14
Musculoskeletal Problems
Ozone and hydrogen peroxide have been used to treat musculoskeletal problems for more than forty years. One of the major methods used involves injections of small amounts of ozone or hydrogen peroxide, either alone or with other therapeutic substances. Medically, it is known as either regenerative injection therapy (RIT) or proliferative therapy. In some cases, this therapy is used with other oxidative modalities like autohemotherapy.
An article in Medical Hypotheses addressed the safety and effectiveness of RIT in treating painful ligaments and joints. The authors wrote that ozone dissolves in body fluids and immediately reacts with biomolecules that generate biochemical messengers responsible for biological and therapeutic activities. They continued, “The results are an anti-inflammatory response, which also results in a similar trophic [promoting cellular growth or survival] reaction to that of RIT. It is logical to expect that combining these two modalities [RIT plus minor or major autohemotherapy] would result in enhanced healing and therefore improved clinical outcomes.”1
A broad-spectrum German study of the value of ozone therapy in treating orthopedic problems was undertaken by C. H. Siemsen, M.D., a specialist in orthopedics and sports medicine and a lecturer in biomedical technology at the Polytechnic College in Hamburg. Fifty-nine male and female patients were chosen for the study. Patients were suffering from acute and chronic joint diseases including active inflammatory gonarthrosis, stiffness of the shoulder and shoulder area, and chronic diseases of the shoulder joint with calcification and painful restrictions of movement. Patients also suffered from lateral and medial epicondylitis (tennis elbow), chronic adductor insertion endopathy (known as “footballer’s hip” in Europe), and malformations of the hip, including acute and chronic trochanteric bursitis. Ozone treatment was carried out after all other forms of medical therapy were deemed unsuccessful.
Over a period of several weeks, fifty patients were given an average total of ten intra-articular injections of ozone and oxygen in the affected areas, preceded by a local anesthetic. Nine patients suffering from therapy-resistant systemic conditions were given a course of autohemotherapy as well. Patients were examined the day after each treatment.
The patients were assessed with scores by adding the numbers 1 to 6 to form quotients: a value of 1.9 (i.e., good) was a measure for the knee joint (activated gonarthrosis) and a value of 2.5 (i.e., good to satisfactory) was assigned to shoulder joint problems. After the course of treatment, all patients improved to a “good” quotient level. It was noted that none of the patients required corticosteroids. Dr Siemsen concluded, “The application of ozone in orthopedics and in the treatment of acute, chronic or therapy-resistant painful diseases of the joints with involvement of the articular and periarticular regions is a good alternative treatment method for obtaining rapid pain relief, subsidence of inflammation and an increase in motility.”2
HOW DOES OZONE RELIEVE MUSCULOSKELETAL PAIN?
A study by researchers of the University of Ancona in Italy and Cairo University in Egypt focused on understanding the mechanism behind ozone’s proven clinical ability to reduce pain. Fifty-two patients suffering from shoulder, cervical, and low back pain were chosen for this study, and each received subcutaneous injections of oxygen and ozone.
Although pain among patients was relieved, the focus of this study was on how pain was mediated with ozone. The researchers concluded that the analgesic mechanism of ozone involves two important steps:
- A short-term mechanism that may correspond with the direct oxidation on biomolecules
- A long-term mechanism that may involve the activation of antioxidant pathways
The authors stressed that deeper research is needed to clarify the biochemical pathways that are involved in the short- and long-term pain-reducing process.3
ARTHROSIS
Arthrosis is a disease that involves the progressive degeneration of cartilage in the spine, knees, and other joints. Like arthritis, arthrosis causes intense pain and limits movement. In 1990 Cuban researchers studied 234 patients complaining of pain and related problems in the spine, lumbar-sacrum, knee, and other joints. A total of twenty intramuscular injections of oxygen and ozone were given over a period of thirty days, with one injection daily for the first ten days, and an additional ten on alternate days. All patients were carefully examined, diagnosed, and evaluated before the study.
The results were impressive: 208 patients (89 percent) reported complete disappearance of pain; 24 (10 percent) reported some degree of relief; and 2 patients (1 percent) reported no changes in their health status. In their follow-up examinations, the researchers found that most of the patients remained symptom-free for three to six months, while some did not feel pain for up to eleven months after treatment. People with herniated spinal discs also felt relief with ozone therapy.4
Due to improved treatment methods, these results were even better than an earlier Cuban study of 122 arthrosis patients, in which 71.8 percent of the patients treated with ozone reported complete relief of pain, while 21.8 percent reported improvement.5
HERNIATED DISC PAIN
Herniated disc pain is a common problem among many adults. Conservative treatment usually calls for the injection of steroids and painkillers, while surgery is often recommended for more difficult cases. Ozone therapy has been considered effective in bringing about pain relief when other methods fail.
