

Fully understanding how the human body digests gluten is very much a scientific work in progress. There is emerging science that is helping us understand why the body has a difficult time fully breaking down gluten. After millions of years of gluten-digesting evolution, the body knows exactly what it is doing when it comes to gluten, and contrary to what many believe, it is not a poison after all.
The latest science is suggesting that some of the gluten consumed may never have been intended to be fully digested. Many of the undigested gluten proteins are escorted into the large intestine, where they dramatically increase the numbers of beneficial gut bacteria. In one study, a gluten-rich diet increased certain enzymes in the large intestine called glutenases, which fully break down the gliadins found in gluten. Here in the large intestine, the gluten acted as a fuel supply for good gut microbes. These microbes were found to boost the production of beneficial short chain fatty acids (SCFA) like the butyric acid that I discussed in Chapter 3. The more gluten in the diet, the more glutanase activity and SCFA production they found. Extra gluten was found excreted in the stools.223
This study concluded that gluten digestion may have evolved to only be partially broken down in the small intestine in healthy people, in order to supply the large intestine with important food for the gut microbes. It seems that a major underlying factor causing wheat, dairy and food sensitivities is linked to the health of the upper digestion.223
When the lining of the small intestine is damaged, these undigested proteins can act as intestinal irritants and find their way into the lymphatic system where they are linked to numerous immune and health concerns. Protecting the integrity of the upper digestion and the intestinal skin is not a new concept. It has been the premise of Ayurveda for thousands of years, and a major focus of this book.
While some of the gluten ingested is earmarked to enter the large intestine, there are also numerous gluten-digesting enzymes and bacteria in the upper digestive system, suggesting that at least in part, gluten was a nutritional source to be broken down and absorbed through the small intestine as well.
![]()
According to a new study, the body starts digesting all of the very hard-to-digest gluten proteins as soon as we put it in our mouths. A multitude of gluten- and gliadin-degrading enzymes were found in normal human saliva that were manufactured by a variety of naturally-occurring oral bacteria.
![]()
The saliva, which is loaded with both the gluten-digesting enzymes and oral bacteria, is produced and swallowed in quantities of up to a liter a day. The oral bacteria and enzymes that are swallowed stay active in a wide pH range, suggesting that this gluten-digesting activity extends into the esophagus and small intestine.224
Not to mention the numerous microbes that can break down gluten, there are also naturally-occurring digestive enzymes in both the pancreas and duodenal mucosa, such as Dipeptidyl peptidase IV (DPP-IV) that break down the gliadins found in gluten and the casein found in dairy. Most active in the brush border of the duodenum, DPP-IV has been shown to completely break down proline-containing epitope of gliadin, the primary allergenic protein in gluten. DPP-IV has also been shown to markedly enhance the gluten- and casein-degrading capacity of other protein-digesting enzymes. This is the same enzyme that I discussed in Chapter 4, that can help break down undigested proteins like gluten and casein in the lymphatic systm.208, 209
All of these digestive enzymes, along with the gluten-digesting bacteria and probiotics I introduced in Chapter 1, depend on a balanced digestive system and the healthy lining of the stomach, small and large intestinal skin. This can be repaired, but first, let’s discuss how we got into this mess in the first place.
For the past forty-plus years, Americans ate fewer eggs and other animal products because the government concluded cholesterol and fat were bad for us. High cholesterol foods ended up on the government’s nutrient concern list28 based on a misinterpreted study on rabbits done in the early 1900s.225
As a result of this verdict against cholesterol, foods were manufactured without it. Animal fats like butter were considered unhealthy, eggs were taboo, fatty foods were replaced with non-fat foods and, overnight, America found itself on a pervasively low-fat, low-cholesterol, carbohydrate-heavy diet. The problem, unfortunately, was that this low-fat diet did not reduce cholesterol levels, nor did it reduce cardiovascular risk. In fact, this low-cholesterol diet took away the important fuel supply from the body that humans have been eating for thousands of years—saturated fat.
Our ancient hunter-gatherer ancestors dug up roots and gathered grains, greens, berries, and seeds, as well as hunted. And while our early ancestors were likely more prolific gatherers than hunters, there is no doubt that hunting was an extremely important part of our evolution as humans. Many researchers believe that our brain literally tripled in size with the ingestion of more saturated animal fats.226
In 1961, when these saturated fats were put on the government’s nutrient concern list and taken out of our diet for the very first time in thousands upon thousands of years,28 they were replaced by a different fuel supply. Wheat and corn replaced fat as the nation’s fuel supply, and in short order, America was fueled by sugar.65
Wheat and corn quickly became the new “it” foods in America.28, 65 They had obvious appeal in certain ways. They were cheap to grow and easily processed into foods that would sit on the shelves for months, as well as be easily processed into sugars like high-fructose corn syrup. Sugar packs a short burst of energy. It is fuel that helps you run away from a bear, get up a tree and save your life. However, sugar is not a sustaining fuel; it’s more of a rollercoaster ride. We burn it fast (“the sugar high”), and our blood sugar crashes after it’s all burned up.
