Common benign lesions/anomalies
• Angiokeratomas: purple/dark red papules on labia majora, scrotum, and penile shaft. Benign hyperkeratosis with dilated capillaries. Rarely associated with Anderson–Fabry disease.
• Ectopic sebaceous glands (Fordyce spots): tiny yellow grouped papules. Occasionally, form larger nodules. Usually found on the mucosal surface of the prepuce and inner labia minora.
• Epidermoid cysts: white or creamy coloured nodules commonly found over scrotum and labia majora. Hair follicles blocked with keratin and filled with sebaceous matter. Can be removed surgically.
• Epidermal naevi: epidermal outgrowths present at birth (50%) or developing during childhood.
• Haemangioma: red macule up to 3–5 mm in diameter on glans penis or vulval mucosa.
• Idiopathic calcinosis of the scrotum with multiple nodules: starts in the teens and may be mistaken for cysts. Surgery may be necessary for troublesome lesions, but should be avoided if possible.
• Melanocytic naevi (moles): genital lesions (keratinized skin) are found in 15% of the population.
• Nabothian follicles: bluish or yellow coloured translucent lumps on cervix. Retention cysts from cervical ‘glands’.
• Pearly penile papules: white dome-shaped papules found at the corona and adjacent to the frenulum. Sometimes confused with warts. Reported in 20–50%, usually <1 mm in size, may extend to 3 mm. Consists of connective tissue core with central, thinned epidermis. Removal generally not recommended, but clearance possible with cryosurgery and CO2 laser ablation.
• Pigmentary changes:
• vitiligo—depigmentation (may also affect hair); association with autoimmunity, especially thyroiditis
• mucosal melanosis (genital lentiginosis)—although unlikely to be malignant, all cases of vulval melanosis should be biopsied.
• Prominent hair follicles: found on penile shaft, scrotum, labia majora.
• Seborrhoeic keratosis: domed, often pigmented, papules. Commonly found on mons pubis, penile shaft, labia majora (usually in those aged >50 years). If removal required, cryosurgery or curettage.
• Skin tags (achrocordon): common around the groin and thighs, especially in those aged >50 years; more common if obese.
• Vulval papillae: fleshy filiform papules, commonly found within the labia minora and often confused with warts. Typically, soft, symmetrical, linear, and pink with separate bases.
Degenerative condition
Ovarian failure, usually  to the menopause, leads to urogenital atrophy, symptomatic in >50%. Symptoms include vulvo-vaginal dryness with discomfort, irritation, and dyspareunia. Often associated with other systemic symptoms, which may influence management. Treat with oestrogen-based hormone replacement therapy, which can be administered by various routes (oral, transdermal, vaginal). Urogenital symptoms may take some months to respond.
to the menopause, leads to urogenital atrophy, symptomatic in >50%. Symptoms include vulvo-vaginal dryness with discomfort, irritation, and dyspareunia. Often associated with other systemic symptoms, which may influence management. Treat with oestrogen-based hormone replacement therapy, which can be administered by various routes (oral, transdermal, vaginal). Urogenital symptoms may take some months to respond.
Infective conditions
Tinea cruris
Dermatophytic fungal infection commonly due to Trichophyton rubrum or Epidermophyton floccosum. Found in those sharing communal facilities (e.g. towels) and auto-inoculation from tinea pedis. Pruritic plaques in the groin, spreading out to the thigh, with well-defined erythematous scaly edge and central clearing.
Diagnosis
Appearance, scraping from margins for microscopy (dekeratinize with potassium hydroxide), and culture.
Management
Topical imidazoles bd for 2 weeks or topical terbinafine for 1–2 weeks; oral terbinafine 250 mg daily for 2–4 weeks or itraconazole 100 mg daily for 15 days or 200 mg daily for 7 days.
Erythrasma
Chronic infection of crural folds (especially axilla and groin) caused by Corynebacterium minutissimum. Associated with hyperhidrosis, diabetes mellitus, and living in crowded conditions. Dull red or brownish uniform scaly patch with little or no pruritus.
