The Facts
Definition
Osteoporosis, or porous bone, is a disease characterized by low bone mass and structural deterioration of bone tissue, leading to bone fragility and an increased susceptibility to fractures, especially of the hip, spine, and wrist, although any bone can be affected.1
Epidemiology
In the hippie days of the 1960s, two fellows crossed Michigan Avenue to Chicago’s Oak Street Beach. “Man, look at the water,” one said. “Like, that lake is big.” The other observed. “And that’s only the top.” So it is with osteoporosis. The extent of the problem is much greater than first meets the eye.
The statistics are hard to ignore: Forty-four million Americans are known to have low bone mass. That amounts to 55 percent of everyone over age 50.2 One in two women and one in four men over age 50 will have an osteoporosis-related fracture in his or her lifetime. Osteoporosis is responsible for more than 1.5 million fractures annually, including roughly
• 300,000 hip fractures,
• 700,000 vertebral fractures,
• 250,000 wrist fractures, and
• 300,000 fractures at other sites.3
In 2001 more than 315,000 people were admitted to American hospitals with hip fractures, most of them due to osteoporosis.
In the year 2000 it was estimated that osteoporosis caused 37,500 deaths in the United States alone.
Men over 50 are more likely to suffer from a hip fracture than prostate cancer.4 A woman’s risk of hip fracture is equal to the combined risk of breast, uterine, and ovarian cancer.5
Women are as likely to die after a hip fracture as they are from breast cancer.6
Thirty-two percent of women will fracture a hip before reaching the age of 80. After reaching 50, the mortality rate in the first year following a hip fracture is 25 percent.7
Twenty percent of those who could walk before a hip fracture were relegated to long-term care afterward. The cost of hip fractures to the United States in 2002 was $18 billion.8
Osteoporosis is in fact a global problem, excluding no ethnic group or gender. More than 200 million people worldwide are faced with the progressive weakening of already thinned bones and the prospect of often-fatal, always painful, and disabling fractures.9 In most cases, the medical support and financial means necessary to diagnose the condition are lacking, as are medications for its amelioration, or treatment for the fractures that will otherwise occur.
Researchers in many countries have investigated osteoporosis and contributed to its understanding. The pressure is on to effectively prevent and treat this threatening condition, which increases in incidence as life expectancy improves.
Why Is Osteoporosis Dangerous?
What osteoporosis does is impressively simple: It breaks bones. Spine and hip fractures grimly result in painful nights awake, invalidism, and demise.10
A staggering percentage of the 10 million Americans whose bones have thinned below a critical level will have spinal fractures, the most common and possibly the most painful type. Yet 34 million people have low bone strength, not quite low enough to warrant the label “osteoporosis,” but significant enough to have a name of its own: osteopenia. Although each individual in this group has lower risk, taken as a whole, people with osteopenia will actually have more spinal fractures than people with osteoporosis.11
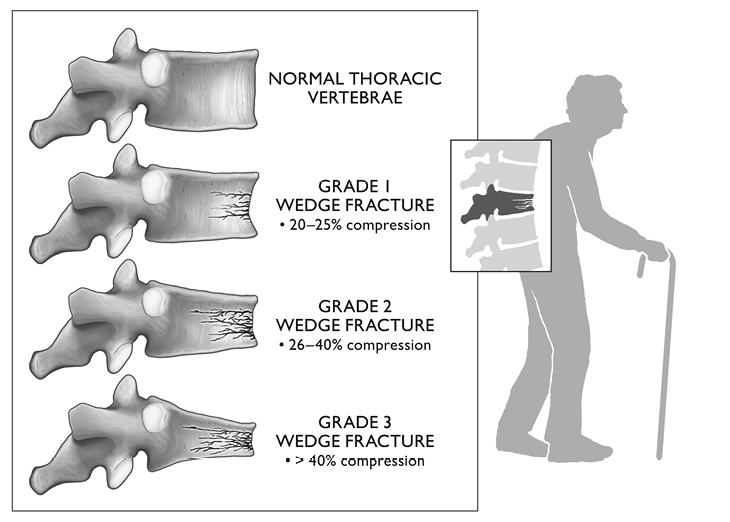
Vertebral fractures may, of course, occur as the result of a fall, but the mechanism is usually different: simple forward slumping, kyphosis or “dowager’s hump,” often seen in the later years, puts so much pressure on the forward parts of the spinal column that osteoporotic bones spontaneously collapse. This type of break is referred to as a wedge fracture.
