CHAPTER |
Everyone Has a Role in Supporting Healthy Eating Patterns |
Introduction
The previous chapters describe the characteristics of healthy eating and physical activity patterns, and it is clear that across all population groups, the vast majority of people in the United States are not meeting these recommendations. In general, Americans are consuming too many calories, are not meeting food group and nutrient recommendations, and are not getting adequate physical activity. In practice, aligning with the Dietary Guidelines (see Aligning With the Dietary Guidelines for Americans: What Does This Mean in Practice? in the Introduction) at the population level requires broad, multisectoral coordination and collaboration. This collective action is needed to create a new paradigm in which healthy lifestyle choices at home, school, work, and in the community are easy, accessible, affordable, and normative. Everyone has a role in helping individuals shift their everyday food,[1] beverage, and physical activity choices to align with the Dietary Guidelines.
The Dietary Guidelines provides recommendations that professionals, especially policymakers, can translate into action to support individuals. This chapter discusses a number of considerations related to translating the Dietary Guidelines into action, including the significance of using multiple strategies across all segments of society to promote healthy eating and physical activity behaviors; the development of educational resources that deliver information in a way that is compelling, inspiring, empowering, and actionable for individuals; and the need to focus on individuals where they are making food and beverage choices.
About This Chapter
This chapter focuses on the fifth Guideline:
1. Follow a healthy eating pattern across the lifespan. All food and beverage choices matter. Choose a healthy eating pattern at an appropriate calorie level to help achieve and maintain a healthy body weight, support nutrient adequacy, and reduce the risk of chronic disease.
2. Focus on variety, nutrient density, and amount. To meet nutrient needs within calorie limits, choose a variety of nutrient-dense foods across and within all food groups in recommended amounts.
3. Limit calories from added sugars and saturated fats and reduce sodium intake. Consume an eating pattern low in added sugars, saturated fats, and sodium. Cut back on foods and beverages higher in these components to amounts that fit within healthy eating patterns.
4. Shift to healthier food and beverage choices. Choose nutrient-dense foods and beverages across and within all food groups in place of less healthy choices. Consider cultural and personal preferences to make these shifts easier to accomplish and maintain.
5. Support healthy eating patterns for all. Everyone has a role in helping to create and support healthy eating patterns in multiple settings nationwide, from home to school to work to communities.
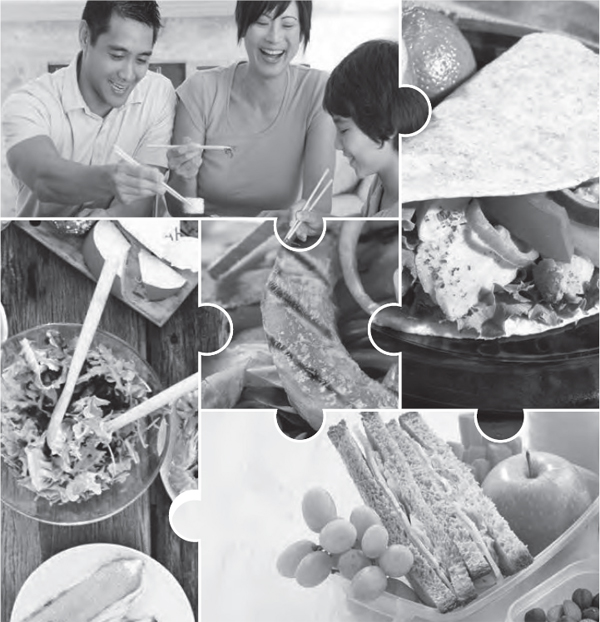
The Social-Ecological Model (Figure 3-1) is used as a framework to illustrate how sectors, settings, social and cultural norms, and individual factors converge to influence food and physical activity choices. The chapter describes contextual factors that influence eating as well as physical activity behaviors and identifies opportunities for professionals, including policymakers, to implement strategies that can help individuals align with the Dietary Guidelines.
Creating & Supporting Healthy Choices
As shown in the Social-Ecological Model, a multitude of choices, messages, individual resources, and other factors affect the food and physical activity choices an individual makes, and these decisions are rarely made in isolation. The following section describes the various components in the Social-Ecological Model and how they play a role in influencing the decisions individuals make about foods and physical activity. Ideas for engaging these components in collaborative ways to influence individual decisions, and ultimately social and cultural norms and values to align with the Dietary Guidelines, are provided.
