

In Chapter 1 we discussed how diabetics and nondiabetics might react to a particular meal. Here we’ll talk about how specific kinds of foods can affect your blood sugar.
A curious fact about diet, nutrition, and medication is that while we can make accurate generalizations about how most of us will react to a particular diet or medical regimen, we cannot predict exactly how each individual will react to a given food or medication—but we can find out by trial and error.
The foods we consume, once you take away the water and indigestible contents, can be grouped into three major categories that provide calories or energy: protein, fat, and carbohydrate. (Alcohol also provides calories, and will be discussed later in this chapter.) Seldom will food from one of these groups contain solely one type of nutrient. Protein foods often contain fat; carbohydrate foods frequently contain some protein and some fat. The common foods that are virtually 100 percent fat are oils, butter, some types of margarine, and lard.
Since our principal concern here is blood sugar control, we’ll concentrate on how these three major sources of calories affect blood sugar. If you’re a long-standing diabetic and have followed standard ADA teachings for years, you’ll find that much of what you’re about to read is radically at odds with the ADA’s dietary guidelines—and with good reason, as you’ll soon learn.
When we eat, the digestive process breaks down the three major food groups into their building blocks. These building blocks are then absorbed into the bloodstream and reassembled into the various products our bodies need in order to function.

Proteins are constructed of building blocks called amino acids. Through digestion, dietary proteins are broken down by enzymes in the digestive tract into their amino acid components. These amino acids can then be reassembled not only into muscle, nerves, and vital organs, but also into hormones, enzymes, and neurochemicals. They can also be converted to glucose, but very slowly and inefficiently.
We acquire dietary protein from a number of sources, but the foods that are richest in it—egg whites, cheese, and meat (including fish and fowl)—contain virtually no carbohydrate. Protein is available in smaller amounts from vegetable sources such as legumes (beans), seeds, and nuts, which also contain fat and carbohydrate.*
Protein and carbohydrate are our two dietary sources of blood sugar. Protein foods from animal sources are only about 20 percent protein by weight (about 6 grams per ounce), the rest being fat, water, and/or indigestible “gristle.” Our liver (and to a lesser degree, our kidneys and intestines), instructed by the hormone glucagon,† can very slowly transform as much as 36 percent of these 6 grams per ounce into glucose‡—if blood sugar descends too low, if serum insulin levels are inadequate, or if the body’s other amino acid needs have been met. Neither carbohydrate nor fat can be transformed into protein.
In many respects—and going against the grain of a number of the medical establishment’s accepted notions about diabetics and protein—protein will become the most important part of your diet if you are going to control blood sugars, just as it was for our hunter-gatherer ancestors.
If you are a long-standing diabetic and are frustrated with the care you’ve received over the years, you have probably been conditioned to think that protein is more of a poison than sugar and is the cause of kidney disease. I was conditioned the same way—many years ago, as I mentioned, I had laboratory evidence of advanced proteinuria, signifying potentially fatal kidney disease—but in this case, the conventional wisdom is just a myth.
Nondiabetics who eat a lot of protein don’t get diabetic kidney disease. Diabetics with normal blood sugars don’t get diabetic kidney disease. High levels of dietary protein do not cause kidney disease in diabetics or anyone else. There is no higher incidence of kidney disease in the cattle-growing states of the United States, where many people eat beef at virtually every meal, than there is in the states where beef is more expensive and consumed to a much lesser degree. Similarly, the incidence of kidney disease in vegetarians is the same as the incidence of kidney disease in nonvegetarians. It is the high blood sugar levels that are unique to diabetes, and to a much lesser degree the high levels of insulin required to cover high carbohydrate consumption (causing hypertension), that cause the complications associated with diabetes.*

Call it the Big Fat Lie. Fat has, through no real fault of its own, become the great demon of the American dietary scene. It is no myth that more than half of Americans are overweight, and the number of obese Americans is growing.
Current dietary recommendations from the government, and nearly every “reputable” organization with an opinion, are to eat no more than 35 percent of calories as fat—which very few people can maintain—and there are some recommendations for even lower percentages than that. The low-fat mania in our culture has spawned an increase in carbohydrate intake. All a candy or cookie has needed is the label “fat-free” to send its sales through the roof. The fallacy that eating fat will make you fat is about as scientifically logical as saying that eating tomatoes will turn you red.
