We’ve all heard it. Eat more fish! Eat more fish! Get your daily minimum requirement of essential omega-3 fatty acids by eating more fish! They’re rich in omega-3s! But what are the facts behind all of this rhetoric?
The American Heart Association urges all adults to eat oily fish at least twice weekly to reduce their cardiovascular disease risk. Other public health organizations and government health agencies make similar recommendations. But what health risks are they overlooking, and why are they overselling the benefits of consuming fish?
You won’t hear any debate from me about the importance of omega-3 fatty acids for human health. Our bodies cannot produce omega-3s, so we must get them from food sources. But over the past half-century, omega-3s have been crowded out of our diet by the less healthful omega-6 fatty acids that are found in meat, cooking oils, and processed foods.
There are three kinds of omega-3 fatty acids. The first two, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), can both be synthesized in the human body from the third kind, alpha-linolenic acid (ALA). This is an important point to emphasize, and I will come back to it later: ALA can be obtained from plants, and it’s all you need. ALA provides the human body with the other two types of omega-3s. You don’t need fish or fish oils.
The health benefits of consuming omega-3 fatty acids are well documented. According to research scientists at the Linus Pauling Institute at Oregon State University, many medical studies have concluded that omega-3 fatty acid intake helps reduce the risk of cardiovascular disease. Omega-3 intake also has been found to decrease the risk of heart attack and other sudden heart conditions. In addition, Alzheimer’s disease and dementia might be triggered in people who don’t consume enough omega-3s.
Beyond preventing some health problems, omega-3 fatty acids can also alleviate existing problems. For example, increasing fatty acid consumption helps treat type 2 diabetes and lower elevated serum triglycerides. In addition, studies indicate that omega-3 fatty acids may be beneficial in treating depression, bipolar disorders, and even schizophrenia. Omega-3s also decrease joint tenderness in rheumatoid arthritis patients, and they are considered important for visual and neurological development in infants, who can get these fatty acids from mother’s milk.
Mainstream medical practitioners usually recommend that we consume 300 to 400 milligrams of omega-3 fatty acids every day to absorb the amounts we need to bolster immune system health and prevent the range of diseases triggered by omega-3 deficiencies. But where should we get the omega-3s that we need? Are fish the only and best source? Or has the public been sold on consuming a product based on vested economic interests, rather than real, scientific data?
Most consumers aren’t aware that the omega-3 fatty acids found in fish aren’t produced by fish. These fatty acids are produced only by plants. When small fish eat marine algae, they absorb the algae’s omega-3 fatty acids, and when large fish gobble up the small fish, they absorb the fatty acids stored in the smaller fish. This process continues up the food chain, until humans consume larger, cold-water fish, such as herring, salmon, and albacore tuna, which contain high concentrations of bioaccumulated fatty acids.
There is evidence that consuming fatty acids from fish raises the risk of contracting coronary heart disease, rather than lowers it, as is commonly proclaimed in so much health-related information today. The earliest research emerged in a 1997 study done in Finland, which examined 21,930 men (ages fifty to sixty-nine) who had no history of cardiovascular disease. It so happened that these men were smokers, so it’s conceivable there was an interaction between eating fish and smoking cigarettes, but since the study authors focused on the omega-3 fatty acids in fish, we have evidence for an association with heart disease that can’t be overlooked. Here is what the research team found: “The intake of omega-3 fatty acids from fish was directly related to the risk of coronary death. . . . The hypothesis that frequent intake of fish is protective of coronary heart disease has recently been challenged by three recent prospective studies.”1
Plant sources of omega-3 fatty acids carry no associated health risks. Of all the plants and nuts containing omega-3s, the richest source of this essential nutrient is marine algae. Studies of human subjects who took marine algae supplements determined that they are a safe, convenient, plant-based source of DHA. In addition, there is evidence that these supplements are easily absorbed by the human body, and they may be absorbed even more efficiently when taken with meals.2
So my strong advice to you is to cut out the middleman (fish) and go right to the source (marine algae) for your omega-3 needs. Eating fish for their omega-3 content is a little like using an intermediary every time you want to withdraw money from your own bank account. Using an intermediary is inefficient. The same holds true when you keep fish in your diet. Consuming fish or fish oil taxes your well-being and adds nothing to your health that you can’t get from more healthful and risk-free sources.
