Don’t eat anything your great-grandmother wouldn’t recognize as food.
In my clinic, we’ve tried many different types of nutritional plans for women with PCOS over the years. One thing I’ve learned is that no one diet program works for everyone with PCOS. As we’ve seen by looking intensively at each of the factors involved, we are all unique. So, although I’ll spell the recommended nutritional program out here, there may be some adjustments that you’ll need to make. First of all, I’ll cover what to eat, as well as macronutrients and meal composition, as sometimes it’s a lot harder to know what you should eat, rather than what you shouldn’t. Then, I'll cover what to avoid.
We’ve already talked about insulin resistance in detail, and it’s important to understand that insulin isn’t, in general, a bad thing. Insulin takes sugar from the bloodstream and helps it to enter the cells to be used for energy or to be stored. It’s like a key that opens the lock to our cells.
It also stops glucose from being released by the liver into the bloodstream. We don’t want to view insulin as the enemy. It’s a very important hormone needed for survival. However, for women with PCOS, it’s also something that we know aggravates our condition hormonally.
Numerous studies show that elevated insulin levels are caused by a combination of genetics, obesity, and a variety of other factors. One thing is clear: Being of an increased weight causes large amounts of insulin to be released, creating insulin resistance. There are numerous cultures that consume a lot of carbohydrates, and yet people from these cultures can be of average weight or lean. This occurs because the overall composition of the diet, lifestyle, and genetics support health and leanness. So, I don’t want to give anyone the impression that carbohydrates are in any way “bad.” In this book, we are addressing PCOS, which has its own set of unique nutritional considerations. There is a population of people who are genetically insulin resistant and are predisposed to type 2 diabetes. For these individuals, consuming foods that spike insulin contributes to their pathology of insulin resistance. Those with PCOS are also insulin resistant. High insulin levels aggravate our insulin-sensitive ovaries and cause them to make testosterone, stalling ovulation and blocking the hormonal cycles. When insulin may be very high already, as is the case in insulin-resistant women with PCOS, we certainly don’t want to add fuel to the fire.
First, let’s talk about a few important concepts: the glycemic index, the glycemic load, and the food insulin index. Then we will get to a new concept—what might very well be one of the best new methods for women with PCOS who want to increase insulin sensitivity.
Let’s talk more about carbohydrates now. As PCOS is so closely linked to insulin resistance and diabetes, this is a much talked about subject. We all have heard that we should limit our carbohydrates and keep the foods that we eat lower on the glycemic index. This is true for many women. However, we know so much more now due to new information on insulin and how it works in our bodies that we have to address other factors as well.
The glycemic index, which you’ve probably heard of, is a marker of how quickly a food breaks down into sugar within the bloodstream. It’s the measurement of how much a food with 50 grams of carbohydrates raises blood sugar over two hours, compared to how much 50 grams of glucose would. The closer to 100, the closer to pure sugar. This has been a popular concept in creating a healthy diet for women with PCOS.
Although the glycemic index has been so widely used, I think there are some other factors to consider in finding the best diet for PCOS. The glycemic index only measures blood glucose rise due to the consumption of carbohydrates and doesn’t take into account the effect of any of the other nutrients on our metabolic health, most especially on that of insulin—clearly an important factor for women with PCOS.
Although it’s popularly thought that only carbohydrates cause the secretion of insulin, proteins also cause significant insulin release. So the glycemic index falls short in this area. Other areas that the glycemic index misses are that its measurement is for 50 grams of a food. And as we know, we eat different serving sizes based on the type of food we consume. For example, 50 grams of jellybeans is very different in size than 50 grams of watermelon.
The glycemic load is what accounts for the quantity consumed when referring to the glycemic index. Basically, it’s the amount of food eaten, multiplied by the glycemic index of the food. So our watermelon would have a low glycemic load, whereas jellybeans would have a high glycemic load. Eating very few jellybeans would raise your blood sugar quite a bit. To get the same rise in blood sugar from watermelon, you would need to eat quite a bit of watermelon. To give you an idea of why this is important, consider the following: If you choose a food that is moderate on the glycemic index and you eat a large quantity of it, you are still increasing the load of carbohydrates to be processed by the body. That being said, although the glycemic load can be helpful when formulating nutritional plans for women with PCOS, it has some limitations. This is because it does not measure the insulin production for each food. And for us, this is the most important thing.
Here’s another important consideration. There are certain foods that are much more filling than others. In fact, this seems to be completely independent of effects on insulin or blood sugar. A measurement called the satiety index was created in the mid-nineties by researcher Dr. Susanna Holt. It charts which foods stave off hunger the best by measuring how full people feel from consuming the same number of calories of different foods. It doesn’t measure anything about nutritional content. Instead, it measures how full a food can keep you feeling. As such, this index is really most helpful for those who are trying to lose weight or maintain weight loss. The factors that help a food come up high on the satiety index include water content, fiber, and protein. Interestingly, potatoes, one of the highest foods on the glycemic index, came in tops on the satiety index!
The satiety index has limits. For example, it only contains thirty-eight foods. However if you look at nutritiondata.self.com, there’s a similar index called the Fullness Factor™. This scale has calculated the ability of a food to create fullness based on the nutrient composition and is thought to be quite accurate overall. It gives each food a satiety rank based on how filling it is per calorie.
Another benefit of this scale is that it allows you to create mixed meals and then generate an overall fullness factor for the whole meal. I do like using this factor, especially for women who would like to lose weight. It definitely makes weight loss much easier when you feel satisfied after eating.
Now I would like to cover what I consider to be the single best way to regulate insulin secretion after meals. This is a new concept that you may not have even heard of, but I think it’s important. This concept was introduced in 1997 by a group of diabetes researchers associated with the University of Sydney, Australia. This is the same group of people, including the esteemed Dr. Jennie Brand-Miller, who are considered to be the world’s foremost experts on the glycemic index and are some of the most brilliant researchers in the field of diabetes.
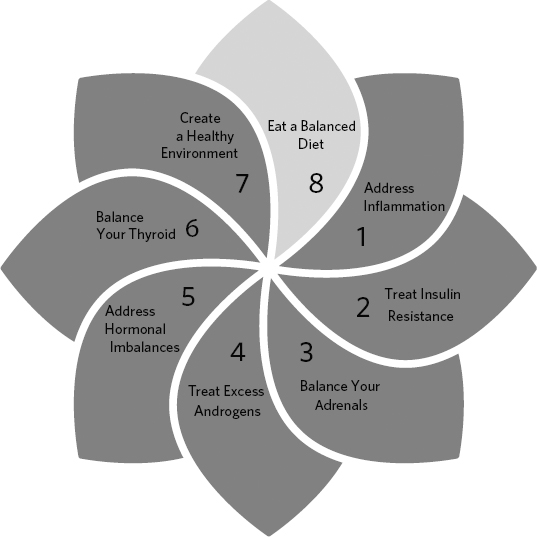
The researchers began by testing thirty-eight foods in healthy volunteers to see how much these foods raised blood insulin after consuming them. They found the foods that raised blood glucose the most (foods high on the glycemic index) also raised blood insulin levels.1 They named this index the food insulin index (FII), which is similar to the glycemic index, but instead of measuring blood glucose responses after eating a specific food, it measures how much insulin your body secretes instead.
Since elevations in blood sugar cause our pancreas to secrete insulin, it makes sense that foods high on the glycemic index are also high on the insulin index. The researchers at the University of Sydney also found something else that was remarkably interesting: Protein-rich foods were capable of raising insulin responses in a way that was disproportionately high compared to their effects on blood sugar. We know that proteins are exceptionally low on the glycemic index, so it was quite interesting to see that they stimulate the release of insulin. This information has the potential to change the clinical practice of diabetes management.
