Viruses display remarkable biological intelligence. They not only cause health conditions and diseases resulting in tissue and organ damage, but as AIDS has shown us, they can disable the immune system itself. Why this happens is still unknown. However, when explored from the evolutionary perspective and the standpoint of energy medicine, answers begin to fall into place and a larger picture emerges that makes more sense than any simplistic germ theory.
This book is not only about viral illnesses but is also about a new paradigm in medical thinking. Therefore in this chapter, alongside the basic, important traditional immunology principles, are the latest concepts about immune function, coupled with evolutionary ideas and principles of energey medicine. These new ideas provide a better theoretical framework in which to understand the principles behind natural alternative antiviral therapies.
The Earth is far from sterile. In fact, we live in a thick biological soup of highly active, aggressive, competitive, and potentially life-threatening microorganisms and chemical substances. Most are naturally occurring and others are manmade. These recently manmade substances are disrupting and challenging a human immune system that has adapted over hundreds of thousands of years to only naturally occurring compounds and organisms. Yet, in only a few hundred years' time, chemical toxic substances have permeated the Earth's atmosphere, crust, ice caps, and water systems, and entered into the food chain to such a degree that some researchers and clinicians, including myself, believe these substances are, to a large degree part of the cause of the current immune deficiency crisis.
If immune dysfunction is caused by modern living, then we must also change the way we live and work. I suggest that we gradually begin to make improvements in the way we live, while enhancing our immune systems with natural substances in the meantime.
So we are faced with a dilemma. There is no doubt that viral diseases are increasing, but do we try to kill the viral invaders or enhance our immunity? If immune dysfunction is caused by modern living, then we must also change the way we live and work—a proposition that is much more difficult to accomplish than to talk about. As the Chinese saying goes, “A journey of a thousand miles begins with a single step,” so I suggest that we gradually begin to make improvements in the way we live, while enhancing our immune systems with natural substances in the meantime.
For those with active viral disease, it is important to manage or reduce the viral load in the body using natural antiviral medications and perhaps even through the wise use of pharmaceutical antivirals. In the end, if we proceed intelligently, diligently, and with significant care, we will arrive at our destination: improved health for ourselves, families, loved ones, and society.
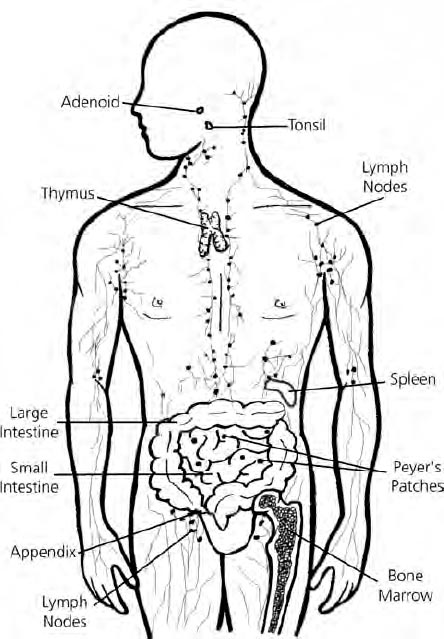
A healthy, well-functioning immune system is a marvel of natural microbiology, physics, and biochemistry (see figure 3-1). Without it, we could not survive for even the shortest period of time on this planet. Every living organism, from animals to plants, has an immune system—each with differences that promote individual survival and health.
Conventional medical immunology identifies several organs that play important roles in the immune system. These are the thymus gland, lymph nodes, spleen, and Peyer's patches in the intestine. Newer models expand this view and include the gut-associated lymphoid tissue (GALT), which includes the appendix as well as the Peyer's patches. Similar groups of tissue protect the lungs and are called bronchial-associated lymphoid tissue (BALT), and the lungs' mucus lining called mucosal-associated lymphoid tissue (MALT). Since all immune cells originate in the bone marrow, it is also considered an immune tissue.
From the viewpoint of functional medicine and naturopathy, insofar as these glands and tissues contribute to the origin and development of mature immune cells, their function is regarded as vital for immune enhancement and general health. Liver detoxification to assist in the removal of toxins from the body, colon cleansing to improve GALT function, lymphatic cleansing, and thymus support are necessary elements of a complete immune-enhancing program.
Figure 3-1: The Human Immune System
Organs, glands, tissues, and vessels of the human immune system.
Immunology is the scientific study of the immune system, and entails the mechanisms by which the body maintains its biochemical identity and defends itself and survives against infectious agents, including viruses, and other foreign substances like toxic chemicals. Medical immunology is concerned with immune related diseases and with substances that affect the immune system and treat the body against infectious microorganisms.
Like most of modern science, those who study immunology do not focus on the whole system, but on the ways in which particular types of cells defend the body by means of recognition and elimination of foreign microbes and other substances. It is a brilliant science of microscopic parts, but it tends to proceed without any sense of how the immune system works as a unified whole.
Traditional immunology is based on a mechanistic model developed in the 1930s and '40s, which originated from studies by Ilya Ilyich Metchnikoff (1845–1916), the Russian who shared the Nobel Prize in Physiology and Medicine in 1908 with Paul Ehrlich for their work on how the body rids itself of foreign particles. According to this model, the immune system is a reactive mechanism designed to defend the body against invading microorganisms, foreign materials, and objects that include pollens, chemicals, dust, animal dander, particles of soot or sand, and toxic chemicals.
In 1960, the Nobel Prize in Physiology and Medicine was jointly awarded to Sir Frank Macfarlane Burnet and Peter Brian Medawar for the discovery of acquired immunological tolerance, a discovery which set the tone for modern immunology. For several decades, their conclusions that there were two immune systems—one innate, the other acquired, and that newborns had immature immunity—remained unchallenged.
Then, in the late 1990s, Marcella Sarzotti-Kelsoe, Ph.D., of the Baltimore Veterans Affairs Medical Center found that newborns in fact did have fully competent immune systems. These findings called for a reinterpretation of the Burnet and Medawar theories, and other scientists followed the call. The immune system began to look more like a continuum with multiple interconnections than a system with two separate mechanical parts.
Another principle of traditional immunology is that the immune system is able to maintain a distinct division between individuals and species, between the individual organism and the environment by distinguishing self from non-self. This recognition ability was considered a key concept in immunology for nearly a century. Not any longer.
Polly Matzinger, Ph.D., of the National Institute of Allergy and Infectious Diseases, found that this kind of classification was limiting and did not fully describe how the immune system worked. Matzinger said that the old theory of a clear division between self and non-self “made it virtually impossible to uncover the rule by which the immune system could make the necessary distinctions” (Matzinger 2001) to function properly. In her view, the immune system is much more complicated. It responds to the vast array of infectious agents, chemicals, and the changing nature of the environment through equal complexity.
Like clinical medicine, traditional immunologists used war analogies to explain their theories: the immune system is like a “double edged sword”; it maintains “first- and second-line defenses”; it is a surveillance system that “guards” and “fights” against “invading” germs; it either “wins” or is “defeated.”
This linear, battle-based way of thinking produces a limited model, in which individual parts are first discovered and studied, then theories are invented afterwards in an attempt to figure out how the parts work. Linear models can never fully explain how a complex system operates and cannot completely accommodate nuances, individual differences, variety, or evolutionary changes that take place continuously in all living systems.
