CHAPTER 13
Sepsis and Septic Shock
DEFINITIONS
• Systemic inflammatory response syndrome (SIRS)—Two or more of the following:
– Fever (oral temperature >38°C) or hypothermia (oral temperature <36°C)
– Tachypnea (>24 breaths/min)
– Tachycardia (>90 beats/min)
– Leukocytosis (>12,000/μL), leukopenia (<4000/μL), or >10% bands; may have a noninfectious etiology
• Sepsis—SIRS with a proven or suspected microbial etiology
• Severe sepsis—Sepsis with one or more signs of organ dysfunction
• Septic shock—Sepsis with hypotension (arterial blood pressure <90 mmHg or 40 mmHg below pt’s normal blood pressure for at least 1 h despite fluid resuscitation) or need for vasopressors to maintain systolic blood pressure ≥90 mmHg or mean arterial pressure ≥70 mmHg
ETIOLOGY
• Blood cultures are positive in 20–40% of sepsis cases and in 40–70% of septic shock cases.
• A single bacterial species accounts for ~70% of isolates in positive blood cultures; the remainder are fungal or polymicrobial.
EPIDEMIOLOGY
• The incidence of severe sepsis and septic shock in the United States continues to increase, with >700,000 cases each year contributing to >200,000 deaths.
• Invasive bacterial infections are a prominent cause of death around the world, especially among young children.
• Sepsis-related incidence and mortality rates increase with age and preexisting comorbidity, with two-thirds of cases occurring in pts with significant underlying disease.
• The increasing incidence of sepsis is attributable to the aging of the population, longer survival of pts with chronic diseases, a relatively high frequency of sepsis among AIDS pts, and medical treatments that circumvent host defenses (e.g., immunosuppressive agents, indwelling catheters, and mechanical devices).
PATHOPHYSIOLOGY
Local and Systemic Host Responses
• Hosts have numerous receptors that recognize highly conserved microbial molecules (e.g., lipopolysaccharide, lipoproteins, double-stranded RNA), triggering the release of cytokines and other host molecules that increase blood flow and neutrophil migration to the infected site, enhance local vascular permeability, and elicit pain.
• Many local and systemic control mechanisms diminish cellular responses to microbial molecules, including intravascular thrombosis (which prevents spread of infection and inflammation) and an increase in anti-inflammatory cytokines (e.g., IL-4 and IL-10).
Organ Dysfunction and Shock
• Widespread vascular endothelial injury is believed to be the major mechanism for multiorgan dysfunction.
• Septic shock is characterized by compromised oxygen delivery to tissues followed by a vasodilatory phase (a decrease in peripheral vascular resistance despite increased levels of vasopressor catecholamines).
CLINICAL FEATURES
• Hyperventilation
• Encephalopathy (disorientation, confusion)
• Acrocyanosis and ischemic necrosis of peripheral tissues (e.g., digits) due to hypotension and DIC
• Skin: hemorrhagic lesions, bullae, cellulitis, pustules. Skin lesions may suggest specific pathogens—e.g., petechiae and purpura suggest Neisseria meningitidis, and ecthyma gangrenosum suggests Pseudomonas aeruginosa.
• Gastrointestinal: nausea, vomiting, diarrhea, ileus, cholestatic jaundice
Major Complications
• Cardiopulmonary manifestations
– Ventilation-perfusion mismatch, increased alveolar capillary permeability, increased pulmonary water content, and decreased pulmonary compliance impede oxygen exchange and lead to acute respiratory distress syndrome (progressive diffuse pulmonary infiltrates and arterial hypoxemia) in ~50% of pts.
– Hypotension: Normal or increased cardiac output and decreased systemic vascular resistance distinguish septic shock from cardiogenic and hypovolemic shock.
– The ejection fraction is decreased, but ventricular dilatation allows maintenance of a normal stroke volume.
• Adrenal insufficiency: May be difficult to diagnose in critically ill pts.
• Renal manifestations: oliguria or polyuria, azotemia, proteinuria, and renal failure due to acute tubular necrosis
• Coagulopathy: thrombocytopenia
• Neurologic manifestations: polyneuropathy with distal motor weakness in prolonged sepsis
• Immunosuppression: Pts may have reactivation of HSV, CMV, or VZV.
Laboratory Findings
• CBC: leukocytosis with a left shift, thrombocytopenia
• Coagulation: prolonged thrombin time, decreased fibrinogen, presence of D-dimers, suggestive of DIC. With DIC, platelet counts usually fall below 50,000/μL.
• Chemistries: metabolic acidosis, elevated anion gap, elevated lactate levels
• LFTs: transaminitis, hyperbilirubinemia, azotemia, hypoalbuminemia
DIAGNOSIS
Definitive diagnosis requires isolation of the microorganism from blood or a local site of infection. Culture of infected cutaneous lesions may help establish the diagnosis.