The Social-Ecological Model
Consistent evidence shows that implementing multiple changes at various levels of the Social-Ecological Model is effective in improving eating and physical activity behaviors. For example, strong evidence from studies with varying designs and generally consistent findings demonstrates that school policies designed to enhance the school food setting leads to improvements in the purchasing behavior of children, resulting in higher dietary quality of the food consumed during the school day. For adults, moderate evidence indicates that worksite nutrition policies can improve dietary intake, and approaches targeting dietary intake and physical activity can favorably affect weight-related outcomes. These examples demonstrate how support and active engagement from various segments of society are needed to help individuals change their eating and physical activity behaviors and achieve positive outcomes. Approaches like these have the potential to improve population health if they can be incorporated into existing organizational structures and maintained over time. Among the components of the Social-Ecological Model, sectors and settings influence change at the population level and are addressed first in this discussion.
Sectors
Sectors include systems (e.g., governments, education, health care, and transportation), organizations (e.g., public health, community, and advocacy), and businesses and industries (e.g., planning and development, agriculture, food and beverage, retail, entertainment, marketing, and media).
Figure 3-1.
A Social-Ecological Model for Food & Physical Activity Decisions
The Social-Ecological Model can help health professionals understand how layers of influence intersect to shape a person’s food and physical activity choices. The model below shows how various factors influence food and beverage intake, physical activity patterns, and ultimately health outcomes.
DATA SOURCES: Adapted from: (1) Centers for Disease Control and Prevention. Division of Nutrition, Physical Activity, and Obesity. National Center for Chronic Disease Prevention and Health Promotion. Addressing Obesity Disparities: Social Ecological Model. Available at: http://www.cdc.gov/obesity/health_equity/addressingtheissue.html. Accessed October 19, 2015. (2) Institute of Medicine. Preventing Childhood Obesity: Health in the Balance, Washington (DC): The National Academies Press; 2005, page 85. (3) Story M, Kaphingst KM, Robinson O Brien R, Glanz K. Creating healthy food and eating environments: Policy and environmental approaches. Annu Rev Public Health 2008; 29:253-272.
These sectors all have an important role in helping individuals make healthy choices because they either influence the degree to which people have access to healthy food and/or opportunities to be physically active, or they influence social norms and values. Positive influences on social norms and values can occur through effective health promotion and marketing strategies.
Professionals in these sectors have many opportunities to identify and develop strategies that help individuals align their choices with the Dietary Guidelines. Strategies could include supporting policy and/or program changes, fostering coalitions and networks, developing or modifying products and menus, and/ or creating opportunities to be physically active. To ensure widespread adoption of these sectoral efforts, complementary efforts can include training, education, and/or motivational strategies.
Settings
Individuals make choices in a variety of settings, both at home and away from home. Away-from-home settings include early care and education programs (e.g., child care, preschool), schools, worksites, community centers, and food retail and food service establishments. These organizational settings determine what foods are offered and what opportunities for physical activity are provided. Strategies to align with the Dietary Guidelines that are implemented in these settings can influence individual choices and have the potential for broader population-level impact if they are integrated with strategies by multiple sectors. In combination, sectors and settings can influence social norms and values.
Social & Cultural Norms & Values
Social and cultural norms are rules that govern thoughts, beliefs, and behaviors. They are shared assumptions of appropriate behaviors, based on the values of a society, and are reflected in everything from laws to personal expectations. With regard to nutrition and physical activity, examples of norms include preferences for certain types of foods, attitudes about acceptable ranges of body weight, and values placed on physical activity and health. Because norms and values are prevalent within a community or setting, changing them can be difficult. However, changes to sectors and settings—as previously discussed—can have a powerful effect on social and cultural norms and values over time and can align with the Dietary Guidelines.
Individual Factors
Individual factors are those that are unique to the individual, such as age, sex, socioeconomic status, race/ethnicity, the presence of a disability, as well as other influences, such as physical health, knowledge and skills, and personal preferences. Education to improve individual food and physical activity choices can be delivered by a wide variety of nutrition and physical activity professionals working alone or in multidisciplinary teams. Resources based on systematic reviews of scientific evidence, such as the Dietary Guidelines and the Physical Activity Guidelines for Americans, provide the foundation for nutrition and public health professionals to develop programs and materials that can help individuals enhance their knowledge, attitudes, and motivation to make healthy choices.
All food and beverage choices are part of an individual’s eating pattern. Professionals can work with individuals in a variety of settings to adapt their choices to develop a healthy eating pattern tailored to accommodate physical health, cultural, ethnic, traditional, and personal preferences, as well as personal food budgets and other issues of accessibility. Eating patterns tailored to the individual are more likely to be motivating, accepted, and maintained over time, thereby having the potential to lead to meaningful shifts in dietary intake, and consequently, improved health.
