frequent colds or infections
• Lung-related problems
Vitamin C is highly sensitive to air, water, and temperature. About 25% of the vitamin C in vegetables can be lost by blanching as well as the freezing and unthawing of vegetables and fruits. Cooking of vegetables and fruits for 10–20 minutes can result in a loss of over 1/2 of the total vitamin C content. When fruits and vegetables are canned and then reheated, only 1/3 of the original vitamin C content may be left. Consumption of vitamin C-rich foods in their fresh, raw form is the best way to maximize vitamin C intake.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for vitamin C for infants up to 1 year old and Recommended Dietary Allowances (RDAs) for all people older than 1 year old. The recommendations are as follows:
• 0–6 months: 40 mg
• 7–12 months: 50 mg
• 1–3 years: 15 mg
• 4–8 years: 25 mg
• 9–13 years: 45 mg
• Males 14–18 years: 75 mg
• Males 19+ years: 90 mg
• Females 14–18 years: 65 mg
• Females 19+ years: 75 mg
• Pregnant females 18 years: 80 mg
• Pregnant females 19+ years: 85 mg
• Lactating females 18 years: 115 mg
• Lactating females 19+ years: 120 mg
The FDA has set the Reference Value for Nutrition Labeling for vitamin C at 60 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin C that may appear on food labels.
The Institute of Medicine established a Tolerable Upper Intake Level (UL) for vitamin C at 2,000 milligrams (2 grams) in 2000.
Vitamin C, also called ascorbic acid, is a water-soluble essential nutrient that we must obtain from our diets. The body has a built-in vitamin C barometer, excreting any excess that is not needed. This nutrient is so critical to living creatures that almost all mammals can use their own cells to make it, although humans cannot synthesize vitamin C.
Humans vary greatly in their vitamin C requirement. It is natural for one person to need 10 times as much vitamin C as another person; and a person’s age and health status can dramatically change his or her need for vitamin C.
Eating foods rich in vitamin C enhances your body’s usage of this important vitamin since these foods naturally contain other nutrients that act in synergy with vitamin C, supporting its physiological function in your body and therefore best contributing to your optimal health.
Vitamin C has important interactions with several key nutrients in the body. Vitamin C can significantly enhance iron uptake and metabolism, even at food-level amounts. Absorption of calcium may be enhanced by vitamin C since calcium ascorbate forms of calcium may be better absorbed than other forms. Excessive intake of vitamin A, for example, is less toxic to the body when vitamin C is readily available. Vitamin C is involved in the regeneration of vitamin E, and these two vitamins appear to work together in their antioxidant effect.
Vitamin C is a primary water-soluble antioxidant in the body, disarming free radicals and preventing damage in the aqueous environment both inside and outside cells. Inside cells, a potential long-term result of excessive free radical damage to DNA is cancer. Especially in areas of the body where cellular turnover is especially rapid, such as the digestive system, preventing DNA mutations translates into preventing cancer. This may be why a good intake of vitamin C is associated with a reduced risk of colon cancer and why cardiovascular diseases, joint diseases and cataracts are all associated with vitamin C deficiency.
Vitamin C, which is also vital for the proper function of a healthy immune system, is good for preventing colds and may be helpful in preventing recurrent ear infections. The immune system relies on a wide variety of mechanisms to help protect the body from infection, including white blood cells, complement proteins, and interferons, and vitamin C is especially important in the function of these immune components.
Poor intake of vitamin C-rich vegetables and fruits is a common contributor to vitamin C deficiency. In the U.S., one third of all adults get less vitamin C from their diet than is recommended by the National Academy of Sciences, and one out of every six adults gets less than half the amount recommended. Smoking and exposure to second hand smoke also increase the risk of vitamin C deficiency.
The body’s immune and detoxification systems make special use of vitamin C and overload in either of these systems can increase risk of deficiency. When the body is exposed to toxins, vitamin C is often required for the body to begin processing the toxins for elimination. Excessive toxic exposure is therefore a risk factor for vitamin C deficiency.
Full-blown symptoms of the vitamin C deficiency disease, scurvy—including bleeding gums and skin discoloration due to ruptured blood vessels—are rare in the U.S. Poor wound healing, however, is not rare, and can be a symptom of vitamin C deficiency. Weak immune function, including susceptibility to colds and other infections, can also be a telltale sign of vitamin C deficiency. Since the lining of our respiratory tract also depends heavily on vitamin C for protection, respiratory infection and other lung-related conditions can also be symptomatic of not getting enough vitamin C.