First, I want to be very clear that PCOS is different than diabetes—it is a condition of insulin resistance and not of hyperglycemia. So, although we do want to maintain blood sugar control, controlling insulin resistance is the main focus. That is why this new index, which is showing great promise for diabetes, may in fact be the most well-suited program for women with PCOS.
In 2011, the FII was increased to include around 120 foods.2 In 2014, researcher Kirstine Bell produced a brilliant PhD thesis, “Clinical Application of the Food Insulin Index to Diabetes Mellitus,” that increased this list by another twenty-six foods and tested the concept in clinical practice. The results were fascinating. Using the FII provided even better control of diabetes than the current gold standard, which is carbohydrate counting. She also detailed a new idea that could be put into clinical practice. This idea is known as food insulin demand (FID). FID is a measurement of the insulin response to a given food, taking into account the FII of the food and, most importantly, how many calories of the food are consumed.
Table 9-1: A Satiety Index of Common Foods
FOOD |
SATIETY INDEX |
|
|
Bone broth (estimated) |
350% + |
Non-starchy vegetables (estimated) |
350% + |
Potatoes, boiled |
323% |
Fish and chicken (estimated) |
225% |
Oranges |
202% |
Apples |
197% |
Beef |
176% |
Grapes |
162% |
Eggs |
150% |
White rice |
138% |
Brown rice |
132% |
White pasta |
119% |
Bananas |
118% |
White bread |
100% |
Potato chips |
91% |
Yogurt |
88% |
Peanuts |
84% |
Chocolate bar |
70% |
Croissant |
47% |
All foods are compared to white bread, which is designated a satiety index of 100. The higher the satiety index, the more satisfying the food is.
Non-starchy vegetables, although not directly tested in the source of this study (though estimated in other indices that can’t be directly compared), are very high on the satiety index. They are exceptionally filling per calorie and would be at the top of this list.
Sources:
Holt SH, Miller JC, Petocz P, Farmakalidis E. A satiety index of common foods. Eur J Clin Nutr. 1995; 49(9):675-690.
I believe that the best marker you can use to track how foods affect your insulin is the FID, because it accounts for different macronutrients, not just carbohydrates. Most of all, it accounts for the rise in insulin after eating, which is a concern for most women with PCOS. Even better, it accounts for how many calories of insulin-spiking foods that you are consuming, providing, in my opinion, the most comprehensive way to track the effects of diet on insulin in our bodies.
As the insulin index of a food is calculated for 239 calories of any given food, the FID is relatively easy to calculate. FID = calories × the FII of the food item/239 calories. I do want to note, however, that just because protein raises insulin levels does not mean you should avoid it.
One of insulin’s jobs is to send amino acids into our muscle tissue, so it makes sense that protein-rich foods would increase insulin, but protein doesn’t increase blood sugar like carbohydrates do. Protein-rich foods are high on the insulin index, yet low on the glycemic index.
That’s where glucagon comes in. Glucagon tells the liver to release glucose into the bloodstream when the blood sugar becomes low, which keeps your blood sugar level stable. When you eat high-protein foods, insulin and glucagon are released. When you eat high-carbohydrate foods, only insulin is released.
Glucagon does increase satiety (fullness), which may partly explain the benefits of high-protein diets on weight loss. Glucagon also keeps the blood sugar quite stable after the consumption of protein, which is beneficial. Another factor in support of eating protein is that the amino acid leucine acts in the brain on special compounds known as the mechanistic target of rapamycin (mTOR) and AMP-activated protein kinase (AMPK). These are the cells’ way of sensing energy, and this pathway seems to be important in the ability of high-protein diets to improve weight loss, increase muscle mass, and reduce fat mass.
So overall, eating protein is exceptionally beneficial. However, we should try to stick more to proteins that are lower in FID whenever possible. Beef has a much higher FID than chicken, for example. This is related to the specific amino acid composition of each type of protein.
Note: This is for around 239 calories of each food as shown in Table 9-2. Remember that 239 calories of a vegetable like cauliflower would come to a much larger amount than 239 calories of pasta. This is why, when choosing foods, the food insulin demand is the more accurate way of measuring a food’s impact on your insulin levels: It not only accounts for the food’s ability to increase insulin but also for the amount you are consuming.
* Weights are for edible portion only.
Values sourced and/or estimated from Nilsson M., Stenberg M., Frid A. H., Holst J. J., Bjorck I. M. 2004. “Glycemia and Insulinemia in Healthy Subjects after Lactose-Equivalent Meals of Milk and Other Food Proteins: The Role Of Plasma Amino Acids and Incretins.” American Journal of Clinical Nutrition. 80 (5):1246–1253.
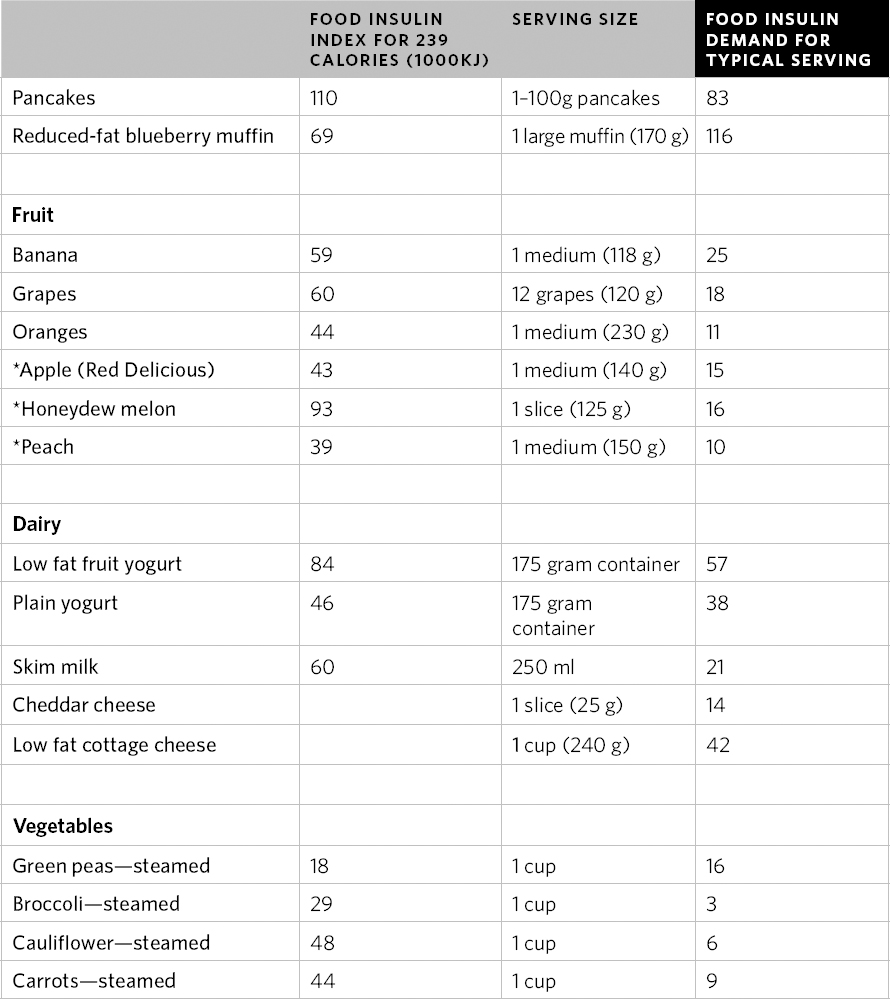
To make things very simple, I have also created an easy to use “insulin count” for you. This is an approximation and is based on the insulin index and FOD, but it makes it easy to calculate the insulin effect of commonly eaten foods and quantities on your metabolic health.