This is the kind of fallacious thinking behind the prevailing “wisdom,” which maintains that there is an unavoidable link between dietary fat and high serum cholesterol. And that if you want to lose weight and reduce cholesterol, all you need to do is eat lots of carbohydrate, limit consumption of meat, and cut out fat as much as possible. But many contemporary researchers exploring this phenomenon have begun to arrive at the conclusion that a high-carbohydrate diet, especially rich in fruit and grain products, is not so benign. In fact, it has been shown—and it is my own observation in myself and in my patients—that such a diet can increase body weight, increase blood insulin levels, and raise most cardiac risk factors.
In an unbiased, clearheaded, and award-winning article published in the respected journal Science on March 30, 2001, the science writer Gary Taubes explores what he calls “The Soft Science of Dietary Fat.” (The full text of this article is available at www.diabetes-book.com/articles/ssdf.shtml.) Taubes cites the failure of the antifat crusade to improve the health of Americans:
Since the early 1970s, for instance, Americans’ average fat intake has dropped from over 40% of total calories to 34%; average serum cholesterol levels have dropped as well….
Meanwhile, obesity in America, which remained constant from the early 1960s through 1980, has surged upward since then—from 14% of the population to over 22%. Diabetes has increased apace. Both obesity and diabetes increase heart disease risk, which could explain why heart disease incidence is not decreasing. That this obesity epidemic occurred just as the government began bombarding Americans with the low-fat message suggests the possibility… that low-fat diets might have unintended consequences—among them, weight gain. “Most of us would have predicted that if we can get the population to change its fat intake, with its dense calories,* we would see a reduction in weight,” admits [Bill] Harlan [of the NIH]. “Instead, we see the exact opposite.”
I urge you to have a look at Taubes’s article, which will give you a notion of the kinds of competing personal, economic, and political interests that go into the formulation of “scientific” guidelines. You might also give your physician a copy of Taubes’s book Why We Get Fat (Knopf, 2010), which is available at Amazon.com.
According to the NIH, the National Health and Nutrition Examination Survey (NHANES) for 2003–2006 and 2007–2008 showed that more than two-thirds (68 percent) of Americans are overweight and more than a third (33.8 percent) are obese. NHANES also showed that 12.5 percent of children ages two to five and 17 percent of those ages six to eleven are overweight, and nearly 18 percent of adolescents ages twelve to nineteen are overweight.
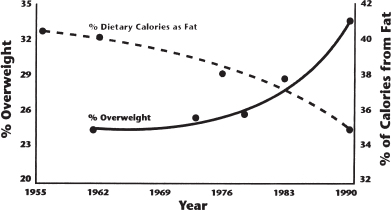
Fig. 9-1. From 1955 to 1990, even as the percentage of calories consumed as fat declined, the percentage of overweight Americans increased by nearly half.
The advent of our agricultural society is comparatively recent in evolutionary terms—that is, it began only about ten thousand years ago. For the millions of years that preceded the constant availability of grain and the more recent year-round availability of a variety of fruits and vegetables, our ancestors were hunters and ate what was available to them in the immediate environment, primarily meat, fish, some fowl, reptiles, and insects—food that was present year-round, and predominantly protein and fat. In warm weather, some may have eaten fruits, nuts, and berries that were available locally in some regions and not deliberately bred for sweetness (agriculture didn’t exist). If they stored fat in their bodies during warm periods, much of that fat was burned up during the winter. Although for the past two centuries, fruit, grain, and vegetables have, in one form or another, been available to us in this country year-round, our collective food supply has historically been interrupted often by famine—in some cultures more than others. The history of the planet as best as we can determine is one of feast (rarely) and famine, and suggests that famine will strike again and again as it has in the past few decades in a variety of places.
Curiously, what today seems in our society to be a genetic predisposition toward obesity functioned during the famines of prehistory as an effective method of survival. Ironically, the ancestors of those who today are most at risk for type 2 diabetes were, during prehistory, not the sick and dying, but the survivors. If famine struck today in the United States, guess who would survive most easily? The same people who are most at risk for type 2 diabetes. For those living in a harsh environment where the availability of food is uncertain, bodies that store fat most efficiently when food is available (for example, by being insulin-resistant and craving carbohydrate, like most type 2 diabetics) survive to reproduce.