A cheap fish is becoming a staple in the diets of low-income people. It’s called tilapia, and consumption in the United States alone doubled between 2003 and 2010. Possible reasons are that tilapia is easy to produce in large quantities on fish farms, and it thrives by consuming inexpensive corn-based feeds. Yet this newly popular farmed fish poses a bigger risk of heart disease than even pork or hamburger. Why? Because tilapia contains very low levels of beneficial omega-3 fatty acids but very high levels of omega-6 fatty acids. This imbalance, contributes to heart disease and other health problems.
This problem is not exclusive to tilapia but also extends to farmed catfish, as was discovered by a team of researchers from the Wake Forest University School of Medicine. The results were published in a 2008 edition of the Journal of the American Dietetic Association.3 The researchers examined tilapia and catfish from seafood distributors that supply supermarkets and restaurants. The fish came from fish farms in several nations and from two South American enterprises that operate international fish distribution companies. All of the samples had been frozen in preparation for gas chromatography analysis of their fatty acid levels.
Here is what one of the researchers told Science Daily: “The recommendation by the medical community for people to eat more fish has resulted in consumption of increasing quantities of fish such as tilapia that may do more harm than good.”4 In both farmed tilapia and catfish, the ratio of omega-6s to omega-3s is 11:1, compared to a 1:1 ratio in salmon. Omega-6 fatty acids contribute to the narrowing of coronary arteries, which is a major risk factor for heart attacks in humans.
Floyd Chilton, a senior author of the study and a professor of physiology and pharmacology at Wake Forest, criticized health organizations for advising consumers to eat more fish. He said, “The classical Hippocratic admonition is ‘First, do no harm.’ I think it behooves us to consider this critical directive when making dietary prescriptions for the sake of health. Cardiologists are telling their patients to go home and eat fish, and if the patients are poor, they’re eating tilapia. And that could translate into a dangerous situation.”5
By now, you know that consuming fish presents a risk to your health because of all the harmful elements they possess, including chemical pollutants and unwanted fats, that can be passed on to you. Still, some people believe it’s okay to use fish oil supplements instead of eating fish to get higher levels of omega-3 fatty acids in their diet. There are many reasons why this is not a safe bet.
Whenever oil is extracted from fish and exposed to air for any length of time, it becomes rancid. Fish oil oxidizes as soon as it’s exposed to oxygen, light, or heat. To extract oil from fish, the entire fish is usually minced, and the oil is extracted using heat and chemical solvents. This process can sometimes create carcinogens, which are left as by-products in the oil.
Fish oil processors usually disguise the dead fish smell by adding antioxidants and preservatives. Some processors also try to remove the chemical contaminants, such as mercury and dioxins, in the fish, which diminishes omega-3 content. They then seal the fish oil in gel capsules so the smell can’t escape. Break open one of these capsules sometime. The rancid odor will assault your sense of smell. (Be warned that fish oil occasionally shows up as an additive in margarine and shortenings produced by major food companies.)
A healthful alternative to fish oil has always been flaxseed oil, which became a fixture in the pantheon of health elixirs as far back as 650 BC when Hippocrates lauded its many therapeutic uses. You don’t have to use flaxseed oil to get the health benefits of flax. Alternatively, you can eat the flaxseeds themselves—either raw, sprouted, or ground up and sprinkled on salads—to get the highest possible concentrations of omega-3s. Chia seeds and hempseeds can be used in the same way.
Fish oil is often promoted by mainstream doctors as a good source of omega-3 fatty acids for people who are at risk of inflammatory bowel diseases. The problem is, fish oil increases the risk of colon cancer and severe colitis. Evidence of this link emerged late in 2010, and many medical practitioners, not to mention consumers, are still unaware of the connection.
Nutrition scientists at Michigan State University hypothesized that feeding fish oil enriched with DHA to mice would decrease their cancer risk. This was a common assumption among mainstream nutrition researchers. What the scientists found, however, was the exact opposite of what the researchers believed to be true. “Our findings support a growing body of literature implicating harmful effects of high doses of fish oil consumption in relation to certain diseases,” commented Jenifer Fenton, the food and human nutrition scientist who led the research team.6
Science Daily reported these findings with stark language: “The research team found an increase in the severity of the cancer and an aggressive progression of the cancer in not only the mice receiving the highest doses but those receiving lower doses as well.”7 It took only four weeks for the tumors to develop in the mice as a result of the increased inflammation caused by the fish oil. While it’s certainly true that these alarming findings were the result of an experiment using lab animals, the mouse has proven over time to be a good indicator of potential disease effects in humans.