Nature, on the other hand, favors balance rather than superior “firepower.” Careful observation reveals that the body dislikes extremes and that pushing it beyond its limits results in ill health. Disrupting the immune system with unnatural toxic chemicals and the exhaustion of vital metabolic and hormonal reserves due to stress and aging further deplete our immune systems' ability to function.
Charles A. Janeway, M.D., of Yale University School of Medicine, suggests that the immune system is more of a “sensory system.” He effectively challenges the idea that the innate immune response is limited to inflammation and simple cellular “search and destroy operations,” like a war machine. In his model, the old idea that innate immunity is nothing more than a rudimentary, evolutionary, kneejerk reaction to an invading non-self organism gives way to the idea that the immune response is a powerful screening mechanism that includes intricate cellular communications, more like a powerful computer antivirus program that continuously monitors your system for abnormal changes and alerts you when things go wrong.
However, to be fair, no matter how linear the current model is, we have learned much about immunity through the study of cellular microbiology. In fact, the more we learn, the more complex it all seems and the more the immune system is appreciated as an integrated, intelligent biosystem. Most contemporary immunology researchers are now well aware of and accept the paradoxical tendencies the immune system demonstrates. For example: immunity is influenced by mood as well as infections; it can display hyperimmune states at the same time as immune-deficient ones. We truly exist in a biochemically interconnected ecological matrix where complexity is the norm rather than the exception.
In light of this discussion, one of my patients comes to mind. A young woman in her late twenties, Beth had advanced rheumatoid arthritis. Besides severe crippling joint pain and swelling, she had allergies and recurrent infections. Her inflammatory symptoms were suppressed with steroid drugs, which depressed her immune system and led to chronic bacterial sinusitis, recurrent colds, and viral infections. When I first saw her, Beth was continuously on antibiotics to treat the sinus infections, which caused constant vaginal yeast infections. Still, her body adapted, and she heroically survived. Though the drugs did not cure her condition or reduce the daily experience of constant pain, they helped her live a relatively normal life that included a marriage and job.
When she first came to see me, Beth immediately asked if stress had anything to do with her condition because she noticed that the symptoms waxed and waned based on her stress levels. I explained that the immune system responds to changes in hormone and neurotransmitter levels due to stress, which can vary with menstrual rhythms. Beth was amazed at how complex her body was.
By applying techniques to regulate the immune system, many of which are described in part 2, Beth was able to reduce her use of steroids to a minimum and eventually to eliminate them altogether, allowing her natural immunity to recover. Her sinus infections cleared completely and she stopped getting colds every few weeks. Antibiotics became unnecessary, and consequently her yeast infections disappeared. Acupuncture treatments and herbal medicines helped to manage her pain and joint inflammation and she was eventually able to eliminate all anti-rheumatic drugs as well. Beth had an autoimmune condition complicated by immune deficiency, but natural therapies helped restore balance to her immune system.
The classical view of immunity divides the immune system into two parts with different lines of defense: nonspecific or innate immunity, and specific or adaptive immunity. Each part has various components and characteristics that contribute to its effectiveness. Since the conventional model still serves as a good starting point in understanding the basic function of the immune system, in this section I will explain the most important components of innate immunity. In the next chapter, I will discuss the innate immune response in more detail and why I consider it one of the most important, and most overlooked, aspects of the current immune crisis. Later in this chapter I discuss specific immunity.
According to the traditional model, the body's first line of defense is the innate immune response. Its essential characteristic is to distinguish between self and non-self, to protect us (“self”) from microbes (“non-self”). Its principle challenge is to detect and then mount a rapid and effective defense against any invading pathogen (microorganisms such as bacteria, parasites, or viruses that cause disease) or antigen (any foreign substance, like pollen, that causes allergies, or otherwise stimulates an immune response).1
The skin is the first barrier against microorganisms, and most types cannot enter healthy unbroken skin. That is one of the reasons why it is important to keep even minor wounds clean and covered, especially when in contact with others who harbor infections.
Innate immunity (also called natural or native) is what we are born with. In the newborn, it is augmented by its mother's mature immunity and is conferred in the colostrum of the first breast milk. That is why breast-feeding for at least a few months is so important to an infant's natural immunity and, sometimes, survival.
The components of innate immunity include physical and chemical barriers that prevent microorganisms from entering the body, as well as specific cells that are on the prowl to eliminate them if they gain access to the body, or so to speak, if they get under your skin. Let's examine these barriers and cells.
Physical and Chemical Barriers: The skin is the first barrier against microorganisms, and most types cannot enter healthy unbroken skin. That is one of the reasons why it is important to keep even minor wounds clean and covered, especially when in contact with others who harbor infections; some microbes can enter directly into the bloodstream through broken skin.
Not only does the skin act as a physical barrier, its secretions serve as a chemical deterrent to pathogens as well. The acidic pH of sweat, unsaturated fatty acid secretions of the sebaceous glands, and enzymes called lysozymes that occur in tears and sweat are natural antiseptics that help to keep the skin free of pathogenic organisms. Even the salt in sweat is mildly antibacterial.
Regular bathing and routine hand washing remove dirt and bacteria from our bodies. However, overly washing one's hands with strong antibacterial soaps may produce more trouble than benefit. Sterilizing everything in sight and trying to get rid of all bacteria is not necessary, and may eliminate some helpful germs in the process. Ordinary soap and regular hand washing before preparing food and after using the restroom are adequate.
Other common areas by which germs, allergens, and pollutants enter the body are the nose, throat, and lungs, through the mouth and the digestive tract, and through the rectum, urinary tract, and sex organs. Natural methods of protection operate in all of these areas of the body. For example, the mucous lining of the respiratory and gastrointestinal tracts trap and remove microorganisms and are expelled in phlegm. One public health measure of earlier days used to be the prohibition of spitting and the removal of spittoons from public buildings. Many microorganisms are also caught on their way to the lungs in the nose and throat by the adenoids and tonsils, both of which are lymphatic glands important to first-line immunity.
The indiscriminate, and often unnecessary, surgical removal of these glands does not solve the underlying immunological problem that caused them to be swollen and diseased in the first place. Often, after a short period of improvement, it leads to chronic allergy problems. If the microorganisms get past the tonsils and adenoids, ciliated microfilaments lining the upper passages of the lungs remove them in secreted phlegm; they do this in a wavelike fashion, much like firemen of an earlier time on a bucket brigade.
Enzymes in the saliva, stomach, and small intestine, along with the acidic pH of the stomach, manage to kill most microbes upon contact. Friendly bacteria, like Staphylococcus albus on the skin, Streptococcus viridans in the throat, and numerous naturally occurring bacteria in the colon, like Lactobacillus acidophilus,2 have a powerful effect on maintaining healthy immune status. In fact, the lower gastrointestinal tract contains the greatest number of immune cells in the body. Urination causes regular flushing of bacteria from the urinary tract, and the acidic pH of the vagina prevents colonization of it by yeast and fungi, as well as by bacteria and viruses.
Phagocytosis: Besides physical, mechanical, and chemical means of preventing microorganisms from entering the body, innate immunity also has cellular defenses. This next line of defense consists of specialized immune cells that destroy the invader once it has entered the body. The destruction of foreign cells inside the body is called phagocytosis, which means the “eating of cells.”
