The most common tumor in women; 229,060 women in the United States have been diagnosed in 2012 and 40,000 died with breast cancer. Men also get breast cancer; F:M is 150:1. Breast cancer is hormone-dependent. Women with late menarche, early menopause, and first full-term pregnancy by age 18 have a significantly reduced risk. The average American woman has about a 1 in 9 lifetime risk of developing breast cancer. Dietary fat is a controversial risk factor. Oral contraceptives have little, if any, effect on risk and lower the risk of endometrial and ovarian cancer. Voluntary interruption of pregnancy does not increase risk. Estrogen replacement therapy may slightly increase the risk, but the beneficial effects of estrogen on quality of life, bone mineral density, and decreased risk of colorectal cancer appear to be somewhat outnumbered by increases in cardiovascular and thrombotic disease. Women who received therapeutic radiation before age 30 are at increased risk. Breast cancer risk is increased when a sister and mother also had the disease.
Perhaps 8–10% of breast cancer is familial. BRCA-1 mutations account for about 5%. BRCA-1 maps to chromosome 17q21 and appears to be involved in transcription-coupled DNA repair. Ashkenazi Jewish women have a 1% chance of having a common mutation (deletion of adenine and guanine at position 185). The BRCA-1 syndrome includes an increased risk of ovarian cancer in women and prostate cancer in men. BRCA-2 on chromosome 11 may account for 2–3% of breast cancer. Mutations are associated with an increased risk of breast cancer in men and women. Germ-line mutations in p53 (Li-Fraumeni syndrome) are very rare, but breast cancer, sarcomas, and other malignancies occur in such families. Germ-line mutations in hCHK2 and PTEN may account for some familial breast cancer. Sporadic breast cancers show many genetic alterations, including overexpression of HER2/neu in 25% of cases, p53 mutations in 40%, and loss of heterozygosity at other loci.
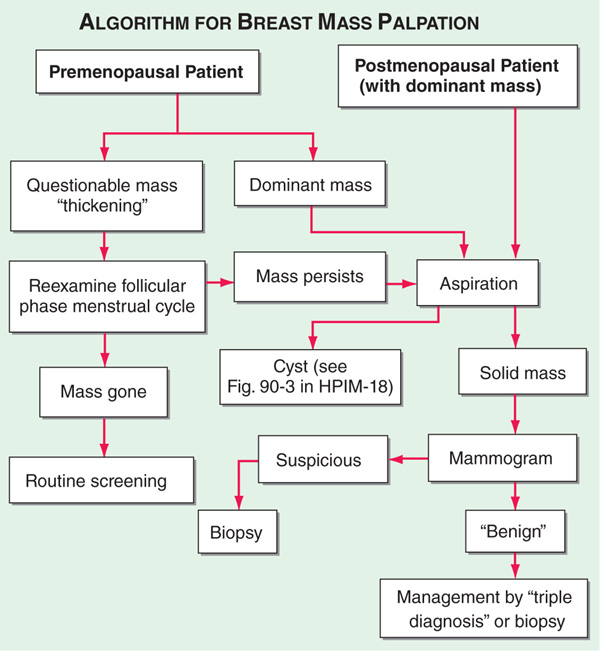
Breast cancer is usually diagnosed by biopsy of a nodule detected by mammogram or by palpation. Women should be strongly encouraged to examine their breasts monthly. In premenopausal women, questionable or nonsuspicious (small) masses should be reexamined in 2–4 weeks (Fig. 77-1). A mass in a premenopausal woman that persists throughout her cycle and any mass in a postmenopausal woman should be aspirated. If the mass is a cyst filled with non-bloody fluid that goes away with aspiration, the pt is returned to routine screening. If the cyst aspiration leaves a residual mass or reveals bloody fluid, the pt should have a mammogram and excisional biopsy. If the mass is solid, the pt should undergo a mammogram and excisional biopsy. Screening mammograms performed every other year beginning at age 50 have been shown to save lives. The controversy regarding screening mammograms beginning at age 40 relates to the following facts: (1) the disease is much less common in the 40-to 49-year age group, and screening is generally less successful for less common problems; (2) workup of mammographic abnormalities in the 40- to 49-year age group less commonly diagnoses cancer; and (3) about 50% of women who are screened annually during their forties have an abnormality at some point that requires a diagnostic procedure (usually a biopsy), yet very few evaluations reveal cancer. However, many believe in the value of screening mammography beginning at age 40. After 13–15 years of follow-up, women who start screening at age 40 have a small survival benefit. Women with familial breast cancer more often have false-negative mammograms. MRI is a better screening tool in these women.
