
Fig. 27.1 Sarcoptes scabiei
Discovered in 1687 by Bonomo, arthropod class Arachnida, subclass Acari, family Sarcoptidae. In the human host, infestation is with Sarcoptes scabiei var hominis
A parasitic mite with no natural predator. The ♀ penetrates the stratum corneum constructing short burrows where she lays 1–3 eggs daily during a lifespan of 4–6 weeks. Eggs are oval and 0.1–0.15 mm long. Six-legged larvae hatch in 3–4 days, then moult to form an eight-legged nymph. After a further moult, the adult develops. The total time to maturity is 10 days with females becoming gravid within 14 days.
The adult is tortoise-like in shape with 8 legs (Fig. 27.1). The two sets of anterior legs end in stalked pulvilli (suckers), which allow the mite to grip the host’s skin, aiding its movement. Spines and bristles cover the body. Mites are blind with no eyes. The adult female measures 0.4 mm across; the male is smaller and dies after mating. It has no spiracles, trachea, or body armour, and obtains its oxygen through its surface. Mites can move rapidly on warm skin at ~2.5 cm/min. Burrows are created at variable rates (0.5–5.0 mm/day) and are lined with scar tissue to prevent them collapsing, thus allowing the mite to breathe and larvae to escape. Mites feed on the lymph and lysed tissue. Survival of the mite away from its host is contentious, but is unlikely to be >48–72 hours and is probably much less.

Fig. 27.1 Sarcoptes scabiei
No. The majority of cases are not sexually transmitted. It commonly occurs in people living closely together and is spread by prolonged skin contact, including holding hands.
Treatment is advised for current and recent sexual partners and intimate household contacts.
No, not if you have used it properly and not been re-infected. Symptoms often take 4–5 weeks to resolve as they are due to a hypersensitivity reaction stimulated by mite products. It usually takes this time for them to be expelled from the skin and for the reaction to settle. If relief is required, topical crotamiton or antihistamines should help.
Appears as sporadic outbreaks, especially in families, schools, dormitories, institutions, and nurseries. Epidemics occur in 15–30 year cycles. Mammals such as domestic cats, dogs, pigs, and horses may be infected with other sarcoptidae (mange), which may be transferred to humans, resulting in irritation without infestation. These lesions are self-limiting. Treatment of mange is of the infested animal.
Holding hands is the most likely route of transmission. The more parasites on a person, the greater the risk of transmission. Prolonged skin-to-skin contact is necessary; mites are transferred after about 10–20 minutes of close contact and can penetrate the epidermis within 30 minutes. The parasites may remain viable on inanimate objects for 2–3 days, but fomite transmission is uncommon.
May occur in those using a bed recently occupied by an infested person. More likely in crusted scabies due to the greater number of mites present. Not vectors of other infections.
Patients may be asymptomatic for the first 4–6 weeks in first infection. Intense irritation occurs due to delayed Type IV hypersensitivity reaction to mites, their faeces, and eggs. In re-infestation, signs and symptoms become evident in 24–48 hours because of previous sensitization. Symmetrical polymorphic lesions appear, most commonly on hands (especially finger webs), wrists, axillae, genitals, buttocks, and extensor aspects of elbows (Fig. 27.2). Back relatively not involved, head spared (except in children). People are infectious before the rash develops. Rash is eczematous and associated with burrows (linear intraepidermal tunnels seen as fine short serpiginous grey channels 5–10 mm long, often with a small associated papule or vesicle). Nodules and papules seen on penis and scrotum. Urticarial lesions are rare. On average, 10–15 mites per host in primary infestations.