Only some foods have been tested for their FII so far, so some of the foods listed in Table 9-3 are approximations based on other similar foods or their individual components. You can also create your own insulin count of mixed foods by adding together their components. If you visit my website at http://drfionand.com/insulin-count, you’ll find this table as well as a calculator that will help you with this. In time, as more foods are tested, we will be able to adjust these counts with more accuracy.
Adapted and estimated from Bao et al., 2011; Holt, Miller, and Petocz, 1997; and K. Bell 1968.
You should also consider that raw vegetables, in addition to having a low insulin count, are high on the satiety index, so if you are feeling hungry, try adding more salad to each meal.
You may also have noticed that protein powders can be quite high on the insulin index—in particular, whey protein. This is because of the large amount of branched chain amino acids that are in whey. These amino acids can easily and quickly enter the bloodstream. One of the best times to use a protein powder such as whey is directly after working out, particularly after weight training. This way, the spike in insulin is used to drive amino acids into the muscle cells for building and repairing tissue. Enjoy a starch, like a few chunks of steamed or baked sweet potato, with your protein powder post-workout and you’re set!
Now that we’ve got the macronutrients down and the effects of different types of food on our insulin responses, I want to talk about food quality and which categories and types of foods are best to eat and avoid for women with PCOS.
There are a variety of healthy food choices you can make if you have PCOS. The foods in this section are those you can include in your diet.
It goes without saying that the vast majority of what you eat should be plants. Plant foods are jam-packed with an exceptionally wide variety of nutrients, including vitamins, minerals, and phytonutrients, as well as both soluble and insoluble fibers. All of these are preventive for the vast majority of diseases that humanity suffers from today. Most of all, study after study highlights their benefits in the prevention of type 2 diabetes, cardiovascular disease, cancer, and their ability to improve metabolic health. For optimal health, you should include vegetables with a wide variety of colors and focus primarily on non-starchy vegetables.
Most non-starchy vegetables are given the green light, meaning you can eat plenty of these every day. They are rich in fiber, water, numerous vitamins and minerals, and they have a high satiety index and low insulin/glycemic indices. Following are some examples of non-starchy vegetables. You should be having at least half a large dinner plate of these with every meal:
Rather than deriving carbohydrates from grains, starchy vegetables are a better choice because they do not contain irritants or phytates that decrease nutrient absorption. If you are exercising, you’ll need more carbohydrates to fuel your work-outs and your recovery.
Starchy vegetables can have a higher glycemic index and have higher carbohydrate loads than non-starchy vegetables, so smaller amounts should be consumed. To make meal prep easier, I often chop and freeze starchy vegetables for the week and use them as needed for meals. Some examples include—
Fruits are an excellent source of fiber, vitamins, and minerals and are one of the main sources of carbohydrates that should be included in a diet for PCOS. They are also a healthy option you can take quickly on the go. As fruits do contain significant amounts of natural sugars, it’s best to choose the lowest sugar fruits as a general rule. Other fruits can also be enjoyed if the quantities are kept in check.
The lowest sugar content fruits are—
*Although not thought of as a fruit, these are an amazingly low-insulin index choice and should be eaten regularly.
Medium-sugar fruits include—
High-sugar fruits include—
**If they are ripe. If they are unripe, they are much lower in sugar.
Oils are an important part of a healthy diet. We were all taught that fat was bad during the low-fat diet phases of the 1990s and 2000s. Recently, this has been completely debunked. Fats can be and are good for you. It’s really the type of fat that makes the difference.
When it comes to vegetable oils, you’ll want to choose them carefully. The reason for this is that vegetable oils are made of primarily unsaturated fats, which means they have delicate bonds within their structure that are sensitive and can be broken down rather easily. There are two major types of unsaturated fats: polyunsaturated and monounsaturated. Polyunsaturated fats, just as the name suggests, have multiple delicate bonds within them. Monounsaturated fats have only one delicate bond within. Because of these extra delicate bonds, polyunsaturated fats are more vulnerable to damage and must be treated with more care. We all have learned that polyunsaturated fats are good for us, and they actually are a very healthy part of our diet, particularly those of the omega-3 variety.
The main issue is that the vast majority of polyunsaturated fats that we consume have been heavily processed. They have also been exposed to heat, chemicals, and light during processing, causing the bonds to break down within the fats. What happens when the bonds break down? The fat changes form into a type of fat known as lipid peroxide, which is quite harmful.
The vegetable oils that are the most concerning are canola oil, sunflower oil, corn oil, safflower oil, and cottonseed oil. These oils are mass-produced and treated with chemicals and heats that damage the very nature of the oil. The oil is extracted from the seed with chemical solvents. In addition, once you take this oil and use it to cook your food, you are heating it up even more, increasing the toxic potential of the oil.
The other negative with many of these oils is that they contain large amounts of omega-6 fatty acids. Too many omega-6 fatty acids can increase inflammation, and it is very difficult to keep the levels of these in your diet in check, since they are present in so many foods.
It’s also important to know that our cell membranes are made up of fatty acids. Polyunsaturated fatty acids can be good for our cell membranes, as are saturated fatty acids. Together, these two types of fatty acids give our cell membranes fluidity. This helps with the function of every cell in the body. However, if polyunsaturated fatty acid is exposed to heat or oxygen, it turns into lipid peroxide, which can damage the cell membranes and also the DNA within our cells. Lipid peroxides can also damage the phospholipids in the cell membrane, eventually poking holes in our cells, allowing free radicals to enter into our cells and damage them.
In addition to lipid peroxides, we all know that trans fats are unhealthy, as they are associated with multiple diseases, including cardiovascular disease and cancer. What isn’t known is that vegetable oils contain trans fats. Research has found that many commonly sold vegetable oils contain these fats, presumably because of the way they are processed. Trans fats don’t exist in nature; they are the result of the processing of oils. When incorporated into cell membranes, a variety of different dysfunction occurs.
When it comes to vegetable oils, the best are avocado oil, extra virgin olive oil, and coconut oil. Avocado oil and extra virgin olive oil contain monounsaturated fats and are far more stable than the polyunsaturated oils. They appear to be stable under very low-heat cooking. Olive oil, in particular, has been researched extensively and has many health benefits. I recommend using only these as your sources of liquid vegetable oils.
As cooking oil for very hot temperatures, extra virgin coconut oil is the best choice. Being comprised of saturated fat, it’s exceptionally stable when heated and when stored. When it comes to avoiding the coconut flavor in your cooking, there is the option of expeller-pressed organic coconut oil, which is available at most organic grocery stores. This doesn’t have as many health benefits as extra virgin coconut oil, but it is still a good choice when you want to avoid coconut flavor in your food.
Another option for high-temperature cooking is clarified butter, also known as ghee. Ghee, particularly when organic and taken from grass-fed cows, has a variety of health benefits and contains a compound known as butyrate, which is beneficial for intestinal health. As much of the milk solids are removed, it does not have the insulin spiking effects that other dairy products have.
That being said, since hormones are always concentrated in the fat portion of dairy, always choose organic and don’t overdo it.
I’m also going to include avocado in the oils section even though it is a fruit, as it contains wonderful fats. Adding a quarter of an avocado to a meal will make you feel fuller longer and provide a wonderful source of nutrition to your diet.
Meats, including fish, poultry, red meats, and game, can be an excellent source of protein and micronutrients for women with PCOS. In addition to protein, meats contain a variety of vitamins, minerals, and omega-3 fatty acids that provide dense nutrition. It’s helpful if you can afford organic and especially pastured or grass-fed meats, as they have improved nutritional composition and less toxicity.
Fish have gotten a bad rap lately due to toxicity; however, they are an excellent source of nutrition. And although they do increase insulin to some degree, like all proteins, they have so many wonderful nutritional benefits and they should definitely be included in the PCOS-friendly diet. High in omega-3 fatty acids, protein, and vitamins A, D, and magnesium, they are an excellent source of lean protein to add to a meal. There are two main contaminants to look out for in fish: mercury and PCB. However, fish is such a healthy food that the benefits often outweigh the risk of contamination, especially if you choose your fish carefully.