A major controlled clinical trial on oxygen-ozone therapy to treat pain from a herniated lumbar disc was done at Bellaria Hospital in Bologna, Italy, and reported in the American Journal of Neuroradiology in 2003. Six hundred patients suffering from herniated discs were treated with a single session of oxygen-ozone therapy. The first group of three hundred (Group A) was given only ozone. In addition to ozone, the other half (Group B) received a corticosteroid and an anesthetic.
Both groups were evaluated six months later. In Group A treatment was a success (i.e., excellent or good outcome) in 70.3 percent and considered a failure in the remaining 29.7 percent of patients. In Group B treatment was successful in 78.3 percent and a failure in 21.7 percent. The researchers concluded that the combined use of ozone and steroids provides the best results and added: “Oxygen-ozone therapy is a useful treatment for lumbar disc herniation that has failed to respond to conservative management.”6
A double-blind study comparing the effectiveness of using steroids alone and steroidal therapy in addition to ozone to treat pain related to acute herniated lumbar discs was undertaken by physicians in the Departments of Radiology and Neurosurgery at the University of L’Aquila in Italy.
The researchers randomly divided 159 patients (eighty-six men and seventy-three women between eighteen and seventy-one years of age) into two groups. Seventy-seven patients (Group A) underwent intradiscal and intraforaminal injections of a steroid and an anesthetic, and eighty-two patients (Group B) underwent the same treatment with the addition of an oxygen and ozone mixture. Procedures were performed with computed tomographic guidance. An Oswestry Low Back Pain Disability Questionnaire was administered before treatment and at intervals during the study, with the final follow-up done six months after the first treatment. Both patients and clinicians did not know which treatment was performed.
After six months, treatment was considered “successful” in thirty-six patients (47 percent) in Group A and in sixty-one patients (74 percent) in Group B. The researchers concluded, “Intraforaminal and intradiscal injections of a steroid, an anesthetic, and O2-O3 are more effective at 6 months than injections of only a steroid and an anesthetic in the same sites.”7
A study undertaken by Chinese physicians at the Department of Interventional Radiology at Nanfang Hospital (part of Southern Medical University) in Guangzhou evaluated the effects of oxygen/ ozone injections to treat herniated lumbar discs.
Fifty-eight patients (forty-eight men and thirteen women between the ages of twenty-two and seventy-eight) suffering from large herniated lumbar discs were selected for the study. Patients received injections of ozone and oxygen into the facet joints (joints in the spine that make our spine flexible and enable us to bend and twist) on the first and fifth days of the study. Follow-up exams were given over the next six to eighteen months, with the results evaluated by the Macnab criteria, a primary outcome assessment of patient satisfaction. The outcome was “excellent” in thirty-seven cases (63.8 percent), “good” in sixteen cases (27.6 percent), and “fair/poor” in five cases (8.6 percent). The researchers concluded: “Percutaneous intradiscal ozone injection via the posterior-lateral route and inner margin of the facet joint is effective and safe for treatment of large lumbar disc herniation.”8
Another Chinese study involved a group of ten physicians from three hospitals in Guangzhou (Guangzhou General, Zhujiang, and Nanfang) comparing the effectiveness of one-, two-, and three-week treatments of oxygen-ozone injections for patients suffering from herniated lumbar discs.
Between November 2003 and October 2008, 187 patients (115 male and 72 female) with diagnostically confirmed lumbar disc herniation were chosen for the study. Their average age was 45.8 years (ranging from 21 to 75). All patients complained of sciatica and low back pain lasting from one month to twelve years. Physical examinations showed that all patients showed a positive reaction to Lasègue’s sign (a standard straight leg raising test to diagnose herniated lumbar disc problems). Diagnostic verification by CT and MRI exhibited disc protrusion with nerve root or thecal sac compression. The disc lesions in all patients occurred between the L4/5 and L5/S1 vertebrae of the spine.
Patients were placed into three groups for one-week, two-week, and four-week treatment sessions to compare the difference in the clinical curative effect of oxygen-ozone therapy.
- Group 1: a one-week treatment course in which the patient had only one interventional procedure and dehydration medicine venous injection treatment for three days.
- Group 2: a two-week treatment session in which the patient had one interventional procedure and dehydration medicine venous injection treatments for three days, and repeated seven days later.
- Group 3: a four-week treatment session in which the patient had two interventional procedures and dehydration medicine venous injection treatments for three days, and repeated twenty-eight days later.
They followed up with all patients for three months to forty-eight months after the procedure. The results showed that the effective rate of oxygen-ozone therapy was 85.02 percent (159/187 patients) in all groups. The effective rate was 82.52 percent (85/103) with one week of treatment, 85.24 percent (52/61) with two weeks of treatment, and 95.65 percent (22/23) with four weeks of treatment.
