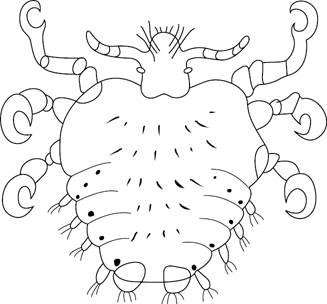
Fig. 28.1 Pthirus pubis
Pthiriasis (pediculosis) is an ancient disease. Nits (eggs of lice) have been discovered on the pubic hair of a 2000-year-old Chilean mummy, and also in fossilized form, dating back 10,000 years. Despite a rise in other STIs in recent years, it is now seen with less frequency in sexual health clinics. It has been suggested that the trend for pubic hair removal (through shaving, waxing, etc.) has resulted in the dramatic decline in the number of cases of pediculosis pubis recorded.
Belonging to the sub-order of Anoplura (sucking lice), the families of Pediculidae (body lice) and Pthiridae (pubic lice) are wingless insects unable to fly or jump. Humans are host to three species of lice. The pubic or crab louse, Pthirus pubis (Fig. 28.1), is classified as a species of the genus Pthirus. Head lice, Pediculus humanus capitis, and body lice, Pediculus humanus or corporis, are morphologically similar to each other and easily distinguished from pubic lice (which are smaller and squatter with thicker crab-like legs). The life-cycle of pubic lice is ~15–25 days occurring in three stages.
• white oval egg <0.8 mm attached to the hair base by a chitinous envelope
• encased by a proteinaceous sheath, except for the operculum, allowing ventilation
• appears to move up the hair and away from the skin as hair grows.
• resembles a pubic louse, but is smaller
• hatches in 7 days by releasing itself from the egg with air expelled from its anus
• migrates back to the hair base to suck blood and mature.
• ~1–2 mm in length, dark grey to brown in colour. ♂ is smaller and has a more pointed tail.
• three distinct pairs of legs, each with claw-like appendages whose grasp is designed to match the diameter of pubic or axillary hair in contrast with the finer scalp hair. Can move ~10 cm/day.
• sensory antennae detect human smell and tactile hairs on its body determine surface type. Eyes are faceted; it is almost blind, but photophobic.
• buries sharp mouthpiece stylets inside a pubic hair follicle to obtain a constant blood supply. Ingests several times its own weight in blood during each feed. May feed at the same place for days.
• single pair of spiracles allow gaseous exchange and prevent dehydration.
• ♀ will lay 2–3 eggs during a 24-hour period and 15–50 eggs over a lifetime.
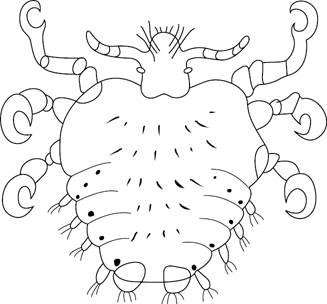
Fig. 28.1 Pthirus pubis
The crab louse is transmitted by close body contact and, hence, during sexual contact. More rarely, infestation can be spread through contact with an infested person’s bed linen, towel, or clothes.
Lice are treated with topical preparations. All body hair needs to be treated, not just the pubic hair. Shaving is not, therefore, recommended as treatment.
Yes, it is recommended that all clothes and bed linen are machine washed on a hot water cycle.
Yes, current sexual partners need treatment. Avoid close body contact until partner(s) have completed treatment. Contact tracing of all partners in the previous 3 months is recommended.
Spelling varies, with both Pthirus and Phthirus widely used. Although the name is derived from the Greek phtheir (louse), the former spelling is used more widely.
• Essentially a human parasite, although reported to infest higher apes.
• Does not occur in epidemics, although more common in the cooler months of the year (unlike body and head lice, which occur more often in the warmer months).
• Considered to be usually sexually transmitted because:
• found most commonly in sexually active adults (aged 16–25 years)
• associated with other STIs, especially chlamydia.
