28
Lipid Disorders
Michael J. Blaha, MD, MPH
The “Lipid Hypothesis” of cardiovascular disease (CVD)—stating that cholesterol is causal in the development of atherosclerotic cardiovascular disease (ASCVD) and that lowering of cholesterol is associated with lower cardiovascular event rates—is generally accepted throughout the medical community. For patients with known CVD (secondary prevention), studies have shown that cholesterol lowering leads to a consistent reduction in total mortality and in recurrent cardiovascular events in men and women; other studies have documented lowered mortality and events in middle-aged and older patients. Among patients without CVD (primary prevention), the data are generally consistent, with rates of cardiovascular events, heart disease mortality, and all-cause mortality differing among studies. Treatment guidelines have been designed to assist clinicians in selecting patients for cholesterol-lowering therapy based predominantly on their overall risk of developing CVD as well as their baseline cholesterol levels.
There are several genetic disorders that provide insight into the pathogenesis of lipid-related diseases. Familial hypercholesterolemia, rare in the homozygous state (about one per million), causes markedly high low-density lipoprotein (LDL) levels and early CVD. The most common genetic defects involve absent or defective LDL receptors, resulting in unregulated LDL metabolism, genetic mutations of apolipoprotein B, or gain of function in proprotein convertase subtilisin/kexin type 9 (PCSK9), a protein that regulates breakdown of LDL receptors. Patients with two abnormal genes (homozygotes) have extremely high levels—up to eight times normal—and present with atherosclerotic disease in childhood. Patients with two abnormal genes (homozygotes) may require liver transplantation or plasmapheresis to correct their severe lipid abnormalities; early treatment with statins appears to confer lifetime benefits in such patients. Those with one defective gene (heterozygotes) have LDL concentrations up to two or three times normal; persons with this condition may develop CVD in their 30s or 40s.
Another rare condition is caused by an abnormality of lipoprotein lipase, the enzyme that enables peripheral tissues to take up triglyceride from chylomicrons and very-low-density lipoprotein (VLDL) particles. Patients with this condition, one cause of familial chylomicronemia syndrome, have marked hypertriglyceridemia with recurrent pancreatitis and hepatosplenomegaly in childhood.
Numerous other genetic abnormalities of lipid metabolism are named for the abnormality noted when serum is electrophoresed (eg, dysbetalipoproteinemia) or from combinations of lipid abnormalities in families (eg, familial combined hyperlipidemia).
 When to Refer
When to Refer
• Known genetic lipid disorders.
• Striking family history of hyperlipidemia or premature atherosclerosis.
• Extremely high serum LDL cholesterol or triglycerides, or extremely low serum high-density lipoprotein (HDL) cholesterol.
Chyzhyk V et al. Familial chylomicronemia syndrome: a rare but devastating autosomal recessive disorder characterized by refractory hypertriglyceridemia and recurrent pancreatitis. Trends Cardiovasc Med. 2020 Feb;30(2):80–5. [PMID: 31003756]
Hegele RA et al. Rare dyslipidaemias, from phenotype to genotype to management: a European Atherosclerosis Society task force consensus statement. Lancet Diabetes Endocrinol. 2020 Jan;8(1):50–67. [PMID: 31582260]
Khera AV et al. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J Am Coll Cardiol. 2016 Jun 7;67(22):2578–89. [PMID: 27050191]
Sniderman AD et al. Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol. 2019 Oct 23. [Epub ahead of print] [PMID: 31642874]
LIPID FRACTIONS & THE RISK OF CORONARY HEART DISEASE
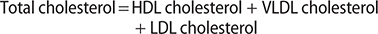
In serum, cholesterol is carried primarily on three different lipoproteins—the VLDL, LDL, and HDL molecules. Total cholesterol equals the sum of these three components:
Using these assumptions, the Friedewald equation states that LDL cholesterol can be estimated as:
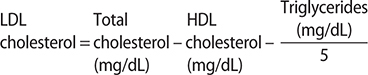
When using SI units, the formula becomes

Modern research has questioned several of the assumptions underlying the Friedewald equation, particularly the assumption that VLDL is always best estimated as triglycerides/5, which is inaccurate when triglycerides are above 150 mg/dL and when LDL cholesterol is less than 70 mg/dL. Therefore, many commercial laboratories have switched to the Martin/Hopkins equation, which uses a flexible factor for deriving VLDL from triglycerides (as opposed to always using 5). The Martin/Hopkins equation reduces the systematic underestimation of LDL cholesterol when triglycerides are greater than 150 mg/dL and LDL is less than 70 mg/dL, and is more accurate in estimating LDL from nonfasting blood specimens.
Non-HDL cholesterol is increasingly recognized as an important measure of the total quantity of apolipoprotein B–containing atherogenic lipid particles. Non-HDL cholesterol is calculated as: total cholesterol – HDL cholesterol. Advantages of non-HDL cholesterol are that it is directly measured, requires no additional cost, is less sensitive to fasting status, and is a better predictor of cardiovascular risk compared to LDL cholesterol.
Lipoprotein(a), a subfraction of LDL that is largely genetically determined, has also been recognized as a causal factor in atherosclerosis. Measuring lipoprotein(a) in patients with a strong family history, with manifestations of early ASCVD, or with familial hypercholesterolemia is useful. The National Lipid Association also recommends cascade screening in family members of those with severe hypercholesterolemia. Values greater than 50 mg/dL or greater than 100 nmol/L are considered elevated. The 2019 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guidelines recommend one-time lipoprotein(a) measurement for all adults to identify those with very high values (greater than 180 mg/dL or greater than 430 nmol/L). Novel antisense oligonucleotide therapies directed at lipoprotein(a) are currently being tested in phase 3 trials of patients with prior myocardial infarction. Currently, lipoprotein(a) is used as a risk-enhancing factor favoring early statin treatment.