If you give it some thought, it makes perfect sense: If a farmer wants to fatten up his pigs or cows, he doesn’t feed them meat or butter and eggs, he feeds them grain. If you want to fatten yourself up, just start loading up on bread, pasta, potatoes, cake, cereal, and cookies—all high-carbohydrate foods. If you want to hasten the fattening process, consume dietary fat with your carbohydrate. Indeed, two studies showed that dietary fat, when consumed as part of a high-carbohydrate diet, was converted to body fat. Fat consumed as part of a low-carbohydrate diet was metabolized, or burned off.
The primary source of body fat for most Americans is not dietary fat but carbohydrate, which is converted to blood sugar and then, with the aid of insulin, to fat by fat cells. Remember, insulin is our main fat-building hormone. Eat a plate of pasta. Your blood sugar will rise and your insulin level (if you have type 2 diabetes or are not diabetic) will also rise in order to cover, or prevent, the jump in blood sugar. All the blood sugar that is not burned as energy or stored as glycogen is turned into fat. So you could, in theory, acquire more body fat from eating a high-carbohydrate “fat-free” dessert than you would from eating a tender steak nicely marbled with fat. Even the fat in the steak is more likely to be stored if it is accompanied by bread, potatoes, corn, and so on.
The fatty-acid building blocks of fats can be metabolized (burned), stored, or converted by your body into other compounds, depending on what it requires. Consequently, fat is always in flux in the body, being stored, appearing in the blood, and being converted to energy. The amount of triglycerides (the storage form of fat) in your bloodstream at any given time will be determined by your heredity, your level of exercise, your blood sugar levels, your diet, your ratio of visceral (abdominal) fat to lean body mass (muscle), and especially your recent consumption of carbohydrate. The slim and fit tend to be very sensitive (i.e., responsive) to insulin and have low serum levels not only of triglycerides but insulin as well. But even their triglyceride levels will increase after a high-carbohydrate meal, as excess blood sugar is converted to fat. The higher the ratio of abdominal fat (and, to a lesser degree, total body fat) to lean body mass, the less sensitive to insulin you’ll tend to be. In the obese, triglycerides tend to be present at high levels in the bloodstream all the time. (This is sometimes exaggerated during weight loss because fat is appearing in the bloodstream as it comes out of storage to be converted into energy.) Not only are high triglyceride levels a direct cause of insulin resistance, but they also contribute to fatty deposits on the walls of your blood vessels (atherosclerosis). Research demonstrates that if high concentrations of triglycerides or fatty acids are injected into the blood supply of the liver of a well-conditioned athlete, someone very sensitive to insulin, she will become temporarily insulin-resistant. (The most important thing to note here is that insulin resistance, as well as other risk factors for diabetic complications, can be reversed by eating less carbohydrate, normalizing blood sugars, and slimming down, which we’ll discuss in greater detail later on.)
If you become overweight, you’ll produce more insulin, become insulin-resistant (which will require you to produce yet more insulin), and become even more overweight because you’ll create more fat and store more fat. You’ll enter the vicious circle depicted in Figure 1-1 (here).
Consider that steak I mentioned earlier. As you know, the body can convert protein to blood sugar, but it does so at a very slow rate, and inefficiently. Serum insulin levels derived from the phase II insulin response or even from insulin injected before a meal may thus be sufficient to prevent a blood sugar rise from protein consumption by itself. Dietary fat cannot be converted to blood sugar, and therefore it doesn’t cause serum insulin levels or requirements for injected insulin to increase.* Say you eat a 6-ounce steak with no carbohydrate side dish—this won’t require much insulin to keep your blood sugar steady, and the lower insulin level will cause only a small amount of the fat to be stored.
Now consider what would happen if you instead ate a “fat-free,” high-carbohydrate dessert with exactly the same number of calories as that steak. Your insulin level will jump dramatically in order to cover the sugar and starches in the dessert. Remember, insulin is the fat-building and fat-storage hormone. Since it’s dessert, you probably won’t be going out to run a marathon after eating, so the largest portion of your newly created blood sugar won’t get burned. Instead much of it will be turned into fat and stored.