This research underscores the dangers of using high doses of fish oil, despite the recommendation of the fish oil manufacturing industry. By some estimates, the recommended doses are twenty times or more what the average person needs. These high levels may be producing overdose reactions in the human body.
A decade before these findings about cancer were released, British researchers with the Institute of Human Nutrition discussed the negative effects of fish oil supplementation and how it could raise the risk of cancer in humans at the International Society for the Study of Fatty Acids and Lipids conference in Japan. It’s remarkable to me that so much time elapsed before additional research showing a possible cancer link was undertaken, given what’s at stake for human health.
Clearly we need to pay close attention to these cancer findings. This is especially true if you use, or have ever used, high levels of fish oil in the belief that its omega-3 content would be beneficial to your health.
It may be a challenge for many people to connect the dots between optimal physical exercise and their consumption of fish oil, but that’s just what a team of French medical researchers did in 2003. Their findings, which were published in the British Journal of Nutrition, should be of concern to any aspiring athlete: fish oil supplementation reduces exercise effectiveness.
The researchers came to this conclusion by measuring exercise performance in a group of men. For the twenty days before the test, each man took six grams of fish oil per day. The researchers found that fish oil supplements decrease fuel production in the muscles during exercise. This decrease in energy could negatively affect the performance of any competitive athlete, whether a cyclist, runner, or bodybuilder.8
1. Fish oil benefits pregnant women. Producers and purveyors of fish oil products have promoted the idea that their supplements can help pregnant women avoid postpartum depression, while simultaneously promoting the cognitive development of their unborn children. Medical researchers in Australia proved this claim to be false in a 2010 study that tested the response of 2,400 pregnant women to fish oil. The women were randomly assigned to take either 800 milligrams of DHA from fish oil per day or placebo capsules containing vegetable oil. Six months after the women gave birth, the rates of postpartum depression were no different between the two groups, indicating that fish oil had no beneficial effect. In addition, the children of women from the two groups did not score any differently at age eighteen months on a battery of tests designed to show whether the mother’s intake of fish oil had been beneficial to them while still in the womb. The fish oil industry ignored these findings.9
2. Fish oil slows mental decline. Another marketing claim trumpeted by the fish oil industry is that fish oil slows the onset of mental decline associated with Alzheimer’s disease. Still another 2010 study has demolished this contention. Funded by the National Institute on Aging and published in the Journal of the American Medical Association, the study randomly assigned four hundred men and women in their mid-seventies who were likely to have Alzheimer’s to either a placebo group or a group that took two grams of DHA from fish oil per day. After eighteen months, there was no difference in the degree of mental decline between the two groups, as measured by a rating scale and mental testing.10
Here is the specific language the study authors used to describe their conclusion about the DHA in fish oil: “Supplementation with DHA compared with placebo did not slow the rate of cognitive and functional decline in patients with mild to moderate Alzheimer’s disease. . . . The hypothesis that DHA slows the progression of mild to moderate Alzheimer’s disease was not supported, so there is no basis for recommending DHA supplementation for patients with Alzheimer’s disease.”11 That clearly tells us that fish oil should not be touted as a preventative for cognitive deterioration and age-related decline.
3. Fish oil strengthens the immune system. Many mainstream physicians love to believe this one, though they seem vague on the details of how it is supposed to happen. We all know how important our immune systems are: they play an indispensible role in preventing illness and disease. So why would you knowingly and consciously engage in an activity that weakens your immune system and makes life-threatening health problems more likely? Supplementing with fish oil may be doing exactly that.