It is difficult to assign a “normal” range for serum lipids. This is because our cholesterol values are vastly higher than our evolutionary ancestors (whose LDL cholesterol may have been 30–50 mg/dL) and because mean values vary across the world. Mean LDL cholesterol levels are currently declining in the United States, including in youths. There is no evidence currently available that adult cholesterol levels can be “too low”; that is, there is no evidence that very low LDL cholesterol is linked with any side effects (eg, cognitive dysfunction).
Quispe R et al. Accuracy of low-density lipoprotein cholesterol estimation at very low levels. BMC Med. 2017 Apr 20;15(1):83. [PMID: 28427464]
Sathiyakumar V et al. Fasting versus nonfasting and low-density lipoprotein cholesterol accuracy. Circulation. 2018 Jan 2;137(1):10–9. [PMID: 29038168]
Wilson DP et al. Use of lipoprotein(a) in clinical practice: a biomarker whose time has come. A scientific statement from the National Lipid Association. J Clin Lipidol. 2019 May–Jun;13(3):374–92. [PMID: 31147269]
THERAPEUTIC EFFECTS OF LOWERING CHOLESTEROL
Reducing cholesterol levels in healthy middle-aged men without coronary heart disease (CHD) (in primary prevention studies) reduces risk in direct proportion to the reduction in LDL cholesterol. Treated adults have statistically significant and clinically important reductions in the rates of myocardial infarctions, new cases of angina, need for coronary artery bypass or other revascularization procedures, peripheral artery disease, and stroke. The West of Scotland Study showed a 31% decrease in myocardial infarctions in middle-aged men treated with pravastatin compared with placebo. The Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS) study showed similar results with lovastatin. As with any primary prevention interventions, large numbers of healthy patients need to be treated to prevent a single event. The numbers of patients needed to treat (NNT) to prevent one nonfatal myocardial infarction or one coronary artery disease death in these two studies were 46 and 50, respectively. The Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) study of atorvastatin in persons with hypertension and other risk factors but without CHD demonstrated a 36% reduction in CHD events. The Justification for the Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER) study showed a 44% reduction in a combined end point of myocardial infarction, stroke, revascularization, hospitalization for unstable angina, or death from cardiovascular causes in both men and women. The NNT for 1 year to prevent one event was 169. The Heart Outcomes Prevention Evaluation (HOPE-3) trial of rosuvastatin showed a 24% reduction in cardiovascular events. The NNT over 5.6 years was 91.
Primary prevention studies have found a less consistent effect on total mortality. The West of Scotland study found a 20% decrease in total mortality, tending toward statistical significance. The AFCAPS/TexCAPS study with lovastatin showed no difference in total mortality. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT-LLT) also showed no reduction either in all-cause mortality or in CHD events when pravastatin was compared with usual care. Persons treated with atorvastatin in the ASCOT study had a 13% reduction in mortality, but the result was not statistically significant. The JUPITER trial demonstrated a statistically significant 20% reduction in death from any cause. The NNT for 1 year was 400. The HOPE-3 trial showed a 7% reduction in all-cause mortality, but the result was not statistically significant.
In secondary prevention studies among patients with established CVD, the mortality benefits of cholesterol lowering are clearer. Major trials with statins have shown significant reductions in cardiovascular events, cardiovascular deaths, and all-cause mortality in men and women with coronary artery disease. The NNT to prevent a nonfatal myocardial infarction or a coronary artery disease death in these studies was between 12 and 34. Aggressive cholesterol lowering with these agents causes regression of atherosclerotic plaques in some patients, reduces the progression of atherosclerosis in saphenous vein grafts, and can slow or reverse carotid artery atherosclerosis. Results with other classes of medications, particularly those with little effect on LDL or the LDL receptor, have been less consistent. For example, patients treated with gemfibrozil had fewer cardiovascular events, but there was no benefit in all-cause mortality when compared with placebo. The benefits and adverse effects of cholesterol lowering may be specific to each type or mechanism of drug; the clinician cannot assume that the effects of new drugs with novel mechanisms of action will generalize to other classes of medication.
The disparities in absolute event lowering between primary and secondary prevention studies highlight a critical aspect of clinical cholesterol lowering. The net benefits from cholesterol lowering depend on the underlying risk of ASCVD as well as the competing risks of other diseases. In middle-aged patients with atherosclerosis and high cholesterol, morbidity and mortality rates are high, and measures that reduce cholesterol-related risk are more likely to provide a robust net benefit to the patient. In older patients with little atherosclerosis and lower cholesterol levels, there may be no meaningful net benefit to cholesterol lowering.
Arnett DK et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019 Sep 10;74(10):1376–414. Erratum in: J Am Coll Cardiol. 2019 Sep 10;74(10):1428–9. [PMID: 30894319]
Collins R et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet. 2016 Nov 19;388(10059):2532–61. Erratum in: Lancet. 2017 Feb 11;389(10069):602. [PMID: 27616593]
Grundy SM et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. Circulation. 2019 Jun 18;139(25):e1046–81. [PMID: 30565953]
Michos ED et al. Lipid management for the prevention of atherosclerotic cardiovascular disease. N Engl J Med. 2019 Oct 17;381(16):1557–67. [PMID: 31618541]
Navarese EP et al. Association between baseline LDL-C level and total and cardiovascular mortality after LDL-C lowering: a systematic review and meta-analysis. JAMA. 2018 Apr 17;319(15):1566–79. [PMID: 29677301]
Ray KK et al. Pharmacological lipid-modification therapies for prevention of ischaemic heart disease: current and future options. Lancet. 2019 Aug 24;394(10199):697–708. [PMID: 31448741]
SECONDARY CONDITIONS THAT AFFECT LIPID METABOLISM
Several factors, including drugs, can influence serum lipids. These are important for two reasons: abnormal lipid levels (or changes in lipid levels) may be the presenting sign of some of these conditions, and correction of the underlying condition may obviate the need to treat an apparent lipid disorder. Thyroid disease, particularly hypothyroidism, is associated with a high LDL. Poorly controlled diabetes mellitus and alcohol use, in particular, are commonly associated with high triglyceride levels that decline with improvements in glycemic control or reduction in alcohol use, respectively. Thus, secondary causes of high blood lipids should be considered in each patient with a lipid disorder before lipid-lowering therapy is started. In most instances, special testing is not needed: a history and physical examination are sufficient.
