Clinical staging
Early in the epidemic, before HIV was discovered, diagnosis of AIDS was largely based on finding Pneumocystis jirovecii pneumonia or Kaposi’s sarcoma. Revised WHO Clinical Staging of HIV/AIDS for Adults and Adolescents is also based on clinical progression and is used in third world countries and as a research tool (Tables 39.1 and 39.2). The Centers for Disease Control and Prevention devised a classification system, revised in 1993, based on clinical features, AIDS-defining illnesses and CD4 counts, see Table 39.3. The CD4 count is a useful predictor for the development of opportunistic infections (OIs) and malignancies, but it should be recognized that this may be influenced by other factors such as inter-current infection.
The revised WHO clinical staging of HIV/AIDS for adults and adolescents
See Table 39.1 for the clinical staging of HIV, and Table 39.2 for AIDS-defining conditions.
Table 39.1 Revised WHO clinical staging of HIV/AIDS for adults and adolescents
| Stage |
Characteristics |
| Primary HIV infection |
• Asymptomatic HIV infection
• Acute retroviral syndrome
|
| Clinical stage 1 |
• Asymptomatic
• Persistent generalized lymphadenopathy
|
| Clinical stage 2 |
• Weight loss (>10% body weight)
• Recurrent respiratory tract infections
• sinusitis
• bronchitis
• otitis media
• Angular cheilitis
• Recurrent oral ulceration
• Herpes zoster
• Papular pruritic eruptions
• Seborrhoiec dermititis
• Onychomycosis
|
| Clinical stage 3 |
• Unexplained chronic diarrhoea >1 month
• Severe weight loss (>10% body weight)
• Oral hairy leukoplakia
• Severe bacterial infection, e.g. empyema, osteomyelitis, pneumonia, meningitis
• Unexplained anaemia (<80 g/l), neutropaenia (<500/µl), thrombocytopaenia (<50000/µl) for >1 month
• Fever intermittent or chronic >1 month
• Oral candidiasis
• Pulmonary TB (in last 2 years)
• Acute necrotizing gingivitis, stomatitis, or periodontitis
|
Data sourced from World Health Organization WHO (2007) Case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. Geneva, World Health Organization.  www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf
www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf
Table 39.2 Clinical Stage 4 (AIDS defining conditions)
| Conditions where presumptive diagnosis may be made based on clinical symptoms/signs |
Conditions where diagnostic tests are required |
|
• HIV wasting syndrome
• Oesophageal candidiasis
• KS
• Extrapulmonary cryptococcosis
• Invasive cervical cancer
• Pneumonia (recurrent severe)
• Pneumocystis pneumonia
• HIV encephalopathy
• Herpes simplex:
• chronic (>1 month)
• oesophageal
|
• Invasive cervical cancer
• Visceral leishmaniasis
• Isosporiasis
• Mycobacterium avium complex
• Mycobacterium tuberculosis
• Any disseminated mycosis, e.g. coccidioidomycosis, histoplasmosis
• Cerebral toxoplasmosis
• Pneumonia (recurrent severe)
• Progressive multifocal leucoencephalopathy
• Salmonella (septicaemia, recurrent)
• Cryptosporidiosis
• CMV
• Lymphoma (cerebral or B cell non-Hodgkins)
|
Data sourced from World Health Organization WHO (2007) Case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. Geneva, World Health Organization.  www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf
www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf
Table 39.3 Revised classification of HIV disease (CDC January 1993)
| Categories CD4 (cells/µL) |
A |
B* |
C |
| Asymptomatic, acute HIV, or PGL |
Symptomatic conditions, not A or C |
AIDS-indicator conditions |
| ≥500 cells/µL |
A1 |
B1 |
C1 |
| 200-499 cells/µL |
A2 |
B2 |
C2 |
| <200 cells/µL |
A3 |
B3 |
C3 |
PGL, persistent generalized lymphadenopathy.
* Category B symptomatic conditions are defined as symptomatic conditions occurring in an HIV-infected adolescent or adult that meet at least one of the following criteria:
• They are attributed to HIV infection or indicate a defect in cell-mediated immunity.
• They are considered to have a clinical course or management that is complicated by HIV infection.
Data sourced from National Center for Infection Diseases Division of HIV/AIDS (1993) Revised Classification System for HIV Infection and Expanded Surveillance Case Definition for AIDS Among Adolescents and Adults. MMWR Recomm Rep. 41(RR-17): 1–19.
Natural history of untreated HIV infection
Characterized by progressive loss of immune function allowing the development of some virulent bacterial infections, certain opportunistic infections, and malignancies that define AIDS (Fig. 39.1). Progression rate varies depending on interactions between host, viral, and environmental factors. The average time between HIV acquisition and AIDS is 10 years if untreated.
The course of the disease can be divided into five continuous stages: seroconverion followed by early, middle, advanced, and late stages. There is significant individual variation between patients in the same clinical stage.
• HIV infection: disseminates widely in the body at seroconversion, usually with a very high VL and a rapid CD4 cell  , which is spontaneously, but not fully reversible.
, which is spontaneously, but not fully reversible.
• Early stage: CD4 count >500 cells/µL, viraemia  (rarely becoming undetectable). Usually asymptomatic apart from generalized lymphadenopathy and certain skin disorders (e.g. seborrhoeic dermatitis, aphthous ulcers, eosinophilic dermatitis, and psoriasis).
(rarely becoming undetectable). Usually asymptomatic apart from generalized lymphadenopathy and certain skin disorders (e.g. seborrhoeic dermatitis, aphthous ulcers, eosinophilic dermatitis, and psoriasis).
• Middle stage: CD4 count 200–500 cells/µL, mostly asymptomatic/mildly symptomatic. Skin disorders of early stage may worsen. Recurrent HSV, varicella zoster (VZV), diarrhoea, weight loss, and intermittent fever may develop. Lung infections caused by community-acquired organisms, such as Streptococcus pneumoniae, Haemophilus influenzae, and Mycobacterium tuberculosis become more common.
• Advanced stage: CD4 count 50–200 cells/µL.  VL with classical manifestations of AIDS, especially PCP, KS, lymphomas, and Mycobacterium avium complex (MAC) infection.
VL with classical manifestations of AIDS, especially PCP, KS, lymphomas, and Mycobacterium avium complex (MAC) infection.
• Late stage: CD4 count <50 cells/µL. Very high levels of viraemia. Further development of conditions associated with severe immune deficiency, e.g. CMV retinitis, disseminated MAC. Neurological manifestations  due to brain lymphoma, multifocal leukoencephalopathy, and dementia. HIV wasting disease is commonly seen at this stage.
due to brain lymphoma, multifocal leukoencephalopathy, and dementia. HIV wasting disease is commonly seen at this stage.
 www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf
www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf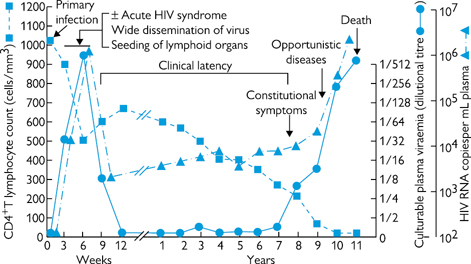
 , which is spontaneously, but not fully reversible.
, which is spontaneously, but not fully reversible. VL with classical manifestations of AIDS, especially PCP, KS, lymphomas, and Mycobacterium avium complex (MAC) infection.
VL with classical manifestations of AIDS, especially PCP, KS, lymphomas, and Mycobacterium avium complex (MAC) infection.