In this chapter, we come to one of the major cruxes of modern immunity. We are experiencing a global immune crisis of unprecedented proportions, one accompanied by serious consequences as seen in AIDS, CFIDS, HCV, and other viral pandemics; increasing incidences of other infectious diseases, many types of cancer, and an epidemic of allergic diseases. Unfortunately for the average patient, it is a situation that has been paid little attention to by most clinicians, and until only very recently by most researchers.
I propose that an increasingly dysfunctional natural immunity, combined with increasing virulence of infectious disease are simultaneous causes of the current health crisis. If this hypothesis is correct, then we should expect to see more problems, not only with new viral diseases but with autoimmune diseases, fatigue states, allergies, asthma, and disorders related to chronic inflammation.
However, many of these conditions overlap, often making it difficult to categorize specific diseases into set categories and for a doctor to recognize an underlying immune problem. For example: a case of multiple sclerosis could be triggered by a virus and also be an autoimmune problem, while at the same time present with fatigue as well as inflammation of the nervous system.
Such cases are difficult to treat. Drugs are powerful agents that exert marked effects on only a few aspects of the body's chemistry and physiology, but in doing so may significantly imbalance other aspects, making the patient much worse from the therapy. Natural therapies and more comprehensive approaches to these new conditions are needed.
In this chapter, I explore this hypothesis further and explain why prevention and correction of underlying immune weakness is more important than treatment of acute symptoms. I focus on the first-line defense mechanisms of inflammation and fever and show how they are disrupted, suppressed, and blunted. I discuss the importance of fatigue and how it is replacing inflammation and fever as the most predominant symptom of the new chronic diseases, and I explain why it's important to understand this aberration from normal immunity. Since treatment is necessary for those with viral illness, later in part 2 I discuss and outline methods of using natural medicines to treat viral diseases and provide specific immune-enhancing techniques.
Put simply, it is as follows:
The cause of this breakdown of the natural immune cycle is multifactorial and therefore it is not easy to pinpoint one particular cause. Unlike the proverbial single rotten apple, it seems that all the “apples” in the immune barrel are spoiling at different stages. However, as the data comes in, researchers seem certain that the causes include environmental toxins, confusion in gene expression by hormone disrupters,1 stress-triggered dysfunction of hormone regulation between the pituitary gland and adrenals (HPA axis), chronic sleep disturbance, increased microbial virulence combined with drug resistance, immune suppressive drugs, and lifestyle-related factors (discussed in previous chapters) such as a nutrient-deficient diet.
The cause of this breakdown of the natural immune cycle is multifactorial and therefore it is not easy to pinpoint one particular cause. Unlike the proverbial single rotten apple, it seems that all the “apples” in the immune barrel are spoiling at different stages.
The increasing prevalence of allergic disorders like asthma, atopic dermatitis (skin rashes), rhinitis (hay fever), and sinusitis is also an indication of an immune imbalance. In the United States, the incidence of asthma has increased by 75 percent between 1980 and 1994 (Wills-Karp 2001). Certainly, worsening indoor and outdoor air quality play a significant role in causing asthma and triggering allergic symptoms, but a more important factor may be the lower incidence of childhood infections, vaccinations, and overuse of antibiotics.
In the absence of minor infections that children in the past were routinely exposed to, which they contracted from other children or from playing in the dirt (a practice that is not condoned by advocates of modern, overly hygienic child-rearing practices), the adaptive immune system does not build up antibodies in preparation for future infections. This lack of adaptive immunity, combined with an artificially manipulated immune response from vaccines, can tip the balance of the helper T cells, allowing for increased reactivity to allergic antigens. Allergic diseases can cause chronic inflammation, setting the stage for autoimmune diseases like rheumatoid arthritis.
It is becoming more common to see cases of chronic low-grade inflammation, as in irritable bowel syndrome (IBS), even though, paradoxically, the innate inflammatory response is blunted or absent in the face of infection. Chronic inflammation has been associated with increased risk for heart disease, Alzheimer's, and it often accompanies chronic fatigue.
Another factor disrupting immunity and contributing to increased allergies and inflammation is the disruption of intestinal flora from antibiotic use and the consumption of refined foods. Antibiotics destroy normal bacteria, like Lactobacillus species, as well as harmful bacteria. A normal intestinal environment is essential for a strong immune system, and appears to also play a role in reducing allergic reactivity. Refined foods do not provide the proper medium for friendly intestinal bacteria to thrive. Foods that promote a healthy intestinal environment are fermented products like miso and yogurt (see part 2).
Illustrative Case: Martha: A case study helps us understand this issue. Martha was a brilliant woman in her mid-thirties who first came to see me with multiple complaints that centered on chronic fatigue. In addition to her low energy, she had allergies, chemical and food sensitivities, recurrent colds, sinus congestion with repeated bouts of sinus infections, and yeast infections. When she first saw me, her medical doctors were treating her with an antidepressant and a drug to kill fungus, and she was self-medicating with an assortment of vitamins and herbs. Interestingly, Martha also was very sensitive to many vitamins (or the binders used to hold the tablets together or fill the capsules), so she ended up with many unusable bottles of supplements.
Reviewing her medical history, I found Martha was previously employed in a job that involved a high degree of toxic exposure to pesticides. Prior to that, she had been very active and healthy, except for childhood allergies for which she had had her tonsils and adenoids removed, both of which are lymphatic tissue and part of the immune system. She had been under high pressure and stress for many years.
Martha traced her problems to what she originally thought was a cold that would not go away. She had been severely ill for about four months, though she pushed herself to continue working, until she sought medical advice. Her conventional doctor gave her an antibiotic for sinusitis and recommended rest; however, she only experienced mild relief and pursued further diagnostic studies.
These revealed that she had been exposed to cytomegalovirus and had an elevated antinuclear antibody (ANA). This is a blood marker found in patients whose immune system is predisposed to or already causing inflammation against their own connective tissue. ANA can be elevated in viral or bacterial infections, cancer, autoimmune hormonal diseases, systemic lupus erythematosus, rheumatoid arthritis, and Sjörgen's syndrome. Martha next went to several specialists including a rheumatologist who prescribed nonsteroidal anti-inflammatory drugs.
In Martha's case, we can see that she had a lifelong allergic condition, which was not addressed properly and for which she had to have her tonsils and adenoids removed as a child because they became so swollen due to inflammation and infection. As a person goes through puberty and adolescence, the increased levels of sex and steroid hormones secreted by the glands responsible for these changes often cause symptoms of allergy and asthma to disappear, and these can re-emerge later in life.