Diagnosis
Coral-pink fluorescence with Wood’s light makes culture of scale unnecessary.
Management
Topical imidazoles for 2 weeks are usually effective. Sodium fusidate ointment 2%, topical erythromycin gel 2% bd for 2 weeks, or oral erythromycin are alternatives.
Inflammatory conditions
Irritant and contact dermatitis
See Box 29.1.
• Irritant: direct response to noxious agent, e.g. urine, chemicals, soaps, disinfectants.
• Allergic: idiosyncratic hypersensitivity reaction, e.g. spermicides, semen, or its contents (e.g. antibiotics), local anaesthetics, latex, deodorants, fragrances, lubricants, and body lotions containing propylene glycol or glycerin, anti-mycotic creams, or other topical medications.
Erythema, excoriation, pruritus
Thin mucosal skin is more prone to react to contact agents. May become chronic (lichen simplex chronicus) with excoriation producing lichenification and erythema, or hyperpigmentation.
Diagnosis
History, appearance, exclude infection. For contact dermatitis, patch testing can be considered, although positive results are often not relevant. Radio-allergosorbent and skin-prick tests can be performed for suspected Type I immediate hypersensitivity.
Management
Advise on avoiding irritants. If moderate to severe, low-potency topical steroids. If lichenified or failure to respond, moderate-potency topical steroids.
Box 29.1 Genital allergic contact hypersensitivity
• Seminal fluid or its contents (e.g. antibiotics): often associated with systemic symptoms.
• Spermicides and lubricants (may cause irritant or contact dermatitis).
• Latex or products used in condom manufacturing (e.g. carbamates).
• Topical skin preparations or chemicals (e.g. steroid preparations, anaesthetics, imidazoles). May cause irritant or allergic contact dermatitis.
• Perfumes and cosmetic preparations:
• female hygiene sprays or wipes
• bubble baths, scented soaps, hair shampoos
• sanitary pads and towels (may be chemically treated).
Seborrhoeic dermatitis
Scaly inflammation of sebaceous skin. More common with HIV infection. Presents as dry erythema with yellow scale (labia minora, sub-preputial sac, and glans penis).
Diagnosis
Appearance of erythematous lesions covered with greasy yellowish scales at other typical sites (scalp, eyebrows, nasolabial folds, sternum, axillae, umbilicus, natal cleft).
Management
Combined imidazole plus hydrocortisone cream, ketoconazole shampoo (can use as shower gel), low-potency topical steroids and oral itraconazole if severe and extensive.
Fixed drug eruption
Reaction at the same site in an individual to repeated use of a systemic agent. Over 500 drugs implicated, including tetracyclines, barbiturates, phenolphthalein (chocolate laxative), sulfonamides, paracetamol. Preferentially affects genitals (especially glans penis). Sudden onset of erythematous macule or bulla with irritation or pain.
Diagnosis
History and appearance.
Management
Stop drug. Spontaneously resolves, but may leave hyperpigmentation.
Psoriasis
Affects ~2% of UK population, 30% familial incidence, increased severity with HIV infection. Anogenital/perigenital lesions common, which may be:
• Well-demarcated erythematous scaly papules or plaques: usually found on skin around genitalia, labia majora, scrotum, penile shaft, and occasionally glans penis.
• Flexural: macular erythematous non-scaly moist patches arising in perigenital flexures, peri-anal, labia minora, sub-preputial sac, and glans penis.
Diagnosis
Appearance: lesions in more classic sites (knees, elbows, scalp, nails with pitting), and histology.
Management
Moderate-potency topical corticosteroids, coal tar preparations. Systemic treatment (methotrexate, acitretin, ciclosporin,) may be necessary if disease is severe or extensive. Increasingly, biological agents such as etanercept are being used.