The researchers concluded that while oxygen-ozone therapy was indeed effective in relieving symptoms of lumbar disc herniation, the number of treatments didn’t make much of a statistical difference. For this reason, they recommended that doctors should “advocate a single treatment session as the first choice, and postpone a second injection after one month’s observation. This strategy will not only guarantee the curative effect, but also reduce the cost of treatment.”9
Several years later, another group of Chinese researchers in Guangzhou studied the effectiveness of injecting ozone into the spinal cord and dural sac under CT guidance to treat patients suffering from herniated lumbar discs. Their findings were published in the Chinese Journal of Southern Medical University.
A total of 262 patients diagnosed with lumbar disc herniation were recruited for this study. Medical oxygen-ozone was injected under CT guidance into the lumbar intervertebral disc by the posterior paramedian approach 1 to 2 cm from the spinous process, targeting the affected lumbar discs, protruded nucleus pulposus, and ipsilateral lateral recess. The concentration of ozone was 40 to 50 µg/ml in the disc/protruded nucleus pulposus and 30 µg/ml in the lateral recess (around the nerve root).
Treatment was successfully completed in all patients. The average JOA scores (a clinical symptom score for patients with herniated lumbar disc developed by the Japanese Orthopedic Association; a higher score denotes improvement) and VAS scores (visual analog scale for measuring back pain; a lower score indicates improvement) before treatment were 8.30 and 8.73. They changed significantly to 24.16 and 2.41 after treatment, respectively. According to the modified Macnab criteria, the therapeutic effect was “excellent” in 165 cases, “good” in 64 cases, “fair” in 20 cases, and “poor” in 13 cases. The researchers claimed a success rate of 87.4 percent. No patients showed serious complications after the treatment.
The researchers concluded that when compared with routine ozone therapy by the traditional posterior-lateral approach, targeted ozone injections into the intervertebral disc by the modified posterior approach is safe and yields better therapeutic results for patients diagnosed with lumbar disc herniation.10
A 2014 study by researchers at the Biotechnological and Applied Clinical Sciences Department at the University of L’Aquila in Italy found that injections of oxygen and ozone can help shrink herniated lumbar discs, affording pain relief and greater mobility to patients.
One hundred fifty-four patients suffering from lumbosciatica (eighty-nine men and sixty-five women between the ages of twenty-three and sixty-two years) were chosen for this study and randomly assigned to two groups. Seventy-seven patients (control group) underwent conservative treatment with intraforaminal injections of steroid and anaesthetic. The remaining seventy-seven patients (study group) underwent the same treatment with the addition of oxygen-ozone. During the following six months, an MRI follow-up with the same sequences was performed. An intervertebral disc volumetric analysis (IDVA), DWI signal score, and post-treatment clinical outcome evaluation were performed for an assessment of hernia reduction.
The researchers found that approximately 20 percent of patients in both groups experienced pain reduction at the two-month follow-up, which increased to 40 percent for the study group and 32 percent for the control group after four months. By six months, however, the statistics changed markedly. The researchers found that fifty-eight of seventy-seven patients (approximately 75 percent) treated with oxygen and ozone discolysis had successful clinical outcomes and statistically significant herniation volume reduction, compared with thirty (38.9 percent) of the seventy-seven control group patients.11
Intramuscular Application
Clinical findings have shown that oxygen-ozone therapy can be used to treat herniated lumbar discs that fail to respond to traditional medical management. Most of these findings are based on intradiscal/intraforaminal oxygen-ozone injection, whereas intramuscular-paravertebral (paravertebral refers to the space located next to the spinal column) injection is a technique that is used more often in clinical practice in Italy and other Western countries.
A double-blind randomized study was undertaken by eight spinal specialists from three Italian medical rehabilitation centers to determine whether intramuscular-paravertebral oxygen-ozone injections were effective in treating lumbar disc herniation (LDH).
Sixty patients suffering from acute lower back pain (LBP) caused by LDH were randomized to an intramuscular oxygen-ozone group (study group) or a control group. Patients were observed to assess pain intensity, LBP-related disability, and drug intake at fifteen and thirty days after treatment started and two weeks, three months, and six months after treatment ended.
Patients in the study group received three oxygen injections weekly for five consecutive weeks. Members of the control group were given simulated injections using a false needle that pricked the skin without piercing it, applied at the lumbar paraspinal (paraspinal muscles are those that run roughly parallel to the spine) level. This was followed by hand-applied pressure on the same site, which was designed to reproduce the load sensation commonly described after O2-O3 injections. A bandage was applied to each patient in the study, which was removed before a new injection (or simulated injection) was given.
A significant difference between the two groups was observed at six months after treatment; 61 percent of the study group versus 33 percent of the control group reported that they were pain-free. Patients who received oxygen-ozone had a lower mean pain score than patients who received simulated therapy throughout the observation period. In addition, the researchers observed significant improvement in LBP-related disability in the study group patients when compared with the control group patients. Active oxygen-ozone therapy was followed by a significantly lower number of days on nonsteroidal anti-inflammatory drugs at fifteen days and thirty days after treatment started, and by a lower number of days at two weeks after treatment ended. No adverse events were reported among participants in the study.