The process deserves closer scrutiny. The different thoracic vertebrae are of relatively equal strength. Thoracic kyphosis places more weight on the forward part of the vertebrae. When one vertebra fractures, the angle of the spine is even more acute, and the weight of the head, shoulders, chest, arms, and vertebrae above the level of the fracture is further concentrated on the front of the spinal column. The previous angle of the uninjured spine was sufficient to cause one vertebra to collapse. The more acute angle that results from the fracture is even more likely to disrupt another vertebra. Following that event, still more angling makes a third fracture more probable. A recent article in the journal Osteoporosis International found that the best predictor of a vertebral fracture is a previous vertebral fracture.12
Hip fractures are strong and sinister, the second-most common fracture overall as well as the most lethal, with deeply felt, often lifelong or life-ending consequences.13 Wrist, ankle, elbow, shoulder, and knee fractures are also common, usually occurring when a person uses an arm or a leg to break a fall. It is the unbroken fall that fractures the hip. A new osteoporotic fracture of any kind raises the risk of mortality by 32 percent, regardless of a person’s age.14 A hip fracture subjects people to time in bed and wheelchairs, weakening muscles and bones still further, and deconditioning the balance mechanisms in the body that were already inconstant enough to produce the fracture. The fracture itself is not the killer. Mortality derives from the life changes that result: weeks of bedrest with the increased chance of pneumonia and other opportunistic infections, decubitus ulcers (bedsores), weaker muscles, digestive ills, and isolation from society, even family. It is hardly surprising that studies find loss of quality in nearly every facet of life after a hip fracture: mobility, emotional status, social interactions, and sleep, to name a few, all declined.15
But the seriousness of a hip fracture also stems from changes that occur before the fall that produces it. Many geriatricians feel that a hip fracture is a “sentinel event,” an indication that irreversible deterioration has passed a critical point. Inevitable infirmities develop with age. As we add years, we attempt to adapt our lives to declining abilities and strength. Eventually, there is no more possibility of compensation, because all the margins of safety that our mental and physical resources can provide are, naturally, declining too. Barring a sudden event, whether we like it or not, many of us will come to a point at which we cannot adequately prepare for and protect ourselves from a fall and its unfortunate consequences. The trick, and a focus of this book, is to build bone before it weakens, countering osteoporosis as effectively and as comfortably as possible.
And like the hippie who only saw the surface of Lake Michigan, we have only scratched the surface of this topic.
Fighting osteoporosis is a lifelong battle. Like a successful general, the first thing we need is an understanding of our foe. In this chapter we’ll begin with the basics of osteoporosis and how a diagnosis is made. In later chapters we’ll discuss factors that influence its development, and the standard treatments. We will not be shy about finding fault with these treatments, since one needs to go into this with open eyes. It is important to bear in mind that there is prevention, which is always more effective than treatment, and certainly less invasive.
Diagnosis of Osteoporosis and Osteopenia
Many people assume that osteoporosis is a woman’s disease. In fact, several studies show that men suffer from osteoporosis at approximately one half to one fourth the rate of women, but are diagnosed only one eighth as often.16 In a growing and aging world population, all the osteoporosis numbers are, naturally, growing too. But men’s rates are increasing faster. In New South Wales older men actually led women in ankle fractures. Also, between 1993 and 2003 the number of wrist fractures in men jumped 71 percent while women’s rose 43 percent.17 In the United States, men represent only one fifth of those diagnosed with osteoporosis, but there are one third as many osteoporotic fractures in men as in women.18 A study in British Columbia found that in spite of the fact that only 12.5 percent of the people diagnosed with osteoporosis were men, 25 to 30 percent of all hip fractures were sustained by men.19
Other studies document ineffective medical intervention in the United States. One hundred and six inner-city New York women with vertebral fractures were prescribed bone density testing. Only six received it. Further, only 15 percent of the initial X-ray reports even mention the fractures.20
In Ann Arbor, Michigan, a telephone survey found that the only lifestyle adjustment 219 women made after being diagnosed with osteoporosis was to increase their use of over-the-counter calcium supplements. These patients were not impressed with the seriousness of their condition; they did not see that the disastrous future consequences of osteoporosis could threaten their well-being.21
This comment from another study identifies a prevalent attitude toward the disease: “Treatment of osteoporosis was more acceptable to participants than exercise classes.”22 In other words, people are inclined to wait until they have osteoporosis and then treat it, rather than being motivated to prevent it. “If it’s not broken, don’t fix it” unfortunately does not apply to our bones. If a bone is getting ever weaker, it needs attention now. In osteoporosis, prevention is not just the better part of cure, it’s the best treatment!23
How to Identify Osteoporosis and Follow Its Course
Since osteoporosis is a disease of bone fragility, it stands to reason that any benign test for it will measure bone strength. The gold standard today is a test for bone mineral density (BMD), which determines how thick and solid the bones are.