Lichen planus
Polygonal violaceous papules (2–10 mm) or annular lesions, which may be covered by white streaks (Wickham’s striae). Usually found around flexor aspect of wrists, but genital involvement common and may cause erosions on mucous epithelium (See Plates 19 and 20) May lead to scarring with narrowing of introitus. Reticulate network over the buccal mucosa is characteristic. Itchy on skin; may be painful on mucous membranes. Has been associated with the development of squamous cell carcinoma (SCC) of the vulva.
Diagnosis
Appearance, classic sites, and histology (showing a band-like lymphohistiocytic infiltrate in the upper dermis, cytoid bodies, and basal cell hydropic degeneration.)
Management
Potent topical corticosteroids. Topical tacrolimus has been shown to be of benefit. This is an unlicensed indication and as the risk of malignancy is unknown, tacrolimus is not recommended as a first line agent.
Plasma cell balanitis (of Zoon)
Condition of middle-aged/older uncircumcised men. Moist shiny area of speckled erythema on glans or mucosal aspect of prepuce and often on adjacent surfaces. Half of cases have multiple lesions. Relatively asymptomatic despite striking appearance.
Diagnosis
Histology with heavy plasma cell infiltration; lozenge-shaped keratinocytes.
Management
Topical corticosteroids often combined with antimicrobials, e.g. Trimovate®, Betnovate C®. Persistent cases respond well to circumcision.
Plasma cell vulvitis
Similar histopathological features, but more symptomatic. Clinically resembles erosive lichen planus. Often associated with other dermatoses, such as lichen sclerosus, lichen planus, vulval and penile intraepithelial neoplasia.
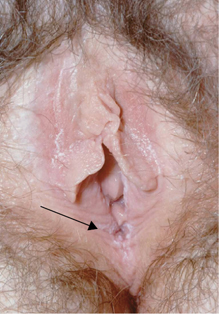
Lichen sclerosus (LS)
Associated with autoimmune conditions, especially thyroid abnormalities in women and with trauma (Koebner phenomenon). Anogenital skin involvement common, but may also occur in extragenital sites. May be asymptomatic or cause pruritus, discomfort, and painful intercourse and defaecation.
Although there may be signs of acute inflammation, typical finding is ivory-white appearance associated with atrophy, purpura, erosions, or lichenification (see Plate 18). Men may develop phimosis and meatal strictures. Women may develop labial adhesions with fusion and anal fissuring, or stenosis and a loss of clitoral architecture. LS may simulate signs of sexual abuse in prepubertal girls, although abuse causing trauma may also predispose. May also cause phimosis in prepubertal boys.
▶ Penile carcinoma rarely reported with LS, but up to 5% ♀ with LS develop SCC of the vulva.
Diagnosis
Histology shows atrophic epidermis, hyalinization of the upper dermis, and a lymphohistiocytic infiltrate.
Management
If active, potent or very potent topical corticosteroids for 3 months then  frequency of application, titrating against response. Topical tacrolimus has been helpful in some cases, but should be used cautiously due to risk of malignancy. Lubricants may help with intercourse. Acitretin has been shown to be of benefit, but is rarely necessary. UVA1 phototherapy has been used with some success. Surgical intervention may be required for urethral stenosis and circumcision for phimosis. Circumcision may be curative in men.
frequency of application, titrating against response. Topical tacrolimus has been helpful in some cases, but should be used cautiously due to risk of malignancy. Lubricants may help with intercourse. Acitretin has been shown to be of benefit, but is rarely necessary. UVA1 phototherapy has been used with some success. Surgical intervention may be required for urethral stenosis and circumcision for phimosis. Circumcision may be curative in men.
Hidradenitis suppurativa
Chronic inflammatory disorder of apocrine glands. Associated with acne, obesity, familial predisposition. Painful nodules, which may progress to abscesses, sinuses, fistulae, and scarring. Found in axillae, groin, buttocks, peri-anal skin.
Diagnosis
Clinical appearance. Exclude Crohn’s disease.