Several years of ongoing stress combined with occupational exposure to toxic chemicals further weakened Martha's immune system, and her allergies not only resurfaced but worsened and were complicated by sinus infections. This was most likely followed by reactivation of a latent cytomegaloviral infection; her immune system was able to contain the virus, yet this condition caused an increase in immune chemicals that promote inflammation and helped cause her fatigue.
After her first visit, I referred her to an allergist specializing in disorders with environmental causes. This doctor was able to pinpoint specific allergens and start her on weekly desensitization allergy injections. I treated Martha with acupuncture, nutrients, and herbal medications, and she improved considerably over the first six weeks of treatment. Her fatigue lessened considerably, the sinus symptoms of congestion and pressure disappeared, and she was able to exercise without fatigue or shortness of breath. Over time, her predisposition to catching colds and flu vanished, she had no yeast problems, and she experienced improved tolerance to chemicals, foods, and was able to use most of her vitamins.
Since the cause of her problem was not depression, and as she felt better, she was able to eliminate her antidepressant drugs. Though she still harbored the virus, Martha's body had managed to reestablish immunological equilibrium between itself and the virus.
This case is typical of hundreds of patients that I have seen and highlights several important points. Underlying allergies or immune and endocrine imbalances are not recognized in childhood; often, only symptoms are treated or surgery is used to remove the inflamed tissue, such as tonsils and adenoids. This does nothing for the underlying cause and generally results in lifelong allergy problems. As stress further weakens the immune system and as symptoms of minor infections such as sinusitis occur, the person is treated with more antibiotics. Antibiotics generally fail to work over time, and often cause fungal infections due to the disruption of the internal ecology between friendly bacteria and yeast.
Next, allergies increase and asthma may develop, which is treated with steroids that further disrupt the immune system and further encourage fungal and yeast growth. The resultant vaginal yeast or nail fungal infections are then treated with an anti-fungal drug. By that time, the patient is also often worried, stressed, anxious, not sleeping well, and very tired. They are then treated with a mild antidepressant. Usually, it is about that time that they start to seek alternative treatment. Often, these same patients will also have fibromyalgia or another condition of chronic pain or inflammation like irritable bowel syndrome.
By themselves, alternative therapies generally are palliative for these conditions, though if applied in a comprehensive manner and if they include diet, exercise, lifestyle changes, and stress management, they help many patients to improve significantly. A better model as I used in Martha's case, uses an integrative approach that evaluates many factors including allergies, gastrointestinal function, detoxification pathways, antioxidant status, inflammatory status, viral activity, and immunological function, and applies multiple therapies appropriate to the individual case to restore immune balance and normal homeostasis, the body's self-regulating mechanisms.
Inflammation is part of the healing response, and it is a complex process involving nonspecific and specific immunological mechanisms designed to protect our bodies from pathogens and to assist in repairing damaged tissue. Healthy, normal tissue is not inflamed. Since inflammation is a protective response, once the offending agent has been removed and the damaged or diseased tissue healed, the body automatically returns to a normal quiescent state.
Inflammation is not only part of the healing response, it is also a symptom that something is wrong: you limp or stay off a sprained ankle; call the doctor if your tonsils are swollen; or apply ice to a twisted knee. Inflammation is a common occurrence of daily living, everyone has experienced pain and swelling from a twisted ankle, sore and enlarged tonsils, a stomachache after eating too much spicy or acidic food, a headache, a blister from tight shoes, a cut from working in the garden, or a sunburn. All are examples of inflammation.
The understanding of inflammation is part of the study of medicine and its characteristics have been known in Western medicine since the time of the Greeks. The main hallmarks of inflammation are redness, swelling, heat, and pain, and all four usually, but not always, occur together. In medical terminology, the suffix “itis” in a word means inflammation. Some examples include tendonitis (inflammation of a tendon); arthritis (joint inflammation); hepatitis (liver inflammation); and gastroenteritis (inflammation of the stomach and intestines).
Inflammatory activity is initiated when injury occurs from an external trauma (cuts or burns) or internal deterioration of tissue (cancer, liver disease, or arthritis). Activation of the inflammatory response also takes place from biological insults, such as infection by microorganisms, including viruses.
Inflammation is divided by location into two types, localized and systemic, and by activity into acute or chronic. Localized inflammation occurs when you bang your thumb or have an eye infection like conjunctivitis. Systemic inflammation affects the whole body, as happens in influenza. When you catch the flu, your joints and muscles ache and fever develops; you feel tired and want to stay in bed. Systemic inflammation also occurs in more serious viral infections and other diseases like pneumonitis (inflammation of the lungs) and hepatitis.
Acute Inflammation: In acute inflammation, several processes occur in a complex chain of events. White blood cell production immediately increases and the number of white cells grows. White blood cells, or leukocytes, make up the immune cells or immunocytes, so once leukocytes arrive at the site of infection they release chemicals that control activities of other cells including secretion of inflammatory mediators. These include histamine, serotonin, interleukin, complement, and prostaglandin, among others. Plasma molecules and antigens are also released. Swelling occurs, accompanied by redness and warmth in the local tissue that increases blood supply to the area, and pus may develop.
For minor acute inflammation the treatment is time, rest, and the application of ice. Elevation of an inflamed appendage reduces some of the pressure caused by the swelling. For inflammation with infection, antibiotics or antimicrobial natural medications are necessary if severe bacterial infection occurs. Occasionally, surgical drainage is necessary to remove pus and infected material.
Stress Response to Inflammation: Inflammation is a stressor on the body so the hypothalamic-pituitary-adrenal (HPA) axis responds by increasing the synthesis of cortisol, a hormone from the adrenal gland. Cortisol has natural anti-inflammatory effects. An increased production of acute-phase proteins occurs, like C-reactive protein (CRP). This binds to the membranes of microorganisms, activating the complement system in order to increase phagocytosis, the nonspecific destruction of invading antigens. CRP has other important biological functions in noninfectious inflammatory processes, most notably in heart disease where an elevated CRP level, as determined by lab test, can serve as a predictor of possible heart attack.
Autoimmune-Induced Inflammation: Autoimmune responses can cause serious and painful progressive inflammation. This type of inflammation does not resolve in a normal fashion, but persists and can lead to further tissue damage, as in the joint destruction of rheumatoid arthritis or the kidney damage of lupus. In these cases, the normally protective and beneficial inflammatory mechanism—usually our ally in healing—becomes our nemesis.
Therapeutically, autoimmune-mediated inflammation must be reduced and neutralized. In conventional medicine the treatment of choice is steroid drugs like prednisone and nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen. Though steroid drugs are effective in controlling symptoms caused by inflammation, they also powerfully suppress immune function.