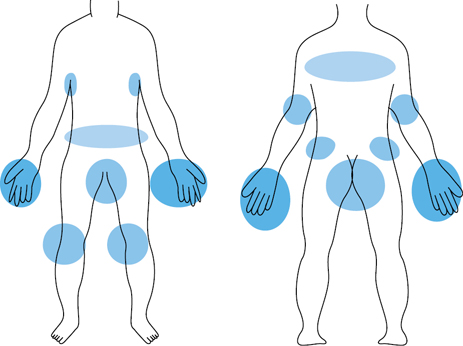
Fig. 27.2 Distribution of scabies
Found in the immunocompromised and elderly; may be related to failure of sensitization to mite antigen. For this reason itch less prominent. Highly contagious, with honeycombed cavities in the skin containing many thousands of mites. Extensive crusted lesions with thick hyperkeratotic scales (‘bread-crumb’) develop over the elbows, palms, knees, and soles of the feet, but can affect any part of the body including the face and scalp (see Plate 36). Scabies contracted by a healthy patient from a patient with crusted scabies is no different from classical scabies. Sepsis is a frequent complication.

Plate 36 Crusted ‘Norwegian’ scabies (27).
Reprinted from Gosney M., Harper A., and Conroy, S. (2012) Geriatric Medicine (Oxford Desk Reference), with permission from Oxford University Press.
May be atypical. Crusted scabies or minimal pruritus (if immunosuppressed), papular lesions, psoriasiform lesions, and generalized pruritus (with few lesions) may all be seen.
Altered picture seen following topical steroids. Widespread atypical papular lesions that mimic eczema.
Scabies should be suspected if history of itch, worse at night, affecting close contacts and classical skin rash (typical lesions, typical distribution). The diagnosis is usually clinical.
Definitive diagnosis is by microscopy.
Material can be obtained by;
• extraction of mites (or eggs) from their burrows with a needle
• scraping the skin using a scalpel blade, following local application of liquid paraffin.
Burrow ink test involves staining the suspected site with a washable felt-tip marker. After removal by washing, the ink will be found to have delineated the burrow (seen as a dark zigzag line running across and away from the lesion).
Mites can be recovered from the wrists (63%), extensor aspect of elbows (11%), feet and ankles (9%), genitals (9%), buttocks (4%), and axillae (2%).
Other possible methods of diagnosis (rarely used clinically) include; videodermatoscopy, epiluminescence microscopy, or skin biopsy. S. scabei DNA can be detected from skin scales using PCR.
Irritation may last for several weeks following successful treatment (antigenic material in the dermis and epidermis). Suspect treatment failure if itch >2–4 weeks following last dose of scabicide. Sedative antihistamines, crotamiton 10% cream bd/tid, or calamine 15% lotion may give symptomatic relief. Potentially contaminated clothes or bed linen (anything used by infested person or their contacts in the 4 days before treatment) should be washed at >60°C and dried in a hot dryer or dry cleaned. Patients with crusted scabies should be isolated in hospital to prevent nosocomial spread.
First line of treatment. Apply to the whole body from chin and ears downwards. Consider application to face and scalp in very young or elderly. Apply to cool skin (not following a hot bath as this may remove it from its site of action by  absorption into the bloodstream.) Allow to dry before dressing. Wash off after 8–12 hours. Reapply after 1 week. If hands are washed with soap within 8 hours, cream should be reapplied to hands.
absorption into the bloodstream.) Allow to dry before dressing. Wash off after 8–12 hours. Reapply after 1 week. If hands are washed with soap within 8 hours, cream should be reapplied to hands.
If permethrin not appropriate (e.g. if a person has an allergy to chrysanthemums.) Advice as above but should be left on body (including hands) for 24 hours before washing off.
• 200 mcg/kg, 2 doses, 2 weeks apart if weight >15kg
• available on a named patient basis, if no response to topical treatments.
Topical permethrin od for 7 days, then twice weekly until cure, plus oral ivermectin on days 1, 2, 8, 9, and 15.
Permethrin is the treatment of choice. Malathion is an alternative. Remove cream or lotion from nipples before breastfeeding and reapply following.
Has been reported to both permethrin and ivermectin.
Treat current sexual and household contacts at the same time. Contact tracing of partners from the previous 1 month is advised.
Further information