All the immune cells spend at least some part or all of their lives in the bloodstream, but before they enter the blood they are created in the bone marrow, which also produces red cells (erythrocytes, cells that carry oxygen), platelets (cells that control bleeding), and the white cells (leukocytes). It is the white cells and their secretions that make up the main components of the immune system. The importance of the white cells may be seen in the diversity of types compared to that of red cells and platelets. There is only one type of red cell and one type of platelet, but more than eight types (or subtypes) of white cells (see figure 3-2).
Figure 3-2: Cells of the Immune System
All cells of the immune system originate in the bone marrow from one hematopoietic stem cell, a self-renewing parent cell involved in the generation of blood cells. This cell divides to produce two specialize types of stem cells: a lymphoid stem cell, which creates T and B lymphocytes and natural killer cells, and a myeloid stem cell. From the common myeloid stem cell arise white blood cells (basophils, eosinophils, neutrophils, and monocytes), red blood cells (erythrocytes), and platelets, which are important in blood clotting. Mast cells are important in allergic responses and macrophages are involved in tissue defense.
References: Janeway, Charles A., et al. Immunobiology; Roitt, Ivan, et al. Immunology; Benjamini, Eli, et al. Immunology, A Short Course.
White cells, or leukocytes, consist of neutrophils, basophils, eosinophils, monocytes, and lymphocytes. Two of these are phagocytic cells: neutrophils and monocytes, which in their mature form are called macrophages. Neutrophils are also called segmented neutrophils or segs. They belong to a group called polymorphonucelar leukocytes, or polys, or simply PMNs, a group that also includes basophils and eosinophils. Phagocytic cells engulf and ingest foreign particles and microorganisms. Once they are ingested, the phagocytes secrete powerful enzymes to digest these particles, and metabolize and remove them from the system, essentially cleaning up after themselves.
These first-line phagocytic cells effectively identify and neutralize the invading particle without overly disturbing the host, your body. They are positioned strategically in areas of the body where they encounter the greatest numbers of microbes and offer the most protection for organs, such as the liver, vulnerable to infection. Besides removing microbes and their toxins, macrophages continuously scavenge dead or worn-out cells. The main sites in the body where macrophages are found in abundance are the Kupffer cells in the liver, the red pulp of the spleen, and the airways of the lungs.
Besides phagocytosis, infection also triggers macrophages to release cytokines. These increase the permeability of blood vessels, allowing fluids, proteins, and immune cells to pass into the damaged tissue area. This process is part of the inflammatory aspect of immunity (discussed in more detail in the next chapter).
Neutrophils are like the pawns on a chessboard. They are so numerous that nearly 60 percent of bone marrow activity is spent producing them, and they make up 50 to 70 percent of all white cells. Once manufactured by the bone marrow, neutrophils continuously circulate in the blood on the lookout for foreign particles.
Neutrophils are short-lived cells that engulf substances, destroy them, and then die. Besides participating in phagocytosis, neutrophils perform a variety of biochemical activities against microorganisms, including production of peroxide and superoxide radicals that act as germ-killing toxic oxidants and the manufacture of lactoferrin, that inhibits bacterial growth by binding up (chelating) iron, thereby with-holding it from iron-hungry bacteria. They also contribute to the destruction of microbes through the production of nitric oxide (a free radical gas). This is a cellular metabolic process also important in many chronic degenerative diseases, so defects in neutrophil function or production often manifest as chronic or recurrent infections.
Monocytes are also phagocytic, but unlike the free-swimming neutrophils, these cells reside in organs, tissues, and specialized cavities in the body, waiting for action there. Their numbers are much smaller than neutrophils, comprising 2–8 percent of white cells. After being produced in the marrow they circulate in the bloodstream for about a day and then settle in their chosen “lairs.” Once there, they differentiate further into specific forms called tissue macrophages or histiocytes. Immunologists give these cells specialized names depending on their site of activity, such as Kupffer cells in the liver, alveolar macrophages in the lungs, microphial cells in the central nervous system, and splenic macrophages in the spleen.
Macrophages lie in wait until activated by any of a variety of physical and biochemical stimuli. Like neutrophils, activated macrophages release an immense range of biologically active chemicals as the immune response. Macrophages are part of the reticuloendothelial system, a group of tissue-based cells that filter and remove debris from the blood, and make up an important part of the first line defense strategy of the immune system in eliminating bacteria and parasites. Macrophages also prepare and mark partially digested cells for further destruction, a process called antigen-presenting.
Natural Killer Cells: Natural killer (NK) cells, a type of cytotoxic cell (toxic to other cells), are a specialized group of lymphocytes responsible for destroying virus-infected cells and cancer cells, as well as cells infected with bacteria and protozoa. NK cells compose between 5–16 percent of the total number of lymphocytes. Very little is known about exactly how NK cells work, but we do know they play an important role in recognizing and eliminating cancer cells in the early stages of cancer growth and in killing viruses. They also contribute to immune activity by secreting various cytokines, primarily interferon.
Since viruses invade and take up residence inside cells, the regular phagocytic cells (neutrophils and macrophages) are unable to get at the viral particle, so the immune system provides an alternative method: NK cells. These release biological weapons against the parasitic virion. They bind to the infected cell and release chemicals that destroy the cellular membrane, causing the target cell to burst. Other immune cells then clean up the cellular debris.
NK cells are particularly important in controlling recurrent herpes viral infections, such as EBV, CMV, and VZV. Natural killer cell numbers tend to be low in chronic viral disease, such as herpes, and in many cancers. This may suggest either that they are being used up in the immune system's attempt to manage the condition, or that lower than normal levels allowed the condition in the first place. We still do not know enough about how the immune system works to interpret much of the clinical information we are able to collect.
NK cell levels and function are affected by a variety of nutritional deficiencies, including protein and overall caloric deficiencies, low levels of vitamins C, E, and D, and of trace minerals such as zinc and magnesium. Toxic metals, like lead, and other noxious environmental substances can depress NK cell levels. Numerous natural immune-modulating substances, such as transfer factor and the mushroom glucans, can increase the number of NK cells. These (and other substances discussed in part 2) are important medications that improve immune function and should play a central role in any plan to rid the body of viral disease.
Biologically Active Immune Substances: Current research has shown that many tissues and immune cells produce a large variety of biochemical substances harmful to microorganisms. These include enzymes, free radicals,3 acids, growth inhibitors, fever-producing pyrogens, tumor necrosis factor, interleukins, and interferons. Macrophages produce interleukin-1 (IL-1) that stimulates helper T lymphocytes. Macrophages also produce tumor necrosis factor that kills cancer cells and helps regulate other immune functions. Alpha interferon is produced by lymphocytes and it also increases NK cell activity.
Circulating Protein Substances: Protein substances circulating in the blood form the complement system4 that recognizes microbes and is involved in the development of inflammation. Paul Ehrlich, winner of the Nobel Prize in Medicine in 1908, described an activity in the blood that assisted, or complemented, the ability of other immune components to destroy bacteria. He was the first to use the term “complement” in this context. The activity of the complement system promotes the killing of microbes, facilitates the clearing of immune complexes that have become unnecessary, and enhances antibody responses. Like many immune complexes, complement can also cause harm if it is activated by an autoimmune response to act against normal body tissues.
Immunologists describe two pathways, classical and alternative, by which the complement system works. The classification of the many components of the complement system is complex and beyond the scope of this book; however, it is important to keep in mind that this system is very influential on innate immune function, and, as with low numbers of NK cells, complement deficiency is associated with increased infections.