Every test is an abstraction. A blood test measures iron outside the context of the human body, and apart from any molecular parts to which the iron was attached; an electrocardiogram records the heart’s electrical impulses without regard to its mass, bloodflow, or temperature. Similarly, we know from the outset that any measure of a bone’s mass isn’t going to take everything into account. In fact, the most commonly used and currently most reliable measure of its strength, bone mineral density, doesn’t consider the different ways in which bones are constructed in different individuals. Moreover, the test is designed and standardized only for women.
For many years osteoporosis has turned up as an incidental finding to a chest X-ray or an X-ray of a bone following a fall. The “ground glass” or lenslike appearance of a long bone such as the femur or humerus is often the tip-off. But the definitive test for osteoporosis is the dual-energy X-ray absorptiometry (DEXA) scan. This X-ray involves so little radiation that the radiology technicians administering it do not wear lead aprons, though they conduct the tests every day. Nevertheless, it is an extremely valuable guide to whether a patient has osteoporosis and whether efforts to counter its progression are effective.
What Is a DEXA Scan?
Osteoporosis, weakening of the bones, is not exactly uniform; some bones may be weaker than others. It is, however, largely a systemic process, affecting all the bones. Modern medical science has defined osteoporosis as a significantly abnormal finding in a specific examination, the DEXA scan. Bone mineral density is measured by determining the amount of energy that is absorbed as X-rays penetrate particular bones. This is proportional to the amount of calcium and other minerals that a particular cross-section of the bone contains: the more minerals, the more X-rays get absorbed. Most DEXA scans study the lumbar vertebral bodies, the iliac bone in the pelvis, and the femur, since those are the bones most commonly fractured.
The DEXA scan’s reading tells how much mineral material stands between the device emitting the X-rays and the collecting plate. Two factors affect the measurement: how densely packed the bone is, and its physical dimensions. A thinner but more closely packed bone might end up with the same reading as a physically larger but less dense one. The reading is only a measure of the quantity of mineral in the tissue X-rayed.
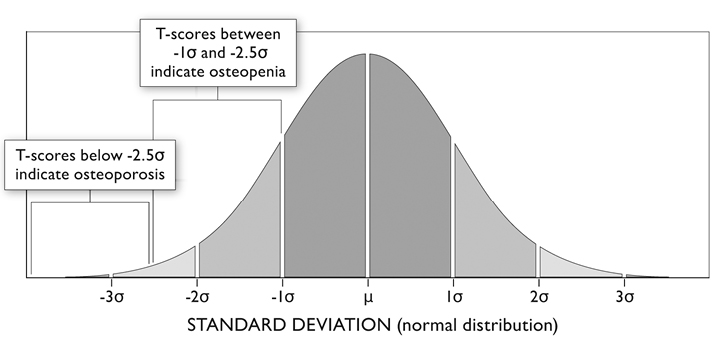
Of course, bone mineral density is not the only factor that determines how likely a person is to have a fracture. The length of one’s bones, whether they are well or poorly knit together, and how many internal cross-struts prop them up are all contributors, as are one’s balance, mental status, and customary walking surface. But in spite of our ignorance about a bone’s inner construction, and even discounting personal and environmental factors, we know that the lower the bone mineral density on the DEXA scan, the higher the risk of fracture.24 In a one-year study of 197,848 postmenopausal American women of five ethnicities, a decrease of one standard deviation in BMD was matched by a 50 percent increased fracture risk in each ethnic group.25 But what is a standard deviation?