FIGURE 77-1 Approach to a palpable breast mass.
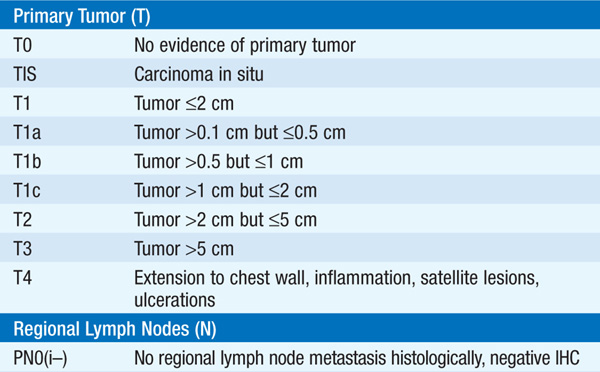
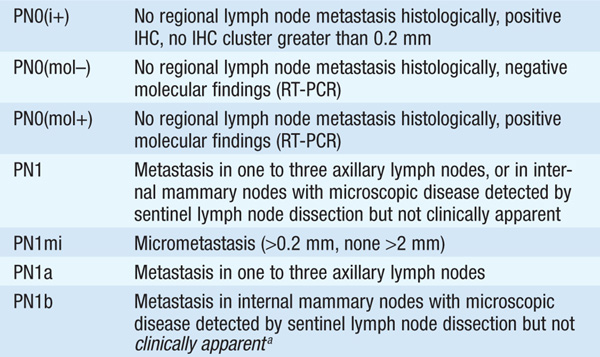
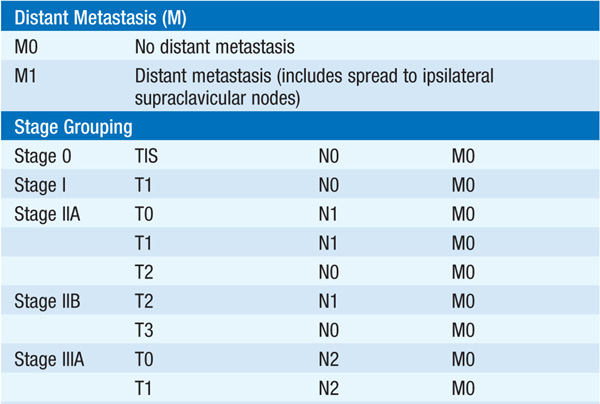
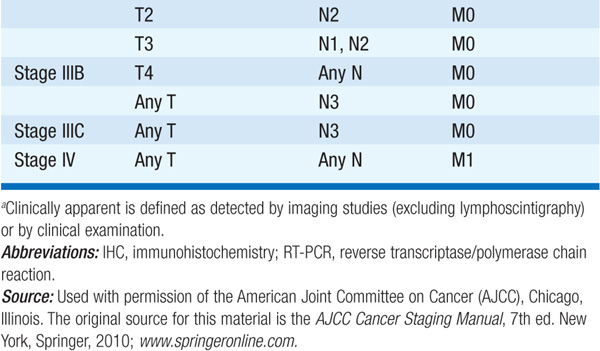
Therapy and prognosis are dictated by stage of disease (Table 77-1). Unless the breast mass is large or fixed to the chest wall, staging of the ipsilateral axilla is performed at the time of lumpectomy (see below). Within pts of a given stage, individual characteristics of the tumor may influence prognosis: expression of estrogen receptor improves prognosis, while overexpression of HER2/neu, mutations in p53, high growth fraction, and aneuploidy worsen the prognosis. Breast cancer can spread almost anywhere but commonly goes to bone, lungs, liver, soft tissue, and brain.
TABLE 77-1 STAGING OF BREAST CANCER

TREATMENT Breast Cancer
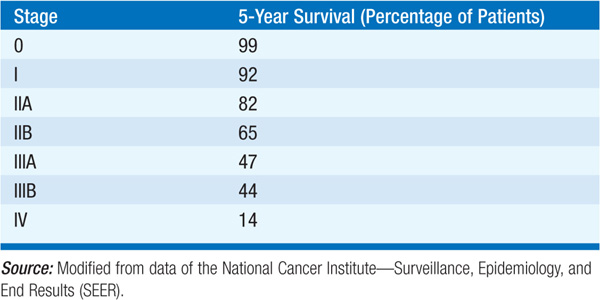
Five-year survival rate by stage is shown in Table 77-2. Treatment varies with stage of disease.