Management
Weight reduction, chlorhexidine wash, topical clindamycin, long-term tetracyclines, other antibiotics used for acne, local or systemic steroids, and surgery for severe disease. A non-controlled study of oral clindamycin combined with rifampicin showed benefit. Biological drugs, including infliximab and etanercept, have been used with benefit in severe cases.
Ulcerative conditions
Aphthous ulcers
Common condition of unknown aetiology. Recurrent oral ulcers, rarely genital (especially vulva and scrotum). May be familial. Shallow painful ulcers about 1–10 mm in diameter with no systemic symptoms.
Diagnosis
Clinical features. Exclude HSV infection and Behçet’s disease.
Management
Local anaesthetic gel, very potent topical steroids (if severe).
Lipschutz ulcers
Rapid onset, painful ulcers affecting vulva (typically labia minora) or lower vagina in young women. Often preceded by glandular fever type illness (has been associated with EBV, and other viral and bacterial infections).
Diagnosis
Classical history. Often a diagnosis of exclusion.
Management
Supportive (self-limiting, heal without scarring), pain relief (topical anaesthetics). Consider topical or short course oral steroids.
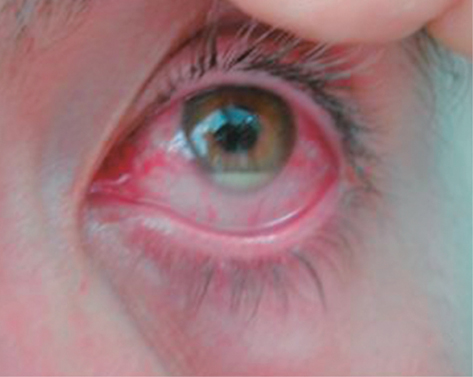
Behçet’s disease
Multisystem disease of unknown aetiology, but more commonly found in the Middle and Far East (Silk Route). Associated with certain HLA types, especially B51.
Diagnosis
Based on defined clinical features according to the International Study Group for Behçet’s disease (see Plates 21–24).
• Recurrent oral ulceration (as aphthosis) at least three times a year and two of the following:
• genital ulcers (including epididymitis)
• eye lesions (iritis, uveitis, cells in vitreous on slit-lamp examination, retinal vasculitis)
• skin lesions (erythema nodosum, folliculitis, or papulopustular lesions, acneiform nodules in post-adolescents not on corticosteroids)
• positive pathergy test (papule/pustule over 2 mm developing at site of hypodermic needle puncture; read at 24–48 hours).
• Neurological (meningoencephalitis, nerve palsies, brainstem, and spinal cord lesions), psychiatric changes, arthritis, thrombophlebitis and gastrointestinal features (diarrhoea, abdominal pain) may appear.
Management
Local topical steroids. Severe disease—systemic steroids, azathioprine, colchicine, dapsone, thalidomide. Anti-TNF therapy shows promise.
Erythema multiforme (EM) and Stevens–Johnson syndrome (SJS)
Acute skin reaction of unknown aetiology, but precipitated by infection (e.g. herpes simplex virus, Mycoplasma pneumoniae, Histoplasma capsulatum), drugs (e.g. sulfonamides, phenytoin, penicillin), autoimmune diseases (e.g. polyarteritis nodosa), sarcoidosis, malignancy,  frequency of SJS with HIV infection. Non-pruritic maculopapular circular lesions with a deep red centre (may form bullae), and erythema producing target or iris lesions, typically found around the hands and feet. The severe bullous form (SJS) includes orogenital bullae with ulceration, urethritis, conjunctivitis and keratitis, pyrexia, and multisystem disease. Secondary infection and death may occur.
frequency of SJS with HIV infection. Non-pruritic maculopapular circular lesions with a deep red centre (may form bullae), and erythema producing target or iris lesions, typically found around the hands and feet. The severe bullous form (SJS) includes orogenital bullae with ulceration, urethritis, conjunctivitis and keratitis, pyrexia, and multisystem disease. Secondary infection and death may occur.
Diagnosis
Clinical features and histopathological changes with necrotic epidermal cells.
