CHAPTER 15
Acute Respiratory Distress Syndrome
DEFINITION AND ETIOLOGY
Acute respiratory distress syndrome (ARDS) develops rapidly and includes severe dyspnea, diffuse pulmonary infiltrates, and hypoxemia; it typically causes respiratory failure. Key diagnostic criteria for ARDS include (1) diffuse bilateral pulmonary infiltrates on chest x-ray (CXR); (2) Pao2 (arterial partial pressure of oxygen in mmHg)/Fio2 (inspired O2 fraction) ≤200 mmHg; and (3) absence of elevated left atrial pressure (pulmonary capillary wedge pressure ≤18 mmHg). Acute lung injury is a related but milder syndrome, with less profound hypoxemia  , that can develop into ARDS. Although many medical and surgical conditions can cause ARDS, most cases (>80%) result from sepsis, bacterial pneumonia, trauma, multiple transfusions, gastric acid aspiration, and drug overdose. Individuals with more than one predisposing factor have a greater risk of developing ARDS. Other risk factors include older age, chronic alcohol abuse, metabolic acidosis, and overall severity of critical illness.
, that can develop into ARDS. Although many medical and surgical conditions can cause ARDS, most cases (>80%) result from sepsis, bacterial pneumonia, trauma, multiple transfusions, gastric acid aspiration, and drug overdose. Individuals with more than one predisposing factor have a greater risk of developing ARDS. Other risk factors include older age, chronic alcohol abuse, metabolic acidosis, and overall severity of critical illness.
CLINICAL COURSE AND PATHOPHYSIOLOGY
There are three phases in the natural history of ARDS:
1. Exudative phase—Characterized by alveolar edema and leukocytic inflammation, with subsequent development of hyaline membranes from diffuse alveolar damage. The alveolar edema is most prominent in the dependent portions of the lung; this causes atelectasis and reduced lung compliance. Hypoxemia, tachypnea, and progressive dyspnea develop, and increased pulmonary dead space can also lead to hypercarbia. CXR reveals bilateral, diffuse alveolar and interstitial opacities. The differential diagnosis is broad, but common alternative etiologies to consider are cardiogenic pulmonary edema, pneumonia, and alveolar hemorrhage. Unlike cardiogenic pulmonary edema, the CXR in ARDS rarely shows cardiomegaly, pleural effusions, or pulmonary vascular redistribution. The exudative phase duration is typically up to 7 days in length and usually begins within 12–36 h after the inciting insult.
2. Proliferative phase—This phase typically lasts from approximately days 7 to 21 after the inciting insult. Although most pts recover, some will develop progressive lung injury and evidence of pulmonary fibrosis. Even among pts who show rapid improvement, dyspnea and hypoxemia often persist during this phase.
3. Fibrotic phase—Although the majority of pts recover within 3–4 weeks of the initial pulmonary injury, some experience progressive fibrosis, necessitating prolonged ventilatory support and/or supplemental O2. Increased risk of pneumothorax, reductions in lung compliance, and increased pulmonary dead space are observed during this phase.
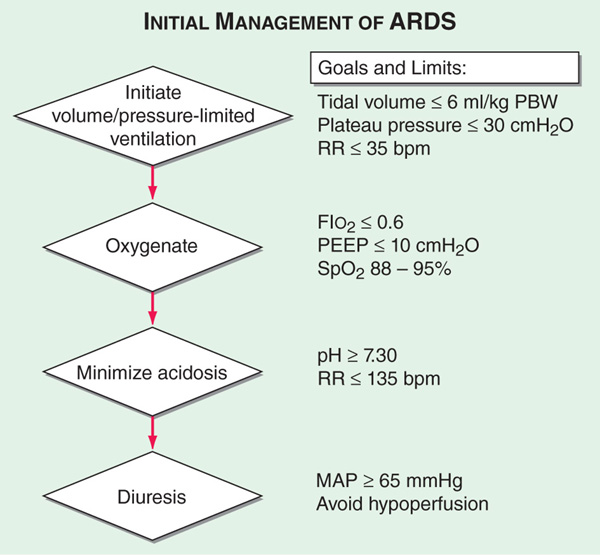
Progress in recent therapy has emphasized the importance of general critical care of pts with ARDS in addition to lung protective ventilator strategies. General care requires treatment of the underlying medical or surgical problem that caused lung injury, minimizing iatrogenic complications (e.g., procedure-related), prophylaxis to prevent venous thromboembolism and GI hemorrhage, prompt treatment of infections, and adequate nutritional support. An algorithm for the initial management of ARDS is presented in Fig. 15-1.