Interestingly enough, eating fat with carbohydrate can actually slow the digestion of carbohydrate, so the jump in your blood sugar level might thereby be slowed. This would probably be relatively effective if you’re talking about eating a green salad with vinegar-and-oil dressing. But if you’re eating a regular dessert, or a baked potato with your steak, the slowdown in digestion would not prevent blood sugar elevation in a diabetic.
Despite what the popular media would have us believe, fat is not evil. In fact, many researchers are becoming quite concerned about the dangerous potential of “fat substitutes.” Fat is absolutely necessary for survival. Much of the brain is constructed from fatty acids. Without essential fatty acids—which, like essential amino acids, cannot be manufactured by the body and must be eaten—you would die.
Diabetics are affected disproportionately by diseases such as atherosclerosis. This has led to the long-standing myth that diabetics have abnormal lipid profiles because they eat more fat than nondiabetics.† It was likewise once thought that dietary fat caused all the long-term complications of diabetes. For many years, this was taken as gospel by most in the medical community. In truth, however, the high lipid profiles in many diabetics with uncontrolled blood sugar have nothing to do with the fat they consume. Most diabetics consume very little fat—they’ve been conditioned to fear it. High lipid profiles are a symptom not of excess dietary fat, but of high blood sugars. Indeed, even in most nondiabetics, the consumption of fat has little if anything to do with their lipid profiles.
On the other hand, high consumption of carbohydrate, as we will discuss shortly, can cause “nondiabetics” to develop some of the complications usually associated with diabetes.
When I was on a very low fat, high-carbohydrate diet about forty-five years ago, I had high fasting triglycerides (usually over 250 mg/dl) and high serum cholesterol (usually over 300 mg/dl), and I developed a number of vascular complications. When I went on a very low carbohydrate diet and did not restrict my fat, my lipids plummeted. Now, in my late seventies, I have the lipid profile of an Olympic athlete, apparently from eating a low-carbohydrate diet in order to normalize my blood sugars. That I exercise regularly probably doesn’t hurt my lipid profile, either—but I was also exercising when my lipid profile was abnormal.
Dare your physician. Ask her if her lipid profile on a low-fat diet can remotely compare to mine, on a high-fat, low-carbohydrate diet:
LDL—the “bad” cholesterol—53 (below 100 is considered normal)
HDL—the “good” cholesterol—123 (above 39 is considered normal)
Triglycerides—45 (below 150 is considered normal)
Lipoprotein(a)—undetectable (below 10 is considered normal)
Contrary to popular myth, fat is not a demon. It’s the body’s way of storing energy and maintaining essential organs such as the brain. Without essential fatty acids, your body would cease to function.

I’ve saved carbohydrate for last because it’s the food group that adversely affects blood sugar most profoundly. If you’re like most diabetics—or virtually everyone who lives in an industrialized society—you probably eat a diet that’s mostly carbohydrate. Grains. Fruit. Bread. Cake. Beans. Snack foods. Rice. Potatoes. Pasta. Breakfast cereal. Bagels. Muffins. They look different, but dietarily speaking, they’re essentially the same.
If you are already obese, you know and I know that you crave—and consume—these foods and probably avoid fats. As studies show, you would be better off eating the fat than the carbohydrate. Fat alone will be burned off. A combination of high-carbohydrate foods and fat will foster fat storage.
It is, therefore, a myth that Americans are overweight due to excessive fat consumption. Americans are fat largely because of sugar, starches, and other high-carbohydrate foods.
In a study that looked at the relationship between dietary sugar intake and cardiovascular health, the American Heart Association (AHA) found that Americans on average consume more than 70 pounds of added sugars each year.* This represents an increase during the period 1970–2004 of almost 20 percent. The key word here is “added.” This doesn’t account for starches and sugars naturally present in food. According to a report from the Oregon Health Sciences University, a 12-ounce Starbucks Grande Caramel Mocha drink contains 45 teaspoons of added sugar.