We now turn to the second pole of the immune system. Adaptive, also called specific or acquired, immunity is characterized by recognition and memory of an encounter with a foreign pathogen. This ability of the immune system to remember is considered the second main principle of traditional immunology. The initial encounter between an invading pathogen and cells of the adaptive immune system produces a delayed immune response that is specific against a particular infectious microorganism. Therefore adaptive immunity is developed only after exposure resulting in natural immunization.
Since the 1950s, microbiologists and immunologists have focused almost entirely on the cellular and chemical components of the adaptive immune response, yielding a wealth of information. However, as mentioned, the immune system is far more elaborate than researchers had previously thought.
Lymphocytes, the principle cells involved in adaptive immunity, come in two major types: T lymphocytes (originating in the thymus gland) and B lymphocytes (the B is for bone marrow, their place of origin). There are two aspects of adaptive immunity: humoral immunity (involving B cells) and cell-mediated immunity (involving T cells).
Humoral Immunity: Humoral immunity is mediated by antibodies, protein substances that help to protect against foreign material,5 produced by B lymphocytes. These cells originate in the bone marrow where they mature, enter the blood circulation, and, over a lengthy process of differentiation, culminate in two types of cells: plasma cells and memory cells. Plasma cells produce antibodies that circulate in the serum and result in humoral or antibody-mediated immunity. B cells make up about 5 to 15 percent of circulating lymphocytes.
Antibodies detect and bind to specific antigens and then activate the complement system and its enzymes to destroy the marked cells or stimulate phagocytes to eliminate the antibody-flagged foreign cells.
There are five types of human antibodies, collectively known as immunoglobulins, which are protein substances secreted by B cells that circulate in the blood and help the immune system recognize foreign substances.6 Each immunoglobulin (Ig) is given a letter to differentiate it: IgA, IgM, IgG, IgD, and IgE, and each immunoglobulin has its own set of biological functions and properties.
Cell-Mediated Immunity: The T lymphocytes are the main cellular component of cell-mediated immunity of the adaptive immune response, and help control intracellular pathogens like viruses. Like all other immune cells, these cells originate in the bone marrow but then migrate to the thymus gland (behind the sternum in the chest) where they mature and are then called thymocytes, or T cells. T cells fight cancer cells and some types of bacterial and fungal infections as well as certain viruses. They circulate freely, like NK cells and neutrophils, and are available for immune defense when needed. Unlike NK cells and neutrophils, they do not destroy antigens at will, but require a specific marker on a cell tagged with an antibody before they start to neutralize the target cell.
T cells do not produce antibodies, but many of their immune functions are interrelated with B cells, which do secrete antibodies. For example, B cells make the antibodies necessary for T cells to kill most viruses. T cell and B cell cooperation involves a subclass of T lymphocytes called T-helper cells that trigger B cells to make antibodies. T-helper cells stimulate the maturation of B cells, cooperate with B cells to promote the production of antibodies, enhance the function of cytotoxic T cells (the second main type of T cell, and an essential cellular component in defense against viruses), and assist in the production of immune chemicals like interleukin 2 (IL-2) and gamma interferon.
T-lymphocyte cells were once divided into just two types: T-helper and T-suppressor cells, but the quantity of new information on T cells has made their classification complex. In recent years, more sophisticated knowledge of how immune cells function has lead to changes in terminology. Immunologists now use the Cluster Designation (CD) system to differentiate different types of immune cells.
Lymphocytes and other white blood cells have different molecules on their surface (called surface markers), which are used to identify subsets of cells. For example, T cells are divided into many different subtypes based upon the different type of surface markers.
CD3 is the general designation for T cells. CD4 cells are a type of T-helper cell that promotes or induces the immune response. In AIDS patients, CD4+ T cells are very low and this deficiency state contributes to increased infections (Lappé 1997).
CD8 cells are cytotoxic cells and also function as suppressor T cells. Less is known about them than CD4 cells, but recent research suggests that CD8 cells are able to kill virus-infected cells. They also inhibit the function of the B cells when sufficient amounts of antibodies have been produced, and suppress the function of cytotoxic T cells when their job has been completed. Cells with the CD56 marker are NK cells.
Measuring the levels by blood testing of the different immune cells following the CD designation provides useful clinical information for the identification of chronic viral infection, cancer, and immune deficiency. Natural immune-enhancing therapies can raise levels of both CD4 and CD8 cells, thereby promoting immune function and preventing viral illness.
Cytotoxic T cells, a third subset of T lymphocytes, attach themselves to a tagged antigen and immediately destroy the target cell. NK cells and cytotoxic T cells are similar as they are both killer cells, but NK cells are nonspecific and can attack a foreign antigen directly upon contact, whereas the cytotoxic T cell is part of acquired immunity and destroys only previously tagged cells.
Chemicals That Communicate: Aside from physical barriers, the inflammatory response (an aspect of immunity involving swelling in response to tissue damage or infection), and cellular components of the immune system, scientists have discovered a vast array of immune modulators that interface with all aspects of immunity and even directly destroy invading pathogens. Immune modulators are substances that modulate, regulate, or influence the immune system (see part 2).
T lymphocytes, macrophages, and other immune cells release substances called cytokines, which are small proteins that function as chemical mediators within the immune system. They are thought to determine whether an immune response will be predominantly cell-mediated or antibody-mediated. Cytokines also communicate with cells from other systems, such as the nervous system and probably with the endocrine system as well, helping to preserve and restore homeostasis—the physiologically balanced state of a healthy body.
Scientists have discovered a vast array of immune modulators that interface with all aspects of immunity and even directly destroy invading pathogens. Immune modulators are substances that modulate, regulate, or influence the immune system.
Cytokines have a variety of functions. Besides regulating the specific immune response, they are involved in the innate immune response to viruses and other microorganisms, and produce inflammation and fever. They also produce delayed hypersensitivity associated with allergic reactions and they affect the movement of leukocytes (white blood cells). There are many known cytokines, such as interleukins (IL 1–18), interferons (INF), tumor necrosis factors (TNF), and immune cell growth factors.
Chemokines, a class of cytokines referred to as chemoattractants, have been called immunology's “high impact factors.” First discovered in relationship to inflammatory responses, there are now over forty known types. Chemokines are mainly responsible for the movement and positioning of immune cells.
This orchestration of immune cells is one of the most important functions of the immune system. Without it, the immune cells cannot interact with one another and are unable to mount an immune response. Ironically, some viruses and other microbes (HIV-1, CMV, and the malaria parasite) have learned to use chemokine receptors to gain entry into the body.
Of particular importance is the therapeutic use of chemokine receptor antagonists. These are drugs currently in development which block chemokine activity. These substances are considered a new generation of anti-inflammatory medications. The chemokine story gets more interesting when we add to it the fact that viruses also appear to use naturally occurring chemokine antagonists to block inflammatory immune responses. This may explain how stealth viruses get past the immune system.
By inhibiting the initial inflammatory mechanisms, the viruses can then enter the bloodstream and circulate through the body, eventually arriving at their chosen site of infection—often the brain and central nervous system in the case of stealth viruses like CMV. In addition, stealth viruses may use chemokines as growth factors. In this case, the virus bypasses the inflammatory response thereby not alerting the specific immune cells; once in the body, it uses chemokines to replicate and produce more viruses.