Opportunities To Align Food Products & Menus With the Dietary Guidelines

During the past few decades, food products and menus have notably evolved in response to consumer demands and public health concerns. The food and beverage and food service sectors and settings have a unique opportunity to continue to evolve and better align with the Dietary Guidelines. Reformulation and menu and retail modification opportunities that align with the Dietary Guidelines include offering more vegetables, fruits, whole grains, low-fat and fat-free dairy, and a greater variety of protein foods that are nutrient dense, while also reducing sodium and added sugars, reducing saturated fats and replacing them with unsaturated fats, and reducing added refined starches. Portion sizes also can be adapted to help individuals make choices that align with the Dietary Guidelines. Food manufacturers are encouraged to consider the entire composition of the food, and not just individual nutrients or ingredients when developing or reformulating products. Similarly, when developing or modifying menus or retail settings, establishments can consider the range of offerings both within and across food groups and other dietary components to determine whether the healthy options offered reflect the proportions in healthy eating patterns. In taking these actions, care should be taken to assess any potential unintended consequences so that as changes are made to better align with the Dietary Guidelines, undesirable changes are not introduced.
Meeting People Where They Are: Contextual Factors & Healthy Eating Patterns
As previously described, the Social-Ecological Model provides a framework for how individuals make food and physical activity choices (where, what, when, why, and how much) each day. Understanding individual choices and motivators and the context that affects them can help professionals identify which strategies are most likely to be effective to promote healthy choices aligned with the Dietary Guidelines.
The scientific literature has described a number of specific circumstances that can limit an individual’s or family’s capacity to choose a healthy diet. These contextual factors—food access, household food insecurity, and acculturation—are particularly important for millions of individuals living in the United States. As appropriate, professionals can consider these critical factors when developing strategies and providing education to enhance interventions.
Food Access
Having access to healthy, safe,[2] and affordable food choices is crucial for an individual to achieve a healthy eating pattern. Food access is influenced by diverse factors, including proximity to food retail outlets (e.g., distance to a store or the number of stores in an area), individual resources (e.g., income or personal transportation), and neighborhood-level resources (e.g., average income of the neighborhood and availability of public transportation). Race/ethnicity, socioeconomic status, geographic location, and the presence of a disability also may affect an individual’s ability to access foods to support healthy eating patterns.
Innovative approaches are emerging to improve food access within communities. These include creating financing programs to incentivize grocery store development; increasing the availability of foods to support healthy eating patterns in retail outlets, including corner stores, bodegas, farmers markets, mobile markets, shelters, food banks, and community gardens/cooperatives; and creating new pathways for wholesale distribution through food hubs.
Food access is important in all settings where people make choices. Improving food access in settings, such as schools, worksites, early care and education programs, and food retail, may include changing organizational policies to improve the availability and provision of healthy food choices, developing or updating nutrition standards for food service operations, and educating customers about how to identify healthy choices, such as through point-of-purchase information. Changes to food options within a setting should not be done in isolation but with consideration of the overall mix of foods provided (e.g., in cafeterias, at meetings, in vending machines, concession stands and elsewhere).
To help everyone make choices that align with the Dietary Guidelines, professionals are encouraged to identify ways to improve food access. Ultimately, individual choices will be enhanced when sectors and settings ensure the accessibility of safe, affordable, and healthy food choices.
Household Food Insecurity
In the United States, about 48 million individuals live in households that experience food insecurity, which occurs when access to nutritionally adequate and safe food is limited or uncertain. Food insecurity can be temporary or persist over time. Living with food insecurity challenges a household’s ability to obtain food and make healthy choices and can exacerbate stress and chronic disease risk. Government and nongovernment nutrition assistance programs play an essential role in providing food and educational resources to help participants make healthy food choices within their budget. Food insecurity persists in the United States, and maintaining current programs, networks, and partnerships is crucial in addressing the problem. Exploring innovative new strategies could provide opportunities to reach more individuals, families, and households experiencing food insecurity. For example, sectors can create networks and partnerships to deliver food and other resources to reach people who are in need and when community services are scarce. Individuals who are supported in this way are better able to obtain and make healthy food choices that align with the Dietary Guidelines.
Acculturation
The United States continues to evolve as a nation of individuals and families who emigrate from other countries. Individuals who come to this country may adopt the attitudes, values, customs, beliefs, and behaviors of a new culture as well as its dietary habits. Healthy eating patterns are designed to be flexible in order to accommodate traditional and cultural foods. Individuals are encouraged to retain the healthy aspects of their eating and physical activity patterns and avoid adopting behaviors that are less healthy. Professionals can help individuals or population groups by recognizing cultural diversity and developing programs and materials that are responsive and appropriate to their belief systems, lifestyles and practices, traditions, and other needs.