Recall the case of the young woman with rheumatoid arthritis who had been on prednisone for several years (discussed earlier in the book). Though the drug helped reduce some of the inflammation, she developed repeated sinus infections. Once I stabilized her condition with natural medications, she was able to reduce and then eliminate the steroid. Her immune system recovered enough so that she did not have any more sinus problems.
Caution: In autoimmune or pro-inflammatory states, it is important not to take substances that might promote or accelerate inflammation. These conditions include rheumatoid arthritis, lupus, scleroderma, and Sjögren's Syndrome. Even minor inflammatory states such as eczema, hives, and irritable bowel syndrome can sometimes be aggravated by immune-enhancing natural medications like echinacea or dairy-based products like colostrum. For more on the potential pro-inflammatory nature of some natural supplements see part 2.
Chronic Inflammation: Another area of major concern, particularly in many of the modern illnesses, is chronic low-grade inflammation. Aging, chronic viral illnesses, irritable bowel syndrome, atherosclerosis, fibromyalgia, low back pain, cardiovascular disease, and many other chronic conditions all have inflammatory characteristics. Chronic inflammation is abnormal and is not a part of healthy tissue or normal aging. In these cases, pain—often constant and debilitating—is usually present as a symptom and a low-grade inflammation persists.
Environmental toxins, free radical pathology, abnormal gut ecology, bacterial and viral infections, and naturally occurring metabolic toxins trigger immunological responses that can cause chronic inflammation. Stress also plays a significant role.
We are just beginning to understand the mechanisms and consequences of chronic inflammation. Though chronic inflammation may be considered a state of imbalance between anti-inflammatory and pro-inflammatory immune modulators, such as cytokines like interleukin-1β and various chemokines, it is more insidious than that and involves multiple events.
An increase in other pro-inflammatory chemicals also occurs: first come prostaglandins, commonly occurring substances derived from arachidonic acid (a fatty acid and key player in the inflammation cycle), involved in many biological processes including roles in the mediation of inflammation; second is Nuclear Factor kappa B (NF-kappa B, a protein that regulates gene expression inside cells). NF-kappa B actually is part of a family of factors that influence immunity, promote the cell proliferation involved in cancer growth, and that induce inflammation. In addition, metabolic and endocrine changes take place concurrently with chronic inflammation, causing fatigue and generalized low-grade malaise.
Normally, the body has several means to resolve recurring inflammation. It may increase inflammatory activity, temporarily causing more swelling and pain, in an attempt to stimulate the tissue response to pass through an acute crisis and heal the diseased area. The body can also automatically neutralize pro-inflammatory immune mediators, like NF-kappa B, and their byproducts by using naturally occurring anti-inflammatory chemicals. For yet unknown reasons, in many of the modern illnesses these naturally occurring mechanisms do not function properly.
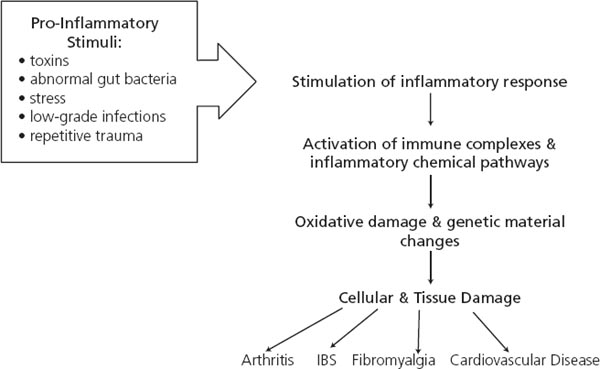
Figure 4-1: Effects of Pro-Inflammatory Stimuli on Chronic Inflammation:
Repeated stimuli from environmental toxins, chronic viral and bacterial infections, repetitive trauma, the effects of stress, and abnormal intestinal bacteria trigger a cascade of biochemical events that result in diseases with chronic inflammation as a common characteristic.
The resulting state of chronic low-grade inflammation is characterized by pain, increased tissue breakdown, and accelerated aging. Though slowly progressing—and usually not differentiating into a specific disease—the consequences of these conditions are low-grade illness, fatigue, and reduced quality of life. Examples of conditions where chronic inflammation plays a significant role include irritable bowel syndrome (IBS), fibromyalgia, myositis, interstitial cystitis, non specific autoimmune disorders, skin diseases like psoriasis, as well as chronic viral illnesses like hepatitis C or herpes virus.
Environmental toxins, free radical pathology, abnormal gut ecology, bacterial and viral infections, and naturally occurring metabolic toxins trigger immunological responses that can cause chronic inflammation (see figure 4-1). Stress also plays a significant role. It can not only trigger inflammation, but can disrupt the hypothalamic-pituitary-adrenal (HPA) axis to such a degree that the naturally occurring anti-inflammatory hormones, such as cortisol, cannot function properly.
As we have seen in previous chapters, stress-induced HPA insufficiency, as this condition is sometimes called, not only weakens the immune system but causes endocrine imbalances that contribute to chronic inflammation, which further weakens the immune system.
Pain Response to Inflammation: The inflammatory process begins with an initiating stimulus, which can be chemical, microbial, or physical. The immune system responds by activating a series of biochemical events, referred to as a cascade because it is like one drop of water on the mountainside that eventually turns into a waterfall. It is not the drop of water that causes the eventual effects; it is the power of the water falling over the waterfall that exerts the most damaging effects on our health.
As the cascade of inflammatory chemicals progresses, prostaglandins, hormone-like substances that contribute to pain and inflammation, produce increased sensitivity of nerve tissue in the locally inflamed area causing diffuse muscle and joint pain. In response to pain and inflammation, interleukin-1 levels increase dramatically in the spinal fluid and travel to the brain. Interleukin-1β leads to production of cyclooxygenose-2 (COX-2) and increased synthesis of prostaglandins, especially prostaglandin E2, a potent inflammatory mediator. COX-2 is an enzyme that acts with arachadonic acid, a lipid substance found in the membranes of all cells in the body, to form prostaglandins. Hypersensitivity to pain results, along with the systemic symptoms of inflammation, such as fever, fatigue, malaise, and anorexia.
There are three blood tests that serve as indicators of inflammation in the body. These are the erythrocyte sedimentation rate (ESR or sed rate); C-reactive protein (CRP); and the antinuclear antibody test (ANA).
ESR: This is the traditional test used to measure generalized inflammatory activity. This test measures how fast the red blood cells (erythrocytes) settle to form a sediment in a test tube. There are different methods of measurement. The Westergren method isone of the most commonly used and normal values are less than 20 millimeters per hour (mm / hr). However, the lower the value the better. ESR is elevated in rheumatoid arthritis and other autoimmune diseases and it is also elevated in a wide range ofother inflammatory conditions and infectious illnesses such as tuberculosis and severe cases of influenza.