This increase in sugar consumption not coincidentally corresponds with the timing of recommendations to eat less fat. It was 1984 when the National Institutes of Health (NIH) began advising everyone within shouting distance to cut fat intake. It also corresponds quite neatly with the creation of a whole new, multibillion-dollar industry in low-fat and nonfat foods, many of which are extremely high in sugar. For more than fifteen years, the government had planned to issue a report once and for all damning fat as the demon some scientists were sure it was. The problem was, researchers couldn’t “reverse engineer” the actual data to make the science fit the assumption. Unfortunately, the program to indict fat was left to die a quiet death, and not so much as a press release was issued to say, “We were wrong.” And so many of us still don’t know the truth. They guessed wrong.
No doubt the popular media have made you aware of the endless procession of books and diets and advertisements for foods all touting the value of high “complex carbohydrate” in the diet. Athletes “carbo-load” before big games or marathons. TV and radio commercials extol the virtues of Brand X sports drink over Brand Y because it contains more “carbs.” That AHA study showed a strong enough link between elevated triglycerides and “bad cholesterol,” not to mention increased likelihood of overweight and obesity, that it recommended drastic reductions in added sugar intake. I’d say the AHA didn’t go far enough, even if it was the strongest such statement the organization had ever made.
As stunning as it sounds—and unbelievable, given the popular media’s recent love affair with a high “complex carbohydrate,” low-fat diet—you can quite easily survive on a diet in which you eat no carbohydrate. There are essential amino acids and essential fatty acids, but there is no such thing as an essential carbohydrate. Furthermore, by sticking to a diet that contains no carbohydrate but has high levels of fat and protein, you can reduce your cardiac risk profile—serum cholesterol, triglycerides, LDL, et cetera—although you’d deprive yourself of all the supposed “fun foods” that we crave most.* We’ve all been trained to think that carbohydrates are our best, most benign source of food, so how can this be?
What if I, a physician, told you, a diabetic, to eat a diet that consisted of 60 percent sugar equivalents, 20 percent protein, and 20 percent fat? More than likely, you’d think I was insane. I’d think I was insane, and I would never make this suggestion to a diabetic (nor would I even make it to a nondiabetic). But this is just the diet the ADA recommended to diabetics for decades. On the surface, these recommendations seemed to make sense because of kidney disease, heart disease, and our abnormal lipid profiles. But this is what is known as single-avenue thinking. It seemed logical to insist that dietary intake of protein and fat be reduced, because no one had looked at elevated blood sugars and the high levels of insulin necessary to bring them down as the possible culprits.
So if you eat very little fat and protein, what’s left to eat? Carbohydrate.
As I discovered in my years of experimentation on myself, and then in my medical training and practice, the real dietary problem for diabetics is not only fast-acting carbohydrate but also large amounts of any carbohydrate. In either case, the result is high blood sugars requiring large amounts of insulin to try to contain them.
So what are carbohydrates?
The technical answer is that carbohydrates are chains of sugar molecules. The carbohydrates we eat are mostly chains of glucose molecules. The shorter the chain, the sweeter the taste. Some chains are longer and more complicated (hence, “simple” and “complex” carbohydrates), having many links and even branches. But simple or complex, carbohydrates are composed entirely of sugar.
“Sugar?” you might ask, holding up a slice of coarse-ground, seven-grain bread. “This is sugar?”
In a word, yes, at least after you digest it.
With a number of important exceptions, carbohydrates, or foods derived primarily from plant sources that are starches, grains, and fruits, have the same ultimate effect on blood glucose levels that table sugar does. (The ADA has recognized officially that, for example, bread is as fast-acting a carbohydrate as table sugar. But instead of issuing a recommendation against eating bread, its response has been to say that table sugar is therefore okay, and can be “exchanged” for other carbohydrates. To me, this is nonsense.) Whether you eat a piece of the nuttiest whole grain bread, drink a Coke, or have mashed potatoes, the effect on blood glucose levels is essentially the same—blood sugar rises, rapidly, and in proportion to carbohydrate content.