There are a number of ways that omega-3 derivative fish oils weaken our immune systems according to research presented by the International Society for the Study of Fatty Acids and Lipids during a 2000 conference in Japan. These initial findings were documented and expanded in a 2003 study published in the prestigious journal Lipids: “High fish oil intake may not be beneficial long term; i.e., it may compromise host immunity and may address only the secondary consequences of immune activation in some clinical conditions.”12
4. Fish oil can prevent cancer. This myth is founded on a huge reservoir of wishful thinking, stirred up by the fish oil manufacturing industry. Several studies in major peer-reviewed medical journals have disproved the theory that fish oil prevents cancer. Let’s focus on one of them, published in a 2006 edition of the British Medical Journal. Thirteen British researchers reviewed nearly one hundred studies that had been conducted worldwide on omega-3 fatty acids and cancer prevention. From this wealth of research, an inescapable conclusion emerged: “We found no evidence that omega-3 fats had an effect on the incidence of cancer, and there was no inconsistency.”13
5. Fish oil prevents artery inflammation. You’ve probably heard this one, too, and wouldn’t it be wonderful if it were the truth? Imagine clearing your arteries of inflammation-causing plaque every time you took a fish oil supplement. In a 2004 study published in Current Atherosclerosis Reports, several researchers reviewed the available evidence and reported this finding: “Fish oil did absolutely nothing significant to decrease the inflammation as evidenced by the failure of CRP [C-reactive protein] to decrease. . . . There was no evidence for an anti-inflammatory effect as judged by CRP levels.”14
6. Fish oil supplementation can prevent heart disease. The widely held view that taking fish oil can decrease your risk of cardiovascular disease persists despite numerous well-designed studies that contradict this notion. In 2010 researchers at the University of Pittsburgh Graduate School of Public Health presented findings to the American Diabetes Association that showed that consuming more omega-3 fatty acids from fish doesn’t lower heart disease risk in women with type 1 diabetes. People with this type of diabetes are generally at much greater risk of developing heart disease, so this population was ideal for determining whether fish oil can stop or reverse the buildup of plaque in the arteries.15
These findings supported previous research, such as the 2002 study in the journal Cardiovascular Research that examined the effect of omega-3s from fish on cerebral arteries and the incidence of stroke. According to the authors, both the fish oil groups and the control groups showed close to equal atherosclerotic progression: “In this group of selected patients with documented coronary artery disease, omega-3 PUFA [polyunsaturated fatty acids] given for two years did not demonstrate an effect on slowing progression of atherosclerosis in carotid arteries as measured by ultrasound.”16
An earlier study from 1999 that was published in the Annals of Internal Medicine examined whether omega-3s from fish or fish oil capsules could prevent atherosclerosis. After two years, researchers concluded that arterial clogging had worsened in both the fish oil group and the placebo control group. Of the forty-eight patients in the placebo group, forty-one showed disease progression based on coronary angiography measurements. Among the fifty-five patients in the fish oil group, thirty-nine showed disease progression.17
A US study involving a great number of subjects examined whether increasing fish in the diet decreased the risk of coronary heart disease. Researchers tracked 44,895 male health professionals (ages forty to seventy-five) over a six-year period using validated dietary questionnaires. Here is what the Harvard School of Public Health research team concluded in 1995: “These data suggest that increasing fish intake from one to two servings per week to five to six servings per week does not substantially reduce the risk of coronary heart disease among men who are initially free of cardiovascular disease.”18
Finally, in case you need even more evidence, here is another fish oil study to think about. University of Wales College of Medicine researchers studied 3,114 men (age seventy and younger) who complained about angina. They were divided into four groups: group one was advised to eat two portions of oily fish each week or to take three fish oil capsules daily; group two was advised to eat more fruit, vegetables, and oats; group three was asked to do what both groups one and two were doing; and group four was given no specific dietary advice.
At years three and nine of the study, mortality among the four groups was determined. The researchers found that the risk of cardiac death was higher among subjects who had been advised to eat oily fish, and the risk for sudden cardiac death was even greater. Furthermore, this excess risk was largely seen among the subgroup given fish oil capsules. These results, which were published in the European Journal of Clinical Nutrition, led the British researchers to this disturbing and inescapable conclusion: “Men advised to eat oily fish, and particularly those supplied with fish oil capsules, had a higher risk of cardiac death.”19
Why fish oil can’t possibly work as claimed was the subject of an intriguing article in the science journal Explore. The article was researched and written by Brian Peskin, a former professor in the Department of Pharmacy and Health Sciences at Texas Southern University. Peskin made a strong case that fish oil supplements supply EPA and DHA in greater amounts than the human body can ever naturally produce—or effectively absorb—on its own.20 This overdosing would help to explain why fish oil might worsen the condition of diabetic patients by raising their blood sugar levels and thwarting the insulin response. It also explains why fish oil causes other health problems.
The article makes a strong case that using fish oil supplements is a misguided attempt to correct essential fatty acid deficiencies in mainstream diets, which are based on processed foods. Because Peskin found that the constituents of fish oils “are far from being correct physiologically for most (human) tissue,” he created a plant-based formula that is more functional and better absorbed by the human body.21 The article also describes the importance of a substance Peskin calls parent essential oils (PEOs), which are the building blocks of all the omega-3 fatty acids. Peskin defines PEOs as unadulterated oils that contain fatty acids but have not been subjected to chemical processing or excessive heat treatments.