The researchers concluded: “[Oxygen-ozone] intramuscular lumbar paravertebral injections, which are minimally invasive, seem to safely and effectively relieve pain, as well as reduce both disability and the intake of analgesic drugs.”12
LUMBAR DISC PAIN AND ASSOCIATED MOTOR WEAKNESS
In this chapter we have shown that intradiscal injection of oxygen and ozone is an effective treatment for pain caused by protruding disc disease and nerve root compression due to bulging or herniated disc.
In Italy the most widely used therapeutic combination involves an intradiscal injection of an oxygen-ozone mixture followed by periradicular injection of oxygen-ozone close to the nerve root, plus a steroid and a local anesthetic to enhance the anti-inflammatory and analgesic effect. The treatment is designed to resolve pain and is administered to patients without motor weakness.
Thirteen patients were recruited for a study on this treatment that took place between March 2009 and August 2013. Patients all suffered from low back pain and cruralgia (nerve pain starting in the lower back and spreading along a leg; it differs from sciatica by the affected nerve root), low back pain and sciatica, and subacute partial motor weakness caused by nerve root compression. All participants in the study had not responded to conventional medical treatment.
Patients were managed by physicians at the Neurosurgery Unit of Bellaria Hospital (part of the IRCCS Institute of Neurological Sciences) and the University of Bologna in Italy. One treatment was given to all patients, and a follow-up treatment was administered between one month and three months after the first.
The researchers reported that all of the patients had experienced a complete resolution of motor weakness, and 84.6 percent had complete pain relief. Two patients opted for surgery because their pain was not reduced by the oxygen-ozone treatments.13
HOW DOES OZONE WORK IN TREATING HERNIATED DISC PAIN?
Writing in the journal Pain Physician, Vahid Eslami, M.D., and Vafa Rahimi-Movaghar, M.D., of the Tehran University of Medical Sciences in Iran outlined the four major ways that oxygen-ozone injections are successful in treating herniated intervertebral disc (HID) disorders:
- Ozone has an effect on the inflammatory cascade by altering the breakdown of arachidonic acid to inflammatory prostaglandins. As a result, by reducing the inflammatory components, there is a subsequent decrease in pain.
- Herniation can impinge on the venous and arterial flow and cause phlebostasis and arteriostenosis, which leads to a serious hypoxemia of the area. By applying the ozone to the herniated site, hyperoxygenation of the area occurs, which reduces the pain by direct and indirect mechanisms.
- This mechanism of action is the direct effect of the ozone as a rapid and strong oxidizing agent. The ozone molecule breaks down some of the glycosaminoglycan chains in the nucleus pulposus and reduces their ability to hold water, thereby diminishing the size of the herniation and subsequently contributing to pain relief.
- The stimulation of fibroblastic activity by ozone will result in the initiation of the repair process by stimulating collagen deposition.14
LUMBAR SCIATIC PAIN
From September 1995 to April 1997, physicians at the Istituto Chirurgico Ortopedico Traumatologico in Latina, Italy, treated over one thousand patients suffering from lumbar sciatic pain with oxygen-ozone injections as an alternative to surgery. Of this group, fifty patients were studied who had received periodic injections of oxygen and ozone. Three- and six-month follow-up examinations were conducted. The results showed 68 percent positive results (40 percent excellent and 28 percent good) and 32 percent negative results (10 percent underwent surgery and 22 percent had to continue medical and physical treatment). Computed tomography (CT) scans (which apparently use different criteria) revealed 82 percent positive results (36 percent excellent, 46 percent good), with no major changes between pre- and post-treatment scans in the remaining 18 percent. The researchers concluded:
Ozone therapy, thanks to its ease of execution and noninvasive-ness, permits the successful outpatient treatment of lumbar sciatic pain. Moreover, the lack of major complications and the good results obtained compared to other methods, such as chemonucleolysis, percutaneous automated discectomy, microsurgery and conventional surgery, suggest that ozone therapy can be considered the treatment of choice for lumbar sciatic pain and a valid alternative to surgery in many cases.15
A later Italian study involving 2,200 patients was carried out by physicians at the neuroradiology department at the Antonio Cardarelli Hospital in Naples. Most patients received treatment with oxygen-ozone injections and physical therapy for at least two months. No side effects were reported. After six months, researchers found an impressive 80 percent success and 20 percent failure rate among 1,750 patients; after eighteen months, the rate dropped to 75 percent success and 25 percent failure among 1,400 patients.16
Similar results were reported by Dr. Matteo Bonetti and colleagues at the Istituto Clinico Citta di Brescia, also in Italy. In this randomized, controlled study, a total of 306 patients suffering from low back pain and sciatica (161 with primary disc disease and 145 with nondisc vertebral disease) were treated either with oxygen-ozone injections or with steroids. Results were evaluated after six months. Clinical outcomes were poor among 15.1 percent of the eighty-one patients with disc disease receiving ozone and in 22.5 percent of eighty patients receiving steroids. Among the patients without disc disease, 8.6 percent of seventy patients receiving ozone had a poor outcome, while 21.4 percent of the seventy-five patients taking steroids had a poor outcome. The researchers concluded: “Oxygen-ozone treatment was highly effective in relieving acute and chronic lower back pain and sciatica. The gas mixture can be administered as a first treatment to replace epidural steroids.”17
SPONDYLOLYSIS
Dr. Bonetti and his colleagues later undertook a clinical trial on patients with first-degree spondylolisthesis and spondylolysis, two very painful lower-back conditions. They chose eighteen patients with low back pain and sciatica (with radiological and CT scan diagnoses of spondylolisthesis and spondylolysis) who had had no success with physical therapy and traditional medical management. Following oxygen-ozone injections into the lysis points guided by CT scan, fifteen (83.3 percent) experienced a complete remission of pain. Follow-up visits at one, three, and six months after treatment revealed no reported recurrence of pain.18
Cervical spondylosis normally occurs in adults aged fifty or older. It is a disorder in which there is abnormal wear on the cartilage and bones of the neck (cervical vertebrae). It is a common cause of chronic neck pain.