CRP: This is a protein produced by the liver that interacts with the complement system and is only present during acute inflammation produced by the innate immune response, especially in bacterial infections. Like the ESR, it is not specific for any disease; however, elevation can occur in autoimmune conditions and heart disease. Recent research indicates that elevated CRP may also be associated with Alzheimer's disease, arthritis, and metastatic cancer. CRP it is an invaluable marker for evaluating inflammation.
ANA: This is also referred to as the fluorescent antinuclear antibody test (FANA). It is a sensitive screening test to evaluate the presence of autoimmune-induced inflammation. ANA is elevated in systemic lupus erthematosus, Sjörgen's syndrome, rheumatoid arthritis, polymyositis, and other connective tissue diseases, but it is not generally elevated in fibromyalgia. ANA can also be elevated when the kidneys or the lungs are inflamed in viral or bacterial infections, and in colitis and liver inflammation.
During a first visit with a new patient complaining of chronic pain, inflammation, chronic viral illness, other infections, or any disease associated with poor immune function, I order these tests along with other lab studies. Patients with chronic illness in the absence of clearly defined pathology often show a moderately elevated ESR in the range of 20–30 mm / hr. Conventional medical doctors are often at a loss to explain to the patient why their sedimentation rate is slightly elevated, and they frequently dismiss it as irrelevant to the case, or as a transient elevation due to a virus. I think this is a serious clinical mistake.
In my opinion, any elevation above 10 mm/hr is suspect for inflammation, and though an elevation around 30 mm / hr may not make you deathly ill, it is still an indication of chronic active inflammation. I always recommend that the cause be found and treated appropriately. As the patient improves, the ESR returns to normal levels.
A similar scenario often occurs with ANA. Patients with chronic illness may have a slightly elevated ANA, and though most conventional medical doctors discount this, I believe that healthy people do not have such elevations, even if nominal.
Blood, saliva, and urinary pH can also serve as indicators of a pre-disposition to inflammation. The pH scale goes from 0 to 14, with 7 being neutral, between 0 and 6.9 acidic, and from 7.1 to 14 alkaline. The body holds tightly to a very narrow pH range, especially in the blood with a pH of between 7.35 and 7.45. Saliva is also slightly alkaline with an average of 7.4, while urine ranges from slightly acidic in the morning (6.5–7.0) to alkaline in the evening (7.5–8.0). If the blood or saliva indicates an acidic condition, neutralizing the body towards a slightly alkaline state by a change in diet can help manage chronic inflammation (see part 2).
The inflammatory response in viral infection is essential in initiating immune defenses, and it plays a role in controlling the spread of infection. Immunologists believe that early immune reactions to a primary viral infection, though poorly understood, can profoundly influence the final outcome. I agree completely. Some viruses, like influenza, trigger strong inflammatory responses, while others, such as hepatitis C, may not cause any response though those initially infected with hepatitis C who experience an acute inflammatory reaction have a better chance of completely clearing the virus.
Inflammation is essentially positive and protective, yet its consequences in the tissues are part of what makes us feel achy and sick. The severity of how sick we feel depends on the virulence of the virus, how actively our immune systems respond, and the site of infection. The brain and central nervous system are critical areas, and in viral encephalitis, infection can cause extreme symptoms from inflammation of the membranes that surround the brain and spinal cord. The skin is a less critical area, and extreme systemic reactions are rare, as with herpes virus or inflammatory skin disorders like psoriasis.
Systemic Effects of Inflammation: Viral infections can produce localized inflammation. However, most produce systemic symptoms affecting the whole body. Immune cells release inflammatory cytokines that produce fatigue, lethargy, sleepiness, and lack of appetite. Fever is also a common symptom of the immune system's inflammatory reaction to infection. These symptoms are an adaptive mechanism urging the patient to rest so that the normal healing process can take place without interference from daily activity. It also is a method of natural quarantine: you are too sick and tired to go to work or to a movie, therefore you do not infect other people.
In contrast, when you take anti-inflammatory medications, you not only temporarily mask symptoms, but by continuing to engage in daily activities, you inhibit your body's normal healing mechanisms and restorative cycle. You also infect others.
Treatment of Inflammation: Western medicine typically relies on synthetic adrenal cortical steroids (prednisone and topical hydrocortisone) and non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, ketoprofen, naproxen, or piroxicam to treat inflammation. COX-2 inhibitors (celecoxib), a newer class of NSAIDs, have recently been developed and are currently in use. Though steroids have wide use in modern medicine and can be lifesaving, they also exert profound counter-wellness effects on the immune system. In chronic viral infections their use should be avoided with the exception of the most serious of cases.
By reducing inflammation, steroids mask symptoms of infection. They suppress immune resistance allowing for increased microbial activity, and they exacerbate latent amebic infections, latent viruses, and fungal infections. They should never be used casually, as they often are in the general medicine practice; they are best reserved for life-threatening situations or conditions uncontrollable by other methods. Hydrocortisone, a short-acting synthetic version of the naturally occurring cortisol, is used in low doses to treat chronic fatigue; it may be a safer alternative in mild forms of chronic inflammation. Its use is discussed later in this chapter.
Besides their anti-inflammatory effects, NSAIDs also reduce pain and fever. Though they are widely used in over-the-counter and prescription forms, the exact way NSAIDs work is still unknown. They are commonly used for the symptomatic relief of pain, inflammation, and fever associated with conditions ranging from the common cold to arthritis. However, at least 25 percent of those using NSAIDs develop side effects.
These include damage to the stomach lining, the liver, and kidneys, and minor stomachaches are common side effects of these medications. In some cases, serious gastrointestinal toxicity can occur, with bleeding and even perforation of the lining of the stomach or intestines. Sometimes the consequences of NSAID use are fatal.
NSAIDs do not cure, and I do not recommend them for longterm use in patients with inflammation associated with chronic viral illness or in chronic nonspecific inflammatory conditions like fibromyalgia.
Many NSAIDs, like ibuprofen and aspirin, are effective COX-2 inhibitors, medications that stop the activity of this inflammation inducing enzyme. Due to the high side-effect profile of long-term NSAID use, newer, or second-generation, COX-2 inhibitors have been developed, such as celecoxib (Celebrex). Though effective for suppressing inflammation and controlling pain, these drugs also have side effects, and since long-term use may create other immune system imbalances, I recommend their use only for short-term symptom management.