There are no documented toxicity effects for vitamin C in relation to food and diet. The Tolerable Upper Intake Level (UL) for vitamin C is 2,000 milligrams (2 grams), an amount difficult to achieve through food sources alone.
Best Sources of Vitamin D from the World’s Healthiest Foods
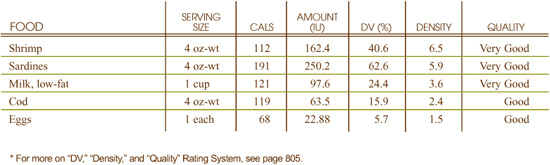
What can vitamin D-rich foods do for you?
• Help keep your bones and teeth strong and healthy
• Regulate the growth and activity of your cells
• Help prevent excessive inflammatory immune-related activity
What events can indicate a need for more vitamin D-rich foods?
• Thinning bones, frequent bone fractures, soft bones
• Bone deformities or growth retardation in children
• Lack of exposure to sunlight
• Being dark-skinned
Vitamin D is a stable compound. Neither cooking nor long-term storage significantly reduce vitamin D levels in food.
In 1997, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for vitamin D. The recommendations are as follows:
• Infants and children: 5 mcg (200 IU)
• Teenagers: 5 mcg (200 IU)
• 19–50 years: 5 mcg (200 IU)
• 51–70 years: 10 mcg (400 IU)
• 70+ years: 15 mcg (600 IU)
• Pregnant and lactating women: 5 mcg (200 IU)
The FDA has set the Reference Value for Nutrition Labeling for vitamin D at 400 IU. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin D that may appear on food labels.
Since the establishment of these vitamin D recommendations in 1997, over 3,000 research studies involving vitamin D have been published in top level science journals. Many of these studies suggest that significantly higher levels of vitamin D may be essential for certain groups of people.
These groups include persons living in more northern geographical areas, for example, residents in the Pacific Northwest or New England; obese persons; persons getting very little sunlight due to indoor jobs or personal habits, including constant use of sunscreen; and persons with naturally darker skin. Individuals in these caregories may require closer to 1000 IU than the 200–600 IU levels listed above.
Recent research suggests that the AI recommendations may be inadequate. Blood levels of no less than 30 ng/ml (nanograms per milliliter) indicate adequate supplies of vitamin D; unless able to receive sufficient sun exposure, most adults need 1,000 IU of vitamin D daily to reach and maintain these levels.
If you are concerned about your vitamin D status, ask your doctor to check your blood levels of 25(OH)D3, which is the major circulating form of vitamin D in the blood. This form of the vitamin is the true barometer of vitamin D status.
Early in the 20th century, scientists discovered that rickets, a childhood disease characterized by improper bone development, could be prevented by a compound isolated from cod liver oil referred to as “fat-soluble factor D,” now known as vitamin D. The vitamin was also called “calciferol,” since it was found to boost calcium deposits in bone. We now know that without adequate vitamin D, our intestines may absorb as little as 1–15% of the calcium in the foods we eat; when our vitamin D supplies are adequate, our intestines absorb 30–80%. Because vitamin D is so important for skeletal growth and strong bones, many foods are fortified with this vitamin to ensure that children obtain adequate amounts.
There are two basic types of vitamin D. Ergosterol is the basic building block of vitamin D in plants. Cholesterol is the basic building block of vitamin D in humans. When ultraviolet light from the sun hits the leaf of a plant, ergosterol is converted into ergocalciferol, or vitamin D2. In just the same way, when ultraviolet light hits the cells of our skin, cholesterol is converted into cholecalciferol, or vitamin D3.
Vitamin D plays a role in maintaining normal blood levels of calcium. As a result, vitamin D impacts the absorption and storage of calcium. Vitamin D also stimulates the absorption of phosphorus. Vitamin D is believed to regulate the production of certain calcium-binding proteins that function in the bones and kidneys. Because these binding proteins are dependent on vitamin K, an interrelationship between vitamin D and vitamin K is also likely.
Eating foods rich in vitamin D enhances your body’s usage of this important vitamin since these foods naturally contain other nutrients that act in synergy with vitamin D, supporting its physiological function in your body and therefore best contributing to your optimal health.