A group of physicians at the 316th Hospital of the People’s Liberation Army in Beijing studied the effect of a unique newly patented therapeutic ozone and laser combined puncture needle on patients.
A total of fifty-eight patients diagnosed with cervical spondylosis were chosen for this novel study. All were treated with the ozone and laser combined puncture needle between August 2008 and February 2010. Visual analog scale (VAS) scores were evaluated before treatment and at one month, three months, and six months after treatment. The visual analog scale is a psychometric response scale used in patient questionnaires. It is an instrument for measuring a patient’s feelings or attitudes regarding pain.
The VAS score of preoperative neck and shoulder pain was (6.57±1.34), which decreased to 1.80±0.65 at one week after treatment. Pain was completely alleviated by the end of one month (with VAS scores of 0~2 after one month, three months, and six months after treatment). VAS scores did not exhibit any significant rebound within six months after treatment. After six months, 29 patients were rated “excellent,” 23 were “good,” and 6 were “fair,” with the overall “excellent” and “good” rate at 89.6 percent.
The doctors concluded: “Ozone and laser combined therapy via puncture needle for the treatment of cervical spondylosis is safe and effective.”19
JOINT PAIN AND PROLOZONE THERAPY
Derived from the word ozone and the Latin word proli (to regenerate or rebuild), Prolozone therapy was developed by Dr. Frank Shallenberger. It involves injecting a mixture of ozone gas, procaine, vitamin B12, and selected homeopathic preparations into soft tissues, ligaments, and/or tendons where they attach to the bone. This causes a localized inflammation and anabolic (muscle-building) effect in these weak areas, which then increases the blood supply and stimulates the deposition of fibroblasts, the cells that the body uses to repair damaged connective tissue. Dr. Shallenberger writes:
Ozone stimulates the cells called fibroblasts and chondroblasts to lay down more collagen and cartilage, and in this way actually heals damaged joints and ligaments. Many patients who were told, “you need a total knee or hip replacement,” are still out running around years later after a series of ozone injections. Injecting ozone into injured or degenerated backs, hips, knees, shoulders, or necks is very rewarding.20
Shallenberger uses this method to treat patients suffering from a wide variety of chronic pain syndromes, including neck pain, whiplash, degenerated or herniated discs, carpal tunnel syndrome, torn tendons, TMJ (temporomandibular joint) syndrome, sciatica, heel spurs, neuromas, tennis elbow, rotator cuff tears, knee injuries, and other sports injuries. He also finds Prolozone useful in reducing scar tissue due to accidents or surgery. Shallenberger writes, “When Prolozone therapy is administered correctly, there is an 85 percent chance for the chronic pain sufferer to become completely pain free.”21
In October 2005 I attended a seminar devoted to Prolozone therapy conducted by Dr. Shallenberger for physicians and witnessed impressive results. Many of the patients complaining of chronic joint pain found almost immediate relief, although a series of four or five treatments is recommended over a period of several months. Figure 14.1 shows a patient receiving a Prolozone injection.
MANDIBULAR OSTEOMYELITIS
Mandibular osteomyelitis is an infectious inflammation of the lower jaw marked by local death and separation of tissue. Russian physicians studied a group of patients suffering from this disease and treated them both locally and generally with oxygen-ozone. They concluded: “Medical ozone exposure promoted more complete and rapid normalization of nonspecific resistance and T-cellular immunity, thus accelerating clinical cure and reducing the incidence of complications.”22
OSTEOARTHRITIS
Osteoarthritis, sometimes called degenerative joint disease, is a slowly progressive disease in which joint cartilage breaks down. When osteoarthritis (OA) occurs, cartilage becomes thin and irregular, resulting in symptoms of joint pain and stiffness. It most often affects the hips, knees, hands, and spine.