Mercury is one of the most toxic metals to the human body. As such, this should be our primary concern when it comes to choosing fish. Large, predatory fish are particularly likely to concentrate mercury in their tissues. As all fish do contain some mercury, when larger fish eat smaller fish, they accumulate more of it in their bodies over time. As mercury comes primarily from industrial contamination, fish that are caught near a coast or freshwater where there is a human population are also more likely to be contaminated.
The fish that are highest in mercury include—
Fish that are generally lower in mercury include—
To learn more about mercury levels in fish, there is an excellent website located at http://seafood.edf.org/seafood-health-alerts. The Environmental Defense Fund also keeps an excellent updated database on the mercury content in fish.
Many people ask about farmed versus wild salmon. My opinion on salmon is that if you can get it, wild Alaska or sockeye salmon are by far your best bet. Wild salmon has a better fatty acid profile than farmed salmon, as farmed salmon are fed a different diet with the goal of fattening up the fish. The main concern with farmed salmon is that they do contain much higher levels of PCBs when compared to wild salmon.3
If you can afford it, wild Alaska salmon is the best choice. Fortunately, most canned salmon is wild Alaska or sockeye, which are excellent healthy and affordable choices. Once in a while, however, farmed salmon can be included in your diet, particularly if you are replacing less healthy choices with it, such as when going out for dinner or at a friend’s home. If you are pregnant, breastfeeding, or trying to conceive, however, I would avoid farmed salmon.
In addition to mercury, the levels of PCB and other contaminants in fish may vary greatly, depending on where the fish are caught. PCBs are particularly concerning for women in their childbearing years, as they can affect the development of the fetus. In addition, increased PCBs have been linked to developmental problems in children. Fish that tend to be the highest in PCBs are those that reside near industrial areas and are bottom feeders. These include wild-striped bass, bluefish, American eel, and sea trout.
Chicken, turkey, Cornish hen, pheasant, and other poultry are an excellent source of lean protein for women with PCOS. They are high in niacin, selenium, and vitamin B6. It is optimal to access pastured poultry from a farmer if you can, due to toxicity concerns detailed below—organic is also a good choice. If you only have access to conventional poultry, be sure to remove the fat before cooking. Poultry, on the whole, has a lower insulin index for a protein-rich food, yet it is highly satisfying and so is helpful for those who are more insulin resistant and want to lose weight. If you get a pastured chicken, be sure to save the bones and make bone broth—you’ll find instructions on how to make this healing, nourishing food in the recipes appendix.
Bone broth can be made from any type of bone—many women find it an excellent addition to breakfast, as a filling, nutritious, and delicious start to the day. Some women also have a cup with dinner. As you can imagine, bone broth is high on the satiety index, given its low energy density, but it also is packed with nutrients. Since bone broth is often cooked for many hours with herbs and vegetables, it contains a variety of vitamins and minerals. In addition, when a bone is cooked for a long period of time, as in bone broth, it becomes rich in amino acids like proline and glycine. Glycine in particular is beneficial, as glucose regulation, insulin sensitivity, and the production of the main intracellular antioxidant, glutathione, rely on it.
Red meat, including beef, lamb, and pork, definitely has excellent nutritional value. It has a good deal of protein and is a rich source of many nutrients, including B vitamins, iron, zinc, selenium, copper, and potassium. Beef and lamb, in particular, are the best sources of zinc, B vitamins, and iron. Pork only offers modest amounts of these.
We talked about certain amino acids being more insulinogenic than others. Well, how does this relate to meats? There are, in fact, meats that are better for women with PCOS to consume. Beef is quite high on the insulin index, so it is the least recommended. If you do consume red meat, you should be aware of the quantity and that, if you are insulin counting, you get less quantity-wise for red meat than you do for poultry. Another major concern for women with PCOS is that red meat, like dairy, contains estrogen, so for that reason, as well, it should be consumed only in moderation.4
When it comes to consuming red meats, you’ll also want to avoid high-heat cooking. Carcinogenic byproducts are created when red meats are heated at high temperatures and through fermentation by the gut microbiome. These toxic products include heterocyclic amines and polyaromatic hydrocarbons (PAH). So, when cooking animal proteins, use low heat whenever possible.
Grass-fed, organic meats are the best choice for beef. Not only do they contain lower amounts of contaminants, such as medications or hormones, they also provide better nutrition. These animals graze on grass, and, as such, their tissues are quite different composition-wise. Animals that are grass fed have more omega-3 fatty acids and micronutrients like vitamin E, zinc, and carotenoids.5, 6 Another popular red meat is bison, which is becoming increasingly available on the market, offering another more natural alternative to conventional beef.
It is unfortunate that in North America, artificial hormones are used on livestock to increase their growth. In the US, recombinant bovine somatotropin (rBST), also known as rBGH, causes an increase in another growth hormone, IGF-1, in treated cows. Some studies have associated risk for breast, colon, and prostate cancer with increased serum levels of IGF-1.7, 8, 9 In addition, cows given rBGH are more prone to infection of their udders, known as mastitis, resulting in an increased need for antibiotics.
Another consideration is that in most modern feedlots where animals are raised, the conditions are unsanitary, and low-dose antibiotics are routinely given to the animals to prevent infection. Antibiotics are also used to increase the growth rates of the animals. Surprisingly, a survey from John Hopkins’s Center found that eighty percent of all antibiotics sold were for use on livestock and poultry.10
Pesticide residues also accumulate in the tissues of animals. Dioxins are one of the most concerning environmental toxins and have been linked to cancer, reproductive problems, cardiovascular disease, and diabetes. It is thought that ninety percent of human exposure to dioxins comes from animal fats, fish, and shellfish.
If you can locate a farmer who sells meat in your area, this is often the best option, as you can inquire about their farming practices. Many farms with ethical, organic practices will provide plenty of information on their websites. Local farmers markets are also good places to source quality meats directly from the farmer. Many small farms offer bulk purchasing of meats, which can make it more affordable to buy quality meats. Another excellent option is community-supported agriculture (CSA). In this situation, you pay a one-time fee to support the farmer each season, and then you receive a biweekly or monthly portion of meat fresh from the farm. The same can be done with organic produce, so if you want to have regular access to more affordable quality food and support local farmers this is a great option.
When consuming meats—
Eggs are one of my favorite foods for women with PCOS. They include a wonderful nutrient profile, including folate, vitamin A, vitamin B2, vitamin B12, choline, and selenium. In addition, they contain an amazing amount of protein for a small amount of calories and are filling and satisfying. A boiled egg or two packed with your lunch or for a breakfast on the go can prevent you from making poor food choices when you are out. Even better, chickens that are fed quality feed, such as those that are pastured (the chickens run free eating insects and feed), as well as organic eggs, have an excellent fatty acid profile and an even better nutritional value.
So what about cholesterol? I get this question often, as women with PCOS are more at risk for high cholesterol, which is an important issue for us. I’ll just let you know for certain that eating eggs does not increase your cholesterol, unless you have a rare form of familial hypercholesterolemia. Your liver manufacturers cholesterol from the foods that you eat, and when you eat eggs, your liver will not make as much as it would normally. For a small percentage of people, eating eggs will mildly raise their total and LDL cholesterol, but for the vast majority of people, eggs raise the good HDL cholesterol. In addition, it appears that eggs increase the LDL cholesterol into a subtype called large LDL. It’s the small, dense LDL that is linked most to heart disease. If you are following the healthy diet recommendations in this chapter, you should see improvements in your cholesterol panel, despite eating eggs on a regular basis. What you eat and your level of exercise will determine your cholesterol levels.