In the June 2011 edition of his newsletter, Second Opinion, physician Robert Rowen wrote about PEOs and analyzed Peskin’s argument. Rowen described a study that used a medical device called a digital pulse analyzer to measure the effects of plant-based PEOs on the human arterial aging process. The research sample included thirty-five people (thirteen males and twenty-two females, age seventy-five and younger) who took PEOs. Half took the PEOs for less than twenty-four months, and half took them for a longer period. In twenty-five of the test subjects, arterial flexibility, a key determinant of heart disease risk, improved. Overall, the subjects’ mean biologic arterial age dropped by nearly nine years, which is truly remarkable.22
Here’s how Rowen characterized the results: “PEOs are so called because they are the eighteen carbon chain fatty acids that are the only true ‘essential fatty acids.’ The longer-chain fatty acids of marine oils, including EPA and DHA, are not ‘essential’ fatty acids. Your body makes these longer-chain fatty acids automatically from the true parent essential oils—if you’re getting enough of the PEOs. We’ve come to believe that somehow humans don’t automatically make sufficient longer-chain fatty acids [EPA and DHA] from the parent oils. We do!!! And this study proves that it’s better to let your body make what it needs in its own wisdom, than to force-feed it what it might not want or need.”23
“The tragedy,” continued Rowen, “is that fish oil taken in the amounts that most physicians recommend can overdose you with 20 times too much DHA and 250 to 500 times too much EPA. Just think what would happen if you took 250 aspirin capsules—you’d be dead. Of course, fatty acids are not a drug like aspirin. But anything can act like a drug in your body if you take it in pharmacological amounts. That’s my concern about the unbridled rise of marine oil consumption. We just don’t know what [it] will do in the long run.”24
This research underscores that fish oil doesn’t provide the eighteen carbon-chain fatty acids known as parent essential oils. In fact, there is evidence that fish, krill, and oils from other marine animals contribute to the oxidation process that is a major cause of vascular disease.
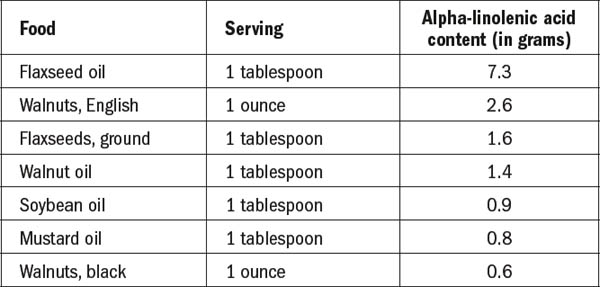
Table 3. Plant-based sources of omega-3 fatty acids (ALA)
Source: Linus Pauling Institute, Oregon State University
When people ask me about a healthful replacement for fish and krill oil, I suggest they try a proprietary blend of chia seeds produced by a company called Mila. I’ve recommended this product for several years, and I’ve seen resounding health benefits from this balanced omega-3 and omega-6 food. Check it out in the supplements store at hippocratesinst.org.
It’s ironic, even strange, that mainstream nutritionists note that marine algae produces the omega-3s that fish bioaccumulate, yet they fail to acknowledge that marine algae can be the most direct and natural food source of these essential fatty acids. It’s as if these traditionalists are so fixated on the alleged health advantages of fish that they have never imagined that green and blue algae could be a human food source. Maybe these so-called experts are so stubborn in their own dietary habits that their professional judgment has become impaired.
Nutritionists also overlook several other foods that are sources of omega-3 fatty acids: chia seeds, raspberry seeds, walnuts, Brazil nuts, sesame seeds, avocados, and dark leafy green vegetables, such as kale, spinach, and collard greens. One of the best ways to get ample amounts of omega-3s in your diet is to eat combinations of these foods in large quantities as often as possible. Let’s take a closer look at three of the top plant-based omega-3 sources: marine algae, spinach, and walnuts.
No longer considered just “pond scum,” blue-green algae, also known as cyanobacteria, has achieved new respectability as a healing agent and a source of healthful nutrients, including omega-3 fatty acids. These algae can be found in both seawater and freshwater environments.
Spirulina, when sold in digestible forms, is a therapeutic type of blue-green algae. Two species—Arthrospira platensis and Arthrospira maxima—are now being used as dietary supplements. Spirulina is rich in protein (up to 77 percent by dry weight) and contains all the essential amino acids, making it a complete protein. It also has thiamine, riboflavin, nicotinamide, pyridoxine, folic acid, and vitamins C, D, A, and E.