In order to understand the result of your DEXA scan, you’ll need to know a bit about statistics. Your measurement is going to be compared to that of others, specifically the “average” measurement of people at the peak of their bone strength, and people of your own age and height.
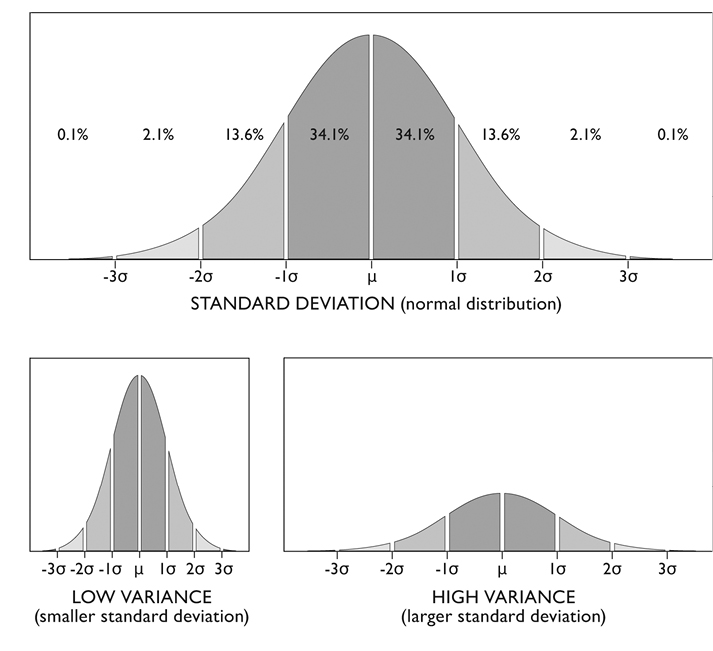
The standard deviation, also referred to by the Greek letter sigma, σ, is a numerical measure of how tightly the members of a group cluster together. It tells you how far different individuals in a group stray from the group’s average, or mean. The mathematical formula determines exactly how far away from the average different proportions of the group can be found. If you look at a “normal” distribution, 68.2 percent of the group will always be located within exactly one standard deviation above and below the mean. A larger standard deviation means that the group is spread out, and 68.2 percent of the group will still be one standard deviation or less away from the mean, but that distance will be farther away from the mean, because the standard deviation is bigger. There is, of course, an average value in any case, but with a larger standard deviation many individuals will differ quite substantially from that average. A smaller standard deviation indicates that most of the group is close to the average.
The standard deviation will vary according to the discrepancy between the average value and the different individual values, but it will always include 68.2 percent of the values. Two standard deviations will include 95 percent of the values. And only 1 percent of the group will lie farther than two and a half standard deviations beyond the mean.
Using this calculation, medical researchers can determine how significantly different from the average a given value is, and what the odds are that this value represents a truly abnormal condition, rather than one that might occur just by chance.
An Example: How Standard Deviations Work
Suppose a group of children had nothing better to do than shoot arrows, trying to land them in the bull’s-eye of a large, reasonably distant target. Suppose further that by dusk there were one thousand arrows arrayed on all sides of the target. Two possible outcomes are shown in figure 3.
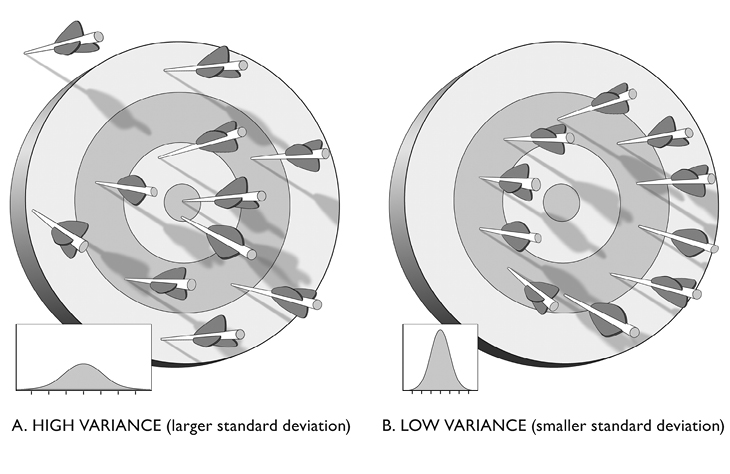
If we wanted to know how close the average arrow came, we could do it by measuring each arrow’s distance from the bull’s-eye, adding them all up, and dividing by the total number of arrows: suppose one arrow in figure 3A was 4 feet from the bull’s-eye, another 14 feet, another 9 feet, another 23 feet, and so on, and that if you added up all the distances, the number for the 1,000 arrows came to 10,000. The average distance that arrows lay from the bull’s-eye would therefore be 10 feet. Calculating the standard deviation tells you how diverse the positions of the different arrows are, based on how far they array themselves from 10, the mean. Statisticians use a formula that goes through each arrow’s distance, subtracting it from 10, and squaring it. The greater the resulting number, the higher the standard deviation. As anyone can see, these arrows’ positions are quite diverse, so the number will be big.