Multi-Component Versus Multi-Level Strategies To Influence Food & Physical Activity Choices
Evidence demonstrates that both multi-component and multi-level changes must be implemented to effectively influence public health. Multi-component changes are those that use a combination of strategies to promote behavior change. These strategies can be employed across or within different settings. For example, a multi-component obesity prevention program at an early care and education center could target classroom education around nutrition and physical activity, ensure the continued nutritional quality of meals and snacks served, make improvements to the mealtime setting, increase opportunities for active play, and initiate active outreach to parents about making positive changes at home.
Multi-level changes are those that target change at the individual level as well as additional levels, such as in community, school, and retail settings. For example, strategies to reduce sodium intake could include providing individual education on how to interpret sodium information on food labels or restaurant menus (e.g., sodium versus salt), reformulating foods and meals to reduce sodium content in retail and food service establishments, and conducting public health campaigns to promote the importance of reducing sodium intake.
Many strategies for implementing these types of multi-component and multi-level actions have shown promise to positively influence food and physical activity choices. For example, moderate evidence indicates that multi-component school-based programs can improve dietary intake and weight status of school-aged children. Fundamental to the success of such actions is tailoring programs to meet the needs of the individual, the community, and/or the organization so as to increase the chances of affecting social and cultural norms and values over time.
Strategies for Action
To shift from current eating patterns to those that align with the Dietary Guidelines, collective action across all segments of society is needed. As previously described, these actions must involve a broad range of sectors, occur across a variety of settings, and address the needs of individuals, families, and communities. These actions include identifying and addressing successful approaches for change; improving knowledge of what constitutes healthy eating and physical activity patterns; enhancing access to adequate amounts of healthy, safe, and affordable food choices; and promoting change in social and cultural norms and values to embrace, support, and maintain healthy eating and physical activity behaviors.
The following examples of strategies exemplify the concerted action needed. It is important to note that no one strategy is likely to be the primary driver to improve individual and population lifestyle choices. Evidence demonstrates that multiple changes both within and across all levels of the Social-Ecological Model are needed to increase the effectiveness of interventions.
Sectors—Examples Include:
• Foster partnerships with food producers, suppliers, and retailers to increase access to foods that align with the Dietary Guidelines.
• Promote the development and availability of food products that align with the Dietary Guidelines in food retail and food service establishments.
• Identify and support policies and/ or programs that promote healthy eating and physical activity patterns.
• Encourage participation in physical activity programs offered in various settings.
Settings—Examples Include:
• Expand access to healthy, safe, and affordable food choices that align with the Dietary Guidelines and provide opportunities for engaging in physical activity.
• Adopt organizational changes and practices, including those that increase the availability, accessibility, and consumption of foods that align with the Dietary Guidelines.
• Provide nutrition assistance programs that support education and promotional activities tailored to the needs of the community.
• Implement educational programs tailored to individuals and change organization practices, approaches, and/or policies to support healthy food choices where food decisions are being made, including at early care and education programs, schools, worksites, and other community settings.
• Encourage opportunities in the workplace for regular physical activity through active commuting, activity breaks, and walking meetings.
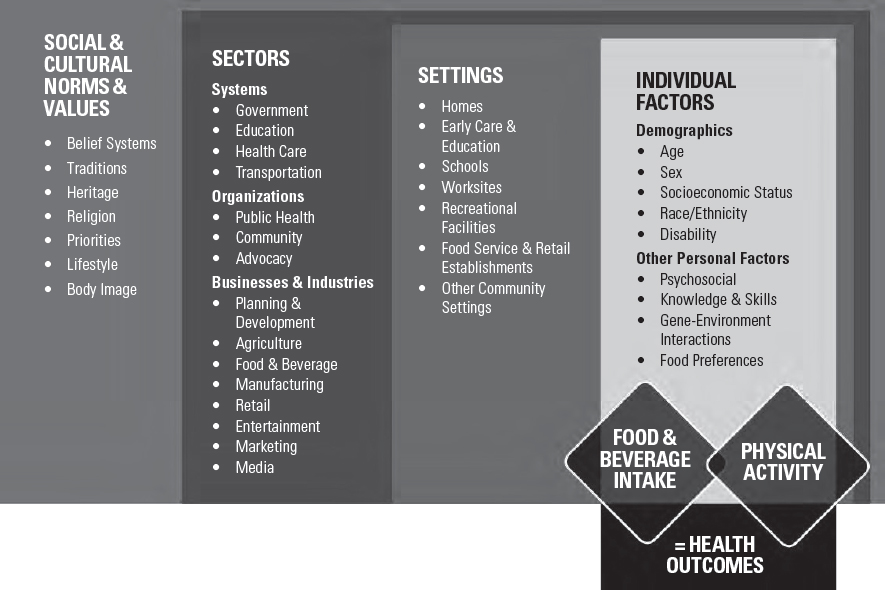
Using MyPlate as a Guide To Support Healthy Eating Patterns
The Dietary Guidelines is developed and written for a professional audience. Therefore, its translation into actionable consumer messages and resources is crucial to help individuals, families, and communities achieve healthy eating patterns. MyPlate is one such example (Figure 3-2). MyPlate is used by professionals across multiple sectors to help individuals become more aware of and educated about making healthy food and beverage choices over time. Created to be used in various settings and to be adaptable to the needs of specific population groups, the MyPlate symbol and its supporting consumer resources at ChooseMyPlate.gov bring together the key elements of healthy eating patterns, translating the Dietary Guidelines into key consumer messages that are used in educational materials and tools for the public.