CLINICAL PRESENTATIONS
Most patients with high cholesterol levels have no specific symptoms or signs. The vast majority of patients with lipid abnormalities are detected by the laboratory, either as part of the workup of a patient with CVD or as part of a preventive screening strategy. Extremely high levels of chylomicrons or VLDL particles (triglyceride level above 1000 mg/dL or 10 mmol/L) result in the formation of eruptive xanthomas (Figure 28–1) (red-yellow papules, especially on the buttocks). High LDL concentrations result in tendinous xanthomas on certain tendons (Achilles, patella, back of the hand). Such xanthomas usually indicate one of the underlying genetic hyperlipidemias. Lipemia retinalis (cream-colored blood vessels in the fundus) is seen with extremely high triglyceride levels (above 2000 mg/dL or 20 mmol/L).

Figure 28–1. Eruptive xanthomas on the arm of a man with untreated hyperlipidemia and diabetes mellitus. (Used, with permission, from Richard P. Usatine, MD, in Usatine RP, Smith MA, Mayeaux EJ Jr, Chumley H. The Color Atlas of Family Medicine, 2nd ed. McGraw-Hill, 2013.)
SCREENING & TREATMENT OF HIGH BLOOD CHOLESTEROL
While screening of all children for cholesterol disorders remains controversial, all adults should have their lipids checked before middle age. Patients with CVD and diabetes deserve the most scrutiny of their lipids since these patients are at the highest risk for suffering additional manifestations in the near term and thus have the most to gain from lipid lowering. Additional risk reduction measures for atherosclerosis are discussed in Chapter 10; lipid lowering should be just one aspect of a program to reduce the progression and effects of atherosclerosis.
The best screening and treatment strategy for adults who do not have ASCVD is less clear. Several algorithms have been developed to guide the clinician in treatment decisions, but management decisions must always be individualized based on the patient’s risk to maximize net benefit.
The 2018 American Heart Association/American College of Cardiology (AHA/ACC)/Multi-society guidelines recommend screening of all adults aged 20 years or older for high blood cholesterol. The 2016 United States Preventive Services Task Force (USPSTF) guidelines recommend beginning at age 20 years only if there are other cardiovascular risk factors such as tobacco use, diabetes, hypertension, obesity, or a family history of premature CVD. For men without other risk factors, screening is recommended beginning at age 35 years. For women and for men aged 20 to 35 without increased risk, the USPSTF makes no recommendation for or against routine screening for lipid disorders. Although there is no established interval for screening, screening can be repeated every 5 years for those with average or low risk and more often for those whose levels are close to therapeutic thresholds.
Individuals without CVD should have their 10-year risk of CVD calculated, with lifetime risk also considered. Although those with LDL cholesterol greater than 190 mg/dL (4.91 mmol/L) are recommended for treatment independent of their 10-year risk of CVD, all other patients are recommended for treatment based on their overall cardiovascular risk. While other calculators (such as SCORE or QRISK) may be more appropriate for other parts of the world, the best method for estimating 10-year risk in the United States is the Pooled Cohort Equations. First introduced in the 2013 ACC/AHA guidelines, the Pooled Cohort Equations include separate equations for white and black patients and estimate the 10-year risk of heart attack, stroke, and cardiovascular death. This represents an improvement over older Framingham 10-year calculator, which includes CHD but not stroke risk. The ACC/AHA risk estimator can be found at http://www.cvriskcalculator.com/, and mobile apps are available for download. While it has been shown to overestimate risk in some modern populations, including those with at least moderate socioeconomic status, the ACC/AHA risk estimator remains an excellent starting point for a risk discussion. Recalibrated versions of the calculator are available for countries across the world. The LIFE-CVD model is the best for illustrating lifetime risk and benefit of therapy (https://www.u-prevent.com/en-GB/HealthyCalculator/HealthyCalculator).
Shared decision making is a central part of cholesterol management in primary prevention. Therefore, the 2018 AHA/ACC/Multi-society guidelines and the 2019 ACC/AHA primary prevention guidelines identify a set of “risk-enhancing factors” that might influence a clinician and patient to favor cholesterol-lowering treatment. Table 28–1 lists these risk-enhancing factors that may be considered, particularly for patients at borderline to intermediate risk (5–20% 10-year cardiovascular risk).
Table 28–1. Risk-enhancing factors that help identify patients who may benefit most from lipid-lowering therapy: 2018 AHA/ACC/Multi-society guidelines.