Fats, on the other hand, are the preferred source of fuel for humans, as they provide long-lasting, stable, calm, non-emergency, sleep-through-the-night, handle-stress, no-anxiety fuel.
As a result of this switch to simple carbohydrates to replace fat, as a culture, we have lost our ability to stay calm and burn fat as a stable source of fuel. Consider this: More than a third of Americans are obese. We find ourselves with a global anxiety and depression problem. Kids cannot sit still in class, people cannot sleep through the night, and people cannot eat enough food to become satisfied. All of these can be linked to a diet high in sugar and low in good fat.
The unintended result of this low-cholesterol, high-sugar diet has set America up for an epidemic of blood sugar-related problems.227, 228 This problem has been blamed on gluten, but as we saw in Chapters 1 and 2, there is plenty of science to the contrary. Gluten-free foods are poised to take the pre-diabetic epidemic to an even more dangerous height. Most of the gluten-free foods are highly processed, hard to find completely organic and rendered with a higher glycemic index than unprocessed whole wheat breads.229, 230 Intestinal permeability and leaky gut has been linked to the processed foods in our diet, so please beware that it is likely the processed nature of our diet in the U.S.—which is much more processed than the food supply in Europe231—that is behind so many food sensitivities and food intolerances.232
Thankfully, in 2014, the governmental committee that develops the country’s dietary guidelines lifted their low-fat diet recommendation. In 2015, longstanding caps on dietary cholesterol were removed, stating there was “no appreciable relationship” between blood cholesterol and dietary cholesterol. The low-fat, no cholesterol era has finally ended!28
Without adequate cholesterol and fat in the diet, the gallbladder can become sluggish, as it requires a certain amount of fat to exercise itself and stay functional. In one study, it was suggested that the leading cause of gallbladder disease is, in fact, a highly touted low-fat diet.233 The U.S. has been on a poor-quality-fat diet for almost 50 years, and slowly we have seen a steady rise in gallbladder issues,234 which are directly linked to both a weak lower and upper digestion.
It is interesting to note that we have a record number of gallbladder surgeries in America. Most people don’t even have to change their diet after they have their gallbladder removed, suggesting that maybe we don’t really need the gallbladder anymore. Perhaps we’ve actually evolved away from needing the little storage sac of bile called the gallbladder.
I would like you to reconsider any notion you may have that the gallbladder is unimportant or expendable. The reality is that the gallbladder holds a sack of bile that is 15 times the concentration of the bile produced from the liver.203, 235
Considering our ancient ancestors, it might be logical to deduce that this kind of bile production was used to digest, perhaps, the brains and the intestines of a woolly mammoth. Eating such large amounts of fat in one sitting followed by periods of no fat tends to force the gallbladder to contract in a major way, decongesting any possible bile and liver congestion.
Today, we have just the opposite problem. We find ourselves with either inadequate amounts of good fats or an abundance of indigestible processed fats in order to produce an adequate amount of bile. As a result, the bile that is reabsorbed from the intestines to the liver is reused on average up to 17 times before it is discarded. It’s like washing our dishes in the same dirty dishwater 17 times in a row!203
The reason why the bile would be reused so often was likely a survival tool in times of famine. When fats were scarce, humans had the ability to reuse bile again and again until hunters brought a new supply of fatty meat. As a result, today we have 94 percent of our bile—with all the toxins in tow—being reabsorbed back to the liver,203 circulating toxins back into the bloodstream where they oxidize our good cholesterol and are potentially being stored in our fat cells and even our brains.23-27
It is this lack of bile flow and bile production that is a major contributor of the slow and steady shutting down of the production of stomach acid. The lack of stomach acid and its coordination with the liver, gallbladder, pancreas and duodenum all contribute to our inability to digest hard-to-digest foods like wheat and dairy.
Lack of bile flow is also responsible for the consistency of the stools. It is the bile that regulates the stool. Plain and simple: No bile, no poop. No bile, no stomach acid. Thus, one can experience poor and painful digestion of wheat, dairy, and fatty foods.