TREATMENT Sepsis and Septic Shock
Pts in whom sepsis is suspected must be managed expeditiously, if possible within 1 h of presentation.
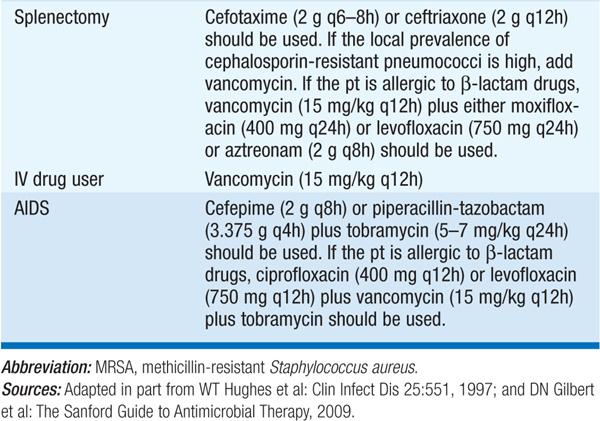
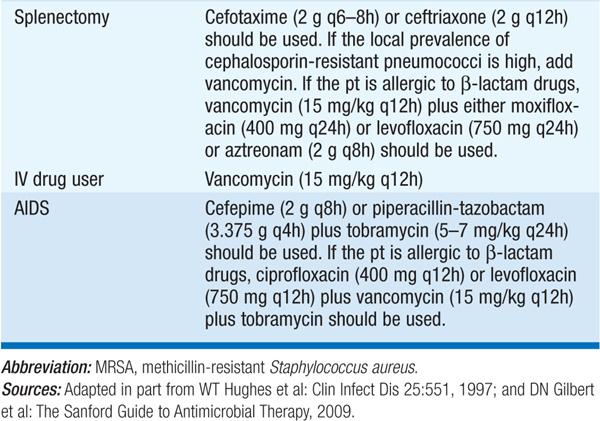
1. Antibiotic treatment: See Table 13-1.
TABLE 13-1 INITIAL ANTIMICROBIAL THERAPY FOR SEVERE SEPSIS WITH NO OBVIOUS SOURCE IN ADULTS WITH NORMAL RENAL FUNCTION

2. Removal or drainage of a focal source of infection
a. Remove indwelling intravascular catheters; replace Foley and other drainage catheters; drain local sources of infection.
b. Rule out sinusitis in pts with nasal intubation.
c. Image the chest, abdomen, and/or pelvis to evaluate for abscess.
3. Hemodynamic, respiratory, and metabolic support
a. Initiate treatment with 1–2 L of normal saline administered over 1–2 h, keeping the central venous pressure at 8–12 cmH2O, urine output at >0.5 mL/kg per hour, and mean arterial blood pressure at >65 mmHg. Add vasopressor therapy if needed.
b. If hypotension does not respond to fluid replacement therapy, hydrocortisone (50 mg IV q6h) should be given. If clinical improvement results within 24–48 h, most experts would continue hydro-cortisone treatment for 5–7 days.
c. Maintain oxygenation with ventilator support as indicated. Recent studies favor the use of low tidal volumes—typically 6 mL/kg of ideal body weight—provided the plateau pressure is ≤30 cmH2O.
d. Erythrocyte transfusion is recommended when the blood hemoglobin level decreases to ≤7 g/dL, with a target level of 9 g/dL.
4. Recombinant activated protein C (aPC) has been approved for treatment of severe sepsis or septic shock in pts with APACHE II scores of ≥25 prior to aPC infusion; however, given the increased risk of severe bleeding and uncertain performance in clinical practice, many experts are awaiting the results of additional trials before recommending further use of aPC.
5. General support: Nutritional supplementation should be given to pts with prolonged sepsis (i.e., that lasting >2–3 days), with available evidence suggesting an enteral delivery route. Prophylactic heparin should be administered to prevent deep-venous thrombosis if no active bleeding or coagulopathy is present. Insulin should be used to maintain the blood glucose concentration below ~150 mg/dL.
PROGNOSIS
In all, 20–35% of pts with severe sepsis and 40–60% of pts with septic shock die within 30 days, and further deaths occur within 6 months. Prognostic stratification systems (e.g., APACHE II) can estimate the risk of dying of severe sepsis.
PREVENTION
Nosocomial infections cause most episodes of severe sepsis and septic shock in the United States. Measures to reduce those infections could reduce the incidence of sepsis.

For a more detailed discussion, see Munford RS: Severe Sepsis and Septic Shock, Chap. 271, p. 2223, in HPIM-18.