The research of Dr. Martin, cited earlier, suggests that a number of the newer antibiotics, notably clarithromycin (Biaxin), that cross the blood-brain barrier are capable of suppressing chemokines. The blood-brain barrier is a term used in medicine to describe the protective ability of the brain and surrounding tissue to keep out toxins and microorganisms. Several natural medications and nutritional products also suppress chemokines and are useful in the treatment of stealth viral infections. These include vitamins B3, B6, B12, and vitamin D. The female sex hormones progesterone and estrogen also have chemokine antagonist properties. The flavonoid antioxidant quercitin has potent activity against chemokines and enzymes that favor viral replication, and it is an important part of the antiviral protocols described in part 2 of this book. Herbal medicines, especially Chinese herbs, may also have activity against unfavorable chemokines (discussed in part 2).
Other Immune Cells: Eosinophils compose 2–5 percent of total white blood cells and are capable of acting as phagocytes to kill microorganisms. They are believed to have a specific role in immunity against parasites. Levels of eosinophils become elevated during parasitic infection. They also deactivate histamine and often are found in increased levels in people with allergies.
Basophils and mast cells are very similar to each other in function and are found in very small numbers in the blood. Mast cells are associated with mucous membranes and connective tissue, and are found in greater profusion during allergic reactions. Platelets, cells usually associated with blood clotting but also involved in immune responses, are important in inflammation and healing after injury. They also release serotonin, a neurotransmitter associated with normal brain and nervous system function.
Advancing knowledge of how the immune system functions has contributed to a greater understanding of its biological complexity. What was once thought of as a system based on two distinct and separate aspects, a nonspecific attack response (innate immunity) and a specific learned response (adaptive immunity), is now known to be an intricate web of interrelated chemical and cellular activity intimately connected to the brain and neuroendocrine system. In The Tao of Immunity, Marc Lappé, Ph.D., an internationally known toxicologist, public health specialist, and the director of the Center for Ethics and Toxics (CETOS) in Gualala, California, says, “The immune system is a kind of modern-day cybernetic machine that fluctuates between stimulating and suppressing, eradicating and enriching, annihilating and restoring” (Lappé 1997).
Though we are just beginning to understand the complexities of the immune system and its evolving nature, there are four characteristics of the immune system that are important to discuss before we go further: redundancy, polymorphism, synergy, and mutual antagonism.
1) Redundancy describes many overlapping systems and repetitious functions of the immune system. To the human mind, this seems inefficient at first glance. However, inefficiency is a human concept, and particularly a Western one, and the immune system is not bound by language, culture, or belief. Its purpose is to work well enough for the survival of the individual, and more importantly, the species.
It is like an ant colony: To obtain a crumb of bread, thousands of ants are sent out from the colony, even if only ten ants can or will actually do the job. On the way, some are killed but others may find the morsel to take back. This is how our immune systems function: Tens of thousands of immune cells are employed to deal with every infection.
Cloning is a characteristic of immune cells that relates to redundancy and is an efficient way of preparing sufficient numbers of cells to neutralize an infection. Identical cells are produced daily, each an exact replica of the other. Immunology is largely a numbers game, so if there are enough active cells, the immune system is constantly prepared for possible penetration by microorganisms. Generally we think of clones as replicas with limited programmed functions; however, the immune system takes cloning a step further. Immune cells display a trait called polymorphism that allows them to meet new and changing circumstances.
2) Polymorphism means something can have more than one shape or function. We are beginning to understand that immune cells can have more than one function and can change their chemical shapes as needed. This trait allows for superb adaptability, especially against super microorganisms that have the ability to mutate their forms, a trait called pleomorphism.
The next two characteristics, synergism and mutual antagonism, imply relationships. All natural things exist in relationship to something, and usually to numerous things.
3) Synergism suggests that one plus one does not simply equal two, but could also equal three, four, or five hundred. Synergism describes a situation in which the whole is greater than the sum of the parts and is also an important therapeutic principle, especially in natural medicine. To many conventional physicians natural medicines are considered weak compared to pharmaceutical drugs; however, when applied correctly using a variety of medications in a synergistic manner, powerful results appear. In part 2, you will learn to use therapeutic synergism to effectively stimulate the immune system.
4) In nature, many things coexist, some that are actually antagonistic or even poisonous to each other. For example: lions live side-by-side with gazelles while other creatures like crocodiles wait unsuspected in the watering holes. In your immune system, there are cells that reduce or trigger inflammation, but these same cells can cause damage to each other. This paradoxical activity is referred to as mutual antagonism.
As mentioned earlier, we live in a biological stew comprised of a staggering array of microorganisms and compounds, including pathogens such as viruses that have no “respect” for age, wealth, or social status. If you were to lie on a lawn, within minutes, ants and numerous other insects will find you and start biting your flesh, crawling into your orifices. To the denizens of the lawn, you are just another organic substance. Nature is neutral, and operates on principles that foster long-term balance in biological systems; such a system does not favor individuals, even though modern humans are obsessed with understanding and controlling these principles.
These principles are intricate and extraordinarily complex, and they are in constant transition, so it is difficult to understand changing phenomena, especially when they involve substances and pathogens at the submolecular level. Many of these are infectious microorganisms with rules of their own, and pay no heed to the workings of Man—or laboratory scientists.
The immune system, as an integral part of the organic natural matrix, continuously attempts to keep up with advancing infections and emerging new diseases, as well as with the “standard” ones. The immune system is considerably more dynamic and adaptive than is conventionally understood. Think of it as a web of interconnectedness that can simultaneously recognize and interface with many different microbes and immune challenges. It manages these challenges selectively, allowing certain infections to exist in our bodies while preventing others from taking root in our cells. Continuously transforming and adapting to circumstances, it brilliantly adjusts to the profile of the invading organism; all of this amazing operation is done without our awareness. However, there are times when the immune system fails.
I am continuously impressed by the beauty and effectiveness of the immune system and its innate ability to protect us from illness. When we are healthy, we take it for granted, but there are many ways in which the immune system can become compromised and dysfunctional. Chief among them are autoimmune disease and immune deficiency.
Immune Malfunction: As mentioned earlier, the biochemical recognition of self from non-self is a key principle of immunity. A healthy immune system displays tolerance of self and does not stage immune responses against its own normal tissue and cells. If the immune system does attack normal tissue, immunologists call this an autoimmune response—against the self—such as what happens in systemic lupus erythematosus (SLE), rheumatoid arthritis, and multiple sclerosis (MS).
Autoimmune reactions can also come as part of the normal immune response to an infection or other disease, such as arthritis with hepatitis B, or MS after CMV infection. Conventional immunology assumes that autoimmune responses are the operation of a malfunctioning or misguided immune system, and this abnormal response must be suppressed with drugs. However, it is possible that in some cases the immune system is attempting to remove damaged or diseased tissue, some virally infected, at the apparent expense of the host.
Autoimmune responses may be part of the normal process of “house-cleaning” by the immune system, meant to be only short-lived, acute, inflammatory episodes. Due to numerous factors including a toxic internal environment, weakened organ function, diminished detoxification pathways, poor nutrition, and stress, the autoimmune response can become chronically active, resulting in connective tissue diseases.