Family history of premature disease (males, age < 55 years; females, age < 65 years)
Primary hypercholesterolemia (LDL cholesterol, 160–189 mg/dL [4.1–4.8 mmol/L]; non–HDL cholesterol, 190–219 mg/dL [4.9–5.6 mmol/L])
Metabolic syndrome
Chronic kidney disease (not end-stage renal disease)
Chronic inflammatory conditions, such as psoriasis, rheumatoid arthritis, or HIV/AIDS
History of preeclampsia or of premature menopause before age 40 years
High-risk race/ethnicities (eg, South Asian ancestry)
Persistently high triglycerides ≥ 175 mg/dL
Elevated high-sensitivity C-reactive protein (≥ 2.0 mg/L)
Elevated lipoprotein(a) (≥ 50 mg/dL or ≥ 125 nmol/L)
Elevated apolipoprotein B (≥ 130 mg/dL)
Ankle brachial index < 0.9
Importantly, the 2018 AHA/ACC/Multi-society guidelines and the 2019 ACC/AHA primary prevention guidelines also identify the coronary artery calcium score as the single best test for additional risk stratification. The coronary calcium score is a simple noncontrast cardiac-gated CT scan that takes about 10–15 minutes to do, is associated with approximately 1 mSv of radiation, and costs between $75 and $300. As opposed to the risk-enhancing factors, which may incline a clinician and patient toward treatment, the coronary artery calcium score may also help identify patients who are unlikely to benefit from cholesterol-lowering therapy. For example, when the coronary artery calcium score is zero in the absence of smoking or diabetes, the patient is low risk and less likely to receive net benefit from therapy; instead, the calcium artery calcium score can be repeated in approximately 5 years. The USPSTF does not endorse calcium scoring as a broad screening test; rather the test should be reserved for situations in which additional data will inform shared decision making and potentially change a therapeutic decision.
Statins are nearly always the first-line therapy. Treatment decisions are based on the presence of clinical CVD or diabetes, LDL cholesterol greater than 190 mg/dL (4.91 mmol/L), patient age, and the estimated 10-year risk of developing CVD. The 2018 AHA/ACC/Multi-society guidelines define four groups of patients who benefit from statin medications: (1) individuals with clinical ASCVD; (2) individuals with primary elevation of LDL cholesterol greater than 190 mg/dL (4.91 mmol/L); (3) individuals aged 40–75 with diabetes and LDL greater than or equal to 70 mg/dL (1.81 mmol/L); and (4) individuals aged 40–75 without clinical ASCVD or diabetes, with LDL 70–189 mg/dL (1.81–4.91 mmol/L), and estimated 10-year CVD risk of 7.5% or higher.
Ezetimibe and PCSK9 inhibitors have the strongest recommendations as second-line therapy for patients with (1) CVD whose LDL on statin therapy remains above the 70 mg/dL treatment threshold or (2) possible familial hypercholesterolemia with baseline LDL greater than 190 mg/dL (4.91 mmol/L) whose LDL remains above the 100 mg/dL treatment threshold. In high-risk patients, ezetimibe therapy is favored in part due to reduced cost, while in very high-risk patients, PCSK9 inhibitor therapy should be considered.
 Screening & Treatment in Women
Screening & Treatment in Women
The foregoing screening and treatment guidelines are designed for both men and women. Meta-analysis of studies including women with known heart disease has found that statins prevent recurrent myocardial infarctions in women. Although most experts recommend application of the same primary prevention guidelines for women as for men, clinicians should be aware of the uncertainty in this area. Estimating the 10-year cardiovascular risk is particularly important in women since a larger percentage of women than men will have estimated 10-year cardiovascular risks below 7.5% per year and thus be advised not to take statins unless their LDL is very high (greater than 190 mg/dL [4.91 mmol/L]).
 Screening & Treatment in Older Patients
Screening & Treatment in Older Patients
Meta-analysis of evidence relating cholesterol to CVD in older adults suggests that cholesterol is a weak risk factor for CVD for persons over age 75 years. Clinical trials have rarely included such individuals. One exception is the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER). In this study, elderly patients with CVD (secondary prevention) benefited from statin therapy, whereas those without CVD (primary prevention) did not. The 2018 AHA/ACC/Multi-society guidelines suggest continuing statin treatment in patients over age 75 who have CVD. The guidelines, however, suggest selectively treating patients over the age of 75 who do not have evidence of CVD. Individual patient decisions to discontinue statin therapy should be based on overall functional status and life expectancy, comorbidities, and patient preference and should be made in context with overall therapeutic goals and end-of-life decisions.
Arnett DK et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019 Sep 10;74(10):1376–414. Erratum in: J Am Coll Cardiol. 2019 Sep 10;74(10):1428–9. [PMID: 30894319]
Cardoso R et al. Selective use of coronary artery calcium testing for shared decision making: guideline endorsed and ready for prime time. Ann Intern Med. 2019 Feb 19;170(4):262–3. [PMID: 30743262]
Dixon DL et al. Recent updates on the use of PCSK9 inhibitors in patients with atherosclerotic cardiovascular disease. Curr Atheroscler Rep. 2019 Mar 16;21(5):16. [PMID: 30877491]
Greenland P et al. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol. 2018 Jul 24;72(4):434–47. [PMID: 30025580]
Grundy SM et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. Circulation. 2019 Jun 18;139(25):e1046–81. [PMID: 30565953]
Jaspers NEM et al. Prediction of individualized lifetime benefit from cholesterol lowering, blood pressure lowering, antithrombotic therapy, and smoking cessation in apparently healthy people. Eur Heart J. 2020 Mar 14;41(11):1190–9. [PMID: 31102402]
Mach F et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020 Jan 1;41(1):111–88. [PMID: 31504418]
Michos ED et al. Lipid management for the prevention of atherosclerotic cardiovascular disease. N Engl J Med. 2019 Oct 17;381(16):1557–67. [PMID: 31618541]
Miedema MD et al. Statin eligibility, coronary artery calcium, and subsequent cardiovascular events according to the 2016 United States Preventive Services Task Force (USPSTF) statin guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Heart Assoc. 2018 Jun 13;7(12):e008920. [PMID: 29899017]
TREATMENT OF HIGH LDL CHOLESTEROL
Reduction of LDL cholesterol with statins is just one part of a program to reduce the risk of CVD. Other measures—including diet, exercise, smoking cessation, hypertension control, diabetes control, and antithrombotic therapy—are also of central importance. For example, exercise (and weight loss) may reduce the LDL cholesterol and increase the HDL.
