A Wollf in Yoga Clothing
This story begins as an engineer wanders into a museum of natural history in the city of Cologne, Germany, where he is commissioned to build a crane. He notices that the areas of reinforcement in the bones of a vulture’s wing have exactly the same form and pattern as the head of the crane he is designing.
The small article he publishes about this remarkable similarity is read by Julius Wollf, a surgeon and anatomist, who looks into the matter. He studies many different bones; the pattern of reinforcement seems to be a widespread phenomenon. A few years later, in 1892, he writes a book on the subject. He puts forward a theory to explain the wonderful job nature does throughout the phylum Chordata, which includes all creatures with bones and spinal cords: Bones strengthen just where they need it the most.1
He formulates a principle that encapsulates the order he has found in nature. Wollf’s law states that the architectonic of a bone, its underlying structural system of support, follows the lines of force to which that bone is subjected.
If loading on a particular bone increases, the bone will remodel itself over time to become stronger and resist that sort of loading. The converse is true as well: If the loading on a bone decreases, the bone will adapt and become lighter and weaker. Numerous studies have found that pressure on the bones is a potent force responsible for bone shape and strength.2
Forces That Strengthen Bone
What produces those pressures? How do they come about; how do they come to bear on the fate of our bones? Let’s begin with a couple of examples.
• Muscular stimulus. Bones in the racket-holding arms of tennis players become much stronger than the bones in the opposite arm, since those bones are routinely under stress.
• Gravity. Astronauts who spend a long time in space will often return to Earth with weaker bones, since their muscles have had no opposition—gravity hasn’t been exerting any load. Their bodies have reabsorbed much of the mineral that was in their bones.
Gravity is not the only force, nor the strongest force, acting upon bones. Although gravity is certainly a power to be reckoned with and an important element in maintaining bone strength and design, two other forces must, by their very nature, be stronger: mechanical leverage and dynamic tension.
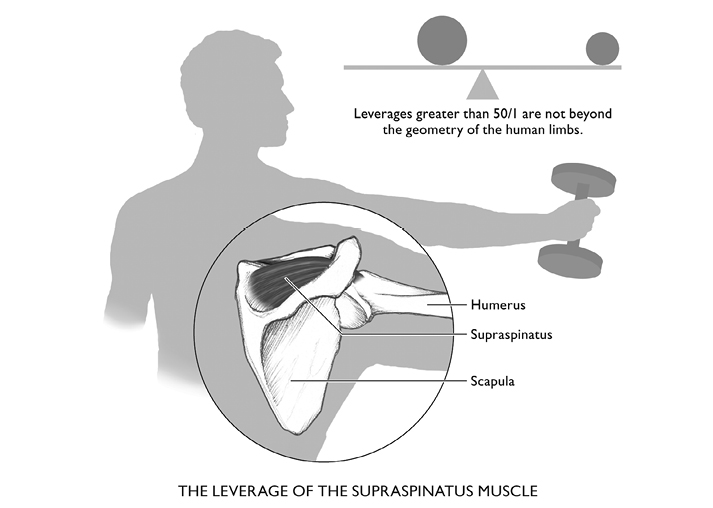
Mechanical leverage is produced by our anatomy. Every 45-pound child knows that if Dad sits close enough to the cross-bar of the teeter-totter, he or she can lift 180 pounds. Many muscles, such as the quadriceps, insert close to the joint they cross, making for considerable leverage. For example, the supraspinatus, located at the edge of the shoulder, attaches to the very tip of the humerus, yielding pressures that are fifty times greater than any weight lifted by the straight arm. This mechanical advantage can multiply gravity’s force many times over.
Dynamic tension occurs when one muscle or muscle group opposes the action of another, and not coincidentally this happens when practicing most yoga poses. The force created is greater than gravity. Since there are two groups of muscles applying opposite pressure, the forces on the bones are doubled. Astronauts could minimize muscle loss, and therefore osteoporosis, by doing yoga in space.