Although typically categorized as a fat-soluble vitamin, vitamin D actually functions more like a hormone than a vitamin. Calcitriol, the most metabolically active form of vitamin D, works with parathyroid hormone (PTH) to maintain proper levels of calcium in the blood. Calcitriol acts to increase the intestinal absorption of calcium, increase the reabsorption of calcium by the kidneys, and stimulate the release of calcium from the bone, thereby increasing blood calcium levels. Alternatively, when blood levels of calcium are high, calcitriol decreases the intestinal absorption of calcium and stimulates the bones to take up calcium, thereby decreasing blood calcium levels.
Through its relationship with calcium metabolism, vitamin D is important for maintaining not only healthy bones, but healthy teeth as well. Studies have found that in men and women over 50 years of age, lack of vitamin D increases risk of periodontal disease.
Vitamin D also helps regulate immune system activity, preventing an excessive or prolonged inflammatory response. Our immune cells, specifically our active T-cells, have receptors for vitamin D. This is important because many autoimmune diseases have a T-cell component of inflammation. Preliminary research suggests that vitamin D’s anti-inflammatory effects may have benefits across a wide spectrum of health conditions including hypertension, type 1 diabetes and psoriasis.
For many years, researchers have known that vitamin D, in the form of calcitriol, participates in the regulation of cell activity. Only recently, however, have studies confirmed the presence of a vitamin D receptor on the membrane of the cell nucleus. Signals throughout the body related to cell multiplication and natural cell death appear to depend on vitamin D. Most minerally-regulated organs, including the bone, kidney, intestine, and parathyroid glands appear to depend on vitamin D availability for their regulation. Because cell cycles play such a key role in the development of cancer, optimal vitamin D intake may turn out to play an important role in prevention and/or treatment of various cancers.
It is important for individuals with limited sun exposure to include good sources of vitamin D in their diets. Homebound individuals, people living in northern latitudes, individuals who use sunscreen and/or wear clothing that completely covers the body, and individuals working in occupations that prevent exposure to sunlight are at risk for vitamin D deficiency. Individuals with dark skin are also at risk for deficiency since their skin contains more melanin pigment, which reduces the skin’s ability to produce vitamin D from sunlight. In addition, since breast milk from vitamin D-deficient mothers may not contain sufficient amounts of this nutrient, exclusively breastfed infants may be a risk for deficiency.
Since vitamin D is a fat-soluble vitamin, a diet that is extremely low in fat and/or the presence of certain medical conditions that cause a reduction in the ability to absorb dietary fat may cause vitamin D deficiency. Under certain circumstances, the conversion of inactive forms of vitamin D to calcitriol is impaired. For example, diseases that affect the parathyroid gland, liver and/or kidney impair the synthesis of the active form of vitamin D. In addition, the production of vitamin D precursors in the skin decreases with age.
Vitamin D deficiency results in decreased absorption of calcium and phosphorus. As a result, prolonged vitamin D deficiency has a negative impact on bone mineralization. In infants and children, such a deficiency manifests itself as rickets, a condition characterized by bone deformities and growth retardation. Adults with vitamin D deficiency may experience bone thinning (osteopenia), bone pain and/or soft bones (osteomalacia).
Excessive dietary intake of vitamin D can be toxic. Toxicity of vitamin D can come from either its plant-based (D2) or animal-based (D3) form. Symptoms of toxicity include loss of appetite, nausea, vomiting, high blood pressure, kidney malfunction, and failure to thrive.
In 1997, the Institute of Medicine set Tolerable Upper Intake Levels (ULs) for vitamin D as follows: infants, 0–12 months, 25 micrograms per day; children and adults, 50 micrograms per day; and pregnant and lactating women, 50 micrograms per day.
Best Sources of Vitamin E from the World’s Healthiest Foods
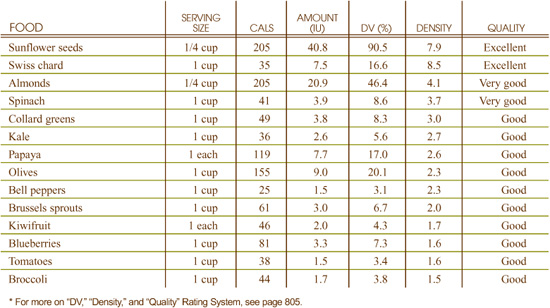
What can vitamin E-rich foods do for you?