For chronic inflammation, natural anti-inflammatory medications are a better first choice and can be readily incorporated into a treatment plan. Naturally occurring antagonists that can block cyclooxygenase isozymes (COX) are the most effective. These are the key enzymes involved in the synthesis of prostaglandins, particularly COX-2 (the “bad” COX) inhibitors. One example is the common ginger root (Zingiber officinale). The active ingredients in ginger affect the production of eicosanoids, a group of biological response substances, which includes prostaglandins, that mediate healing mechanisms and immune function. Rosemary oil and the resin from frankincense (Boswellia serrata), both rich in ursolic and oleanoic acid, also have COX-2 inhibiting activity.
Chronic inflammation can accelerate cellular damage caused by use of oxygen that generates free radicals. Protection from oxidative damage to tissues and cells is helped by a process called redox, involving antioxidants. Vitamin C, lipoic acid, N-acetyle cysteine, coenzyme CoQ10, and the flavonoids in green tea are antioxidants that protect against inflammation. Curcumin, the active ingredient in medicinal turmeric (Curcuma longa), is both a powerful antioxidant and anti-inflammatory and is useful for the control of pain associated with inflammation.
As in the case of inflammation, the physiological phenomenon of fever was well known to the Greek physicians more than two thousand years ago. Hippocrates wrote extensively on its causes and manifestations. Even earlier than the Greeks, the Chinese observed the manifestation of fever in disease and developed extensive theories and ideas, some which are still in use today.
Fever is one of the most common manifestations of infection and inflammation. It is so common and universal that even non-medically trained people know that fever is associated with illness. Nearly everyone has experienced a fever with symptoms of elevated temperature, chills, and sweating, and every mother has spent at least one sleepless night sponging down a small child in fever.
Normal healthy people do not have fever. The body maintains a very tightly regulated temperature through the hypothalamus, a gland within the brain. There is no exact “normal” temperature; the “average” body temperature of 98.6º F (37º C) varies considerably from person to person, and even at different times of the day. The fever response to infection is triggered by pyrogens, cytokines that act on the hypothalamus to raise body temperature. Once the temperature rises close to or over 100º F, feverish sensations usually appear, and include warmth or flushing, chills, sweating, and aching joints and muscles.
Generally, high fever (102º–104º F, or even as high as 106º F) indicates acute infectious illness and is accompanied by severe chills, profuse sweating, and even hallucinations. In chronic disease, patients can have a low-grade fever that lingers between 99º F and 100º F and may appear periodically at certain times of the day, usually in the late afternoon; this is called tidal fever.
Fever in Viral Illness: Fever is present in nearly every case of local and systemic infections including viral illnesses. The fever response to viral infection is not well understood, but immunologists think it involves interleukin-1 and interleukin-6, produced by macrophages arriving at the scene of infection. Evolutionary biologists and naturopathic doctors contend that fever is an adaptive mechanism to help the body fight infection, and therefore should not be suppressed. Human viruses are generally intolerant of heat and even a slight elevation in temperature inhibits replication of viruses, making fever an ally in fighting disease, rather than an enemy.
The intensity of fever in viral infections can vary from barely any elevation (the common cold) to very high temperatures (dengue). In acute infections like dengue fever, febrile symptoms can be very severe, with bone-shaking chills and high fever coming in waves.
Benefits of Fever and Risks of Suppressing Mild Fevers: Naturopathic physicians and Oriental medicine practitioners contend that suppressing fever with acetaminophen or aspirin thwarts the natural immune function and predisposes one to further illness or allows deeper penetration of the viral agent into the body. Fever, we say, is an unpleasant and even painful, but useful process; assisting the body's natural defense mechanisms is a wiser way of preventing chronic and degenerative diseases than relying on drugs for every symptom. Evolutionary biologists and some medical researchers tend to agree. However, there are very few scientific studies done on the benefits of the febrile response, so conventional medical doctors are not ready to embrace these theories.
Naturopathic physicians and Oriental medicine practitioners contend that suppressing fever with acetaminophen or aspirin thwarts the natural immune function and predisposes one to further illness or allows deeper penetration of the viral agent into the body.
Fever as an adaptive mechanism has evolved among humans and other mammals over more than a hundred million years.3 Fever's presence is not only a cardinal manifestation or sign of disease, but it is an integral part of the healing process. Its purpose is still not fully understood, yet modern medicine somehow considers it a condition to be suppressed. Using drugs to suppress fever interferes with evolutionary mechanisms and may set the stage for further disease.
Of course, this does not happen in every person who uses an over-the-counter medication to suppress a fever from the common cold or average flu, but over time, people who repeatedly use these medications may develop dysfunctional immune responses. The key point is this: If the inflammatory and febrile responses are blunted, you are more susceptible to chronic infection.
Repeatedly suppressing a fever may affect the immune response of future generations. Many children now do not manifest systemic febrile responses, but harbor recurrent infections with localized inflammation. Antibiotics are commonly prescribed, and as the gut flora is wiped out by these drugs, stronger pathogenic microorganisms resistant to antibiotics take their place. The result is that the entire internal ecosystem of the child is unbalanced, which predisposes the child to further infections. Suppressing the fever and the inflammatory response may also reduce the antibody response, allowing for increased vulnerability to future infections. So it is not surprising that repeated ear infections, recurrent colds, and viral infections are on the rise.
In the meantime, viruses are not idle. They are actively evolving organisms that take advantage of those with weakened immunity. It would not surprise me if they also were encoding messages into the nuclear material of the cells announcing an “easy ride” to other viruses. This is not unlike a story my great aunt told me. She said that during the Great Depression of the 1930s, hobos would mark telephone poles with chalk to indicate houses that provided easy handouts.
Treating Fever: I have always believed, and taught my students, that one of the hallmarks of the good doctor is his skill in managing fever. In years past, this seemed a straightforward process. Before the modern drug era, the art of medicine was about deciding when to let a fever run its course and when to suppress it. In serious illnesses, the doctor was often helpless to alter the course of an acute disease, so treatment was limited to monitoring the patient and providing fluids and comfort. Now, a variety of over-the-counter medications are available to treat minor inflammations and fever, as well as many prescription strength drugs. Unfortunately, these are highly overused by the general public and doctors.
Since acute fever is a sign of an infection, the swift diagnosis and successful treatment of the underlying cause to eliminate the fever is appropriate. However, universal suppression of all fevers is not only unnecessary, but could be dangerous to your health. According to naturopathy, mild fevers between 99–101° F should be allowed to run their course since they are considered part of the body's natural protective processes.