Muscular activity stimulates bones to strengthen themselves much more vigorously than weight-bearing alone, and in so doing can protect the bones from inordinate thinning. This effect seems to operate even in conditions of calcium deficiency.3 Contemporary science has traced and verified the phenomenom just about every step of the way; a convincing number of biochemical markers of the bone-building process have been measured before and after different activities that involve dynamic tension. One biochemical marker, 3H-uridine, is relatively easy to measure. Its level increased six times over levels seen in resting tissue after pressure was applied to bones both in the laboratory and in live animals.4 The duration of the pressure is an important factor as well. In another study it took only eight seconds of dynamic loading to initiate physiologic processes that prevent weakening of bone.5 In yoga, we hold poses for longer than eight seconds.
That is one of the reasons yoga is such a good choice for preventing bone density problems, and for reducing existing ones: Yoga positions are held for periods of time; there is not the constant shifting that you see in tennis, biking, and many other sports. Through yoga practice, the bone has the stimulus duration required to promote the processes of strengthening.
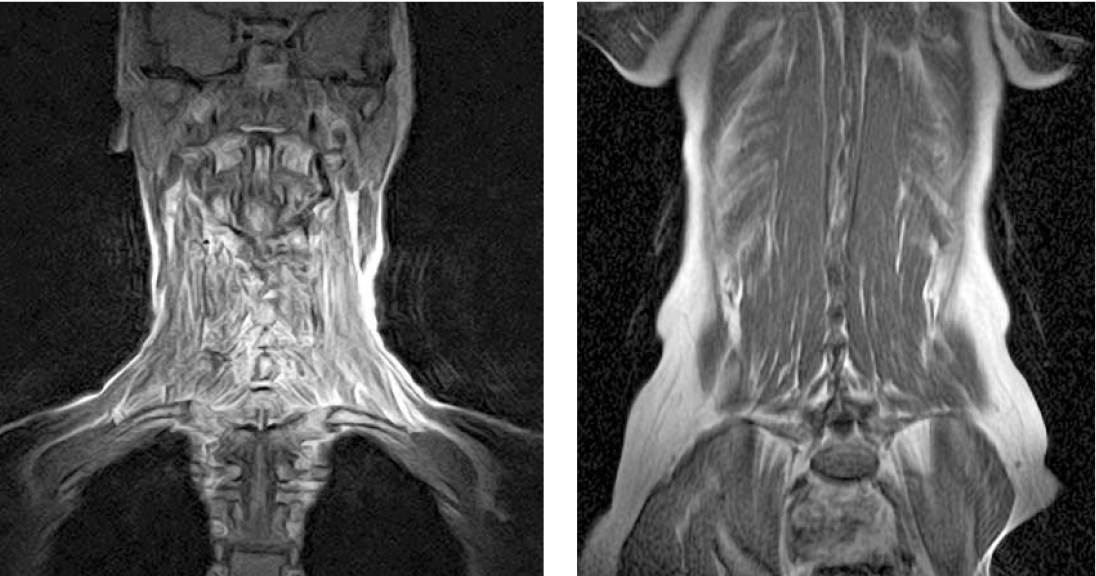
Figure 18. Frontal MRI views of cervical (left) and lumbar (right) spinal musculature. Cervical and cranial muscles insert largely on the scapulae, clavicles, and sternum. Using the arms to lift or support weight gives stimulating compression to the cervical vertebrae. The same applies to the muscles that interconnect the bodies and transverse processes of the lumbar vertebrae.
Mechanoreception, Wherein Lies the Magic
We have seen how osteoblasts come to surround themselves with the protein they secrete, and before long have become almost totally isolated from other similar cells. At this point they change from oval osteoblasts to star-shaped osteocytes. One of their new functions is to maintain the collagen-plus-calcium that makes up the bone. Another is to secrete the new protein matrix on which new bone forms. The key to this entire process is mechanoreceptors: tiny parts of the cell wall that respond to movement by altering the cell’s function. Tiny hairs that protrude from receptor cells in the ears, responsible for turning vibrations of air into the sounds we hear, are an example. All the nerve cells that let us know when something touches us and convey sensations of movement are in this category. Mechanoreceptors react to some physical impingement, something that jostles or juts against the membrane, the sound or the touch, by sending an impulse to the brain. At the ear, we do not “feel” the vibration, we hear it. On the skin, we are not aware of how deep an impression a commuter handle makes when we grasp it; we feel the cold metal and its shape, that’s all. The actual moving of cell membranes goes on at the microscopic level. Mechanoreceptors have probably been part of cells for a very long time. They appear in primitive bacteria and fungi, suggesting that they occurred in a common ancestor; the division of these two fundamental categories of life happened some 3.5 billion years ago.