At the Center of Medical-Surgical Studies in Cuba, sixty patients with osteoarthritis (mostly affecting the knee) were given one intra-articular injection of ozone per week for a total of ten weeks. Of the sixty patients, only four experienced the return of painful symptoms after two months, while the majority (93.3 percent) were symptom free. The researchers concluded that this easily applied and low-cost therapy produced “disappearance of pain after the first several ozone applications, as well as diminished clinical inflammation of the joints and restoration of normal joint movement.”23
One of the current trends in oxygen therapy research has involved evaluating the value of medical ozone as an adjuvant to other types of medical therapy. Adjuvant has been defined as a substance or therapy that enhances the effectiveness of another medicine or form of treatment.
One such a study was carried out by researchers at the Beijing Geriatric Hospital to evaluate the clinical effectiveness of ozone therapy in combination with fugui gutong granule (FGG, a traditional Chinese medicine prepared with eight different herbs) in treating middle-aged and elderly patients with knee osteoarthritis (KOA) due to what the Chinese call “yang-deficiency induced cold-damp syndrome (YDICDS).”
Two hundred patients diagnosed with knee osteoarthritis were randomly assigned to four groups: the control group (Group A), the Chinese medicine treatment group (Group B), the ozone group (Group C), and the Chinese-medicine treatment plus ozone group (Group D). Patients in Group A took oral Voltaren, a nonsteroidal antiinflammatory drug. Those in Group B took FGG. Patients in Group C received an oxygen-ozone injection (10 to 18 ml) in the knee joint cavity at 25 mg/L, once weekly for four weeks. Those in Group D received oxygen-ozone injections plus FGG. The therapeutic course for all participants in the study was one month. The efficacy of the various treatments was assessed using the visual analogue scale (VAS) and Western Ontario and MacMaster Universities Osteoarthritis Index (WOMAC).
The researchers found that the VAS score was markedly lower in Group D than in Group B and Group A at twenty-four hours and one week after the first treatment. After one month of treatment, the VAS score was markedly lower in Group D than in Groups A, B, and C. After treatment, the WOMAC score was 25.34 in Group D, which was substantially lower than that in Group A (44.72), Group B (40.58), and Group C (38.53). The pain score, the joint stiffness score, and the score for daily activities were lower in Group D than in Group A. The level of cure was 76.0 percent in Group D, which was much higher than that of Group A (25 percent), Group B (25 percent), and Group C (43.8 percent). Ozone therapy alone worked better than any other method tested but was even more effective when combined with fugui gutong.24
An article appearing in ScienceDaily highlighted a study done at two Brazilian institutions—the Federal University of São Paulo and the Paulista School of Medicine—designed to find out if ozone and oxygen injected into joints would reduce pain, increase joint function, and improve the quality of life of patients diagnosed with osteoarthritis.
The researchers followed ninety-eight people through the course of the study. Sixty-three of the participants received 10 ml injections of oxygen-ozone throughout the study, and thirty-five received 10 ml injections of air as a placebo. The researchers evaluated the participants at the beginning of the study, after their fourth and eighth injections, and eight weeks after their last injection. They paid special attention to changes in pain, joint function, and the ability to sit, stand, and walk.
Timed up and go tests (known as “TUG tests”) were performed on members of both groups to determine the time it took to stand up, walk a set distance, return, and sit. The researchers found no significant differences in how the two groups performed in these tests. However, the group receiving oxygen-ozone injections had significantly better results in tests that measured pain, function, and overall health throughout the course of the study. At the end of the study, participants were given a quality-of-life survey (obtained using the Short Form-36 Health Survey). Participants in the ozone group reported improvement in all areas that pertain to quality of life after their fourth injection.
The researchers, who presented their results at the annual meeting of the American College of Rheumatology in San Francisco in November 2015, concluded, “We think the work means that ozone can give the patient a better quality of life with less pain and more independence in daily life activities. . . . Ozone is also capable of delaying the need for joint replacement surgery. It is a tool for the clinician to reduce pain or to help control it.”25

Figure 14.1. Patient receiving a Prolozone injection for lower back pain. (Photograph by Nathaniel Altman.)
OSTEOPOROSIS
Dr. Kief has also treated patients suffering from osteoporosis, a degenerative disease involving a lack of calcium and the resultant softening of the bones. During my visit to his clinic, he spoke of a seventy-two-yearold patient suffering from both immune vascularitis (inflammation of the blood vessels) and advanced osteoporosis. The patient was first given autohemotherapy, followed by long-term autohomologous immunotherapy (AHIT), which Dr. Kief believes is more effective.26 After one year, X-rays showed the normal calcification of bones, as seen in figure 14.2.