The use of medications to raise the HDL cholesterol has not been demonstrated to provide additional benefit. For example, cholesteryl ester transfer protein inhibitors are a class of medicines being investigated to raise HDL levels; however, agents in this class have not been shown to be effective in so doing. The addition of niacin to statins has also been carefully studied in the AIM-HIGH study and the HPS2-THRIVE study in patients at high risk for CVD and shown not to produce any further benefit (ie, to decrease parameters of cardiovascular risk).
Zeman M et al. Niacin in the treatment of hyperlipidemias in light of new clinical trials: has niacin lost its place? Med Sci Monit. 2015 Jul 25;21:2156–62. [PMID: 26210594]
 Diet Therapy
Diet Therapy
Studies of nonhospitalized adults have reported only modest cholesterol-lowering benefits of individual dietary therapies, typically in the range of a 5–10% decrease in LDL cholesterol, and even less over the long term. The effect of diet therapies, however, may be additive; some patients will have striking reductions in LDL cholesterol—up to a 25–30% decrease—whereas others will have clinically important increases. Thus, the results of diet therapy should be assessed about 4 weeks after initiation.
Several nutritional approaches to diet therapy are available. Most Americans currently eat over 35% of calories as fat, of which 15% is saturated fat. A traditional cholesterol-lowering diet recommends reducing total fat to 25–30% and saturated fat to less than 7% of calories, with complete elimination of trans fats. These diets replace fat, particularly saturated fat, with carbohydrate. Other diet plans, including the Dean Ornish Diet and most vegetarian diets, restrict fat even further. Low-fat, high-carbohydrate diets may, however, result in insulin resistance and reductions in HDL cholesterol.
An alternative strategy is the Mediterranean diet, which maintains total fat at approximately 35–40% of total calories but replaces saturated fat with monounsaturated fat such as that found in canola oil and in olives, peanuts, avocados, and their oils. This diet is equally effective at lowering LDL cholesterol, and is less likely to lead to reductions in HDL cholesterol. Several studies have suggested that this diet may also be associated with reductions in endothelial dysfunction, insulin resistance, and markers of vascular inflammation and may result in better resolution of the metabolic syndrome than traditional cholesterol-lowering diets. A clinical trial demonstrated reduced cardiovascular events in persons on a Mediterranean diet supplemented with additional nuts or extra-virgin olive oil compared to persons on a less intensive standard Mediterranean diet.
Other dietary changes may also result in beneficial changes in blood lipids. Soluble fiber, such as that found in oat bran or psyllium, may reduce LDL cholesterol by 5–10%. Plant stanols and sterols can reduce LDL cholesterol by 10%. Intake of garlic, soy protein, vitamin C, and pecans may also yield modest reductions of LDL cholesterol. Because oxidation of LDL cholesterol is a potential initiating event in atherogenesis, diets rich in antioxidants, found primarily in fruits and vegetables, may be helpful (see Chapter 29). Studies have suggested that when all of these elements are combined into a single dietary prescription, the impact of diet on LDL cholesterol may approach that of statin medications, lowering LDL cholesterol by close to 30%.
Abdelhamid AS et al. Polyunsaturated fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2018 Jul 18;7:CD012345. [PMID: 30019767]
Arnett DK et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019 Sep 10;74(10):1376–414. Erratum in: J Am Coll Cardiol. 2019 Sep 10;74(10):1428–9. [PMID: 30894319]
Astrup A et al. WHO draft guidelines on dietary saturated and trans fatty acids: time for a new approach? BMJ. 2019 Jul 3;366:l4137. [PMID: 31270106]
Grundy SM et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. Circulation. 2019 Jun 18;139(25):e1046–81. [PMID: 30565953]
Khera AV et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med. 2016 Dec 15;375(24):2349–58. [PMID: 27959714]
Pallazola VA et al. A clinician’s guide to healthy eating for cardiovascular disease prevention. Mayo Clin Proc Innov Qual Outcomes. 2019 Aug 1;3(3):251–67. [PMID: 31485563]
Sotos-Prieto M et al. Association of changes in diet quality with total and cause-specific mortality. N Engl J Med. 2017 Jul 13;377(2):143–53. [PMID: 28700845]
 Pharmacologic Therapy
Pharmacologic Therapy
There are seven classes of medications currently available for consideration in patients who require drug treatment of an elevated cholesterol (statins, ezetimibe, PCSK9 inhibitors, omega-3 fatty acids, bile-acid–binding resins, fibrates, and niacin). As discussed above, statins are the cornerstone of nearly all medical regimens, and current guidelines define four groups of patients who benefit from statin medications (adults with diabetes mellitus, those with existing ASCVD, LDL cholesterol greater than 190 mg/dL, or 10-year risk of ASCVD greater than 7.5%). For LDL cholesterol, the evidence is strongest for ezetimibe and PCSK9 inhibitors; for triglycerides, the evidence is strongest for adding prescription-grade omega-3 fatty acid preparations. There is less evidence for cholesterol absorption inhibitors, fibrates, and niacin. Bempedoic acid, an inhibitor of adenosine triphosphate citrate lyase (ACL)—the enzyme two steps upstream from HMG-CoA reductase, the target of statins—was approved by the FDA in 2020 and represents a new option for LDL lowering (~17%) in patients with statin intolerance.
A. Statins (Hydroxymethylglutaryl-Coenzyme A [HMG-CoA] Reductase Inhibitors)
The statins (HMG-CoA reductase inhibitors) work by inhibiting the rate-limiting enzyme in the formation of cholesterol. Cholesterol synthesis in the liver is reduced, with a compensatory increase in hepatic LDL receptors (so that the liver can take more of the cholesterol that it needs from the blood) and a reduction in the circulating LDL cholesterol level by 50% or more at the highest doses. There are also modest increases in HDL levels, substantial decreases in triglyceride levels, and marked reductions in high-sensitivity C-reactive protein levels.