Management
EM resolves without scarring in 2–3 weeks. Currently, no active therapeutic regimen with unequivocal benefit exists for SJS, although a number of agents including systemic steroids, IV immunoglobulin, and ciclosporin have been tried.
Pyoderma gangrenosum
Associated with many conditions, particularly inflammatory bowel disease, seropositive and seronegative arthritis, and blood dyscrasias. Initial pustule progressing to a painful necrotic ulcer, occasionally affecting the vulva, penis, or scrotum.
Diagnosis
Appearance of ulcer with black undermined edge and associated pathology. Histology usually non-specific.
Management
Treat underlying condition. Topical or systemic corticosteroids, topical tacrolimus, ciclosporin. There are case reports of other immunomodulatory agents and biological drugs including infliximab and adalumimab being of value in treatment.
Pemphigus vulgaris
Most common type of pemphigus. Autoimmune condition. Age group 50–60 years usually affected. Cutaneous lesions appear as flaccid bullae, which burst to form erosions or ulcers. The mucosae, especially the mouth, are commonly involved. Genital ulcers are slow to heal, but only occasionally scar. Finger pressure on skin may cause epidermis to separate because of its poor attachment.
Diagnosis
Histology with direct or immunofluorescence to show intercellular deposits of IgG, and complement and serology to show circulating anti-epidermal antibodies.
Management
Local or systemic corticosteroids, tetracyclines, immunosuppressants (dapsone, azathioprine, mycophenolate mofetil). Biological drugs, especially rituximab, look promising in refractory cases.
Premalignant conditions
Extra-mammary Paget’s disease
Most commonly found around anus and genitals, especially labia majora, typically presenting as well-defined erythematous scaly plaques, which may be itchy. May be associated with underlying adnexal carcinoma, possibly of sweat glands. A significant proportion have a primary carcinoma of other organs, particularly rectum, urethra, cervix, or breast.
Diagnosis
Histology shows typical large clear Paget cells in the epidermis.
Management
Excision where possible, but recurrence is common, as it is often multifocal. Topical imiquimod and photodynamic therapy have been reported to be helpful. Patients should be investigated for other carcinomas as above.
High-grade squamous intraepithelial lesions (HSIL) and low-grade squamous intraepithelial lesions (LSIL) of the genital tract
These pathological descriptive names encompass and replace other terms used to describe dysplasia and squamous cell carcinoma in situ, including Bowen’s disease, bowenoid papulosis, and erythroplasia of Queyrat. Intra-epithelial neoplasia (IN) is commonly associated with LS, high-risk HPV infection and risk of IN elsewhere and is also found more frequently in those who are immunosuppressed (including with HIV infection). In 2004, the International Society for the Study of Vulvovaginal Diseases suggested only HSIL be classified as VIN, which was subdivided into usual type (associated with carcinogenic genotypes of HPV, smoking, and immunocompromised states) and differentiated type (associated with dermatological conditions such as LS). In 2015, a further reclassification was suggested, in which HSIL is analogous to usual type VIN and differentiated VIN remains the same. Flat lesions associated with basal cell atypia and koilocytic changes (formerly termed VIN1) are considered LSIL.
Vulval lesions
Usually ♀ aged 30–40 years, 70% current or past cigarette smokers, 50–90% association with HPV (especially type 16). Clinical appearance varies, but often presents as white plaques or nodular lesions, which may be pigmented, with multifocal involvement (see Plate 17).
Penile lesions
Associated with HPV (especially type 16), smoking, and possibly agricultural chemicals. High-grade lesions found most commonly in the 6th decade. Usually presents as multiple lesions which may be:
• flat (grey/red, well demarcated with increased vascularity)
• small plaques of leukoplakia (hyperkeratinized)
• papular and pigmented.
In addition, usually in older uncircumcised ♂, there may be mucosal erythroplastic lesions (shiny friable moist red lesions on glans penis or mucosal surface of prepuce).