RHEUMATOID ARTHRITIS
Rheumatoid arthritis is a chronic, systemic disease that causes one’s joints to swell up and become painful. It is usually treated with anti-inflammatory drugs. Research carried out at Cuba’s Institute of Rheumatology in 1988 compared the effectiveness of ozone and anti-inflammatory drugs on seventeen patients. In this study doctors administered a very low dose (0.7 mg) of ozone intramuscularly each day to ten patients for eight weeks, while the control group of seven patients was given traditional anti-inflammatory drugs. In all areas of criteria (including morning stiffness, painful movements, onset of fatigue, strength of handclasp, and joint swelling), the patients who received ozone scored approximately 25 percent better than those receiving drug therapy. In addition, these patients suffered no adverse side effects, while all the nonozonated patients either had to receive additional steroids or suffered symptoms of gastritis.27
Approximately 10 percent of all patients seeking care at the Kief Clinic in Germany suffer from rheumatoid arthritis. In a statistical study of eighty-four such patients receiving AHIT therapy, Dr. Kief reported the following results: 16 percent experienced a full remission of symptoms, 36 percent showed significant improvement (including a decrease in swelling, improved mobility, and less pain), 32 percent experienced some improvement, and 12 percent had no improvement at all. Apparently 4 percent dropped out of the study.28
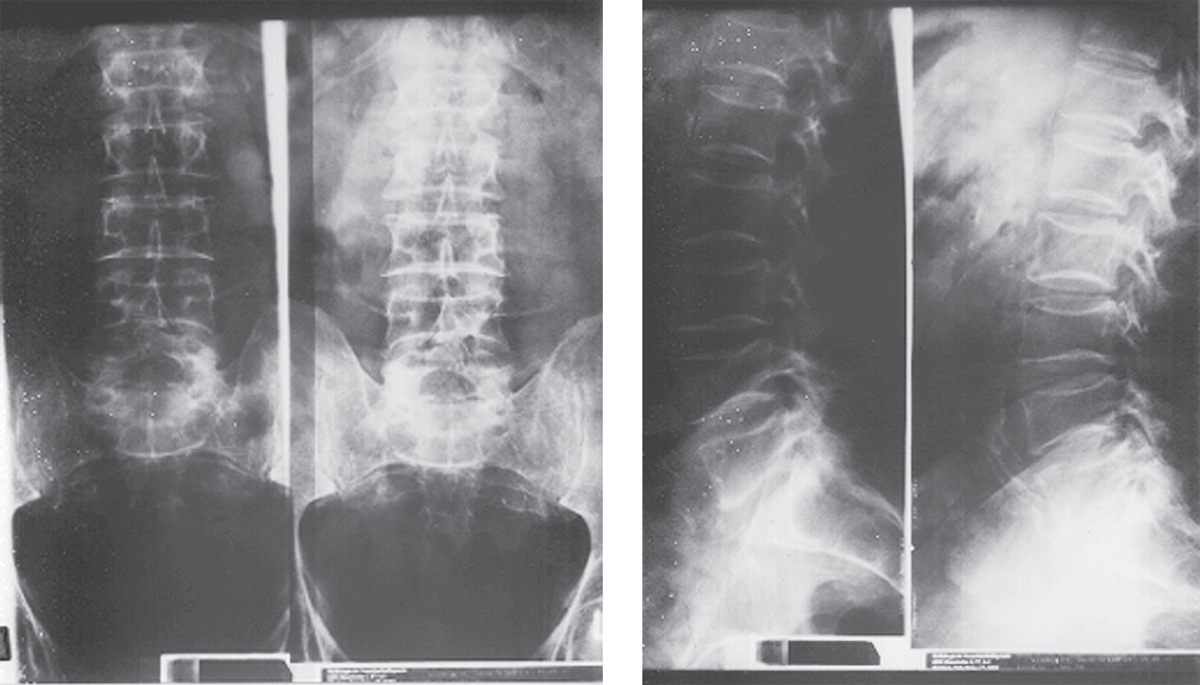
Figure 14.2. X-ray photographs of a seventy-two-year-old patient with osteoporosis, before and after major autohemotherapy. (Photographs courtesy of Dr. Horst Kief.)
TMD/TMJD PAIN
Temporomandibular joint dysfunction (TMD or TMJD)—also known as temporomandibular joint dysfunction syndrome—is a general term covering pain and dysfunction of the muscles that move the jaw and the joints that connect the jaw to the skull. A pioneer study carried out by researchers at the Cumhuriyet University School of Medicine in Turkey found that high-frequency bio-oxidative therapy proved more effective than medication in treating painful temporomandibular joint (TMJ) disorder.