Note: Before you start increasing the fats in your diet, you must first stop eating sugar, processed foods and reboot the function of the gallbladder. More on this in Part II.
Let’s take a journey through one person’s digestive system to better understand exactly how it can weaken and break down, and what can be done to resolve these issues and heal from the inside out. This is the story of Daniel,3 a patient who came to see me in 2014.
Daniel came to see me complaining of anxiety, chest pain, and shortness of breath. When a patient shares symptoms like these, I immediately recommend they get checked out by a cardiologist, and then I do my best to dig into the cause of the problem.
Getting Acquainted with Your Digestive Anatomy
Daniel had a history of constipation as a child, which had become chronic, and was now experiencing alternating bouts of constipation, diarrhea, and mucus in the stool. He also complained about heartburn, gas and bloating, and years of indigestion.
He told me he had stopped eating fatty or fried food and any heavy or rich food, for that matter years ago, because it would make his heartburn worse. He would either end up with a feeling of nausea or the food would just sit there like a rock.
In an attempt to solve his digestive issues, he told me he had experimented with taking foods out of his diet. First, he removed most fatty foods, then wheat and dairy. Like Mary, he reported feeling somewhat better each time he took another food group out of his diet. While each food elimination worked for a time, the symptoms kept returning.
Daniel was like so many of my patients. He experienced an initial benefit in removing wheat and dairy, but the benefit didn’t last. The symptoms return even without these foods. This is not to say that wheat and dairy will not exacerbate such symptoms, they often do, which is why so many people understandably choose to avoid these foods. But once again, this elimination approach to food sensitivities treats the effect, the symptoms, when we need to be treating the cause in order to stay healthy and prevent more serious health concerns in the future.
After years of adjusting his diet and eliminating more and more foods, Daniel began to experience bouts of anxiety, chest pain, and shortness of breath, which is when he came to see me. What is interesting about all of Daniel’s symptoms is that they’re all linked to an underlying digestive imbalance. The body never does anything without a good reason. Each symptom is a logical expression of the body trying to deal with a history of constipation and resultant lymph congestion. Each symptom represents the body trying to move impurities out through alternative detoxification pathways other than its main, clogged waste removal channels.
In Daniel’s case, the history of constipation caused chronic dryness in the intestinal mucous membranes. The intestinal skin, like the respiratory skin, cannot be too dry or too wet with mucus.236 The conditions have to be just right for the microbes that support optimal health to proliferate and for the neurotransmitters manufactured in the gut to stabilize mood and support the nervous system.237-252
If the intestinal tract becomes too dry or too wet, the villi and lacteals of the intestinal wall can break down, predisposing the intestinal tract to irritation, damage, and a type of leaky gut syndrome that allows these toxins and hard-to-digest proteins to enter the body’s lymphatic system, creating the perfect storm for food intolerances.236, 253-255
When the skin of the intestinal tract breaks down and toxins cannot be removed through the congested intestinal lymphatics (where many of the gluten symptoms first manifest), the toxins will eventually be redirected through the enteric cycle back to the liver.
The liver’s job is to break down fats and toxins that have been processed through the intestines and lymphatic system, and to gobble them up with bile.
Bile is like a Pac-Man inside the liver, gobbling up toxins, fatty acids, environmental pollutants, pesticides, cholesterol, and other fatty impurities. When we ingest fatty foods, for instance, the bile is secreted from the liver and gallbladder into the intestinal tract, where it continues to gobble up more of the same—toxins, fatty acids, environmental pollutants, preservatives, chemicals, parasites, and other undesirable bacteria, just to name a few.256
Once the bile gets into the intestinal tract, it attaches itself to fiber in the gut and is escorted to the toilet with all the toxins in tow. This is a wonderfully efficient process of removing waste, as long as we have enough fiber in our diet to get the job done.
Our hunter-gatherer ancestors ate about 100 grams of fiber each day. The average American has 15–20 grams of fiber in their diet each day.257 So as a result, our ancestors had about 5 times more fiber in their diet than we do, and therefore had at least 5 times the efficiency of fat-soluble waste removal than we do. Bile, which is attached to numerous toxins, will be reabsorbed back into the liver, back into circulation, instead of being eliminated and escorted into the toilet if we have an inadequate amount of fiber in our diet.