TABLE 77-2 5-YEAR SURVIVAL RATE FOR BREAST CANCER BY STAGE
Ductal carcinoma in situ is noninvasive tumor present in the breast ducts. Treatment of choice is wide excision with breast radiation therapy. In one study, adjuvant tamoxifen further reduced the risk of recurrence.
Invasive breast cancer can be classified as operable, locally advanced, and metastatic. In operable breast cancer, outcome of primary therapy is the same with modified radical mastectomy or lumpectomy followed by breast radiation therapy. Axillary dissection may be replaced with sentinel node biopsy to evaluate node involvement. The sentinel node is identified by injecting a dye in the tumor site at surgery; the first node in which dye appears is the sentinel node. Women with tumors <1 cm and negative axillary nodes require no additional therapy beyond their primary lumpectomy and breast radiation. Adjuvant combination chemotherapy for 6 months appears to benefit premenopausal women with positive lymph nodes, pre- and postmenopausal women with negative lymph nodes but with large tumors or poor prognostic features, and postmenopausal women with positive lymph nodes whose tumors do not express estrogen receptors. Estrogen receptor–positive tumors >1 cm with or without involvement of lymph nodes are treated with aromatase inhibitors. Women who began treatment with tamoxifen before aroma-tase inhibitors were approved should switch to an aromatase inhibitor after 5 years of tamoxifen and continue for another 5 years.
Adjuvant chemotherapy is added to hormonal therapy in estrogen receptor–positive, node-positive women and is used without hormonal therapy in estrogen receptor–negative node-positive women, whether they are pre- or postmenopausal. Various regimens have been used. The most effective regimen appears to be four cycles of doxorubicin, 60 mg/m2, plus cyclophosphamide, 600 mg/m2, IV on day 1 of each 3-week cycle followed by four cycles of paclitaxel, 175 mg/m2, by 3-h infusion on day 1 of each 3-week cycle. In women with HER2+ tumors, trastuzumab augments the ability of chemotherapy to prevent recurrence. The activity of other combinations is being explored. In premenopausal women, ovarian ablation [e.g., with the luteinizing hormone–releasing hormone (LHRH) inhibitor goserelin] may be as effective as adjuvant chemotherapy.
Tamoxifen adjuvant therapy (20 mg/d for 5 years) or an aromatase inhibitor (anastrozole, letrozole, exemestane) is used for postmenopausal women with tumors expressing estrogen receptors whose nodes are positive or whose nodes are negative but with large tumors or poor prognostic features. Breast cancer will recur in about half of pts with localized disease. High-dose adjuvant therapy with marrow support does not appear to benefit even women with high risk of recurrence.
Pts with locally advanced breast cancer benefit from neoadjuvant combination chemotherapy (e.g., CAF: cyclophosphamide 500 mg/m2, doxorubicin 50 mg/m2, and 5-fluorouracil 500 mg/m2 all given IV on days 1 and 8 of a monthly cycle for 6 cycles) followed by surgery plus breast radiation therapy.
Treatment for metastatic disease depends on estrogen receptor status and treatment philosophy. No therapy is known to cure pts with metastatic disease. Randomized trials do not show that the use of high-dose therapy with hematopoietic stem cell support improves survival. Median survival is about 16 months with conventional treatment: aromatase inhibitors for estrogen receptor–positive tumors and combination chemotherapy for receptor-negative tumors. Pts whose tumors express HER2/neu have higher response rates by adding trastuzumab (anti-HER2/neu) to chemotherapy. Some advocate sequential use of active single agents in the setting of metastatic disease. Active agents in anthracycline- and taxane-resistant disease include capecitabine, vinorelbine, gemcitabine, irinotecan, and platinum agents. Pts progressing on adjuvant tamoxifen may benefit from an aromatase inhibitor such as letrozole or anastrozole. Half of pts who respond to one endocrine therapy will respond to another. Bisphosphonates reduce skeletal complications and may promote antitumor effects of other therapy. Radiation therapy is useful for palliation of symptoms.
Women with breast cancer have a 0.5% per year risk of developing a second breast cancer. Women at increased risk of breast cancer can reduce their risk by 49% by taking tamoxifen for 5 years. Aromatase inhibitors are probably at least as effective as tamoxifen and are under study. Women with BRCA-1 mutations can reduce the risk by 90% with simple mastectomy.

For a more detailed discussion, see Lippman ME: Breast Cancer, Chap. 90, p. 754, in HPIM-18.