• Prevent cell damage from free radicals
• Protect your skin from ultraviolet light
• Allow your cells to communicate effectively
What events can indicate a need for more vitamin E-rich foods?
• Digestive system problems, especially malabsorption
• Tingling or loss of sensation in the arms, hands, legs, or feet
• Liver or gallbladder problems
Exposure to air and factory processing can be particularly damaging to the vitamin E content of food. In wheat, for example, where most of the vitamin E is found in the germ layer, commercial processing removes 50–90% of the food’s vitamin E content. In 60% extraction wheat flour, the alpha-tocopherol content drops almost 90%, and the beta-tocopherol content drops 43%. To help protect their vitamin E content, vegetable oils like olive oil, sunflower seed oil, and peanut oil should be kept in tightly capped containers to avoid unnecessary exposure to air.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for vitamin E for infants up to 1 year old and Recommended Dietary Allowances (RDAs) for all people older than 1 year old. The recommendations are as follows:
• 0–6 months: 4 mg (6 IU)
• 6–12 months: 6 mg (7.5 IU)
• 1–3 years: 6 mg (9 IU)
• 4–8 years: 7 mg (10.5 IU)
• 9–13 years: 11 mg (16.5 IU)
• 14+ years: 15 mg (22.5 IU)
• Pregnant females, 18+ year: 15 mg (22.5 IU)
• Lactating females, 18+ years: 19 mg (28.5 IU)
The FDA has set the Reference Value for Nutrition Labeling for vitamin E at 30mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for vitamin E that may appear on food labels.
The Institute of Medicine established a Tolerable Upper Intake Level (UL) for vitamin E at 1,000 mg (1,500 IU). This daily limit applies to supplemental vitamin E only, and is intended to apply to all individuals age 19 and older.
Even though its name makes it sound like a single substance, vitamin E is actually a family of fat-soluble vitamins that are active throughout the body. Some members of the vitamin E family are called tocopherols. These members include alpha-tocopherol, beta-tocopherol, gamma-tocopherol, and delta-tocopherol. Other members of the vitamin E family are called tocotrienols. These members include alpha-, beta-, gamma-, and delta-tocotrienol. As increasing information has become available about these forms of vitamin E, more and more of them are understood to have unique functions. Unlike most dietary supplements, which typically contain only alpha-tocopherol and often provide a strictly synthetic form of this vitamin E fraction called dl-alpha tocopherol, foods contain the full spectrum of the vitamin E family.
Eating foods rich in vitamin E enhances your body’s usage of this important vitamin since these foods naturally contain other nutrients that act in synergy with vitamin E, supporting its physiological function in your body and therefore best contributing to your optimal health.
Although humans must breathe oxygen to stay alive, oxygen is a risky substance inside the body because it can make molecules overly reactive. When oxygen-containing molecules become too reactive, they can start damaging the cell structures around them. In chemistry, this imbalanced situation involving oxygen is called oxidative stress.
Vitamin E helps prevent oxidative stress by working together with a group of nutrients—vitamin C, vitamin B3, selenium and glutathione—to prevent oxygen molecules from becoming too reactive. Some researchers believe that vitamin E is the most important member of this oxidative stress-preventing group. Oxidative stress has been linked to a host of different chronic diseases including cardiovascular disease, arthritis, asthma, and various cancers.
Vitamin E has sometimes been described as the “lightning rod” of the cell, allowing reactive molecules to strike the cell, like lightning, without causing damage. This “lightning rod” function of vitamin E is particularly apparent in the case of the skin, since vitamin E directly protects the skin from ultraviolet radiation (also called UV light). In numerous research studies, vitamin E applied topically to the skin has been shown to prevent UV damage. When the diet contains vitamin E-rich foods, vitamin E can travel to the skin cell membranes and exert this same protective effect.
While most of the research on vitamin E has focused on its role in prevention of oxidative stress, a variety of new roles have recently been suggested. Most of these new roles involve the transfer of chemical information from one cell to another, or across different structures inside of a cell. This transfer of chemical information is referred to as “cell signaling,” and many researchers believe that cell signaling cannot accurately take place without the help of vitamin E.
Since vitamin E is a fat-soluble vitamin, poor absorption of fat in the digestive tract can contribute to vitamin E deficiency. Some specific health conditions that can cause fat malabsorption include pancreatic disease, celiac disease, and gallbladder disease. Premature birth has also been shown to increase risk of vitamin E deficiency in infants.
