
APPROACH TO THE PATIENT Disorders of Consciousness
Disorders of consciousness are common; these always signify a disorder of the nervous system. Assessment should determine whether there is a change in level of consciousness (drowsy, stuporous, comatose) and/or content of consciousness (confusion, perseveration, hallucinations). Confusion is a lack of clarity in thinking with inattentiveness; delirium is used to describe an acute confusional state; stupor, a state in which vigorous stimuli are needed to elicit a response; coma, a condition of unresponsiveness. Pts in such states are usually seriously ill, and etio-logic factors must be assessed (Tables 17-1 and 17-2).
TABLE 17-1 COMMON ETIOLOGIES OF DELIRIUM


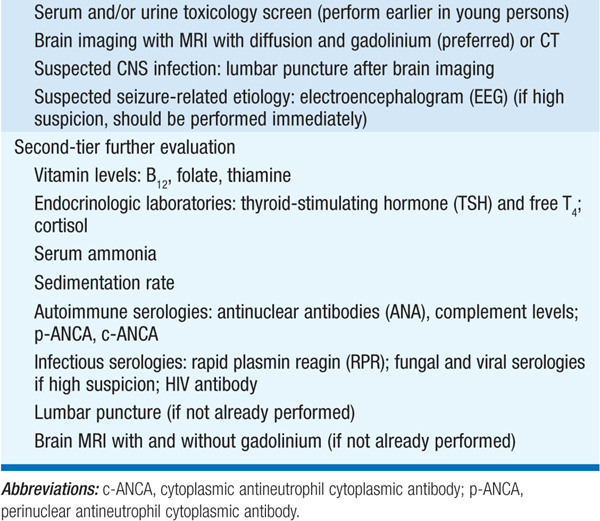
TABLE 17-2 STEPWISE EVALUATION OF A PATIENT WITH DELIRIUM
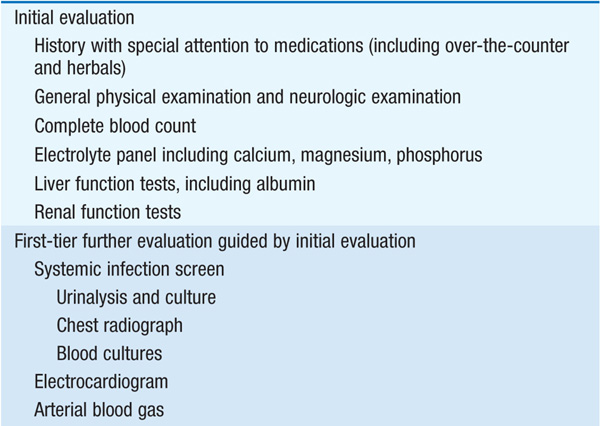
Delirium is a clinical diagnosis made at the bedside; a careful history and physical exam are necessary, focusing on common etiologies of delirium, especially toxins and metabolic conditions. Observation will usually reveal an altered level of consciousness or a deficit of attention. Attention can be assessed through a simple bedside test of digits forward—pts are asked to repeat successively longer random strings of digits beginning with two digits in a row; a digit span of four digits or less usually indicates an attentional deficit unless hearing or language barriers are present. Delirium is vastly underrecognized, especially in pts presenting with a quiet, hypoactive state.
A cost-effective approach to the evaluation of delirium allows the history and physical exam to guide tests. No single algorithm will fit all pts due to the large number of potential etiologies, but one step-wise approach is shown in Table 17-2.
Management of the delirious pt begins with treatment of the underlying inciting factor (e.g., pts with systemic infections should be given appropriate antibiotics, and electrolyte disturbances judiciously corrected). Relatively simple methods of supportive care can be quite effective, such as frequent reorientation by staff, preservation of sleep-wake cycles, and attempting to mimic the home environment as much as possible. Chemical restraints exacerbate delirium and should be used only when necessary to protect pt or staff from possible injury; antipsychotics at low dose are usually the treatment of choice.