As noted in the introduction to this chapter, the digestion process breaks each of the major food groups down into its basic elements, and these elements are then utilized by the body as needed. The basic element of most carbohydrate foods is glucose. We usually think of simple carbohydrates as sugars and complex carbohydrates as fruits and grains and vegetables. In reality, most fruit and grain products, and some vegetables, are what I prefer to talk about as “fast-acting” carbohydrates. Our saliva and digestive tract contain enzymes that can rapidly chop the chains down into free glucose. We haven’t the enzymes to break down some carbohydrates, such as cellulose, or “indigestible fiber.” Still, our saliva can break starches into the shorter chains on contact and then convert those into pure glucose.
Pasta, which is often made from durum wheat flour and water (but can also be made from plain white flour and egg yolks, or other variants), has been touted as a dream food—particularly for runners carbo-loading before marathons—but it quickly becomes glucose, and can raise blood sugar very rapidly for diabetics.
In the type 2 diabetic with impaired phase I insulin response, it takes hours for the phase II insulin to catch up with the postprandial levels of glucose in the blood, and day after day, during that time, the high blood sugars can wreak havoc. In the diabetic who injects insulin, there is a tremendous amount of (rarely successful) guesswork involved in finding the proper dosage and timing of insulin to cover a carbohydrate-heavy meal, and the injected insulin not only doesn’t work fast enough, it is also highly unpredictable when taken in large doses in attempts to cover large amounts of carbohydrate (see Chapter 7, “The Laws of Small Numbers”).
Some carbohydrate foods, like fruit, contain high levels of simple, fast-acting carbohydrates. Maltose and fructose—malt sugar and fruit sugar—for example, are slower-acting than sucrose—table or cane sugar—but they will cause the same increase in blood sugar levels. It may be the difference between nearly instant elevation and elevation in 2 hours, but the elevation is still high, and a lot of insulin is still required to bring it into line. And, if the insulin is injected, there’s the further problem of guesswork in timing and dosage. Despite the old admonition that an apple a day keeps the doctor away, I haven’t had fruit since 1970, and I am considerably healthier for it. Some whole-plant vegetables—that is, those that come mostly from the stalks and leaves—are of value to the diabetic and nondiabetic alike because they contain considerable amounts of vitamins, minerals, and other nutrients. (The recipe section of this book shows you a number of tasty and satisfying ways to work these vegetables into your diet.)
As noted previously, most Americans who are obese are overweight not because of dietary fat, but because of excessive dietary carbohydrate. Much of this obesity is due to “pigging out” on carbohydrate-rich snack foods or junk foods, or even on supposed healthy foods like whole grain bread and pasta. It’s my belief that this pigging out has little to do with hunger and nothing at all to do with being a pig.
I’m convinced that people who crave carbohydrate have inherited this problem. To some extent, we all have a natural craving for carbohydrate—it makes us feel good. The more people overeat carbohydrates, the more they will become obese, even if they exercise a lot. But certain people have a natural, overwhelming desire for carbohydrate that doesn’t correlate to hunger. These people in all likelihood have a genetic predisposition toward carbohydrate craving, as well as a genetic predisposition toward insulin resistance and diabetes. (See “The Thrifty Genotype,” here.) This craving can be reduced for many by eliminating such foods from the diet and embarking upon a low-carbohydrate diet.
In light of the above, you might guess that I advocate a no-carbohydrate diet. In fact, in the next chapter you’ll discover that I include small amounts of slow-acting carbohydrate in my meal plan. Back in 1970, as I was still experimenting with blood sugar normalization, I remembered that during the twentieth century a new vitamin had been discovered every fifteen years or so. While there may be no such thing as an essential carbohydrate, it seemed reasonable to conclude that, since our prehistoric ancestors consumed some plants, plant foods might well contain essential nutrients that were not yet present in vitamin supplements and had not even been discovered. I therefore added small amounts of low-carbohydrate vegetables (not starchy or sweet) to my personal meal plan. All of a sudden I was eating salads and cooked vegetables instead of the bread, fruit, cereal, skim milk, and pasta that I had been eating on my prior ADA diet. It took a while to get used to salads, but now I relish them. Only recently, in my lifetime, have phytochemicals (essential nutrients found in plant foods) been discovered. Phytochemicals are now incorporated into some vitamin pills, but research on the use of isolated phytochemicals is still in its early stages. You may have heard of such phytochemical supplements as lutein, lycopene, and so on. It would appear that many chemicals—large numbers of which are likely not even known about yet—work together to provide beneficial effects. So at this point, it certainly makes sense to eat low-carbohydrate salads and vegetables. (Although fruits contain the same phytochemicals as vegetables, they are too high in fast-acting carbohydrate to be part of a restricted-carbohydrate diet, as the next chapter will explain.)