Immune Compromise: There are times when the immune system cannot keep up with the job of processing every foreign substance and organism, especially if they are novel or exotic chemicals and microbes. Viruses in particular can be difficult to eradicate. Once inside the body, they enter individual cells and may even pocket themselves away into recesses of organs and tissues. The drain on immune capacity can be severe resulting in weakened immune reserves. Many other conditions that adversely affect the immune system include:
Malnutrition and dietary stressors
Infections
Chronic stress
Chemical toxins
Aging
Chronic pain
Overexposure to ultraviolet light
MALNUTRITION AND DIETARY STRESSORS: Worldwide, malnutrition, dietary stress, and starvation cause more deaths and indirectly more fatal and chronic disease than any other one cause. It's estimated that a billion people are malnourished or undernourished in the world today. Protein-energy malnutrition (PEM) is a form of chronic macronutrient (protein, carbohydrate, and fat) starvation and results in anemia, retarded growth, weakness, and edema; it is what you usually see in the horrific photographs of African children reduced to skin and bones. In less severe forms it can affect elderly people, anorexics, lower-income people, and those on protein-restricted diets. Macronutrient starvation has a severe impact on the immune system, so starving and weakened individuals are more susceptible to infections.
Vitamin-deficiency diseases like scurvy and beriberi are now rare in the wealthier countries, but chronic poor or insufficient nutrition is very common, even in the midst of plenty. Also called micronutrient starvation, this condition gradually leads to reduced immune system function. In this case, the diet does not provide sufficient amounts of essential immune nutrients like vitamin A, zinc, and beta-carotene. Teenagers eating a diet of predominantly junk foods, as well as marginalized low-income people eating excess refined carbohydrates, are chronically undernourished in this manner. And, over time, they may develop a chronic low-level immune deficiency.
In industrialized nations, overeating and consuming excess amounts of the wrong foods cause the most problems. Dietary stressors cause disease and can negatively affect the immune system. Ironically, people can be overweight and undernourished.
One reason is that they consume large amounts of refined carbohydrates or hydrogenated fats and not enough fresh fruits and vegetables. This way of eating provides an excess of calories that the body cannot use, and it stores the excess as adipose tissue, or body fat. At the same time, these foods are notoriously low in nutrients, especially the trace elements vital for a healthy immune system.
Nutritional influences on illness and immune strength are more far-reaching than once thought by Western physicians. Think of nutritional deficiency midway on a continuum, with the severe forms of PEM and vitamin deficiency diseases on one end, and optimal nutrition, which can be defined as a diet rich in nutrient-dense foods, on the other (see figure 3-3).
These include fresh seasonal organic fruits and vegetables; dairy products (for those not allergic to them or who do not have lactose intolerance, a condition characterized by the absence of the enzyme lactase that digests milk proteins); seeds and nuts; vegetable oils like olive and safflower oils; condiments and spices like oregano, cumin, basil, and other culinary herbs; as well as adequate amounts of complete protein from plant and animal sources; and complex carbohydrates such as whole wheat (for those not allergic to gluten), rice, corn, potatoes, winter squash, and other sources of energy like the South American grain quinoa.
Optimal nutrition also means avoiding foods that have detrimental effects on health, such as refined carbohydrates like white sugar and white flour, products containing these ingredients such as commercial cookies and pastries, overly processed foods and foods containing toxic preservatives, additives, and dyes. It also means avoiding the excess use of alcohol and the unnecessary use of pharmaceutical drugs. These foods and substances promote obesity and degenerative diseases like diabetes. In addition to correct food choices, optimal nutrition includes supplementing the diet with vitamins and minerals (see part 2).
Figure 3-3: The Dietary Continuum
At one end of the dietary continuum are starvation and death, and at the other end are optimal nutrition and health. In the middle are sub-optimal nutritional states resulting from vitamin deficiencies, foods of poor nutritional quality, and excess amounts of foods that are high in refined carbohydrates and low in nutritional value.
Optimal nutrition promotes a healthy immune system and prevents disease. Unfortunately, most people in the West consume far too much animal protein, fat, and refined sugar. Patrick Quillin, Ph.D., the author of Beating Cancer With Nutrition, estimates that only about 10 percent of Americans are optimally nourished, a situation that leads to sub-optimal nutrition (Quillin 1994). In these cases, for the majority of people a gradual erosion of immune status takes place allowing for disease processes to occur including cancer, autoimmune diseases, and increased susceptibility to viruses.
INFECTIONS: Not only do certain viruses weaken specific immune cells (HIV and CD4+ T cells),7 but many chronic infections cause poor immune system function and predispose the body to other infections, fatigue syndromes, and possible tissue and organ failure including cancer. This can be seen with HCV and hepatocellular carcinoma.
Chronic and hidden bacterial infections also weaken the immune system. Chronic sinusitis, dental abscesses, chronic prostate infection, chronic appendicitis, diverticulosis (a condition of small pockets forming in the colon), gall bladder infections, and other conditions can weaken the body systems and fatigue our natural immunity.
Parasitic infections can be worse. Excess populations of normal gut bacteria, like klebsiella (a gram-negative bacteria in the Enterobacteriaceae family), can lead to rheumatic joint inflammation; malaria is notoriously immunosuppressant; and the Lyme spirochete not only causes damage to the nervous system but also weakens the immune system. Fungal infections are becoming more common and are equally a sign that the immune system is weakened. For example, chronic candida yeast infection causes a wide array of symptoms very similar to allergies and chronic viral infection, including fatigue, cloudy thinking, and gastrointestinal bloating.
CHRONIC STRESS: There is considerable scientific evidence that stress weakens the immune system. There are several models of how stress affects the immune system, and each has a common component: stress triggers a nervous system response, causing a brain response, which in turn affects glandular, and thus hormonal, function. Stress hormones then affect the hypothalamus, the region of the brain responsible for maintaining normal physiological functions like heart rate, temperature, hunger, weight control, and sleep.
Three interrelated glands—hypothalamus, pituitary, adrenals—interact with the nervous system and affect the immune system. As part of what's called the hypothalamic-pituitary-adrenal axis (HPA), cortisol is released by the adrenal gland in response to signals from the pituitary. High levels of cortisol suppress lymphocyte production and inhibit the release of IL-2 (Interleukin-2, an immune-enhancing cytokine).8 In addition, epinephrine and norepinephrine—commonly called adrenaline, the chemicals that produce the “fight-or-flight” response—become elevated under stress. This can reduce the levels of CD4 helper T lymphocytes.
People with clinical depression have been shown to have more out-breaks of cold sores, genital herpes, and more frequent symptoms of the common cold. They also have poorer outcomes from cancer and degenerative diseases. Surprisingly, overly strenuous exercise causes increased numbers of free radicals from the burning of more oxygen demanded by intense activity. This results in depletion of antioxidants,9 one of the key components of optimal immune function.
There is now an epidemic of sleep disorders in the United States. In our fast-paced society, it is a luxury to spend a day in bed. One of my Chinese medical colleagues said to me that in America we treat our bodies like machines, expecting them to run at high efficiency whenever we want, just like our cars. However, the body is not a machine. It needs adequate rest and sleep as part of its restorative cycle in order to function effectively.
Several studies have shown that going without sleep and enduring chronic sleep deprivation are harmful to immunity. In one study, sleep deprivation reduced natural killer cell levels. Carol Everson, Ph.D., a neurobiology researcher at the University of Chicago, found startling evidence here. In chronic progressive loss of sleep a “negative energy” balance resulted in reduced immunity, and it allowed normally occurring gut bacteria to migrate to otherwise healthy tissue sites, resulting in infection (Everson 1993).