Nuts and seeds are excellent sources of nutrition. They contain healthy fats, protein, vitamins, and minerals, such as vitamin E and magnesium, and best of all, they are satiating. They do contain phytates, so they should not be consumed with each meal. The other downside of nuts and seeds is that they have a very high caloric density. It’s very easy to eat handfuls of nuts, and before you know it, you will have consumed a thousand calories. As such, I often recommend measuring nuts and seeds and placing them on a plate before consuming them. As is the case with legumes, sprouting or soaking nuts and seeds will reduce the phytate concentration. Quinoa, although thought of as a grain, is actually a seed. It’s something that I recommend in moderation also, and, if possible, sprouted to reduce phytate concentration.
The most nutrient dense nuts and seeds are—
Legumes include beans, chickpeas, lentils, and peanuts and are what I would consider a nutritional grey area. Legumes do contain significant amounts of phytic acid and may inhibit the absorption of nutrients. That being said, legumes can be an excellent source of fiber, vitamins, and minerals, so I often tell patients that legumes are one of those areas for which you have to make an individual choice. If you do choose to consume legumes, sprouting, soaking, and fermenting will reduce the phytic acid content significantly. In many cases, these processes can almost entirely remove phytic acid and may substantially increase the nutritional value of these foods. In some cases, however, legumes can be quite aggravating to digestion. If you notice bloating or digestive discomfort after eating them, they may be best to avoid while you are going through the healing process.
As we all know, water is absolutely the best beverage of all. It’s what our body really needs. Women with PCOS often lose weight more easily when they increase their water intake. It’s phenomenal what this one simple act can do. A recent study in The American Journal of Clinical Nutrition found that when subjects replaced diet soda with water after each meal on a twenty-four-week weight loss program, they lost fourteen percent more weight, and their insulin resistance markers improved by forty-one percent.11
If you are wondering how well hydrated you are, you can measure by the color of your urine. If it is lighter, it’s a sign you are probably getting enough water. Strong-smelling or dark-colored urine is a sign you need more. That is, unless you are taking B vitamins. Vitamin B1 changes the color of your urine to a fluorescent yellow hue, which is completely normal. Another at-home test you can do to check your hydration is to purchase some chemstrips online. The specific gravity is the measure of how concentrated your urine is. Aim for a specific gravity of less than 1.10. Anything above means that you are moderately dehydrated.
Other healthy beverages include—
Coffee is something that I personally enjoy, but I have done research into whether it is healthy or harmful. It depends on your individual condition overall; however, it can actually be a healthy part of your diet.
The pros of coffee are that it has clear benefits for your brain function. It can improve your mood, your focus, and your concentration, and according to significant research, it can keep neurodegenerative processes, such as Alzheimer’s disease, at bay.12 It also boosts your metabolism, a clear benefit for women with PCOS. However, if you drink coffee every day, this effect may wear off in time. People who drink coffee have also been found to have a lower incidence of metabolic syndrome and lower triglycerides, presumably due to its effects on insulin resistance.13 In addition to this, coffee contains antioxidants, which may have numerous benefits for cell health.
The cons of coffee are in part related to its stimulating effects. For those with anxiety, or those who have adrenal hyperactivity and high cortisol levels, it may actually exacerbate and aggravate their condition. It can cause insomnia, so those who already suffer from insomnia should avoid it entirely. It can also be irritating to the gastrointestinal tract, both due to its stimulating nature and to some of its physical composition. It is also not recommended for women who are pregnant or trying to conceive, as there have really been no clearly established safety rules for pregnancy.
That being said, I do think that most women with PCOS can enjoy moderate amounts of coffee (1–2 cups per day), if they tolerate it. It can boost mood, ward off depression, increase exercise results, and improve metabolic health. Each person is unique in their ability to tolerate and metabolize coffee. Some cannot metabolize caffeine, and the effects will be magnified in these individuals. I recommend that women with PCOS take their coffee black. This may be a stretch; however, you’ll find that after a short period of time, you will not miss the sugar or cream.
Now we are going to look at foods that can trigger symptoms in those suffering from PCOS. I recommend avoiding the foods listed in this section to reduce your symptoms as you work to reverse your PCOS. I just want to make a note here about nutritional restriction. In most cases, the strict avoidance of the foods on this list is not necessary, or even healthy. Although it is helpful to avoid certain foods in general, if you eat something on the avoid list occasionally, it will not have much of a negative impact. It’s important not to let nutrition be a stressor for you and to know that perfection isn’t required to make changes that will transform your health. There are some exceptions: For those wanting to lose weight, following these guidelines more closely will definitely result in more success. For those who have intolerances, or autoimmune diseases that are aggravated by specific food triggers, you probably already know that more compliance is needed to support your health.
My goal is not for you to look at foods as either good or bad, but rather to learn to make the best choices on a daily basis. These choices often come naturally when you are armed with information on nutrition, and you’ll feel at your best when you focus on eating real, whole foods.
This is the number one thing that should be avoided if you have PCOS. As we know, many foods contain natural sugar, and we’ll need to watch that also since as women with PCOS we are far more sensitive to all types of sugar, both natural and added. However, it’s the added sugars that are particularly harmful, because they tend to be more dense and without nutrients like fiber, vitamins, and minerals.
I often recommend avoiding all types of sugar, whether it’s fructose or glucose. Sugar in the form of glucose directly increases insulin, and women with PCOS have shown intense inflammatory responses to a dose of sugar almost immediately after ingestion.14 Women without PCOS don’t have this same inflammatory response. As such, we need to be much more careful about our sugar consumption than others do.
Fructose, however, is a different animal. Sucrose—what we typically call “table sugar”—is about half fructose and half glucose. Glucose can be absorbed and metabolized by all of the different cells in the body through the action of insulin. Fructose, however, is different: It is primarily absorbed by the liver without the help of insulin. As a result, fructose doesn’t raise the blood sugar or insulin level much after it is consumed. Instead, the liver takes it up and stores it into an energy form known as glycogen, which is basically a storage tank of sugar within the liver. When a small amount of fructose is consumed, such as in a small serving of fruit, the body can handle this easily.
When we fast, when we sleep, for example, the body will use up the glycogen in the liver for fuel. The same thing happens after we exercise, because exercising also requires the burning of the glycogen, which is stored. This is why having some starchy carbohydrate is a good idea after exercise: It refills the tank of glycogen that has been depleted.
It’s a totally different matter, however, when a large amount of fructose is consumed, particularly when the glycogen tank is already full (which it is, most of the time). The excess fructose has nowhere to go and must be converted into fat, much of which deposits right in the liver. This action is linked to causing nonalcoholic fatty liver disease (NAFLD), which is a common PCOS-related condition.
Eating too much fructose has also been associated with increased abdominal fat deposition, cardiovascular disease, and insulin resistance. For more information about this condition, which is common in women with PCOS, please see Appendix C.
Fructose also decreases circulating insulin and leptin levels when it enters your system and increases ghrelin levels.15 Because leptin and insulin decrease appetite and ghrelin increases appetite, it’s thought that this may be why fructose has been linked to weight gain.
Sugar also disrupts the bacterial balance within our small intestines, shifting the millions of microorganisms that reside there, known as the microbiome, and changing the very type of species that live there. Eating a lot of sugar, or a standard Western diet, can shift the microbiome toward one that is associated with obesity and insulin resistance.16
The microbes that live in our gut can either help us have good metabolic health, or they can hinder us and contribute to insulin resistance, obesity, and inflammation. Sugar feeds the wrong types of bacteria, causing them to flourish and overgrow, leaving little room for the friendly bacteria that are linked to good metabolic health.