In fevers over 101º F, tepid baths or sponge baths with cool water are necessary to manage a fever and keep it from further elevation. In some cases, especially with children, high fever can cause delirium, seizures, and brain injury, so body temperatures above 102° F should be aggressively managed. In children, mild fevers can be managed with homeopathic remedies and herbs; liquid Tylenol may be necessary if the natural remedies do not work within a few hours.
The acute high fevers associated with malaria, dengue, encephalitis, and other serious infectious diseases require aggressive and effective medical management. Do not attempt to manage these on your own. High fever accompanied by sweating can cause loss of fluids and electrolytes; therefore, additional water, juices, and vegetable broths are necessary. Fluid loss to the point of dehydration may require hospitalization for intravenous fluid and electrolyte replacement.
Fevers associated with common infections like colds or flu can be managed at home. Dr. N. C. A. Vogel, and other “Nature cure” doctors of previous decades, advocated a natural comprehensive management of fever. In his book, The Nature Doctor, Dr. Vogel (1952) emphasizes that the body will manage the fever itself if given the opportunity.
However, he stresses the importance of keeping the eliminative organs functioning by using an enema, sponging down the skin, or using diaphoretic (sweat-promoting) herbs to open the pores, and even drinking mild diuretic (urine-promoting) teas. Dr. Vogel also recommends reducing solid food intake during the fever and while there is no appetite. Diluted juices or honey and water keep the blood sugar levels up and prevent hypoglycemia and exhaustion. Additional fluids in the form of pure water, non-acidic fruit juices, and vegetable broths and mixed vegetable juices are also necessary.
Common herbal remedies for managing fever include elder flowers (Sambucus nigra) or yarrow flower (Achillea millefolium). Drink one cup, taken as an infusion, until mild sweating occurs. Chinese herbs are excellent for managing fever; they are used as teas, instant granules, tablets, powders, or capsules containing concentrated extracts (see part 2).
Homeopaths are legendary for the number of remedies they use for managing febrile illnesses. The most useful are Aconite, Belladonna, and Gelsemium. These are taken in low potency (6 to 30 X)6 frequently until the fever subsides. There are also several excellent combination remedies for inflammation and fever. A detailed discussion on homeopathy is beyond the scope of this book; however, for more information on the specialized use of homeopathic medicines for viral illnesses see part 2.
Caution: Homeopathy is the study and practice of specially prepared remedies. The dispensing of these remedies follows specific guidelines, so consult a homeopath or carefully read a homeopathic home treatment guide before using homeopathic remedies.
Management strategies are different for chronic low grade or intermittent fevers. With the new chronic diseases, it is difficult to tell if the fever is part of the healing process or a sign of deterioration in the patient's condition. Usually it is a sign of poor immune function, generalized poor health, the body's inability to neutralize toxins, and chronic infection. In these cases, traditional nature cure doctors who practice “by the book” might encourage promoting the fever. However, in my experience, it is a mistake to attempt to promote a fever associated with chronic disease.
Increased inflammation may result, not only causing the patient more discomfort, but more tissue damage may occur. The course of action for these conditions is to find the underlying cause through accurate diagnosis and remove the cause to eliminate the fever. Obviously, this requires the expertise of a skilled physician.
Hyperthermia, raising the body temperature over a sustained period of time, is another way of using the febrile response therapeutically. This form of therapy is mainly used for cancer patients, but it might have a role in the treatment of other chronic diseases including viral illnesses. Exercise, saunas, steam baths, and sweat lodge ceremonies are also ways to raise body temperature to manage chronic inflammation, though some conditions, such as multiple sclerosis, are also worsened by heat.
The answer is yes. However, it is such a complicated and poorly understood issue that an explanation is difficult to find. Certainly there appears to be something awry with the immune response in an increasing number of people, especially the initial non-specific inflammatory process. We are blunted by stress, drugs, and overwork, so viruses now have easy access to our bodies. Once in the bloodstream, they are able to penetrate to deep regions of the body like the liver or brain where they are difficult, if not impossible, to eradicate. In addition to this, the normal cellular immune responses appear to be dysfunctional.
I have seen patient after patient report essentially the same thing. They do not know how they ended up in their conditions. When I question them, invariably they tell me that they do not remember a serious infection or a particularly stressful event that caused their symptoms. At times, I can trace their history back to recurrent throat infections or overuse of antibiotics for childhood ear infections, but more often, it is difficult to isolate a specific cause. This leads me to believe that either their inflammatory immune responses were already blunted and they were unaware of an infection, or an accumulation of environmental, psychological, and infectious stressors gradually eroded their health.
There are two different explanations for this increasingly common condition: either the immune system did not recognize the virus as a pathogenic agent or the virus evolved strategies that helped it evade the immune response. As mentioned already, the two most common reactions of the immune system to infection are fever and inflammation. Without these symptoms, you cannot tell that you were infected.
Once the virus bypasses the immune response and enters the body, it lodges in the cells of its target organ. Gradual tissue injury occurs, along with low-grade inflammation, accumulations of toxic byproducts of viral damage to the host cells, and impaired function of the target organ. This is clearly seen in chronic hepatitis C.
In the absence of any initial immune response of fever and inflammation, the infected individual is completely unaware that infection by the virus took place. It is often only until years later when symptoms appear that the person realizes they are infected. Chronic hepatitis C infection causes liver tissue damage resulting in inflammation and impaired liver function. The patient may feel fatigued for no apparent reason as a result of the inflammation and reduced organ function. If the fatigue is severe enough, the patient will eventually seek a doctor's advice, but usually not until after trying many over-the-counter remedies, increasing the intake of stimulants like coffee, and taking a variety of herbs and vitamin supplements.
The scenario for epidemics of chronic viral disease is set. Due to environmental changes and ecological pressure, new viruses are emerging and old viruses are becoming more virulent. The human immune system is in a state of imbalance with an impaired innate response (absence of fever and initial inflammation), and at the same time there is an increase in allergic and autoimmune diseases. Opportunistic bacterial, parasitic, and fungal infections occur more easily. These are treated with antibiotics, antiparasitic, and antifungal drugs, which cause further disruption of homeostasis and immunity.
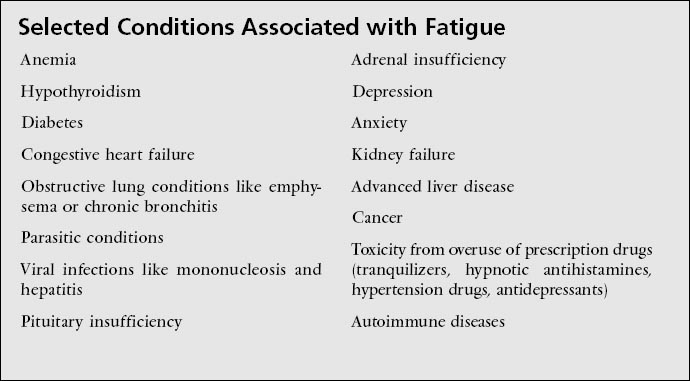
Figure 4-2: Conditions Causing Fatigue States:
The results of disrupted immunity (increased allergic and autoimmune diseases plus decreased fever and inflammatory response), in combination, predispose one to a variety of conditions including chronic inflammation, chronic opportunistic infections, tissue damage, disturbance of normal organ and endocrine function, and chronic disease states. All have fatigue as a leading symptom.