Osteocytes are a third example of mechanoreceptors. We don’t generally know that our bones are being bent or twisted, yet many studies document that this is exactly what happens. While lifting, carrying, steering, stooping, the bones arch and torque under every strain. When the osteocytes’ outer membranes are stretched or squeezed, as they are by any bending or twisting of the bone itself, they quickly react by synthesizing more of the protein spicules that make up the matrix of new bone.
Osteocytes extend long tentacles, greatly increasing their surface area and the regions in which they are sensitive to positional change.6 A change in the shape, however slight, of a cell’s outer surface alters its inner metabolism and function. Most commonly, tiny electric charges generated by the membrane’s movement supply energy sufficient to change messenger molecules at the cell membrane’s interior. These molecules then make their way to the nucleus. There they fit into the nuclear membrane in a way that influences the nuclear processes themselves. Almost like a neurotransmitter, these tiny messengers from the cell’s outer border affect its very core; they change the DNA, RNA, and the proteins made by the cell thereafter, transforming what the cell can send out into the body. In the case of osteocytes, the process leads to synthesis of more bone-making protein that is then extruded by the cell into the boney matrix surrounding it. The matrix attracts calcium and other minerals that strengthen the bone, and subsequently damp down the movement of the osteocytes’ membranes. This in turn stiffens the bone against bending, which cuts the stimulation for new bone to form. The entire process is the biochemical basis for Wollf’s law.7

Figure 19. Deformation of the cell wall triggers electron discharges that initiate chemical reactions, forming specific molecules at the cell wall’s inner surface. These molecular signals diffuse throughout the cell, reaching to the cell’s nucleus. The nucleus responds by transcribing a new batch of DNA into RNA, which in turn makes new proteins. These are then extruded from the cell into the boney matrix, attracting minerals that strengthen the bone exactly where the strain originally occurred, reducing further deformation.
After Junqueira and Carniero, p. 156, with permission of the publisher.
What pressure does for the osteocytes, it seems to do for cartilage as well. Perhaps this is not startling since the cells that create bone and those that create cartilage both develop from mesenchymal stem cells. Surprising or not, understanding the process does form a fuller picture of yoga’s advantages: You can strengthen bone by opposing one muscle to another, and renew cartilage by applying no-impact stress and increasing range of motion. In this way, yoga may reduce osteoporosis, and osteoarthritis as well.
There is another noteworthy aspect of mechanoreception that Wollf anticipated: Osteocytes respond locally to motion exactly along the axis where the bone is bending, making it resistant to that very bending. As the process continues and the bone strengthens itself against that stress, there is less bending, and the buildup is moderated. This feedback loop keeps bones from outgrowing their usefulness: They are stimulated to thicken at a given point to the extent that is necessary to minimize bending, and no further. The process modulates the creation and destruction cycle of osteocytes and osteoclasts, allowing only enough bending to stimulate bone-building equal to the destruction wrought by osteoclasts.
The same consideration also explains why eccentric pulls, stretches against some resistance (like those that occur so commonly in yoga), are particularly useful. The bone mineral density relates to all-around thickness of the bone. Eccentric, unusual pulls stimulate bone in many more places, thickening and strengthening it overall, protecting it from many points of impact or strain. Opposing the bone’s long axis with unusual stresses, as all of yoga’s bends and extensions do, is bound to stimulate new bone production. For these reasons it is likely to be particularly effective against the compression fractures that commonly damage vertebrae, including six of the seven cervical vertebrae.