Sixty-three patients were chosen for this study. Thirty were given three medications—Ketoprofen, Bi-Profenid, and thiocolchicoside—for seven days. The thirty-three others received oxygen-ozone therapy through an Omega probe to both joint sides. The researchers wrote about this novel delivery method: “Inside the glass probe, which is formed by a double glass camera, is a mixture of noble gases that conducts and emits electromagnetic energy. When the tip of the probe comes into contact with the body, it emits energy around the treated area and splits environmental, diatomic oxygen into singular atomic oxygen and ozone.” These treatments were administered for ten minutes three times during the week. There were no reports of pain, although patients felt a mild increase in temperature in the areas treated.
After a week of treatments, the researchers found that 24 percent of the medicated group showed a significant reduction in TMJ pain, while the figure for patients treated with ozone was 29 percent. Four patients in the group treated with ozone did not complain of any pain after treatment, while none of the patients treated with medication had complete relief. The authors concluded, “The study showed that bio-oxidative therapy was a more effective treatment than medication therapy for relieving TMJ pain.”29
FAILED BACK SURGERY SYNDROME
A pilot study was undertaken by researchers at the School of Medicine of the University of São Paulo to evaluate the effects of ozone administered by spinal endoscopy in patients with chronic pain related to failed back surgery. Spinal endoscopy is a procedure in which a small endoscope is passed up through the tailbone into the epidural space. It is sometimes used to allow medications to better reach the affected areas, especially the spinal nerve roots.
The investigators studied thirteen patients of both sexes between the ages of eighteen and seventy suffering from persistent chronic pain (i.e., for more than six months) in the lumbar region and in the lower limbs related to failed back surgery. Pain was classified as neuropathic (nerverelated) and non-neuropathic of the lumbar spine and legs, based on the DN4 (Douleur Neuropathique 4) questionnaire. The patients received the ozone gas in the lumbar epidural space via spinal-sacral endoscopy. Clinical evaluations were performed before, twenty-four hours after, and one month, three months, and six months after intervention using both a visual analog scale and the Oswestry Disability Index (ODI).
The researchers found that overall, at six months patients had a 43.7 percent reduction in lumbar pain and a 60.9 percent reduction in leg pain, followed by a 44.0 percent improvement in ODI scores. They also found that reduction of pain and better scores in the disability index were markedly greater in patients with non-neuropathic predominant pain; patients saw 95.2 percent, 80.6 percent, and 75.3 percent improvement in lumbar pain, leg pain, and ODI respectively. By contrast, patients with neuropathic predominant pain experienced only 12.5 percent, 42.4 percent, and 20.9 percent improvement, respectively. No infectious complications were observed during either treatment or follow-up.
The researchers concluded, “The present data suggests that epidural ozone might be a therapeutic option for persistent low back pain, especially in non-neuropathic predominant pain patients, but double-blind controlled studies are still required to prove its efficacy.”30
FIBROMYALGIA
Fibromyalgia is a chronic disease affecting over five million Americans. Its exact cause is unknown but is believed to involve psychological, genetic, neurobiological, and environmental factors. Although generalized pain is considered to be the primary symptom, many other associated symptoms are common, especially sleep disturbance, chronic fatigue, anxiety, and depression.
A pilot study was undertaken by researchers at the Universities of Granada and Almeria in Spain along with scientists from the National Center for Scientific Research in Cuba to evaluate the effectiveness and tolerability of ozone therapy by rectal insufflation as an add-on therapy in fibromyalgia management.
A total of thirty-six patients diagnosed with fibromyalgia (thirty-three women and three men) were recruited for this study. They received twenty-four sessions of ozone therapy during a twelve-week period. At each session, the administered dose of ozone was 8 mg (200 ml of gas, at a concentration of 40 μg/ml). Ozone sessions were given five days a week during the first two weeks, twice a week from weeks three through six, and weekly from weeks seven through twelve. The Fibromyalgia Impact Questionnaire was the main measure of outcome, and it was administered when the study began and at weeks four, eight, and twelve. Secondary outcome measures, administered at the beginning and end of the study, included the Pittsburgh Sleep Quality Index, the Beck Depression Inventory, the State-Trait Anxiety Inventory, and the SF-12, the abbreviated form of the Short Form Health Survey. Adverse reactions to treatment were also recorded.
The researchers found that the total scores of the Fibromyalgia Impact Questionnaire decreased significantly during the study period, with the decrease being observed in the first four weeks of the study. Significant improvement was also seen both in depression scores and in the physical summary score of the SF-12. Most of the positive effects of ozone therapy had to do with a reduction of physical symptoms, but depression was reduced in 47 percent of the patients. Transient meteorism (distension of the abdomen due to air or gas in the intestine) after ozone therapy sessions was the most frequently reported side effect, and it impacted approximately 36 percent of the patients at some point during treatment.
The researchers concluded, “At the dose and number of sessions used in this study, ozone therapy by rectal insufflation seems to be beneficial for physical symptoms and depression of fibromyalgia.”31