This immune-disrupting cycle becomes self-perpetuating, and in the next section, I discuss why fatigue plays such an important role (see figure 4-2).
Fatigue and Malaise Instead of Fever: It is my clinical observation that in the absence of the normal inflammatory process and with a blunted febrile response, the most prevalent symptom in chronic disease has become fatigue rather than fever. Fatigue is even less understood than fever. Interestingly, in researching material for this book I regularly consulted several textbooks on medical immunology and not one of them had fatigue as an entry in their indices.
Fatigue and malaise are part of the general process of inflammation. Characterized by a sense of weakness, loss of energy, sleepiness, and a generalized sense of feeling sick, one has the desire to lie down. This is a natural response. The body requires rest to fight off the illness and recuperate, and it automatically withdraws energy, causing tiredness. We all have had this experience when sick with the flu. We feel exhausted and need to stay in bed for a few days or longer to recover. In the case of mononucleosis or hepatitis, one can feel profoundly weak, and often a month of bed rest is required.
However, in our modern, super-rushed, high-tech, information overloaded culture, we push this natural process aside and force ourselves to continue working. This behavior deprives our bodies of rest, uses up more energy, and furthers weakens our organs, leading to more fatigue, and increased susceptibility to viral infection and illness.
The body is not only tired from the effects of the illness, but it is fatigued from fighting it without all of its healing mechanisms in full operation. As mentioned in the previous chapter, there are numerous environmental chemicals and drugs that are immunosuppressive. Of course, this only worsens the scenario.
Fatigue may occur from many causes. The obvious ones are overexertion, poor nutrition or lack of energy-providing foods, generally poor fitness, inadequate sleep, obesity, and illness. The list of diseases that cause fatigue is long, and includes anemia, cancer, and rheumatoid arthritis and other autoimmune diseases. Endocrine conditions such as hypothyroidism, low testosterone, and reduced adrenal function also cause fatigue.
As I have suggested, fatigue is a symptom, but it is not appreciated sufficiently as such by most doctors. Though it is true that fatigue and the feeling of not wanting to do anything are associated with depression and chronic pain, medical doctors routinely misdiagnose fatigued patients as being depressed. The most common form of treatment is an antidepressant drug which, of course, does nothing for the fatigue unless it is directly associated with clinical depression.
There is an easy way to assess fatigue. In depressed patients, if they push themselves to exercise, they feel not only less depressed but also have more energy. On the other hand, when the pathologically-fatigued patient tries to exercise, even slight exertion worsens the exhaustion, often putting them to bed for days.
Do not accept a diagnosis of depression and treatment with drugs to treat a mood disorder if your complaint is chronic fatigue. Of course, there may be times when your fatigue may indeed be associated with depression, and you should discuss and review this carefully with your doctor.
Fatigue and Viral Illness: Though patients with chronic viral illnesses commonly experience fatigue, there is surprisingly little information about this condition, even for such a universally occurring illness as hepatitis. According to Mark Swain, M.D., assistant professor of medicine at the University of Calgary in Edmonton, Canada, “The rigorous examination of fatigue as a symptom in viral hepatitis has only recently received scientific scrutiny” (Swain 1998).
Perhaps this lack of information is due to the fact that fatigue has been long considered a symptom rather than a condition, and there are no specific medications in Western pharmacology to specifically treat fatigue. This is not the case in Chinese medicine, where numerous herbs, such as ginseng, are used to prevent and treat fatigued states.
Even so, fatigue is mysterious and paradoxical, and therefore difficult to understand. For example, it is not routinely present in all cases of chronic hepatitis C, HIV positive, and other chronic viral illnesses such as Epstein-Barr virus. On the other hand, fatigue can be a profound symptom in some of these cases. It is universal in mononucleosis and other acute viruses but absent in others. To complicate things further, despite much clinical investigation, there has been no conclusive evidence that chronic fatigue syndrome is caused by a specific virus.
In viral illnesses, fatigue and sleepiness are associated with the acute phase of the inflammatory response. You feel tired and have the desire to lie down or sleep when you have the flu, mono, or hepatitis A (the food-borne type). The fatigue effect is thought to be caused by the action of inflammatory cytokines on the brain and central nervous system. The stress of an infection also affects the HPA axis, and changes in adrenal and other hormones occur that also cause fatigue. Since this type of fatigue passes, and the individual returns to normal after recovering from an acute viral infection, no further clinical questions are usually asked.
Figure 4-3: Viral Infection and Fatigue Mechanisms
Acute viral infection, in a healthy person with a well-functioning immune system, generates a febrile and inflammatory response causing temporary fatigue and then resolves without complications. In the presence of a dysfunctional immune system, the acute phase may not reach resolution and pass directly to the chronic stage. In a person with a blunted initial immune response, the virus bypasses the initial response entirely and proceeds to the chronic stage. Fatigue becomes the main symptom of the chronic stage.
However, less is known about the causes of fatigue in chronic viral infections or why some people experience more tiredness than others. Instead of one cause, there seems to be a series of events that trigger a sustained fatigue response. In this case, fatigue becomes central in the symptom profile and less of a transient, minor occurrence as in acute infections; it involves sustained imbalances in the stress response and blunting of the immune system (see figure 4-3).
The Real Issue with Chronic Fatigue: As mentioned, in Western medicine fatigue is considered a symptom of underlying disease and not a condition in and of itself. It was not until more than a decade after chronic fatigue cases first appeared that it was given a disease category of its own. In 1988, chronic fatigue syndrome (CFS), referred to as chronic fatigue immunodeficiency syndrome (CFIDS) in its severe form, was officially recognized as a disease condition. Though many years have passed since then, the real cause of this condition remains unknown, although several theories have been put forward, some sounder then others.
In general, they all agree that the cause of CFIDS is associated with stress disruption of the HPA axis that result in adrenal dysfunction, changes in such immune parameters with a reduced number of natural killer cells and abnormal levels of cytokines, the activity of environmental toxins that interrupt mitochondrial function (the energy producing part of cells), the presence of viral infections, and co-infections by parasites, fungal organisms, bacteria, and other viruses.