TABLE 17-3 DIFFERENTIAL DIAGNOSIS OF COMA
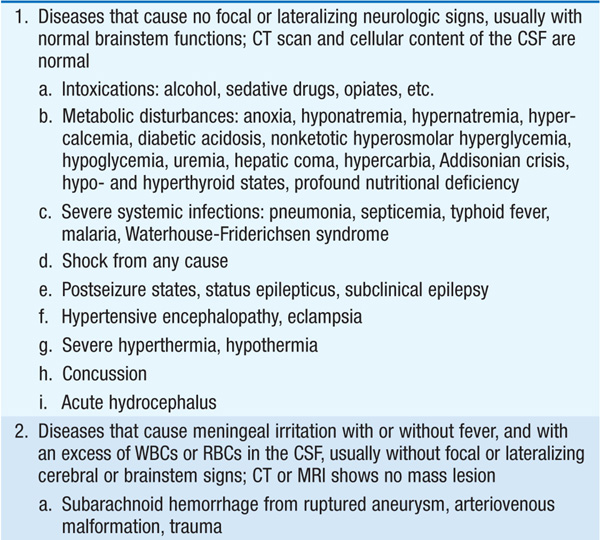

Because coma demands immediate attention, the physician must employ an organized approach. Almost all instances of coma can be traced to widespread abnormalities of the bilateral cerebral hemispheres or to reduced activity of the reticular activating system in the brainstem.
Pt should be aroused, if possible, and questioned regarding use of insulin, narcotics, anticoagulants, other prescription drugs, suicidal intent, recent trauma, headache, epilepsy, significant medical problems, and preceding symptoms. Witnesses and family members should be interviewed, often by phone. History of sudden headache followed by loss of consciousness suggests intracranial hemorrhage; preceding vertigo, nausea, diplopia, ataxia, hemi-sensory disorder suggest basilar insufficiency; chest pain, palpitations, and faintness suggest a cardiovascular cause.
Acute respiratory and cardiovascular problems should be attended to prior to the neurologic assessment. Vital signs should be evaluated, and appropriate support initiated. Thiamine, glucose, and naloxone should be administered if the etiology of coma is not immediately apparent. Blood should be drawn for glucose, electrolytes, calcium, and renal (BUN, creatinine) and hepatic (ammonia, transaminases) function; also screen for presence of alcohol and other toxins, and obtain blood cultures if infection is suspected. Arterial blood-gas analysis is helpful in pts with lung disease and acid-base disorders. Fever, especially with petechial rash, suggests meningitis. Examination of CSF is essential in diagnosis of meningitis and encephalitis; lumbar puncture should not be deferred if meningitis is a possibility, but CT scan should be obtained first to exclude a mass lesion. Empirical antibiotic and glucocorticoid coverage for meningitis may be instituted until CSF results are available. Fever with dry skin suggests heat shock or intoxication with anticholinergics. Hypothermia suggests myxedema, intoxication, sepsis, exposure, or hypoglycemia. Marked hypertension occurs with increased intracranial pressure (ICP) and hypertensive encephalopathy.
Focus on establishing pt’s best level of function and uncovering signs that enable a specific diagnosis. Comatose pt’s best motor and sensory function should be assessed by testing reflex responses to noxious stimuli; carefully note any asymmetric responses, which suggest a focal lesion. Multifocal myoclonus indicates that a metabolic disorder is likely; intermittent twitching may be the only sign of a seizure.
Stimuli of increasing intensity are applied to gauge the degree of unresponsiveness and any asymmetry in sensory or motor function. Motor responses may be purposeful or reflexive. Spontaneous flexion of elbows with leg extension, termed decortication, accompanies severe damage to contralateral hemisphere above midbrain. Internal rotation of the arms with extension of elbows, wrists, and legs, termed decerebration, suggests damage to midbrain or diencephalon. These postural reflexes occur in profound encephalopathic states.