Deficiency symptoms for vitamin E are difficult to pinpoint and controversial in the research literature. The area of broadest agreement involves malabsorption. In many research studies, low levels of vitamin E are associated with digestive system problems where nutrients are poorly absorbed from the digestive tract.
A second area of focus for vitamin E deficiency symptoms is called peripheral neuropathy. This area focuses on nervous system problems in the arms, hands, legs, and feet. Pain, tingling, and loss of sensation in these extremities have been associated with vitamin E deficiency. Although many healthcare practitioners report that skin problems appear closely linked to vitamin E deficiency, there are limited human research studies to support this view.
When obtained from food sources alone, vitamin E has no documented research of toxicity. The Institute of Medicine set a Tolerable Upper Intake Level (UL) for vitamin E of 1,000 mg (or 1,500 IU of vitamin E in the form of alpha-tocopherol). This daily limit applies to supplemental vitamin E only and is intended to apply to all individuals age 19 and older.
Best Sources of Vitamin K from the World’s Healthiest Foods
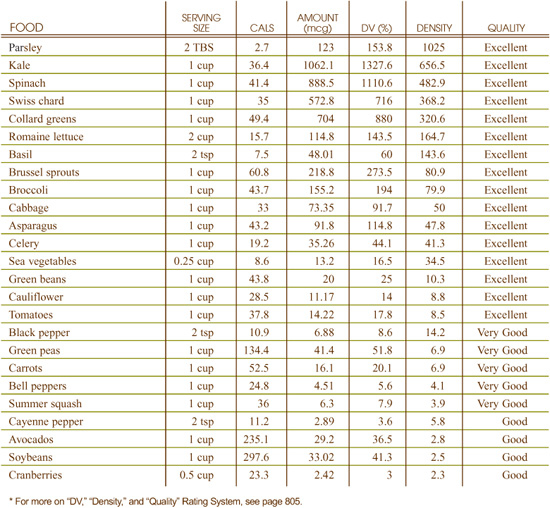
What can vitamin K-rich foods do for you?
• Allow your blood to clot normally
• Help protect against osteoporosis
• Prevent oxidative cell damage
What events can indicate a need for more vitamin K-rich foods?
• Excessive bruising and bleeding
• Digestive system problems, especially malabsorption
• Liver or gallbladder problems
Even though vitamin K is more resilient to processing than many vitamins, fresh foods still offer the highest amounts. Naturally occurring forms of vitamin K exist as oils and are resistant to heat and moisture, but are destroyed by acid, base, oxidizers and light; therefore, little is lost during normal cooking. Foods that are processed into low-fat versions will have less naturally occurring vitamin K, since it has been removed with the other fats. Freezing a food can decrease its vitamin K content. For example, 100 grams of raw spinach has 483 micrograms of vitamin K. One hundred grams of frozen spinach has 377 micrograms, or about 20% less.
In 2000, the Institute of Medicine at the National Academy of Sciences issued new Adequate Intake (AI) levels for vitamin K. The recommendations are as follows:
• 0–6 months: 2 mcg
• 7–12 months: 2.5 mcg
• 4–8 years: 55 mcg
• 9–13 years: 60 mcg
• 14–18 years: 75 mcg
• Males 19+ years: 120 mcg
• Females 19+ years: 90 mcg
• Pregnant and lactating females up to 18 years: 75 mcg
• Pregnant and lactating females 19+ years: 90 mcg
The Institute of Medicine did not establish a Tolerable Upper Intake Level (UL) for vitamin K in its 2000 recommendations.
There are three forms of vitamin K: vitamin K1, also called phylloquinone, is the natural, plant form of this nutrient; vitamin K2, also called menaquinone, is produced by the bacteria in animal and human intestines; and vitamin K3, also called menadione, is the synthetic version. While the three forms are about equally helpful for blood clotting, vitamin K1, the form that only occurs in green plants, is the best form for protecting against osteoporosis. Leafy green vegetables, which are rich sources of vitamin K1, also provide concentrated amounts of other bone-building nutrients, including calcium and boron.
Vitamin K1, the form of the vitamin found in food, helps maintain bone mass because it is used to activate osteocalcin, the major noncollagen protein in bone. Activated osteocalcin anchors calcium molecules inside of the bone. Therefore, without enough vitamin K1, osteocalcin levels are inadequate, so bone mineralization is impaired. Researchers are identifying other ways in which vitamin K aids bone health. For example, vitamin K may both prevent the formation and increase the rate at which osteoclasts, the cells that break down bone, die. Low levels of blood vitamin K have been found to be associated with lower bone mineral density and higher fracture rates with dietary intake of vitamin K associated with reduced risk of hip fractures.