Figure 3-2.
Implementation of the Dietary Guidelines Through MyPlate
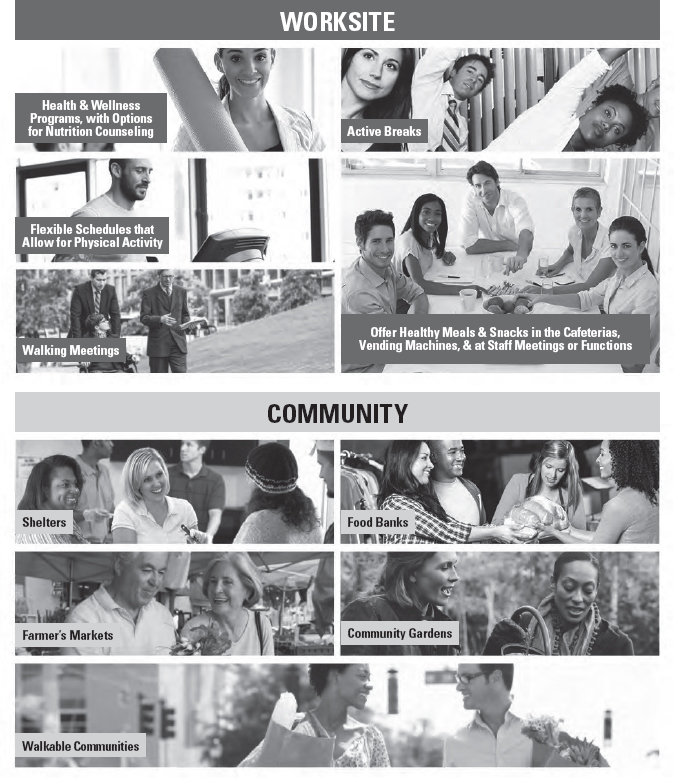
Figure 3-3.
Strategies To Align Settings With the 2015-2020 Dietary Guidelines
Americans make food and beverage choices in a variety of settings at home, at work, and at play. Aligning these settings with the 2015-2020 Dietary Guidelines will not only influence individual choices—it can also have broader population level impact when multiple sectors commit to make changes together.


Professionals Working With Individuals—Examples Include:
• Help individuals become more aware of the foods and beverages that make up their own or their family’s eating patterns and identify areas, such as modifying recipes and/or food selections, where they can make shifts to align with the Dietary Guidelines.
• Teach skills like gardening, cooking, meal planning, and label reading that help support healthy eating patterns.
• Suggest ways that individuals can model healthy eating behaviors for friends and family members.
• Develop plans to help individuals limit screen time and time spent being sedentary and increase physical activity to meet the Physical Activity Guidelines for Americans.
This is not an all-inclusive list; many strategies are available that can result in shifts to improve dietary intake and, ultimately, improve health. Professionals should help individuals understand that they can adapt their choices to create healthy eating patterns that encompass all foods and beverages, meet food group and nutrient needs, and stay within calorie limits.

Summary
Concerted efforts among professionals within communities, businesses and industries, organizations, governments, and other segments of society are needed to support individuals and families in making lifestyle choices that align with the Dietary Guidelines. Professionals have an important role in leading disease-prevention efforts within their organizations and communities to make healthy eating and regular physical activity an organizational and societal norm. Changes at multiple levels of the Social-Ecological Model are needed, and these changes, in combination and over time, can have a meaningful impact on the health of current and future generations.
[1] If not specified explicitly, references to “foods” refer to “foods and beverages.”
[2] See Appendix 14. Food Safety Principles and Guidance for guidance on food safety principles and practices.