Dr. Everson also found that this deep negative energy balance caused by chronic sleep deprivation reduced the normal inflammatory response, allowing abnormal levels of bacteria to survive unmolested by the immune system. Negative energy balance is a state where more energy is expended than is replenished in the normal restorative cycle of sleep, rest, and eating.
Dr. Everson also found that this deep negative energy balance caused by chronic sleep deprivation reduced the normal inflammatory response, allowing abnormal levels of bacteria to survive unmolested by the immune system. Negative energy balance is a state where more energy is expended than is replenished in the normal restorative cycle of sleep, rest, and eating. A host of symptoms appear when sleep deprivation occurs including fatigue, increased appetite (the body's way of attempting to make up for lost energy by eating more), weight loss, increased susceptibility to common infections like colds and sinusitis, and hormonal changes such as low levels of thyroid hormone and growth hormone.
During times of stress, getting enough sleep and being able to sleep deeply and uninterruptedly greatly improves immune function.
CHEMICAL TOXINS: Excessive toxic load from environmental chemical exposure caused one of the most significant adverse effects on health in the twentieth century. It is accelerating into this century as well, and will continue to unless we make significant changes in the way we live. The liver, the most important detoxification organ, has evolved extraordinarily effective mechanisms to detoxify normal levels of naturally occurring toxins, such as plant toxins in foods. However, it becomes incapable of dealing with or keeping up with the immense amount of novel chemical toxins from over-the-counter and prescription drugs, preservatives in foods, insecticides, fungicides, hydrocarbons, and other environmental poisons in the air, food, and water we consume.
There are several classes of chemicals that cause disease in humans. These are mutagens, teratogens, and immunosuppressants. Mutagens are chemicals that cause abnormal cell changes (or mutations) that lead to cancer. If these mutagenic changes occur in the genetic material, altered genes can pass from parent to child, causing disease for generations.
Teratogens are chemicals that cause abnormal tissue changes in the fetus, leading to birth defects. Since the immune system is unable to successfully deal with these chemicals once they have gained entry into the body and have caused irreparable cellular damage, the body may put other systems into play to keep us from exposure. One researcher found that the increasing incidence of morning sickness, which is now called nausea of pregnancy or pregnancy sickness, may be a natural way of preventing the mother from eating, thereby reducing her exposure to birth-defect-causing chemicals in foods.
The field of toxicology has mainly focused on cancer-causing agents and less on the immune system. However, immunotoxicology—the study of how toxic chemicals damage immune function—describes not only carcinogenic, or cancer-causing, agents, but also the mechanics of reduced general immunity and increased susceptibility to infection.
Immunosuppressants are toxic environmental chemicals that cause suppression of the immune system, thereby allowing for increased vulnerability to infection or causing direct acute toxicity and even death. Long-term, low-level exposure to these substances can insidiously alter immune response, a condition which might first manifest as more frequent cold-like or allergic symptoms or asthma, but which can eventually lead to more complex degenerative illness. It may even participate in destabilizing the immune system, allowing reactivated herpes viruses infections, or it may reduce resistance to common bacterial, viral, or fungal infections. Xenobiotics—foreign chemicals that interact with living systems and even mimic hormones and other naturally occurring substances—are considered the most dangerous of environmental toxins.
The list of these toxic substances is long and includes the polychlorinated biphenyls (PCBs) and related substances such as polychlorinated dibenzofurans (PCDFs) and polychlorinated dibenzodioxins (PCDDs)—a group that includes the toxic agent dioxin. As PCBs concentrate in the food chain, people who eat fatty meats and large amounts of fish are particularly at risk. Organophosphate pesticides (diazinon, malathion) residues on foods, heavy metals (iron, lead, mercury, zinc), and scores of other environmental toxins also cause immune damage.
In addition, many prescription drugs—ironically even some, like AZT, used to treat immunodeficiency—and the abuse of recreational drugs and alcohol also cause significant immune damage. Chemical substances and drugs like acetaminophen cause liver toxicity, indirectly fostering illness and immune system compromise. Steroid drugs, like Prednisone, routinely used for only minor respiratory tract inflammations, are powerful immune suppressants.
AGING: Aging, or senescence, is the gradual wearing out of living organisms, and it is one of medicine's greatest mysteries. Though we may not know exactly why we age, we do know some of the effects of aging. Among the many aspects of aging is a decline in immune function and an increased predisposition to chronic inflammation. Persistent inflammation can damage important tissues such as the coronary arteries of the heart, and inflict the joint pain of arthritis. Ironically, this inflammation can be triggered by immune reactions. The same system that works to promote our survival may also participate in our aging.
During our lives, we are exposed to an increasing toxic chemical load and this causes tissue and cellular damage from free radicals associated with or produced by the toxic substances. This damage, referred to as free radical pathology, also weakens our immune status (see part 2).
Hormonal decline also occurs with age. Steroid, sex, and stress hormones help to manage inflammation and tissue damage, but if they are deficient, as happens in aging, the tissue damage can become chronic, leading to a predisposition to disease and the reactivation of viral infections. On the other hand, using steroid hormone drugs like Prednisone reduces inflammation but causes significant immune suppression.
The thymus gland in the chest is of particular importance to immune senescence. It tends to atrophy with age, and this shrinking-gland phenomenon causes reduced immune function and increased susceptibility to infection. The function of hormones and immunity is discussed in part 2, including ways to supplement hormonal deficiency.
CHRONIC PAIN: Ongoing pain, in the low back or neck and as found in arthritis, is one of the most common complaints reported to doctors, and it can weaken your immunity. Pain causes the release of inflammatory chemicals that suppress immunity. The stress of chronic pain and the sleep disruption that pain creates also reduce your immune system's ability to fight infections. The immune-suppressing trio of stress, sleep deprivation, and pain over an extended period of time can weaken your health and make you more susceptible to cancer and viral disease.
OVEREXPOSURE TO ULTRAVIOLET LIGHT: Repeated or long exposure to ultraviolet radiation can suppress the immune system. Research has shown that activation of chemicals in the skin and the secretion of interleukin-10 (IL-10, a cytokine) reduces resistance to tumor formation and infections.
Outbreaks of oral herpes simplex virus can be triggered by sunlight. People in tropical countries, where there are more hours of daylight per year and where the highest levels of solar radiation occur, experience the highest incidence of infectious disease, including oral herpes virus. Of course, there are other factors that cause more infections in tropical countries than in temperate regions, such as poor diet due to poverty. Besides the sun, other sources of ultraviolet light include indoor lighting, growth lamps for plants, and tanning beds.
PURPOSEFUL IMMUNOSUPPRESSION: Modern medicine uses drugs and radiation to suppress the immune system. In the case of rheumatoid arthritis, an autoimmune disease characterized by aggressive joint inflammation, drugs such as methotrexate and cortisone are used. In organ transplant patients, the immune system must be continually suppressed for the transplanted organ to be retained and accepted. Radiation, a common therapy in cancer, suppresses production of white cells in the bone marrow.
In all these cases, increasingly large numbers of people in the general population are artificially immunosuppressed by drugs. These patients are more prone to simple infections and are often on multiple courses of antibiotics to treat and prevent opportunistic bacterial infections. This may result in these individuals harboring drug resistant species of viruses, bacteria, and fungi—essentially becoming living, walking test tubes for super bugs.