Now examine the second picture, figure 3B, and consider the standard deviation. Once again the average distance of any arrow from the bull’s-eye is 10 feet. But the standard deviation, determined by subtracting each individual arrow’s distance from the average distance, will be very small. That small number reflects the fact that the arrows’ distance from the bull’s eye are nearly identical.
In the first picture, an arrow that’s 20 feet from the center is nothing remarkable. Even though it’s twice the average distance, that sort of thing happened frequently. Another way of saying this is that the standard deviation is very large. An arrow that lands 20 feet from the bull’s-eye is, therefore, less than one standard deviation beyond the mean, and a fairly probable event.
We see clusters of things all the time, from the size of people’s footprints at the beach to scores on national tests. A very tight clustering of values is remarkable, and makes us ask “What would make the arrows line up as they did in figure 3B?” Possibly tornado-like winds, or a magnetic vortex that gripped every arrow-tip and whirled it down in a tight ring. We do not know why, but the power of statistics is such that we do not need to. Given the standard deviation of the situation depicted in figure 3B, an arrow falling 20 feet beyond the bull’s-eye would be a most unlikely thing. This position would be many standard deviations beyond the mean. It would require an explanation.
Your Diagnosis
The standard DEXA test in the United States scans three sites: the lumbar vertebrae, the total hip, and the surgical neck of the thigh bone. The image your bones generate in the DEXA scan is compared with the average image seen in healthy 25- to 30-year-old women, and with average healthy women of your age, height, and weight. Your T-score is how many standard deviations your measured bone mineral density is beyond the average DEXA value seen in healthy women between 25 and 30 years of age; the Z-score is how many standard deviations your score lies beyond the average DEXA value seen in healthy women of your age, height, and weight. A positive score puts you above the average, a negative score indicates that the average person has stronger bones than you do. If your T-score falls 2.5 standard deviations below the mean, indicating that your bones are weaker than 99 percent of women between ages 25 and 30, women at the peak of their bone strength, then you’ve got osteoporosis. T-scores that fall between 1.0 and 2.5 standard deviations below the mean indicate osteopenia, a danger zone—the bones are approaching an osteoporotic state. The DEXA-based diagnostic criteria are quite precise. If the T-score at any of the three sites reaches either of these values, then the diagnosis is made.
How Reliable Is the DEXA Scan?
The correlation between a low bone mineral density reading on the DEXA scan and a fracture is stronger than the relationship between high blood pressure and stroke.26 Still, the test is not universally or entirely accurate. DEXA scans detect 9 out of 10 people with osteoporosis and wrongly diagnose healthy people somewhere between 5 and 7 percent of the time.
There is a 3–4 percent margin of error in the instruments.27 if your score has fallen no more than 0.1, don’t take it too seriously, since a number of external conditions may affect the accuracy of the test. These include
• Spinal surgery,
• Hardware (certain pain-relief devices, or plates, rods, or screws used to fix broken bones),
• Vertebral deformities, including arthritis and previous fractures, and
• Calcified blood vessels that may lie close to the spinal column.