Chlorella is a single-celled green algae that contains the photosynthetic pigments chlorophyll a and b. It also is a complete protein. Dried chlorella is composed of nearly 50 percent protein and 10 percent vitamins and minerals. The remaining content is fats and carbohydrates. Chlorella acts as a detoxifier when absorbed by humans. In addition, chlorella’s ability to reduce cholesterol and high blood pressure and to enhance the immune system has been proved in scientific experiments.
In a three-volume series that I authored, Food IS Medicine: The Scientific Evidence, I collected thousands of peer-reviewed medical studies showing the healing powers of various plant foods, and marine algae turned out to be the most powerful healing agent of all. About forty-five different medical conditions, from cancer to diabetes, can be prevented or treated using marine algae. Here are some examples of the research I found in scientific journals:
• Nutrition, 2009. Key finding: “Chlorella supplementation resulted in the conservation of plasma antioxidant nutrient status and improvement in erythrocyte [red blood cell] antioxidant enzyme activities in subjects. Therefore, our results are supportive of an antioxidant role for chlorella and indicate that chlorella is an important whole-food supplement that should be included as a key component of a healthy diet.”25
• Journal of Medicinal Food, 2009. Key finding: “In humans, Spirulina maxima intake decreases blood pressure and plasma lipid concentrations, especially triacylglycerols and low-density lipoprotein cholesterol, and indirectly modifies the total cholesterol and high-density lipoprotein cholesterol values.”26
• Journal of Medicinal Food, 2001. Key finding: “These findings suggest the beneficial effect of spirulina supplementation in controlling blood glucose levels and in improving the lipid profile of subjects with type 2 diabetes mellitus.”27
• Annals of Nutrition and Metabolism, 2008. Key finding: “The results demonstrate that spirulina has favorable effects on lipid profiles, immune variables, and antioxidant capacity in healthy, elderly male and female subjects and is suitable as a functional food.”28
• IBC Library Series, 1998. Key finding: A team of medical researchers at Royal Victoria Hospital in Canada examined how Super Blue-Green Algae strengthens the human immune system. In this double-blind study, fifty people consumed 1.5 grams of this algae. As a result, their natural killer cell activity increased significantly, provoking these immune cells to move from the bloodstream into body tissues to scavenge for sick cells and toxic invaders.29
Spinach, one of the most nutritious of all vegetables, contains high levels of antioxidants and vitamins A, C, E, and K, along with zinc, iron, selenium, folic acid, and numerous other nutrients in addition to omega-3 fatty acids. Medical studies have documented that spinach consumption reduces the risk for at least nine types of cancer. Here are three representative studies that show the health benefits of eating spinach:
• Journal of Neuroscience, 1998. Key finding: Spinach may be beneficial in retarding functional age-related cognitive behavioral deficits and may have some benefit in combating neurodegenerative disease.30
• Asia Pacific Journal of Clinical Nutrition, 2008. Key finding: Spinach was one of the top candidates among twenty-two dietary sources tested for the potential to treat secondary complications of diabetes.31
• Oncology Reports, 2005. Key finding: Spinach may suppress tumor growth by suppressing angiogenesis and might be one of the best anticancer agents.32 (Angiogenesis refers to the formation of blood vessels.)
English walnuts are known to contain higher concentrations of omega-3 fatty acids than any other type of nuts. In addition, walnuts boast high levels of protein, magnesium, phosphorous, potassium, and such vitamins as A, B12, C, D, and E. Here are some noteworthy research findings about walnuts:
• European Journal of Clinical Nutrition, 2009. Key finding: Walnuts produced significant reductions in fasting insulin levels, an effect seen largely in the first three months of use.33
• American Journal of Cardiology, 2006. Key finding: Sources of plant-derived omega-3 fatty acids include walnuts. Because of the remarkable cardioprotective effects of omega-3 fatty acids, consumption of food sources that provide them should be increased in the diet.34
• European Journal of Clinical Nutrition, 1998. Key finding: Walnuts in the diet showed changes that might be expected to reduce the risk of cardiovascular disease.35
• Nutrition and Cancer, 2008. Key finding: Research mice that were engineered to develop cancer were fed a diet including walnuts (amounts equivalent to two ounces a day for humans) and were compared to mice that were fed a similar diet without walnuts. The mice that ate walnuts were less likely to develop breast tumors. After 145 days, 100 percent of the mice that were not fed walnuts had developed cancer, whereas only 50 percent of the mice that ate walnuts had developed cancer.36
BLUE WATER BITE
A Exclusive Limited Edition Print created by Artist Jim Barry