There are two prominent intestinal bacterial species, known as the fermicutes and bacteriodes. When these species are in good equilibrium, our metabolism is healthy, but when the ratio of these is poor in the intestine, the person will actually gain weight. Transplantation of bacteria from insulin-resistant medically “obese” donors into a recipient can actually cause weight gain.17 It’s thought that differences in the microbiome even play a large role in our resting metabolic rate and how many calories we burn while asleep. Over time, we will learn more, but it’s clear that the microbiome plays a huge role in our metabolic health, inflammation, and insulin resistance.
When it comes to sweeteners, I generally ask my patients to avoid even natural sweeteners for a period of thirty days. This is to reduce their desire for sweet and to turn off the areas of the brain that are asking them to eat sugar. Artificial sweeteners may be able to disrupt the insulin pathways, creating a similar response to sugar in the brain. In addition, some studies have even found that artificial sweeteners may increase hunger, cravings, and/or food intake.18 I recommend that you avoid these entirely.
In this section, I’ve included a list of sugars to avoid. Note that sugars are often hidden skillfully under a variety of names on a label. You’ll want to become familiar with these so you can detect them before buying a food. Being sugar savvy will help you on your journey toward better health.
These sugars in the following list are names you may recognize from packaging. Keep an eye out for them, as these are all different forms of sugar:
Generally, it’s also best to avoid natural sugars, but they can be enjoyed occasionally as part of a treat. Of the natural sugars listed here, blackstrap molasses offers a good nutritional punch, as it includes iron, calcium, magnesium, manganese, antioxidants, and vitamin B6. Date sugar is another good choice, as it is the natural sugar richest in antioxidants and is quite sweet, so less can be used.
These are not recommended for women with PCOS as a general rule. Concentrated fructose, as mentioned earlier, is metabolized through the liver, can raise triglycerides, and contributes to fatty liver. It is also associated with weight gain. Try to avoid the following for that reason:
Stevia is the leaf of a plant known as Stevia rebaudiana. Stevia has an intensely sweet taste, and so very little of it is required to sweeten. Overall, it’s very likely to be safe when consumed occasionally and in small amounts. One caution with stevia is that it has been linked to infertility in animal studies, so women who are trying to conceive should avoid it. If stevia is used, natural green leaf stevia is the best type.
These are forms of sugar that are slightly different in structure, having an extra oxygen and hydrogen atom attached. This puts them into the category of a sugar alcohol. These do occur naturally in fruits but only in small quantities. The sugar alcohols are less sweet than sugar, have fewer calories than sugar, and have less of an effect in raising blood glucose. Unfortunately, many people react with digestive symptoms, such as bloating, gas, and diarrhea, upon eating sugar alcohols. This is because they are poorly absorbed and travel down to the colon and act as substrate for certain types
of bacteria in the gut. In some individuals, this can seriously aggravate intestinal health. As such, they are generally best to avoid; however, of the list provided, erythrytol is the best choice, as it is absorbed almost completely in the small intestine, avoiding passage to the colon and fermentation by microbes:
Artificial sweeteners should be avoided. They have been linked to insulin resistance and can alter the human microbiome. Most of all, my main concern with them is that there is evidence suggesting that certain artificial sweeteners may be linked to cancer. Until more safety information is available, it is definitely best to avoid these altogether and choose from the many other options for the occasional consumption of sweetener. These sweeteners include—
The dairy industry has told us repeatedly that dairy is a health food and is actually required in order to be healthy. This is not the case at all. Now, some people do feel very well with quality dairy products. However, the reality is that for PCOS, dairy is something that should be avoided.
When you think about dairy, what is its purpose? Milk is a food that is made to nourish a baby animal before it can consume nutrients through other food sources. As such, it is biologically engineered to stimulate and support the rapid growth of a young animal. It is nutrient dense and made to provide a large amount of everything needed to support tissue growth, all within a very small volume. This is great for a baby animal with a relatively small stomach that is growing at a very rapid pace.
However, does this seem like something we should be having if we are insulin resistant and are already metabolic conservers? Absolutely not! As we saw when we went through the insulin index, dairy products, even fermented ones, such as yogurt, are some of the most insulinemic foods out there. In fact, on the insulin index, yogurt rates as high as white bread!
In particular, amino acids, the building blocks of protein, especially the branched chain variety (valine, isoleucine, and leucine), can cause a spike of insulin that is quite significant. Dairy contains these amino acids. So, for women with PCOS, it wreaks havoc with insulin levels in a similar manner as white bread. In addition to the specific amino acids in dairy that cause our insulin levels to spike, dairy also contains several other compounds that are concerning for metabolic health. For a baby animal, these compounds have an important and useful function. In an adult, they may present issues depending on your metabolic health status. For example, dairy contains—
-Estrone
-Estriol
-17-alpha estradiol
-17-beta estradiol
Cow’s milk contains considerable amounts of female sex hormones in particular. These may compound the already existing hormonal imbalances in PCOS. In addition, since women with PCOS are more at risk for endometrial cancer, the consumption of additional estrogen in dairy would be concerning, given its link to cancer.
In modern dairy production, cows are milked hundreds of times per year and are pregnant for much of that time. Toward the end of pregnancy, the amount of female sex hormones in the milk is quite high. This could also be a very important factor to consider for mothers of daughters with PCOS, since seventy-five percent of children consume dairy daily. The amount of estrogen that girls at risk for PCOS are consuming in the pubertal period could have unknown health outcomes years from now. Studies have already linked hormonally positive cancers of the breast and prostate to dairy consumption, so there just isn’t any good reason to be consuming this food. Of course, dairy produced in a more natural way, or purchased from a farm where more natural methods are practiced, would contain much lower levels of hormones.
Overall, such a nutrient-dense, made-to-build-tissue food may work wonderfully in the calf’s body, for which it was designed. However, for an adult woman who has the tendency to deposit abdominal fat, this is the exact opposite of what we should be eating. The leptin in milk also contributes further to the leptin resistance that many women with PCOS are fighting against. IGF-1 and IGF-2 are also growth-promoting factors. As such, we do not need to be directly consuming these either.
Then we come to the steroid hormones, namely the estrogen, testosterone, progesterone, and cortisol that are present in milk. In a system that is already prone to hormonal flatline, adding more to that mix will only further confuse our receptors, our hypothalamus, and our ovaries. Our goal is to restore the normal signaling environment of the hormones, one that is primarily disrupted in PCOS. Dairy products only serve to further confuse our hormonal systems, and for that reason, I ask most women with PCOS to avoid them entirely.
Source: Blum and Baumrucker, 2008; Pape-Zambito, Roberts, and Kensinger, 2010
I am not totally against dairy as a general rule, and it is true that quality, grass-fed dairy products can provide good nutrition for some individuals. However, in the typical woman with PCOS, they are arguably one of the most important foods to avoid.
My patients often ask me how they can get their calcium if they do not consume dairy. The first thing to note is that consuming large amounts of calcium, as we have been advised by government agencies, does not necessarily correlate with reduced fracture risk. The World Health Organization has reduced its recommendations for the consumption of calcium in favor of exercise (which has proven to benefit bone density), maintaining good vitamin D levels, and increasing the consumption of fruits and vegetables.
Protein can actually increase the excretion of calcium,19 so we must look at calcium intake as a function of the overall diet you are following. If you are consuming calcium with animal protein, such as cow’s milk, the absorption is far less than what you might think. If you are eating a healthy diet, avoiding processed foods, consuming a large variety of calcium-rich, healthy, leafy green vegetables, and getting regular exercise, you should easily reach the amount of calcium recommended. Beware of calcium supplements, particularly those of lower quality. Though the label may read a large amount of calcium, only a small amount is actually absorbed by the body.