Blood clotting is a vital function in the body that solidifies blood to prevent us from bleeding to death when a blood vessel is damaged either from an external wound or internally. Another benefit of blood clotting is that it secludes the area of an infection or injury and begins the healing process. Vitamin K is required to activate enzymes at many stages in the intricate clotting process called the clotting cascade. Without it, the amount of blood clotting proteins decreases and bleeding time increases. Vitamin K is best known as being required for blood to clot. Interestingly, it is also required to activate several proteins that decrease blood clotting. Thus, research is showing that vitamin K not only helps to initiate blood clotting, but it is also necessary for its complex regulation.
Although humans must breathe oxygen to stay alive, oxygen is a risky substance inside the body because its use can result in the production of free radicals. Unless quickly neutralized by antioxidants, these overly reactive, oxygen-containing molecules can damage the cell structures around them.
When vitamin K is used by an enzyme to alter proteins, it too is altered. This altered vitamin K is then regenerated and reused continuously in what is called the vitamin K cycle. During this cycle, vitamin K functions as an antioxidant, inactivating free radicals that would otherwise damage the delicate fats that are the primary constituents of our cell membranes.
Since vitamin K is a fat-soluble vitamin, poor absorption of fat in the digestive tract can contribute to vitamin K deficiency. Some specific health conditions that can cause fat malabsorption include pancreatic disease, celiac disease, and gallbladder disease. Premature birth has also been shown to increase risk of vitamin K deficiency in infants. Certain medications for heart disease block vitamin K in order to decrease blood clotting and could result in vitamin K deficiency. Anti-coagulant medications, such as Coumadin, are designed to decrease clotting by interfering with vitamin K. (Therefore, eating a diet that is high in vitamin K can make anticoagulant medications less effective. People taking anticoagulant medications, such as Coumadin, should monitor their vitamin K intake and discuss this with their physician.)
Vitamin K deficiency is rare but can cause poor blood coagulation and therefore longer bleeding time. Severe deficiency can lead to fatal anemia. When animals are deprived of vitamin K for long periods of time, they have problems crystallizing bone, and they stop growing taller.
When vitamin K deficiency does occur, it is most likely to happen in newborns, especially if they are premature, breastfed, or their mother was taking anticoagulant medication. Babies are born with sterile intestines; therefore there are no bacteria in their intestines to produce vitamin K2, making them more susceptible to vitamin K deficiency if their diet has inadequate amounts.
Even in high doses, natural forms of vitamin K have not produced symptoms of toxicity. For this reason, the Institute of Medicine at the National Academy of Sciences chose not to set a Tolerable Upper Intake Level (UL) for vitamin K when it revised its public health recommendations for this vitamin in 2000. Consuming more than the body’s needs for dietary vitamin K does not cause the blood to clot excessively in healthy people. However, this does not mean that no potential exists for adverse effects resulting from high intakes.
Best Sources of Zinc from the World’s Healthiest Foods
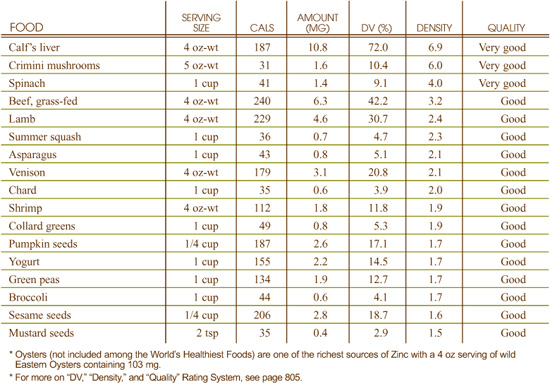
What can zinc-rich foods do for you?
• Help balance blood sugar
• Stabilize your metabolic rate
• Prevent a weakened immune system
• Support an optimal sense of smell and taste
What events can indicate a need for more zinc-rich foods?
• Frequent colds and infections
• Depression
• Impaired sense of taste or smell
• Lack of appetite
• Growth failure in children
Like most minerals, zinc is present in many different forms in food and can vary greatly in its response to cooking and processing. In some foods, where a greater percent of zinc is found in water-soluble form and contact with water is great, high losses of zinc can occur. For example, when navy beans are cooked, 50% of the original zinc is lost.