Even with these explanations, many questions remain unanswered. One of the main ones is whether CFIDS is an immune deficiency syndrome or a virally-induced condition. Though the potential of a viral cause has been well researched, there is still no agreement as to what virus it may be. The possible players include any of the herpes virus family, most notably EBV, CMV, or HHV-6. Other possible viruses include HIV subtypes, polio mutants and other vaccination-borne viruses, undiagnosed chronic HCV, and perhaps an as yet unidentified emerging virus.
The proponents of the conventional medical paradigm insist on finding one specific infectious agent for chronic fatigue. Certainly many cases of fatigue have a viral or bacterial cause, and it is well known that fatigue accompanies chronic viral infections like chronic hepatitis, but it is likely that more than one virus may be involved, working synergistically to enhance the effects of the others. However, if the majority of clinicians and researchers are looking for a single infectious agent that does not exist, years will be wasted on dead-ends, prolonging the suffering of patients.
It is difficult for the proponents of the old paradigm to look at CFIDS from either an evolutionary or multifactorial point of view, but unless we are able to make the transition from linear thinking to more complex thinking in which purposefulness, though not immediately evident, is accepted as integral to the web of life, there is little chance of understanding chronic fatigue.
It is difficult for the proponents of the old paradigm to look at CFIDS from either an evolutionary or multifactorial point of view, but unless we are able to make the transition from linear thinking to more complex thinking, there is little chance of understanding chronic fatigue.
Even so, chronic fatigue is still a spreading epidemic. In 1991, Science put the estimated number of cases in the United States at 100,000, but a recent study at DePaul University indicates that there are as many as 800,000 Americans with CFIDS, and that the majority of these are still undiagnosed and many that have been diagnosed with CFIDS are not receiving effective medical care.
Majid Ali, M.D., president of Capital University of Integrated Medicine in Washington, D.C., in his The Canary and Chronic Fatigue (1995) says, “Chronic fatigue will be the dominant chronic health disorder of the next century.” Dr. Ali contends that CFIDS is a disease of accelerated oxidative molecular damage caused by modern living. He says it is both preventable and curable.
Dr. Ali's three main points of clinical strategy are to catch it in the early stages, avoid drugs for treatment, and prevent relapses. His treatments include increasing antioxidant nutrients to normalize the effects of dysfunctional oxygen metabolism in the cells. Antioxidants include vitamin C, zinc, selenium, and other vitamins, minerals, and amino acids (discussed in part 2).
Jeffrey Bland, Ph.D., a nutritional biochemist and founder of HealthComm International and the Functional Medicine Research Center in Gig Harbor, Washington, promotes a similar theory. However, Dr. Bland emphasizes defects in cellular metabolism and a biochemical energy crisis that cause dysfunction in genomic expression (Bland 2000). In this model of chronic fatigue, hereditary predispositions for certain diseases are encoded into the individual's genome. Environmental toxins, an unhealthy lifestyle, and poor diet contribute to biochemical disturbances in cellular metabolism, where all of the body's energy is manufactured. The combination of environmental and lifestyle factors on genetic defects result in a deficiency of the production of energy, in effect a biochemical energy crisis—the cells run out of usable material to generate energy.
According to Dr. Bland, chronic fatigue is the result. The underlying cause for this crisis is abnormal immune system activation, tissue oxidative stress, and imbalanced HPA axis function. His treatment protocol uses diet, antioxidants, nutritional supplements, and lowdose hydrocortisone.
As mentioned earlier, hydrocortisone is the synthetic version of cortisol—a naturally occurring adrenal hormone. An interesting historical note here is that some doctors were already treating fatigued states in patients in the 1960s. They termed the condition hypoadrenia, adrenal insufficiency, adrenal exhaustion, or “a bite of Addison's” disease—a condition of adrenal hypofunction characterized by weakness, fatigue, low blood pressure, and increased skin pigmentation. Since the normal adrenal gland produces 20 to 30 mg of cortisol daily, based upon the work of William Jefferies, M.D., in Safe Uses of Cortisol (1981), some doctors recommend between 5 and 20 mg of hydrocortisone daily.
Recently several articles were published on hydrocortisone use in the British journal Lancet (Jeffcoate 1999) and one in the Journal of the American Medical Association in 1998 (McKenzie 1998). Clinically, physicians who use this therapy for CFIDS report that some patients respond dramatically. However, in my clinical opinion, successes are exaggerated because the approach still follows the old “one disease, one drug” paradigm, and it is not a comprehensive strategy—the evolutionary and energetic components are missing.
Testing for CFIDS: It is vital that you and your doctor understand what type of fatigue you are experiencing. If you have the complex of symptoms that constitute CFIDS, your condition must be ultimately diagnosed from a functional medicine point of view. There is no specific laboratory test that defines the diagnosis of CFIDS. Rather, a combination of clinical history, results of the examination and questionnaire, and a variety of lab tests suggest a state of chronic fatigue. However, since fatigue may be caused by many conditions, you should first be tested to rule out or eliminate common conditions, such as anemia or low thyroid function.
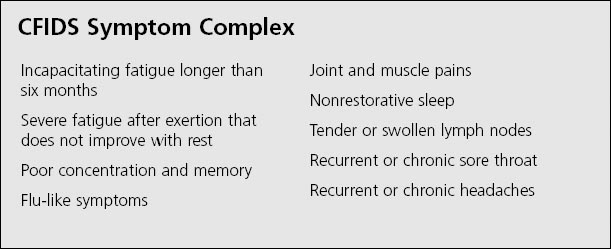
If you do not have any of the common causes of fatigue, then proceed with tests to rule out viral infections such as HIV, HHIV-6, EBV, CMV, and chronic HBV and HCV. Consider screening for influenza-A virus antibodies if your condition started after a flu-like illness. Antibody testing for other chronic infectious such as the yeast Candida albicans, parasites, Lyme disease, and chlamydia, a sexually transmitted bacteria (trachomatis), should also be considered.
The next step is a functional diagnosis of the immune system with a blood panel including natural killer cell activity and counts of the different lymphocytes. Another functional test is the Comprehensive Digestive Stool Analysis (CDSA) to evaluate gut bacteria and parasites. (See part 2 for information on lab tests.)
Caution: It is unlikely that you will be able to manage the conditions discussed in this chapter on your own. You need to find a naturopathic physician (N.D.), a doctor of Oriental Medicine (O.M.D.), a skilled homeopath or acupuncturist, or an osteopath (D.O.) or medical doctor (M.D.) trained in functional medicine to assist you in understanding how to manage febrile illness and treat chronic inflammation with natural medicines.