Physicians and anyone interested in reading scientific studies that compare low-carb and low-fat diets should visit the archives of the Nutrition and Metabolism Society at http://locarbvslofat.org.

Alcohol can provide calories, or energy, without directly raising blood sugar, but if you’re an insulin-dependent diabetic, you need to be cautious about drinking. Ethyl alcohol, which is the active ingredient in hard liquor, beer, and wine, has no direct effect on blood sugar because the body does not convert it into glucose. In the case of distilled spirits and very dry wine, the alcohol generally isn’t accompanied by enough carbohydrate to affect your blood sugar very much. For example, 100-proof gin has 83 calories per ounce. These extra calories can increase your weight slightly if accompanied by carbohydrate, but not your blood sugar. Different beers—ales, stouts, and lagers—can have varying amounts of carbohydrate, which is slow enough in its action that if you figure it into your meal plan, it may not raise your blood sugar. Mixed drinks and dessert wines can be loaded with sugar, so they’re best avoided. Exceptions would be a dry martini or mixed drinks that can be made with a sugar-free mixer, such as sugar-free tonic water.
Ethyl alcohol, however, can indirectly lower the blood sugars of some diabetics if consumed at the time of a meal. It does this by partially paralyzing the liver and thereby inhibiting gluconeogenesis so that it can’t convert enough protein from the meal into glucose. For the average adult, this appears to be a significant effect with doses greater than 1½ ounces of distilled spirits, or one standard shot glass. If you have two 1½-ounce servings of gin with a meal, your liver’s ability to convert protein into glucose may be impaired. If you’re insulin-dependent and your calculation of how much insulin you’ll require to cover your meal is based on, say, two hot dogs, and those hot dogs don’t get 7.5 percent converted to glucose, the insulin you’ve injected will take your blood sugar too low. You’ll have hypoglycemia, or low blood sugar.
The problem of hypoglycemia itself is a relatively simple matter to correct—you just eat some glucose and your blood sugar will rise. But this gets you into the kind of messy jerking up and down of your blood sugar that can cause problems. It’s best if you can avoid hypo- and hyperglycemia (high blood sugar) entirely.
Another problem with alcohol and hypoglycemia is that if you consume much alcohol, you’ll have symptoms typical of both alcohol intoxication and hypoglycemia—light-headedness, confusion, and slurring of speech. The only way you’ll know the cause of your symptoms is if you’ve been monitoring your blood sugar throughout your meal. This is unlikely. So you could find yourself thinking you’ve consumed too much alcohol when in fact your problem is dangerously low blood sugar. In such a situation, it wouldn’t even occur to you to check your blood sugar. Remember, that early blood sugar–measuring device I got was developed in order to help emergency room staffs tell the difference between unconscious alcoholics and unconscious diabetics. Don’t make yourself an unconscious diabetic. A simple oversight could turn fatal.
Many of the symptoms of alcohol intoxication mimic those of ketoacidosis, or the extreme high blood sugar and ketone buildup in the body that can result in diabetic coma. The great buildup of ketones causes a diabetic’s breath to have an aroma rather like that of someone who’s been drinking. If you don’t die of severe hypoglycemia, then you might easily die of embarrassment when you come to and your friends are aghast and terrified that the emergency squad had to be called to bring you around.
In small amounts, alcohol is relatively harmless—one glass of dry wine or “lite” beer with dinner—but if you’re the type who can’t limit drinking, it’s best to avoid it entirely. For the reasons already discussed, and contrary to the guidelines of the ADA, alcohol can be more benign between meals than it is at meals. One benevolent effect of alcohol is that it can enable some diabetics to consume one “lite” beer or one small Bloody Mary (tomato juice mixed with an ounce and a half of vodka) without raising blood sugar.
I will personally answer questions from readers for one hour every month. This free service is available by visiting www.askdrbernstein.net.