Symptoms of a Compromised Immunity: The immune system is extraordinarily resilient. Under normal circumstances of regular exposure to infectious illnesses, the immune system manages quite well. However, under siege by toxins, stress, complicated with adaptation to new viruses and antibiotic-resistant bacteria, and combined with age, sleep deprivation, and other physiological stressors, it gradually becomes compromised. Once the immune system reaches a point where deficiencies and imbalances occur, symptoms show themselves. When immune compromise is severe, life-threatening conditions occur, usually caused by opportunistic infections like CMV and pneumonia.
Deficiency of specific components of the immune system results in primary immune deficiency syndromes (see table 6), considered rare clinical diseases. However, larger numbers of people seem to be exhibiting signs of immune deficiency patterns. Perhaps, as I previously mentioned, there is a continuum of disease states related to immune deficiency with early signs and symptoms that might go unnoticed.
Fortunately, most early immune deficiencies do not develop into much more than frequent colds or recurrent bacterial infections. However, at the extreme end we find CFIDS and AIDS. In the case of AIDS, the immune system becomes so compromised that immune-deficiency diseases, such as chronic skin and mucous membrane infection by the fungus Candida albicans, once thought rare, occur with significant frequency.
Many common viruses become lethal in patients who are immunocompromised due to chemotherapy (cytotoxic treatments) and drugs used to suppress the immune system in transplants. They include herpes simplex and zoster that can cause severe local infections, and cytomegalovirus that can cause pneumonitis (a lung infection), which can lead to death.
The immune system's response to viruses is complex. There are thousands of viruses, and each infects the host in a different way and elicits a different immune response. There is not one specific immune component, chemical, or cell that specifically reacts to a virally infected cell; rather, many different immune cells and processes work together to neutralize a viral insult. In addition, due to the small size of viruses and their ability to lie dormant within individual cells, the immune system may attack the whole cell, tissues, or entire organs containing the virus in order to destroy it. In the process an autoimmune reaction may be triggered, disabling or killing not just the cell but the host as well, as in hemorrhagic fevers and dengue shock syndrome.
After more than twenty years of clinical practice, a large part of it spent treating patients with an immunological aspect of their condition including allergies, CFIDS, fibromyalgia, chronic hepatitis, and cancer, I have come to think of immune compromise and resultant deficiency states in levels.
Viruses are not passive organisms. They have evolved highly sophisticated strategies for avoiding recognition by the immune system of the host, including the production of decoy proteins that interfere with antiviral defenses and the utilization of the host's own chemokines to support their proliferation.
Before they can replicate, viruses must infect a living cell. To do so, they must enter the body. After the virus gains entry into the body, it attaches itself to a target cell and penetrates the cell membrane. Once inside the host cell, it replicates and reassembles into unique virion particles, which burst the host cell and escape (see figure 3-4).
Figure 3-4: Stages of Cell Infection
After entry into the body, viruses infect individual cells by (1) attaching themselves to a target cell (host) and then (2) penetrating its cell membrane thereby gaining entry into the host cell. Before beginning the replication process, the virus (3) uncoats its own membrane and then (4) replicates itself using the genetic material of the host cell. The virions then (5) reassemble and escape the former host (now dead) cell through a process of (6) release by budding (forming a new envelope) or by dissolving the former host's cell membrane (cytolysis without an envelope). Each new virus is capable of re-infecting additional target cells.
Key Immune Components Active Against Viruses: The main immune system components specific to viral immunity are antibodies, produced by the B lymphocytes in cooperation with T lymphocytes, and components of cell-mediated immunity, especially NK cells, and helper and suppressor T lymphocytes. Interferons and interleukins are an early protective mechanism and also play a role in response to viruses. The complement system provides some protection against viruses by damaging their envelopes.
Newly discovered immune enzymes also play a role. Robert J. Suhadolnik, Ph.D., of Temple University School of Medicine in Philadelphia has defined a specific enzymatic pathway (2', 5'-oligoad-enylate trimer 5'-triphosphate, 2-5A), which involves a molecule that activates an enzyme, RNase L, which in turn degrades viral RNA. Though Suhadolnik's research is predominantly on HIV, he found that this enzyme was significantly active in CFIDS patients.
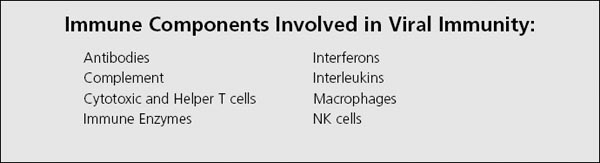
Innate Immune Response: The early immune protective phase against viral infection is seen in nonspecific mechanical events of the innate immune system, such as increased amounts of mucus with respiratory infections and diarrhea in gastrointestinal viruses. Once the virus has entered the body and infected the cells, the innate immune systems responds with activity by NK cells and macrophages.
At this stage, interferons and interleukins also play a role. Interferon alerts neighboring cells of imminent infection, enabling them to prepare a defense. In an active early-stage immune response, fever and inflammation occur (see next chapter). Interferon also activates NK cells, which are active within two days after initial infection and go to work to attack and mop up viruses (see figure 3-5).
Adaptive Response: As the infection spreads, cytotoxic T cells, helper T cells, and antiviral antibodies appear to continue the work started by the innate response. IgA production is increased in the mucosal tissue to prevent reinfection. Other antibodies also arrive on the scene, including IgM and IgG molecules. Though antibodies block viruses from attaching to and entering host cells, they are only effective against free viruses, those that have not yet entered a cell. Once a virus has entered a cell, it is considerably more difficult to eradicate without damaging the host cell. Complement may work along with antibodies to damage the virion envelope and neutralize free viruses.
The body's T-cell system is highly specific and very efficient against viruses. Both CD4 (helper) and CD8 (cytotoxic) T cells play major roles in the immune response against viral infection. Interferon and tumor necrosis factor are key cytokines in the adaptive response against viruses.
Figure 3-5: Viral Pathways and Immune Response
Primary viral infection can generate three types of immune responses. (1) A typical infection proceeds to the acute stage (influenza or cold) and is acted upon by the innate and adaptive immune system and then usually resolves (goes away without consequences). However, acute primary infections can also lead to latency or chronic illness (as with some herpes viruses). In the absence of an adequate immune response, a primary viral infection can proceed directly to (2) latency, or (3) chronic illness (as in chronic hepatitis C).
Resolution of Infection and Return to Normal: As the immune system is responding to viral infection, the virus goes through its own process and eventually is shed from the body. Once outside the body, it remains active and may infect other people, thereby continuing the cycle of immune response and viral replication. The best-case scenario is when the immune system completely eliminates all viral residue so that no viral particles remain dormant inside the body. The worst-case scenario is if the virus takes up permanent residency in the body's tissues. However, if all goes well, the infected individual returns to normal and the immune system is readied for the next challenge.
Absence of the Immune Response: As you have seen in this chapter, under normal and reasonable circumstances, the immune system is more than capable of neutralizing viral infections. However, due to the overwhelming amounts of environmental toxins, the effects of stress, improper diet, and other factors that suppress immune function, the immune response is sometimes unable to effectively deal with the challenge of infection. In these cases, complete resolution does not occur and the virus either enters a latent stage or produces a chronic infection, causing increasing symptoms.
Often the manifestation of these symptoms is completely different from an active infection. For example, multiple sclerosis can be caused by an autoimmune response, which could have been triggered by a viral infection. Looking at the symptomatic presentation alone and giving immune suppressing drugs can temporarily reduce symptoms but further weaken the immune system's ability to neutralize the virus.