Anal lesions
Found most commonly in MSM, especially those with HIV infection, and in ♀ with a history of anal sex. Human papilloma virus 16 is associated with anal SCC.
Management of external anogenital IN
There is little evidence-based data on the management of this group of conditions. Current practice depends on the grading and extent of the pathology, influenced by clinical factors, such as appearance and symptoms. Patients should be screened for HIV infection. If HIV +ve, review should be maintained indefinitely. HSIL carries a 5–10% risk of subsequent SCC; therefore, treatment is usually advised. This includes topical imiquimod, surgical excision, and destructive methods including laser and electrodessication. Review after treatment required as ~30% recur within 5 years.
Malignant conditions
Rarely seen in the GUM clinic, but require urgent referral elsewhere.
• SCC: associated with IN and LS.
• Melanoma: rare on penis, but genital lesions reported to account for 2–3% of melanomas in ♀.
• Basal cell carcinoma: rare on surfaces not commonly exposed to the sun. However, genital lesions have been reported, especially scrotal.
Topical treatments
Emollients
Oil-based emollients are preferable to water-based emollients as they are better absorbed and contain fewer preservatives, which can be potentially irritant or sensitizing.
It may be helpful to give patients a selection of emollient samples so that they can choose their favourite and, therefore, improve adherence.
Aqueous cream should only be used as a soap substitute. It is not suitable as a ‘leave-on’ product, as it contains sodium lauryl sulphate.
Spray emollients can be useful as they are easy to apply and can reduce ‘drag’ on delicate, inflamed skin/genital mucosa.
Steroids
See Table 29.1.
Table 29.1 Topical steroid preparations
| Strength |
Name |
| Mild |
Hydrocortisone 0.1–2.5%
Mild with antimicrobials: e.g. Canesten HC® |
| Moderate |
Betamethasone valerate 0.025%: e.g. Betnovate-RD®
Clobetasone butyrate 0.05%: e.g. Eumovate®
Moderate with antimicrobials: e.g. Trimovate® |
| Potent |
Beclomethasone diproprionate 0.025%: e.g. Betnovate®
Hydrocortisone butyrate 0.1%: e.g. Locoid®
Potent with antimicrobials: e.g. Betnovate-C® |
| Very potent |
Clobetasol propionate 0.05%: e.g. Dermovate®
Diflucortolone valerate 0.3%: e.g. Nerisone Forte®
Very potent with antimicrobials: e.g. clobetasol with neomycin and nystatin ‘Dermovate® NN’ |
 to the menopause, leads to urogenital atrophy, symptomatic in >50%. Symptoms include vulvo-vaginal dryness with discomfort, irritation, and dyspareunia. Often associated with other systemic symptoms, which may influence management. Treat with oestrogen-based hormone replacement therapy, which can be administered by various routes (oral, transdermal, vaginal). Urogenital symptoms may take some months to respond.
to the menopause, leads to urogenital atrophy, symptomatic in >50%. Symptoms include vulvo-vaginal dryness with discomfort, irritation, and dyspareunia. Often associated with other systemic symptoms, which may influence management. Treat with oestrogen-based hormone replacement therapy, which can be administered by various routes (oral, transdermal, vaginal). Urogenital symptoms may take some months to respond.





 frequency of SJS with HIV infection. Non-pruritic maculopapular circular lesions with a deep red centre (may form bullae), and erythema producing target or iris lesions, typically found around the hands and feet. The severe bullous form (SJS) includes orogenital bullae with ulceration, urethritis, conjunctivitis and keratitis, pyrexia, and multisystem disease. Secondary infection and death may occur.
frequency of SJS with HIV infection. Non-pruritic maculopapular circular lesions with a deep red centre (may form bullae), and erythema producing target or iris lesions, typically found around the hands and feet. The severe bullous form (SJS) includes orogenital bullae with ulceration, urethritis, conjunctivitis and keratitis, pyrexia, and multisystem disease. Secondary infection and death may occur.