The processing of wheat is another example of the susceptibility of zinc to substantial loss. In 60% extraction wheat flour—the kind that is used to make over 90% of all breads, baked goods, and pastas sold in the U.S.—almost 75% of the original zinc is lost.
In 1999, the Institute of Medicine at the National Academy of Sciences issued new Recommended Dietary Allowances (RDAs) for zinc. The recommendations are as follows:
• 0–6 months: 2 mg
• 6 months–3 years: 3 mg
• 4–8 years: 5 mg
• 9–13 years: 8 mg
• Males 14+ years: 11 mg
• Females 14–18 years: 9 mg
• Females 19+ years: 8 mg
• Pregnant females 18 years or younger: 12 mg
• Pregnant females, 19+ years: 11 mg
• Lactating females under 18 years: 14 mg
• Lactating females 19+ years: 12 mg
The FDA has set the Reference Value for Nutrition Labeling for zinc at 15 mg. This is the recommended intake value used by the FDA to calculate the %Daily Value for zinc that may appear on food labels.
Details on zinc’s Tolerable Upper Intake Levels (UL) are provided under the heading “Can You Consume Too Much Zinc?”
Eating foods rich in zinc enhances your body’s usage of this important mineral since these foods naturally contain other nutrients that act in synergy with zinc, supporting its physiological function in your body and therefore best contributing to your optimal health.
Zinc is a trace mineral needed in the diet on a daily basis. The first research studies to demonstrate zinc’s importance in the diet focused on the issue of growth. When foods did not supply sufficient amounts of zinc, young men were found to have impaired overall growth as well as impaired sexual maturation. These initial studies on zinc reflected some of the key functions served by this mineral, including regulation of genetic activity, and balance of carbohydrate metabolism and blood sugar.
Many types of immune cells appear to depend upon zinc for optimal function. Particularly in children, researchers have studied the effects of zinc deficiency (and zinc supplementation) on immune response and the number of white blood cells, including specific studies on T lymphocytes, macrophages, and B cells. In these studies, zinc deficiency has been shown to compromise white blood cell numbers and immune response, while zinc supplementation has been shown to restore conditions to normal.
Insulin, a hormone made by the pancreas, is required to move sugar from our bloodstream into our cells. The response of our cells to insulin is called the insulin response. When the foods in our diet do not provide us with enough zinc, our insulin response decreases, and our blood sugar becomes more difficult to stabilize. Metabolic rate—the rate at which we create and use up energy—also depends on zinc for its regulation. When zinc is deficient in our diet, metabolic rate drops (along with hormonal output by our thyroid gland).
Zinc must be linked to gustin, a protein involved in our sense of taste, in order for this sense function to work properly. Because of this relationship between zinc and taste, and because taste and smell are so closely linked in human physiology, impaired sense of taste and smell are common symptoms of zinc deficiency.
Zinc is an important regulator of many genetic activities. Zinc is essential for reading genetic instructions, and when diets do not contain foods rich in zinc, instructions can be misread, or not read at all.
In addition to dietary deficiency, problems in the digestive tract can contribute to zinc deficiency. These problems include irritable and inflammatory bowel disorders, as well as insufficient output of digestive enzymes by the pancreas, which results in impaired digestion of food. Protein deficiency, and specifically deficiency of the amino acid cysteine, can also contribute to zinc deficiency by preventing synthesis of transport and storage molecules that are used to shuttle and store zinc in the body. Loss of zinc through chronic diarrhea or profuse sweating (as might occur with heavy physical labor or athletic training) can also contribute to deficiency of this trace mineral.
Because of the link between zinc and the taste-related protein called gustin, impaired sense of taste and/or smell are common symptoms of zinc deficiency. Depression, lack of appetite, growth failure in children, and frequent colds and infections can also be symptomatic of insufficient dietary zinc.
Zinc toxicity has been reported in the research literature, and in 2000 the Institute of Medicine set Tolerable Upper Intake Level (UL) of 40 milligrams for daily intake of zinc for all individuals age 19 and over. This amount is difficult, but possible, to attain from food sources alone. A metallic, bitter taste in the mouth can be indicative of zinc toxicity, as can stomach pain, nausea, vomiting, and cramps.