The 2018 AHA/ACC/Multi-society guidelines divide statins into two categories: “high-intensity” and “moderate-intensity” statins (Table 28–2). High-intensity statins lower LDL cholesterol by approximately 50%. Examples include high-dose atorvastatin 40–80 mg/day and rosuvastatin 20–40 mg/day (Table 28–3). Moderate-intensity statins lower LDL cholesterol by approximately 30–50%. Examples include simvastatin 20–40 mg/day, pravastatin 40–80 mg/day, and lovastatin 40 mg/day, as well as low-dose atorvastatin 10–20 mg/day and rosuvastatin 5–10 mg/day. All statins are given once daily in the morning or evening.
Table 28–2. Indications for high-intensity and moderate-intensity statins: recommendations of the 2018 AHA/ACC/Multi-society guidelines.

Table 28–3. Effects of selected lipid-modifying drugs (listed alphabetically).

Statin-associated muscle aches, with normal serum creatine kinase levels, occur in up to 10% of patients, and often such patients can tolerate the statin upon rechallenge. The Statin-Associated Muscle Symptom Clinical Index (SAMS-CI) is a useful tool to help differentiate statin-related symptoms from symptoms unrelated to statins. More serious, but very uncommon, muscle disease includes myositis and rhabdomyolysis, with moderate and marked elevations of serum creatine kinase levels, respectively. Such muscle disease occurs more often when the statin is taken with niacin or a fibrate, as well as with erythromycin, antifungal medications, nefazodone, or cyclosporine. Simvastatin at the highest approved dose (80 mg) is associated with an elevated risk of muscle injury or myopathy; this dose should be used only in patients who have been taking simvastatin at a lower dose for longer than 1 year without muscle toxicity. Liver disease, with elevations of serum transaminases, is another uncommon side effect of statin therapy and is again more common in patients who are also taking fibrates or niacin. Manufacturers of statins recommend monitoring liver enzymes before initiating therapy and as clinically indicated thereafter; current guidelines do not recommend routine monitoring. Liver failure can occur but is extremely uncommon. Finally, statin therapy is associated with a 10% increase in risk of developing diabetes mellitus in at-risk individuals (eg, those with the metabolic syndrome).
B. Ezetimibe
Ezetimibe inhibits the intestinal absorption of dietary and biliary cholesterol across the intestinal wall by inhibiting a cholesterol transporter. The dose of ezetimibe is 10 mg/day orally. Ezetimibe reduces LDL cholesterol between 15% and 20% when used as monotherapy, reduces high-sensitivity C-reactive protein, and can further reduce LDL in patients taking statins in whom the therapeutic goal has not been reached. While beneficial effects of ezetimibe monotherapy on cardiovascular outcomes are available from only a large open-label trial, the double-blind IMPROVE-IT trial showed that adding ezetimibe to a statin resulted in a small incremental 5–10% relative risk reduction in detrimental cardiovascular outcomes. At the end of 7 years of study, patients taking ezetimibe-simvastatin had a 2% absolute reduction in cardiovascular events compared to patients taking simvastatin alone. Current guidelines recommend adding ezetimibe therapy to maximally tolerated statin therapy in patients at high risk for CVD whose LDL cholesterol remains above the treatment threshold of 70 mg/dL.
C. Proprotein Convertase Subtilisin/Kexin Type 9 (PCSK9) Inhibitors
PCSK9 inhibitors are fully human monoclonal antibodies that inhibit PCSK9-mediated LDL-receptor degradation and lower LDL cholesterol levels by 50–60% and lipoprotein(a) by up to 20–30%. Two agents, alirocumab and evolocumab, are approved for use in the United States for patients with familial hypercholesterolemia or CVD who require additional lowering of LDL cholesterol. The medications are injected subcutaneously every 2–4 weeks. No significant increase in adverse events has been observed compared to placebo. The FOURIER (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) trial compared evolocumab with placebo in 27,564 patients with established atherosclerotic disease already taking statin therapy; participants were monitored for a median of 2.2 years. LDL cholesterol was reduced by 59%. Patients receiving the evolocumab plus statin had a 15% reduction in the primary composite endpoint of cardiovascular death, myocardial infarction, stroke, hospital admission for unstable angina, or coronary revascularization and a 20% reduction in the secondary outcome of cardiovascular death, myocardial infarction, or stroke. The ODYSSEY-OUTCOMES study randomized 18,924 patients with recent acute coronary syndrome to alirocumab or placebo, demonstrating a 15% reduction in the primary composite cardiovascular endpoint and a 15% reduction in all-cause mortality in secondary statistical testing after median 2.8-year follow-up.
However, despite encouraging results from multiple clinical trials, initial cost-effectiveness models suggested that PCSK9 inhibitors were not cost-effective. After marked price reductions in 2018 and 2019, PCSK9 inhibitors are closer to being cost-effective; however, guidelines suggest that their relatively high cost must still remain part of the consideration regarding their use. Current guidelines recommend addition of PCSK9 inhibitors to statins at maximally tolerated doses in patients at very high risk for CVD when on-treatment LDL cholesterol remains above 70 mg/dL (or above 100 mg/dL in patients with familial hypercholesterolemia). Patients considered to be at very high-risk for CVD include those with recent acute coronary syndrome within 12 months; multiple prior myocardial infarctions or strokes; significant unrevascularized coronary artery disease; and polyvascular disease (coronary plus cerebrovascular or peripheral vascular disease).