In comatose pts, equal, round, reactive pupils exclude mid-brain damage as cause and suggest a metabolic abnormality. Pinpoint pupils occur in narcotic overdose (except meperidine, which can cause midsize pupils), pontine damage, hydrocephalus, or thalamic hemorrhage; the response to naloxone and presence of reflex eye movements (usually intact with drug overdose) can distinguish these. A unilateral, enlarged, often oval, poorly reactive pupil is caused by midbrain lesions or compression of third cranial nerve, as occurs in transtentorial herniation. Bilaterally dilated, unreactive pupils indicate severe bilateral midbrain damage, anticholinergic overdose, or ocular trauma.
Examine spontaneous and reflex eye movements. Intermittent horizontal divergence is common in drowsiness. Slow, to-and-fro horizontal movements suggest bihemispheric dysfunction. Conjugate eye deviation to one side indicates damage to the pons on the opposite side or a lesion in the frontal lobe on the same side (“The eyes look toward a hemispheral lesion and away from a brainstem lesion”). An adducted eye at rest with impaired ability to turn eye laterally indicates an abducens (VI) nerve palsy, common in raised ICP or pontine damage. The eye with a dilated, unreactive pupil is often abducted at rest and cannot adduct fully due to third nerve dysfunction, as occurs with transtentorial herniation. Vertical separation of ocular axes (skew deviation) occurs in pontine or cerebellar lesions. Doll’s head maneuver (oculocephalic reflex) and cold caloric–induced eye movements allow diagnosis of gaze or cranial nerve palsies in pts who do not move their eyes purposefully. Doll’s head maneuver is tested by observing eye movements in response to lateral rotation of head (this should not be performed in pts with possible neck injury); full conjugate movement of eyes occurs in bihemispheric dysfunction. In comatose pts with intact brainstem function, raising head to 60° above the horizontal and irrigating external auditory canal with cool water causes tonic deviation of gaze to side of irrigated ear (“cold calorics”). In conscious pts, it causes nystagmus, vertigo, and emesis.
Respiratory pattern may suggest site of neurologic damage. Cheyne-Stokes (periodic) breathing occurs in bihemispheric dysfunction and is common in metabolic encephalopathies. Respiratory patterns composed of gasps or other irregular breathing patterns are indicative of lower brainstem damage; such pts usually require intubation and ventilatory assistance.
Lesions causing raised ICP commonly cause impaired consciousness. CT or MRI scan of the brain is often abnormal in coma but may not be diagnostic; appropriate therapy should not be postponed while awaiting a CT or MRI scan. Pts with disordered consciousness due to high ICP can deteriorate rapidly; emergent CT study is necessary to confirm presence of mass effect and to guide surgical decompression. CT scan is normal in some pts with subarachnoid hemorrhage; the diagnosis then rests on clinical history combined with RBCs or xanthochromia in spinal fluid. CT, MR, or conventional angiography may be necessary to establish basilar artery stroke as cause of coma in pts with brainstem signs. The EEG is useful in metabolic or drug-induced states but is rarely diagnostic; exceptions are coma due to seizures or herpesvirus encephalitis.
This results from total cessation of cerebral function while somatic function is maintained by artificial means and the heart continues to pump. It is legally and ethically equivalent to cardiorespiratory death. The pt is unresponsive to all forms of stimulation (widespread cortical destruction), brainstem reflexes are absent (global brainstem damage), and there is complete apnea (destruction of the medulla). Demonstration of apnea requires that the Pco2 be high enough to stimulate respiration, while Po2 and bp are maintained. EEG is isoelectric at high gain. The absence of deep tendon reflexes is not required because the spinal cord may remain functional. Special care must be taken to exclude drug toxicity and hypothermia prior to making a diagnosis of brain death. Diagnosis should be made only if the state persists for some agreed-upon period, usually 6–24 h.

For a more detailed discussion, see Josephson SA, Miller BL: Confusion and Delirium, Chap. 25, p. 196, in HPIM-18. and Ropper AH: Coma, Chap. 274, p. 2247, in HPIM-18.