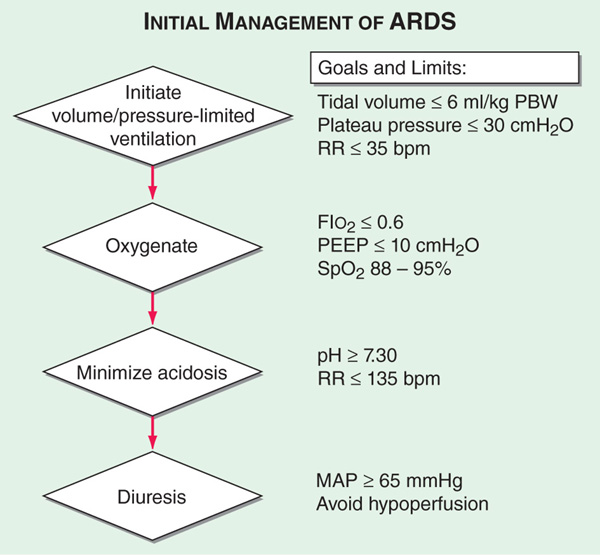
FIGURE 15-1 Algorithm for the initial management of ARDS. Clinical trials have provided evidence-based therapeutic goals for a step-wise approach to the early mechanical ventilation, oxygenation, correction of acidosis and diuresis of critically ill pts with ARDS.
MECHANICAL VENTILATORY SUPPORT Pts with ARDS typically require mechanical ventilatory support due to hypoxemia and increased work of breathing. A substantial improvement in outcomes from ARDS occurred with the recognition that mechanical ventilator–related over-distention of normal lung units with positive pressure can produce or exacerbate lung injury, causing or worsening ARDS. Currently recommended ventilator strategies limit alveolar distention but maintain adequate tissue oxygenation.
It has been clearly shown that low tidal volumes (≤6 mL/kg predicted body weight) provide reduced mortality compared with higher tidal volumes (12 mL/kg predicted body weight). In ARDS, alveolar collapse can occur due to alveolar/interstitial fluid accumulation and loss of surfactant, thus worsening hypoxemia. Therefore, low tidal volumes are combined with the use of positive end-expiratory pressure (PEEP) at levels that strive to minimize alveolar collapse and achieve adequate oxygenation with the lowest Fio2. Use of PEEP levels higher than required to optimize oxygenation has not been proven to be of benefit. Measurement of esophageal pressures to estimate transpulmonary pressure may help to identify an optimal level of PEEP. Other techniques that may improve oxygenation while limiting alveolar distention include extending the time of inspiration on the ventilator (inverse ratio ventilation) and placing the pt in the prone position. However, these approaches are not of proven benefit in reducing mortality from ARDS.
ANCILLARY THERAPIES Pts with ARDS have increased pulmonary vascular permeability leading to interstitial and alveolar edema. Therefore, they should receive IV fluids only as needed to achieve adequate cardiac output and tissue O2 delivery as assessed by urine output, acid-base status, and arterial pressure. There is not convincing evidence currently to support the use of glucocorticoids or nitric oxide in ARDS.
OUTCOMES
Mortality from ARDS has declined with improvements in general critical care treatment and with the introduction of low tidal volume ventilation. Current mortality from ARDS is 26–44%, with most deaths due to sepsis and nonpulmonary organ failure. Increased risk of mortality from ARDS is associated with advanced age, preexisting organ dysfunction (e.g., chronic liver disease, chronic alcohol abuse, chronic immunosuppression, and chronic renal disease), and direct lung injury (e.g., pneumonia, pulmonary contusion, and aspiration) compared with indirect lung injury (e.g., sepsis, trauma, and pancreatitis). Most surviving ARDS pts do not have significant long-term pulmonary disability.

For a more detailed discussion, see Levy BD, Choi AMK: Acute Respiratory Distress Syndrome, Chap. 268, p. 2205, in HPIM-18.
 , that can develop into ARDS. Although many medical and surgical conditions can cause ARDS, most cases (>80%) result from sepsis, bacterial pneumonia, trauma, multiple transfusions, gastric acid aspiration, and drug overdose. Individuals with more than one predisposing factor have a greater risk of developing ARDS. Other risk factors include older age, chronic alcohol abuse, metabolic acidosis, and overall severity of critical illness.
, that can develop into ARDS. Although many medical and surgical conditions can cause ARDS, most cases (>80%) result from sepsis, bacterial pneumonia, trauma, multiple transfusions, gastric acid aspiration, and drug overdose. Individuals with more than one predisposing factor have a greater risk of developing ARDS. Other risk factors include older age, chronic alcohol abuse, metabolic acidosis, and overall severity of critical illness.