In the Harvard Nurses’ Health Study, which followed more than 70,000 women for more than twelve years, it was found that consuming dairy products had no effect on the fracture risk in these women.20 If after increasing your consumption of green leafy vegetables you feel you are still deficient in reaching your requirements for calcium, it’s much better to choose a quality calcium supplement to achieve your daily needs. Until recently, the recommended daily amount of calcium for women of reproductive age has been approximately 1,000 mg. However, several health agencies have recently made changes to their recommendations on calcium requirements. The World Health Organization now recommends 500 mg per day, and Dr. Walter Willett, chair of the Department of Nutrition at the Harvard T. H. Chan School of Public Health, agrees. He states that high-dose calcium doesn’t provide any benefits and that between 500 and 700 mg per day should suffice.
When it comes to supplementation, there are differences between the forms of calcium. Many inexpensive forms of calcium, such as calcium carbonate, do not have the same ability to slow the breakdown process of bone. In fact, studies have found that better forms of calcium, such as calcium citrate, may have increased benefits in slowing bone breakdown by as much as thirty percent. Other forms, which also have good absorption, include calcium malate and calcium hydroxyapatite. However, as hydroxyapatite is sourced from an animal (usually cows), the brand must be chosen carefully.
Some foods are also fortified with calcium. Dairy alternatives abound these days and there are many to choose from. The options include—
I do not recommend that women with PCOS consume soy milk, for reasons I’ll explain later. My favorites of the milks listed for women with PCOS are almond milk, cashew milk, and coconut milk. Each has a slightly different profile, with almond milk generally being the lowest in calories. Cashew milk and coconut milk offer a higher healthy fat profile and are more filling. Rice milk is higher in carbohydrates and therefore not the best option.
Many boxed-milk alternatives contain carrageenan, which can irritate the intestines for some individuals. There are now organic brands that are free of this additive, so read your labels. Even better: You may want to try making your own nut milks. It’s very easy with a blender.
Gluten, which is found in wheat, spelt, rye, and barley, is a food I recommend that women with PCOS avoid, for the most part, though this may vary from woman to woman. Gluten is made up of gliadin and glutenin. The gliadin is the problematic part for most individuals. In people with celiac disease, reactions to gluten can be severe, damaging the intestines and causing severe destruction of the intestinal cells. However, only one percent of the population has celiac disease, so how does that apply to you?
First, gluten can be an inflammatory food. It creates leaky gut and triggers immune reactions in many people. A growing body of evidence suggests that a large percentage of people who do not have celiac disease are sensitive to gluten, primarily because of these inflammatory effects. Some people may have antibodies to gluten in their stool or blood, yet they do not have celiac disease. Those who are sensitive secrete increased amounts of a protein known as zonulin in their intestines after consuming gluten. This protein causes the intestinal barrier to leak, which can create a host of negative effects for intestinal health. Around forty percent of people carry the genes for celiac disease, predisposing them to sensitivities to gluten, even though they may never develop full-blown celiac disease. Now, thankfully out of the realm of being considered an imaginary syndrome, non-celiac gluten sensitivity has been confirmed as a real condition with increased intestinal permeability responses to gluten ingestion, without the autoimmunity of celiac disease.21
As women with PCOS have an excessive amount of inflammation, this is problematic. I’ve found that many women with PCOS feel much better without gluten as part of their diet. The only real way to know if you are sensitive to gluten is to eliminate it from your diet for a month. If you feel better, don’t eat it! That being said, it is not necessary for the vast majority of women with PCOS to avoid gluten to the degree that someone with celiac disease would.
It’s also interesting to note that gluten can have negative effects on anyone, even if they are not particularly sensitive to it. It causes permeability of the gut lining, allowing products from the intestine to activate inflammatory responses, and has been linked to irritable bowel syndrome.22
One of the best reasons to avoid gluten is that it increases leptin resistance. A recent study showed a fifty percent increase in leptin resistance after cells were exposed to gluten.23 Leptin resistance increases hunger, causing us to eat more. This may be why wheat is addictive, in a similar way sugar is. Gluten also contains small peptides called exorphins, with opioid-like properties that some researchers believe play a role in its addictiveness.
When it comes to grains in general, there may be good reason to minimize their consumption. Many grains contain similarly irritating, inflammatory substances such as gliadin. Grains, such as corn, are one of the more common allergens, and the vast majority are genetically modified.
Grains also contain phytates. Phytates have received mixed reviews, so I’d like to take a closer look with you. Phytates are found in plant seeds (grains) and have been referred to as “anti-nutrients.” Phytates are also found in legumes and certain nuts, which I’ll discuss in the next section. The amount of phytates in foods is variable as well.
The main argument against phytates is that they decrease the absorption of different minerals, including iron, zinc, and calcium. This effect is only present directly after eating the food itself and doesn’t last for long periods of time. So, as you can see, phytates are something that you wouldn’t want to be consuming with every meal, or you could potentially develop nutritional deficiencies over time. In addition, if you are consuming a variety of foods with phytates, you increase this effect exponentially. Therefore, I would suggest that it’s best to be selective with your phytates: mostly nuts and some legumes, if you are able to tolerate them.
Phytates are not all bad. They do have antioxidant and anti-cancer properties. As such, we have to look at them as something to balance in our diet rather than be afraid of. Although grains, such as buckwheat, contain inositols, a compound we know is quite beneficial for women with PCOS, the inositol must be cleaved from the phytates within to be accessed. As such, I do not recommend that women obtain their inositols from grains, because to get the recommended amount, a large quantity would have to be consumed, and this could disrupt the absorption of other minerals from the diet.
Rice may be an exception and is most likely one of the best-tolerated grains, because it tends to have little allergenic potential. That being said, its high insulin index means that it should be used in small quantities only. In addition, although brown rice has been long recommended as the healthier rice, it contains higher amounts of phytic acid, which, for reasons stated earlier, may negate some of its benefits. The occasional consumption of small amounts of steel cut oats or quinoa would also be an exception for those who are not sensitive to these, but this should be done within the following insulin index guidelines.
Before calculating the insulin counts of your meals, the first step is learning to structure the components on your plate—protein, vegetables, carbohydrates, and fat. Start with lean protein. The portion should be about the size of the palm of your hand. Depending on the protein you choose and your recommended insulin count, which we will address next, you may be able to have more or less. You’ll get a lot more portion-wise from choosing poultry or fish when compared to beef. Half of your plate should be comprised of vegetables. Add a serving of healthy fats (around one tablespoon of a healthy oil or one serving of avocado or nuts).
Finally, add a small serving of carbohydrates. Choose from the most nutritionally dense and least inflammatory carbohydrates first, like berries, sweet potatoes, and squash. Yes, that's right, fruits are carbohydrates! You can occasionally have quinoa or white or brown rice if your body tolerates it. Bread is not recommended, particularly for those who want to lose weight, as it is typically made of processed grains and almost always contains gluten. There are, however, some gluten- and grain-free homemade breads high in healthy fats and proteins that are an exception.
Now that you’ve got an idea of how to structure your plate, let’s talk about insulin counting. The insulin count that is best for you depends on a few different things, including your level of insulin resistance, your desire to achieve weight loss, and your personal response to different levels of carbohydrate restriction. Once you are used to the process of insulin counting, my hope is that you will be able to estimate your most optimal meal structure without measuring or calculating. At first, you may want to invest in a small kitchen scale and some measuring cups to get familiar with the recommended portions, particularly if weight loss is your goal.
Insulin counting is very easy: You simply add up the count of each food or ingredient in your meal. Adjust the count for the quantity that you consume. So, if you have double the quantity listed of a food, just double the insulin count. As insulin indices have been measured for certain foods, there are likely many foods you would like to enjoy that are not included. In this case, just substitute the insulin count of the most similar food when it comes to carbohydrate or protein content. In time, the list will grow and many more foods will be included.