Once the liver becomes overwhelmed with detoxification projects, such as dealing with recirculated toxic bile, the liver can become congested and these toxic fats can literally build up in the liver, causing a well-known condition called “fatty liver” while oxidizing or damaging the good healthy cholesterols. Oxidized cholesterol particles are now understood to be the real culprit of the cholesterol-based cardiovascular risk. More importantly, the congestion in the liver can cause a lack of bile production, a lack of bile flow, and a thickening or increased viscosity of the bile itself. Thick, viscous bile can congest the bile ducts and literally turn off the digestive process and the ability to break down wheat and dairy.258
![]()
Thick, viscous bile is an extremely common condition in America. Thick bile can result in an inability for the body to digest fats well. In the case study above, Daniel had a history of constipation where the intestinal wall was unable to process waste efficiently through the intestinal lymphatic tissue, and therefore his body was defaulting these toxins back to the liver.
![]()
Once Daniel’s liver became congested and his bile became thick, he was unable to digest fatty foods. Being able to digest and deliver good fats to the brain, heart, skin and nervous system is critically important. Over time, lack of healthy fat metabolism can cause an inability to keep the nervous system stable and predisposes many people to anxiety and other stress-related concerns, similar to what Daniel was experiencing.259
When Daniel did eat some fatty food, and there was insufficient bile to break it down, the stomach chose to hold onto the fats and wait for the bile to be produced. In Daniel’s case, the constipation and bile congestion became chronic, leaving Daniel with an inadequate supply of bile to break down fats. As a result, the stomach was holding onto the fats longer than it should’ve, and Daniel would feel nauseous and heavy. Without adequate bile to digest a fatty meal, the heavy or fatty foods would just sit there like a rock and not digest— sound familiar?
Avoiding fatty foods was Daniel’s initial solution to this problem, but it didn’t last. Here is why:
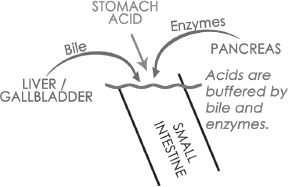
The bile in the gallbladder and liver not only emulsifies fats, but it also buffers acids such as the hydrochloric acid (HCl) in the stomach. When the stomach is trying to break down hard-to-digest proteins like gluten in wheat and the casein in dairy, it requires a very strong production of stomach acid.
If there is limited bile production in the liver, the stomach will sometimes hold onto the excess acid, as if to wait for the bile to be produced in order to buffer the harsh stomach acids. This is a very common cause for experiencing symptoms of heartburn. According to a recent survey, 44 percent of Americans experience heartburn at least once a month, and about 7 percent or 22 million Americans experience a daily bout of heartburn.260, 261
In some cases, the stomach will allow the acids to leave the stomach in an attempt to protect the stomach lining from excess acid. When this happens without adequate bile to buffer those acids, the acids may burn and damage the intestinal wall, causing duodenal ulcers, intestinal irritation, leaky gut, and a detrimental alteration in the intestinal microbiology. Unbuffered acids from the stomach moving into the intestinal tract could cause severe intestinal inflammatory symptoms, which would make the intestinal tract and lymphatic system even more vulnerable and susceptible to being irritated by hard-to-digest or undigested proteins from wheat and dairy.
The stomach will try its best to hold onto the stomach acid for as long as possible, but in time, the excess acid will irritate the stomach lining, setting the body up for chronic gas, bloating, indigestion and bouts of nausea, heartburn and shortness of breath, as seen in Daniel’s case. Daniel’s history of constipation may have caused congestion of the liver and gallbladder, compromising bile flow, the ability to digest fats and the inability to effectively buffer the stomach’s digestive acids.262
Intestinal irritation from a lack of bile flow or the passing of unbuffered stomach acids into the intestines can also cause bouts of diarrhea with mucus either lining the stool or mixed into the looser stool, which we saw in Daniel’s case history. Mucus production in the stool is common and often caused by excessive stress and worry along with the breakdown of the upper digestive process.
When the stomach is pushing so persistently in an upward direction onto the diaphragm that the stomach literally herniates through the lower esophageal sphincter and the diaphragmatic wall, it’s considered a “hiatal hernia.” The stomach is designed to hang down off the diaphragm and not push up against it. This kind of chronic upward pushing of the stomach onto the diaphragm is common, and can be the result of poor bile flow and the delayed emptying of the stomach acids and fats as I previously described. Pregnancy can also exacerbate this tendency, as the baby naturally puts upward pressure on the stomach and diaphragm.263 Normally, after delivery, the stomach returns to its original position, but many women never feel quite the same after they have had their babies, and this may be why.
In the case of a hiatal hernia, for example, the upward pressure took years for the stomach to actually herniate through the lower esophageal sphincter of the diaphragm. Years before the stomach herniates, bouts of chronic heartburn and indigestion could be putting undue pressure on the diaphragm and sometimes even adhering parts of the stomach wall to the underside of the diaphragm. As you might expect, when this happens, neither the stomach nor diaphragm can function well and this area can become very tight and tender. Unfortunately, this is extremely common in my patients with food intolerances. (In Chapter 10, I will share a home exercise called “stomach pulling” to help resolve this problem.)