Calling on Wollf for Prevention and Treatment of Osteoporosis
Almost all experts agree that prevention of osteoporosis is more effective than treatment. Any diligent prevention regimen takes into account the arc that, with minor variation, charts out the natural history of thickening and subsequent weakening of every person’s bones (see the graph of BMD vs. age on page 19). Beginning a yoga practice early in life—twenties, teens, even younger!—will help the bones strengthen at a time when conditions are maximal. Applying the pressures inherent in yoga will raise peak bone mass, maxing it out at a higher level. Add the benefits of cartilaginous and ligamentous irrigation that stretching and compression provide, and the greater range of motion that stretching obviously brings, there is a fairly compelling picture for yoga as preventive practice. (For more information on yoga as prevention and treatment for joint disease, see our book Yoga for Arthritis.)
We have been studying yoga’s effect on bones for years. In our latest study we solicited men and women with osteopenia or osteoporosis through advertisements, and we also invited patients who had come to us for other reasons. Each patient gave blood and urine samples, so we could be sure that they had no metabolic conditions that would have an unpredictable effect on the results of the study. Each had a DEXA scan, unless they had completed one within the previous six months. We taught them ten yoga poses, designed for safety, that specifically strengthen the parts of the body most vulnerable to fracture: the lumbar and thoracic vertebrae, the hip, and the thigh. These are also the very places that the DEXA scan measures.
Some subjects came to our offices a number of times to learn the poses correctly; sometimes two or three sessions were enough. Others learned the poses with step-by-step instructions from our Web site, sciatica.org. We made contact with everybody every three to four months to find out how they were doing; to ask whether they were practicing the yoga, and if so, how much and how often; whether there had been any adverse effects; and, of course, to answer any questions. We modified the yoga poses for people who were stiff, or who had other medical conditions; some were able to upgrade their practices in time. We also began a monthly newsletter and bulletin board, both accessible from sciatica.org.
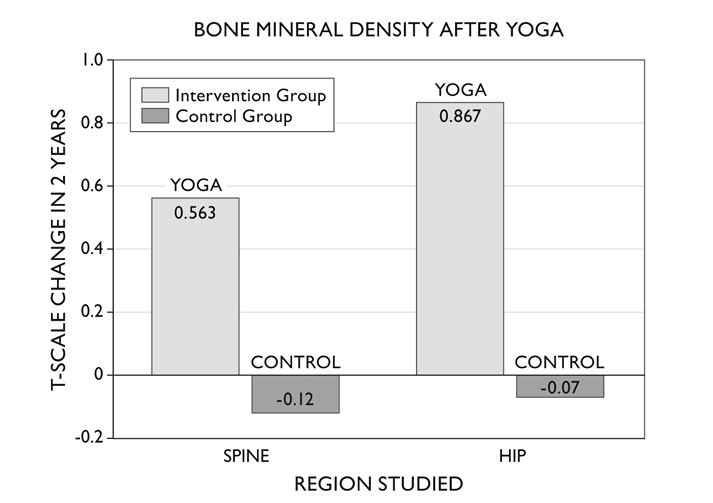
The study is still in progress. Even at this early point, the twelve people who have been doing yoga for two years to improve their bone mineral density have shown a statistically significant rise in their DEXA scores for both the vertebral column and the hip!
The study patients showed an increase in spine BMD equivalent to 0.563 units on the T-scale; their hip BMD increased 0.867 units. Control patients (those who were not practicing yoga) values were –0.12 and –0.07 for spine and hip respectively over the two-year study period. The patients doing yoga gained enough bone in their spine to return most osteopenics’ measurements to normal, and enough bone to restore a minimally osteoporotic hip nearer to the bone density of a healthy 25- to 30-year-old.
There were only seven patients in the control group, so we compared the boney gains of the twelve patients practicing yoga to the null hypothesis, the proposition that yoga did not improve bone mineral density. This is an overly stringent condition, going further than we need to go. These early findings are encouraging, to say the least. To learn more about the study, including our efforts to continue and expand it, see www.sciatica.org and click on the osteoporosis section in the left-hand column.