As a general rule, for women who are insulin resistant, carry extra weight around the abdomen, or who want to lose a significant amount of weight, aiming for an insulin count of between fifty and sixty per meal is often optimal. Some women may do even better under fifty, but this should be supervised by a health-care practitioner.
Table 9-7: Foods and Insulin Counts for Women with Significant Insulin Resistance
SAMPLE CHOICE |
INSULIN COUNT |
Four ounces of roast chicken breast |
17 |
Two cups of green vegetables |
5 |
One half of an avocado |
4 |
One half of a medium sweet potato (76 g) |
23 |
Total |
49 |
SAMPLE CHOICE |
INSULIN COUNT |
Four ounces of white fish |
15 |
Two cups of mashed cauliflower |
12 |
One tablespoon of extra virgin olive oil |
2 |
One cup of leafy green salad with lemon juice |
0 |
One apple |
15 |
Total |
44 |
For women who are of average weight and mildly insulin resistant, start with an insulin count of approximately fifty-five to sixty-five per meal.
Table 9-8: Additional Foods and Insulin Counts
SAMPLE CHOICE |
INSULIN COUNT |
Four ounces of roast chicken breast |
17 |
Two cups of cooked broccoli |
5 |
Half an avocado |
4 |
Half a cup of rice |
24 |
Total |
50 |
For women with PCOS who are underweight, very lean, athletic, and not insulin-resistant, aim for an insulin count between sixty-five and ninety, as needed to support energy levels. You'll soon learn what feels best.
Table 9-9: Additional Foods and Insulin Counts for Lean PCOS—Non-Insulin Resistant
SAMPLE CHOICE |
INSULIN COUNT |
Six ounces roast chicken breast |
26 |
Two cups of cooked cauliflower |
12 |
Half an avocado |
4 |
Half a cup of rice |
24 |
One peach |
10 |
Total |
76 |
Adequate insulin is needed to support leptin levels in the brain. This is why the very low-carb approach is often unsuccessful in women with PCOS who are underweight, very lean, and non-insulin resistant. This is particularly true for those women who have difficulty gaining weight. Typical recommended eating plans for PCOS can actually make matters worse in this situation. In these cases, there is a predisposition to low leptin, and going too low on the insulin count can shock the hypothalamus and interfere with ovulation. I usually recommend adding extra protein for women such as this. As you’ll see in the next table, additional protein is included as well as ensuring that at least thirty-five points are achieved through carbohydrates at each meal.
Table 9-10: Sample Foods and Insulin Counts for Very Lean or Athletic Women with PCOS
SAMPLE CHOICE |
INSULIN COUNT |
175 grams roast chicken breast |
25.5 |
Two cups of cooked cauliflower |
20 |
One half of an avocado |
4 |
1 serving baked sweet potato fries |
37 |
Dessert: One peach |
9 |
Total |
95.5 |
Some very athletic women will need many more calories than this to support their activity level, so follow the same general structure for your meal and increase the amount of each food, but try to keep the composition approximately the same. Additional mini-meals and snacks should also be added as needed for very active women.
Again, this does not have to be exact, particularly in those who don’t need or want to lose weight, but it serves as a general guideline that can be followed. Over time, you’ll learn how to combine your foods for optimal insulin responses in your body—and your insulin sensitivity will gradually increase. In addition, there are always exceptions, and some of you may feel best at a higher or lower insulin count than your category indicates. I would tell you to listen to your body and adjust to what feels right for you!
For those who want to lose significant weight, it may be beneficial to determine your ideal intake with a nutritional practitioner, such as a naturopathic doctor, dietician, or nutritionist, as you’ll be able to get the personalized guidance you need along your journey.
Following are some guidelines for you as you plan your meals and snacks. I have included some recommended diets, along with sample recipes, for you in Appendix D. Also, please visit my page at http://www.drfionand.com/insulincount for calculators to help you with determining and tracking your insulin count.
According to research, a breakfast high in healthy fats is associated with metabolic benefits for the rest of the day.24 Because fats are low on the insulin index, you may find that a lower insulin count of 35–45 for breakfast may be beneficial, particularly if you are insulin resistant. As always, it’s important to listen to your body and do what feels best for you. Smoothies are a great option, as they are fast, easy, and nutritious. I always recommend the following format:
I’d like for you to think outside the box. Most women with PCOS can’t handle high carbohydrate loads very well, and most of our traditional breakfasts are carbohydrate based, so we need to think outside of traditional Western-style breakfasts and make choices that are healthy for us. I recommend having a serving of vegetables with each and every meal, including breakfast.
Eggs are a popular breakfast food, and to add vegetables, we can enjoy omelets with onions, peppers, mushrooms, and spinach for breakfast. Some other breakfast choices include—
As a general rule, you’ll want to portion your meals as already outlined. This should, as a general rule, produce a good insulin count. Choose a protein source approximately the size and thickness of the palm of your hand. Fill the rest of your plate with vegetables. Add a healthy fat source, such as avocado; some healthy oil, such as coconut oil, avocado oil, or extra virgin olive oil; or two tablespoons of nuts or seeds. Also, stop eating altogether after dinnertime. If you are hungry, have a glass of herbal tea, sparkling water with lemon, or even better, meditate, exercise, or read. This will produce a time of intermittent fasting which many report helps with weight loss.
Sometimes you won’t have time to make an elaborate meal. As such, you can make these quick meals in a matter of minutes that will be full of nutrition and will keep your blood sugar stable:
See Appendix D for a week’s meal plan with recipes.
Women with Mild to Significant Insulin Resistance
When it comes to snacking, it is always good to preplan your snacks and to avoid grazing outside of your snacking times. One morning and one afternoon snack with an insulin count of less than fifteen is ideal. Some women who are severely insulin resistant actually do far better avoiding snacking between meals, as this allows insulin levels to drop when not eating. Some examples include—
Women Who Are Non-Insulin Resistant, Athletic, or Underweight
It’s always best to preplan your snacks. However, if you feel hungry, you may add additional snacks as needed. One morning and one afternoon snack with an insulin count of around twenty is a good idea. Some examples of healthy snacks include—
All women with PCOS should have a snack within fifteen to twenty minutes of working out. This snack should be low in fat and contain carbohydrates and protein. An insulin count of around twenty to thirty is best. Some good examples include—
For women who are significantly insulin resistant and who find it very challenging to lose weight around the abdomen despite making dietary changes and exercising, intermittent fasting can help break this pattern. The most basic type of intermittent fasting involves fasting after dinner for a fourteen-hour span. In those who are severely insulin resistant, insulin levels can remain very high, and fasting allows the insulin levels to drop. Intermittent fasting is often an easy way to address the plateaus of weight loss resistance. Part of insulin’s action is to inhibit the breakdown of fat, but when levels are continuously high, as they are in insulin resistant people, the cells remain in storage mode. Each time we eat, our insulin levels rise again. Fasting gives the metabolic system a break, and it has no choice but to release stored fat. Intermittent fasting can range from hours to days. Please see the resources section or visit my website for more information.
Overall, this nutrition plan offers a lot of flexibility, as most types of healthy, whole foods can be included. Insulin counting gives you a method to manage the impact that foods are having on your PCOS by managing the single most aggravating nutritional factor to the condition: foods that spike insulin levels. When you eat well-structured meals as a habit, you’ll feel better. It also helps prevent disease and heals your metabolism. And when you choose whole, real, clean foods, you’ll be safeguarding not only your health but that of future generations as well. Two tablespoons of vinegar before meals and at bedtime may improve insulin sensitivity for those who are insulin resistant. Raw apple cider vinegar is a popular choice because it also contains fiber as a pectin.
This program is not meant to be a restrictive diet plan, but rather a new way of viewing food and nutrition for the betterment of your overall health. I hope that you’ll be able to take this information and use it as a stepping-stone to learning the most optimal way of eating for your unique expression of PCOS.