 Tip: Check for soreness, tightness or pain on the abdomen, just under the ribs or both sides.
Tip: Check for soreness, tightness or pain on the abdomen, just under the ribs or both sides.
As a result of Daniel’s long-standing constipation, toxins were reabsorbed back into the liver where his bile ducts became congested, resulting in the holding on to stomach acid and heartburn. Daniel was a tricky case, because not only did we need to free up his stomach and diaphragm, we needed to decongest his bile ducts and bring his elimination back into balance. I will how to do this, step by step, in Part II.
In Daniel’s case, the diaphragm itself became unable to fully contract and pull air deeply into the lower lobes of the lungs. This is important because the lower lobes of the lungs are where a predominance of parasympathetic nerve receptors is located. When we breathe deeply into the lower lobes of the lungs, we activate the calming, rest-and-digest parasympathetic nervous system. When we lose access to the lower lobes of the lungs, the tendency is to breathe only into the upper lobes, where there is a predominance of fight-or-flight nerve receptors.264, 265
Commonly, this can be the cause of chest pressure and difficulty breathing, as we saw in Daniel’s case. In this case, it is also common to experience yourself frequently trying to catch your breath, getting side aches when you run, feeling out of shape, and this can even contribute to asthma, allergies, snoring and sleep apnea. There are also lymph vessels that drain the lungs and respiratory system that, when congested as a result of digestive imbalance, can be linked to a host of congestive respiratory concerns.266 Yoga and backward stretches that open the chest and stomach area helped Daniel resolve his breathing and chest pressure considerably. I will describe these in Chapter 13.
Over time, the stomach lining can become irritated, inflamed, and even ulcerated from the HCl build-up that is lingering in the stomach due to poor or congested bile flow. In an attempt to protect itself from the lingering HCl, the stomach can make an executive decision to turn down the stomach fire, decreasing the production of stomach acid to match the lack of production of bile in the liver and gallbladder.
![]()
If there is inadequate production of bile, there will be a lack of production of stomach acid.262 Without adequate production of stomach acid, hard-to-digest proteins like gluten and dairy will simply not be initially digested and broken down.
![]()
In 91 percent of people, the bile duct and the pancreatic duct join together before they enter into the small intestine.203 If the bile ducts have become congested, as in Daniel’s case, and like I commonly see in my practice, the pancreatic ducts will also become congested, blocking pancreatic digestive enzymes from moving into the intestinal tract to support the buffering of stomach acids and the breaking down of hard-to-digest foods.
There is a coordinated effort between the stomach producing the appropriate amount of HCl that triggers the release of bile, which triggers the release of pancreatic enzymes, which triggers release of the duodenal enzymes. All of these are required to create the perfect environment for the intestinal microbiology to proliferate. When both intestinal environment and upper digestion are healthy and the digestive process is coordinated, only then are elements required for a healthy microbiome and the digestion of wheat and dairy in place.
Many of my patients find benefit from taking digestive enzymes. Many naturopaths and medical professionals suggest that, as we age, we simply stop producing digestive acid in the stomach, bile flow in the liver, and pancreatic enzymes from the pancreas. Others find themselves propping up their weak digestion by taking HCl pills, pancreatic enzyme pills, and herbal laxative pills to keep their digestive system moving along.
The reality is that the vast majority of Americans have thick, viscous bile as a result of eating highly processed food over many years. This has not only congested the bile and pancreatic ducts, but has shut down the optimal production of acid in the stomach—all of which are required to detox and digest well. When the bile becomes thick and the bile ducts congested, the pancreatic duct also becomes blocked. Pancreatic digestive enzymes simply cannot get through the congested bile ducts to do their job. As a result, you may reach for digestive enzymes. This may help alleviate the symptoms, but as you can see, once again we are only treating the symptoms and not the cause of the issue, which can set us up for other health issues down the road.
Instead of investing in digestive enzymes or other digestive aids, consider a more efficient and long-term plan to target the root cause—your digestion.
Read on to discover how I helped Daniel stimulate bile flow, and strengthen and balance weak digestion in Part II of this book. It is time to take action and reboot your digestion so you can once again—or perhaps for the first time that you can remember—enjoy your bread and butter!
__________________
3 All names of patients have been changed throughout this book to protect their privacy, and all patients have given permission to share the story of their health journey in this book.