In late 2020, the FDA will consider approval of a novel PCSK9 inhibitor called inclisiran that uses silencing RNA technology to reduce PCSK9 protein production by the liver, enabling dosing every 6 months.
D. Omega-3 Fatty Acid Preparations
Omega-3 fatty acids are essential fatty acids that must be consumed in the diet and are a prominent feature of Mediterranean-style diets. In pharmacologic doses, omega-3 fatty acid preparations can lower triglycerides by up to 30%, with modest reductions in apolipoprotein-B–containing lipoproteins and high-sensitivity C-reactive protein. Pharmacologic therapy should be differentiated from dietary omega-3 fatty acid supplements. The former is an FDA-approved product usually given at a much higher dose; dietary supplements are variable, the supporting evidence is much weaker, and they are not currently regulated.
There is modest evidence from meta-analyses that omega-3 fatty acid supplementation reduces myocardial infarctions, though with no reduction in total or cardiovascular mortality. Omega-3 ethyl esters have not been associated with cardiovascular event reduction when added to statin therapy.
In contrast, icosapent ethyl, which is a highly purified eicosapentaenoic acid (EPA) only preparation, was shown to reduce cardiovascular deaths, nonfatal myocardial infarctions, nonfatal strokes, coronary revascularizations, and unstable angina by 25% in statin-treated patients with triglycerides greater than 135 mg/dL in the 8179 person REDUCE-IT randomized clinical trial compared to a mineral oil placebo. The mechanism of action of icosapent ethyl is not yet clear but likely involves multiple mechanisms beyond lipid lowering, including antiplatelet activity, anti-inflammatory activity, and arrhythmia prevention. In 2019, the FDA granted icosapent ethyl a broad indication for CVD event lowering in patients with triglycerides over 150 mg/dL and either established CVD or diabetes mellitus plus two or more additional risk factors for CVD.
E. Bile Acid–Binding Resins
The bile acid–binding resins include cholestyramine, colesevelam, and colestipol. In the pre-statin era, treatment with these agents reduced the incidence of coronary events in middle-aged men by about 20%, with no significant effect on total mortality. The resins work by binding bile acids in the intestine. The resultant reduction in the enterohepatic circulation causes the liver to increase its production of bile acids, using hepatic cholesterol. Thus, hepatic LDL receptor activity increases, with a decline in plasma LDL levels. The triglyceride level tends to increase in some patients treated with bile acid–binding resins; these resins should be used with caution in patients with elevated triglycerides and not at all in patients who have triglyceride levels above 500 mg/dL. The clinician can anticipate a reduction of 15–25% in the LDL cholesterol level, with insignificant effects on the HDL level.
These agents often cause gastrointestinal symptoms, such as constipation and gas. They may interfere with the absorption of fat-soluble vitamins (thereby complicating the management of patients receiving warfarin) and may bind other drugs in the intestine. Concurrent use of psyllium may ameliorate the gastrointestinal side effects.
F. Fibric Acid Derivatives
The fibrates are peroxisome proliferative-activated receptor-alpha (PPAR-alpha) agonists that result in significant reductions of plasma triglycerides and increases in HDL cholesterol. They reduce LDL levels by about 10–15% (although the result is variable) and triglyceride levels by about 40% and raise HDL levels by about 15–20%. The fibric acid derivatives or fibrates approved for use in the United States are gemfibrozil and fenofibrate. Ciprofibrate and bezafibrate are also available for use internationally.
Gemfibrozil monotherapy reduced CHD rates in hypercholesterolemic middle-aged men free of coronary disease in the Helsinki Heart Study. The effect was observed only among those who also had lower HDL cholesterol levels and high triglyceride levels. In a Veteran Affairs study, gemfibrozil monotherapy was also shown to reduce cardiovascular events in men with existing CHD whose primary lipid abnormality was a low HDL cholesterol. There was no effect on all-cause mortality.
However, fibrates have not been shown to reduce cardiovascular events in all statin-treated patients with CVD or diabetes. For example, in the ACCORD study, addition of fenofibrate to statin in patients with diabetes and mild triglyceride elevations resulted in no benefit.
The usual dose of gemfibrozil is 600 mg once or twice a day. Side effects include cholelithiasis, hepatitis, and myositis. The incidence of the latter two conditions may be higher among patients also taking other lipid-lowering agents. Fenofibrate, 48–145 mg daily, can be used and has slightly fewer side effects than gemfibrozil. Resins are the only lipid-modifying medication considered safe in pregnancy.
G. Niacin (Nicotinic Acid)
Niacin reduces the production of VLDL particles, with secondary reduction in LDL and increases in HDL cholesterol levels. The average effect of full-dose niacin therapy is a 15–25% reduction in LDL cholesterol and a 25–35% increase in HDL cholesterol.
There is very little evidence to support the use of niacin in the modern era. In two large pivotal clinical trials, AIM-HIGH and HPS2-THRIVE, extended-release niacin did not reduce cardiovascular events when added to statin therapy in high-risk patients. Therefore, niacin should be rarely used.
 Treatment Algorithms
Treatment Algorithms
For patients who require a lipid-modifying medication, an HMG-CoA reductase inhibitor (statin) is recommended. In patients with CVD, this should be at its maximally tolerated dose.
Combination therapy is indicated for (1) patients with familial hypercholesterolemia with on-treatment LDL cholesterol that is above 100 mg/dL; (2) patients with existing CVD with on-treatment LDL cholesterol that remains above 70 mg/dL; (3) many high-risk patients with triglycerides greater than 150 mg/dL or non-HDL cholesterol greater than 100 mg/dL.