Women should not undergo DEXA scans during pregnancy. Even the minuscule amounts of radiation emitted by the bone scan are thought harmful to a fetus. For patients with any conditions that contraindicate a DEXA scan, there are other tests. The peripheral dual-energy X-ray absorptiometry (pDEXA) measures bone density in distal bones, such as the finger, wrist, and heel. Single-energy X-ray absorptiometry (SEXA) uses a small, portable device similar to the DEXA scanner, but it emits a single X-ray beam rather than two. It is used to measure bone density in the heel or forearm. If results are abnormal, and a more specific test such as the standard DEXA scan cannot be performed, it is wisest to treat the individual just as one would if the DEXA scan were positive.28
There are other ways to diagnose osteoporosis and osteopenia. Ultrasound, particularly of the heel or the wrist bones, is used when the DEXA scan is either unavailable or inadvisable.29 Magnetic resonance imaging (MRI) and computed tomography (CT) scanning are used today in research, such as bone quality studies. They are also valuable under special conditions when other diagnostic possibilities loom, such as the bone-affecting cancer multiple myeloma, or metabolic or nutritional states such as osteomalacia.
Whether detected through DEXA, pDEXA, SEXA, ultrasound, MRI, or CT scanning, the idea is always the same: Thin and weak bones are vulnerable to fracture. How vulnerable?
Bone Density and Fracture Risk
One standard deviation below the mean in a T-score comes out somewhere between 2.0 and 2.6 times greater probability of hip fracture. The correlation between BMD and fracture risk is so strong that researchers at Washington University have constructed a “fracture risk calculator” to estimate fracture risk based on bone density; you can try it yourself at http://courses.washington.edu/bonephys/FxRiskCalculator.html.

Figure 5. The relationship between bone density and factor risk is shown in results from a 39,000-patient study conducted in Europe, North America, and Japan. 30
Yet we must bear in mind that the risk of fracture in any given individual is a function of other factors as well:
1. Gender and age (see figure 5)
2. Bone quality: This subject is being pursued quite vigorously today. New micro-MRI technology and fractal analysis may enable research that assesses the importance of bones’ inner structure in their ability to resist fracture.
3. Sensory losses: Any deficit of sight, hearing, or the ability to feel one’s feet increases the danger of a fall. Those in need should be encouraged to use eyeglasses, hearing aids, and assistive devices. This is especially true for people with osteoporosis.
4. Activity level: More daily activity will strengthen bones, but higher activity levels also put people at greater risk. Pick your exercise carefully.
As with just about any medical condition, there are two sides to fracture: susceptibility, that is, bone fragility, and exposure, that is, the history and environment that determines your risk of falling. Race-car drivers have a higher risk of fracture, regardless of their DEXA scores.
One reliable measure of susceptibility and exposure to falls, the Morse Fall Scale, sums mental status, independence in walking, any other diagnoses, IV or heparin-lock use, and, naturally, any history of falls. On this basis the scale determines your risk of sustaining a fracture, very much like the way college admission committees determine whether candidates will make the grade.31 The Cummings Hip Scale uses physical and social function, bodily pain, emotional role, mental health, and general vigor to calculate the same thing.32 Both methods quantify an individual’s exposure to falls, and therefore an appropriate level of concern about having strong bones.
Your Allies against Fractures
Fractures from falls are so detrimental to health that it is important to marshal all foTXTrces against them. Exposure to risk can be reduced, but the aging processes are inexorable. It makes sense to initiate contrary processes that are stronger. There are three basic elements to work on:
• Strength. Greater muscular strength puts greater strain on the bones in almost every action. The stress stimulates the bones to create more bone tissue. Greater strength also better counters gravity, reducing vulnerability to falling. Be aware that muscular strength can overpower bone strength. We once treated a circus strong man who had met a strong man from another circus. Unsurprisingly, they arm wrestled. His humerus was broken in three places: the combined strength of their biceps (and their wills to win) were stronger than his bone!
• Mental status. Decreased ability to recognize objects, such as furniture, automobiles, and staircases; reduced alertness; and confusion lead to fracturing falls. Less activity goes with lower mental status.
• Balance. People with better balance have fewer falls. A simple fact, but an important one to remember.
Naturally these are interrelated: a person of low activity level is, insofar as that is concerned, at lower risk of fracture. But strength, balance, and bone quality (as well as bone density) all tend to improve with greater activity. On the other hand, for a person of lower mental status, a person who is disoriented, extremely forgetful, or distractible, higher activity is definitely a higher risk. It is important to choose the right level of activity for an individual’s condition.