• Related to crowded living conditions, poor personal hygiene, and low socio-economic status.
• Infestation of the scalp is rare (about 1% of louse infestation), but occurs more often in red-headed people, who have fewer hairs per unit area than others.
• Rarely reported in the scalp and eyelashes of children. Acquisition from nipple hairs during breastfeeding has been reported and transmission through other close body contact is recognized. Sexual abuse should be considered.
• Can be used as a forensic tool. A mixed DNA profile of two hosts can be detectable in blood meals of the lice that have had close contact between an assailant and a victim.
• Not known to be vectors of human disease (unlike body and head lice, which may carry organisms responsible for epidemic or louse-borne typhus, trench fever, and louse-borne relapsing fever).
• Usually by skin-to-skin contact with up to 95% of sexual contacts of an active carrier developing an infestation.
• Occasionally by clothing, bedding, or towels.
• It is unlikely that lice can survive for more than 24–48 hours if removed from the host.
Pediculosis pubis is the name of the condition caused by infestation of the pubic hair by Pthirus pubis. ~76% complain of intense irritation in the genital area because of hypersensitivity, with ~40% of patients experiencing erythema. In the hirsute, infestation may spread to the thighs, perineum, trunk, abdomen, or axillary hair.
Pediculosis ciliaris or pthiriasis palpebrarum is infestation of the eyelashes by the pubic louse, where it can be responsible for a severe blepharoconjunctivitis. Eyebrows may also be infested. Headlice are very rarely responsible for eyelash infestation.
Blue macules (maculae cerulae) caused by an enzyme secreted from the salivary glands of the lice may be visible at feeding sites. They are 2–3 mm in diameter, with an irregular outline, painless, do not disappear on pressure, and appear to be in the deeper tissues. They become apparent some hours after the louse has fed, and last for several days. ‘Black spots’ on underwear or in the genital area usually indicate insect faecal matter or blood spots.
Concomitant STIs are present in ~30% of those infested.
Identify lice, eggs, or maculae cerulae with the naked eye. Low-power microscopy of the louse may show movement, sucking pumps in the head, and a blood-filled oesophagus.
Offer full screening for STIs and advise avoidance of close body contact until patient and partner(s) complete treatment. Clothes and bed linen should be washed at 50°C or dry-cleaned.
Because of the delicate nature of the genital skin, aqueous, rather than alcohol-based preparations are recommended. Lotions are more effective than shampoos. All body hair should be treated (to include genital and anal areas, thighs, trunk, axillae, moustache and beard areas) and left on as per manufacturer’s instructions. A second treatment after 7 days is advisable to kill lice emerging from any surviving nits. Dead nits may continue to adhere to hairs for several weeks following treatment and can be removed with a fine-tooth comb.
• Permethrin 5% dermal cream (a pyrethoid).
• Malathion 0.5% aqueous lotion (an organophosphate).
• Phenothrin 0.2% (a pyrethoid) only available as an alcoholic preparation and, therefore, more irritant. Same type of insecticide as permethrin; therefore, confers no advantage in cases of suspected permethrin resistance.
• Ivermectin (po) can be considered in resistant cases.
Eyes must be kept closed throughout. Insecticide should be applied for 5–10 minutes and then rinsed off thoroughly. Treatment should be repeated after 7 days:
• Permethrin, 1% cream rinse, ensuring patient keeps eyes closed throughout the procedure and for the following 10 minutes.
• Malathion, 1% cream shampoo (unlicensed for eyelashes and cannot be prescribed on the NHS, but can be bought over the counter).
• Application of yellow soft paraffin or white soft paraffin, which suffocates and kills the lice by occluding their spiracles. This should be done bd for 8–10 days.
• Removal of lice with forceps.
Sexual partners within the previous 3 months should be advised to seek screening and treatment. Those sharing the same bedding may also require treatment.
Further information