Patients with heterozygous familial hypercholesterolemia or premature CVD may need two or more medications to get below the treatment threshold, while those without CVD (primary prevention) less commonly need multiple medications. The 2018 AHA/ACC/Multi-society guidelines recommend addition of ezetimibe in high-risk patients, while reserving PCSK9 inhibitor therapy for very high-risk patients or those taking maximally tolerated statin therapy and ezetimibe with LDL cholesterol still not below 70 mg/dL (Figure 28–2). Notably, the 2019 European Society of Cardiology guidelines have endorsed an LDL cholesterol treatment goal of less than 55 mg/dL in very high risk patients. Other guidelines, including the American Diabetes Association and the National Lipid Association, have endorsed the use of icosapent ethyl in high-risk patients with CVD or diabetes and on-treatment triglycerides greater than 150 mg/dL.

Figure 28–2. Clinical treatment algorithm for patients with atherosclerotic cardiovascular disease (ASCVD). (Used, with permission, from Grundy SM et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. Circulation. 2019 Jun 18;139(25):e1046–81. © 2018 American Heart Association, Inc.)
Patients with homozygous familial hypercholesterolemia may need plasmapheresis and/or special lipid-lowering therapies uniquely approved for this population (Table 28–3).
Bhatt DL et al; REDUCE-IT Investigators. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019 Jan 3;380(1):11–22. [PMID: 30415628]
Grundy SM et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. Circulation. 2019 Jun 18;139(25):e1046–81. [PMID: 30565953]
Karmali KN et al. Drugs for primary prevention of atherosclerotic cardiovascular disease: an overview of systematic reviews. JAMA Cardiol. 2016 Jun 1;1(3):341–9. [PMID: 27438118]
Mach F et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020 Jan 1;41(1):111–88. [PMID: 31504418]
Mark DB et al. PCSK9 inhibitors and the choice between innovation, efficiency, and affordability. JAMA. 2017 Aug 22;318(8):711–2. [PMID: 28829851]
Orringer CE et al. National Lipid Association Scientific Statement on the use of icosapent ethyl in statin-treated patients with elevated triglycerides and high or very-high ASCVD risk. J Clin Lipidol. 2019 Nov–Dec;13(6):860–72. [PMID: 31787586]
Rosenson RS et al. Optimizing cholesterol treatment in patients with muscle complaints. J Am Coll Cardiol. 2017 Sep 5;70(10):1290–301. [PMID: 28859793]
Rosenson RS et al. The Statin-Associated Muscle Symptom Clinical Index (SAMS-CI): revision for clinical use, content validation, and inter-rater reliability. Cardiovasc Drugs Ther. 2017 Apr;31(2):179–86. [PMID: 28421332]
Sabatine MS et al. Clinical benefit of evolocumab by severity and extent of coronary artery disease. Circulation. 2018 Aug 21;138(8):756–66. [PMID: 29626068]
Schwartz GG et al; ODYSSEY OUTCOMES Committees and Investigators. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018 Nov 29;379(22):2097–107. [PMID: 30403574]
Wiggins BS et al. Recommendations for management of clinically significant drug-drug interactions with statins and select agents used in patients with cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2016 Nov 22;134(21):e468–95. [PMID: 27754879]
HIGH BLOOD TRIGLYCERIDES
Patients with very high levels of serum triglycerides (greater than 1000 mg/dL) are at risk for pancreatitis. The pathophysiology is not certain, since pancreatitis never develops in some patients with very high triglyceride levels. Most patients with congenital abnormalities in triglyceride metabolism present in childhood; hypertriglyceridemia-induced pancreatitis first presenting in adults is more commonly due to an acquired problem in lipid metabolism.
Although there are no clear triglyceride levels that predict pancreatitis, most clinicians treat fasting levels above 500 mg/dL (5 mmol/L). The risk of pancreatitis may be more related to the triglyceride level following consumption of a fatty meal. Because postprandial increases in triglyceride are inevitable if fat-containing foods are eaten, fasting triglyceride levels in persons prone to pancreatitis should be kept well below that level.
The primary therapy for high triglyceride levels is dietary, avoiding alcohol, simple sugars, refined starches, and saturated and trans fatty acids, and restricting total calories. Control of secondary causes of high triglyceride levels may also be helpful. In patients with fasting triglycerides greater than or equal to 500 mg/dL (5 mmol/L) despite adequate dietary compliance—and certainly in those with a previous episode of pancreatitis—therapy with a triglyceride-lowering drug (eg, statins, omega-3 preparations, or fibric acid derivatives) is indicated. Combinations of these medications may also be used.
Currently, drug treatment for patients with triglycerides greater than 150 mg/dL (1.5 mmol/L) is reserved for those with established CVD with well-controlled LDL cholesterol on maximally tolerated therapy with statins or other agents. Currently, data are strongest for icosapent ethyl.
Bhatt DL et al; REDUCE-IT Investigators. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019 Jan 3;380(1):11–22. [PMID: 30415628]
Chaudhry R et al. Pharmacological treatment options for severe hypertriglyceridemia and familial chylomicronemia syndrome. Expert Rev Clin Pharmacol. 2018 Jun;11(6):589–98. [PMID: 29842811]
Orringer CE et al. National Lipid Association Scientific Statement on the use of icosapent ethyl in statin-treated patients with elevated triglycerides and high or very-high ASCVD risk. J Clin Lipidol. 2019 Nov–Dec;13(6):860–72. [PMID: 31787586]
Rygiel K. Hypertriglyceridemia—common causes, prevention and treatment strategies. Curr Cardiol Rev. 2018 Mar 14;14(1):67–76. [PMID: 29366425]
Saeed A et al. Remnant-like particle cholesterol, low-density lipoprotein triglycerides, and incident cardiovascular disease. J Am Coll Cardiol. 2018 Jul 10;72(2):156–69. [PMID: 29976289]
Wiesner P et al. Triglycerides: a reappraisal. Trends Cardiovasc Med. 2017 Aug;27(6):428–32. [PMID: 28438398]