Tachyarrhythmias may appear in the presence or absence of structural heart disease; they are more serious in the former. Conditions that provoke arrhythmias include (1) myocardial ischemia, (2) heart failure, (3) hypoxemia, (4) hypercapnia, (5) hypotension, (6) electrolyte disturbances (e.g., hypokalemia and/or hypomagnesemia), (7) drug toxicity (digoxin, pharmacologic agents that prolong the QT interval), (8) caffeine consumption, (9) ethanol consumption.
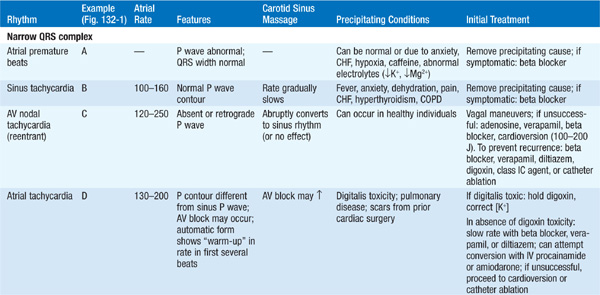
Examine ECG for evidence of ischemic changes (Chap. 120), prolonged or shortened QT interval, characteristics of Wolff-Parkinson-White (WPW) syndrome (see below), or ST elevation in leads V1–V3 typical of Brugada syndrome. See Fig. 132-1 and Table 132-1 for diagnosis of tachyarrhythmias; always identify atrial activity and relationship between P waves and QRS complexes. To aid the diagnosis:
TABLE 132-1 CLINICAL AND ELECTROCARDIOGRAPHIC FEATURES OF COMMON ARRHYTHMIAS
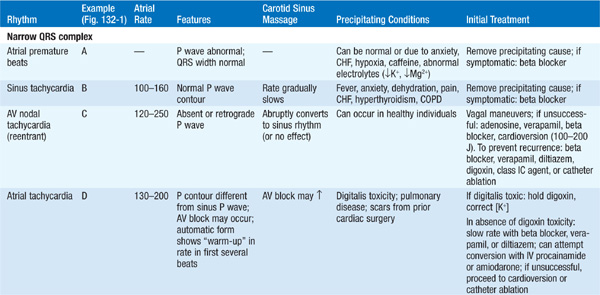
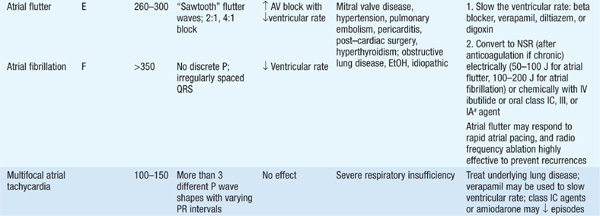
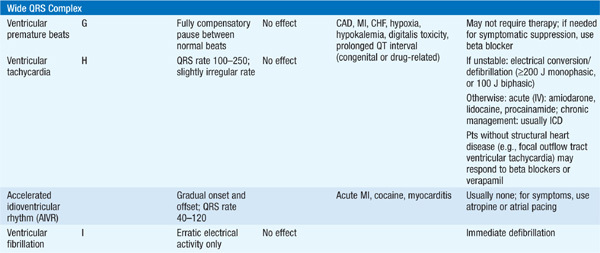
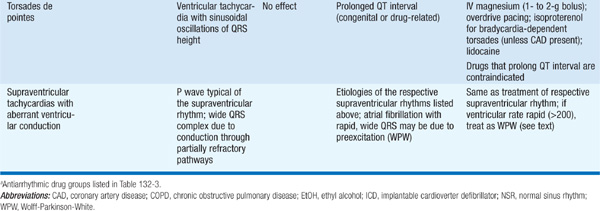
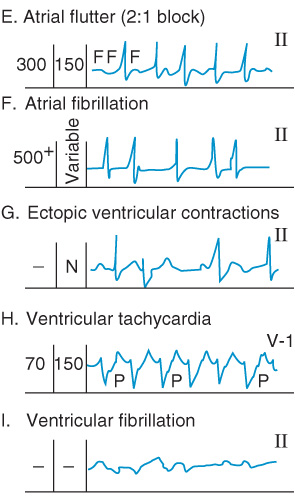
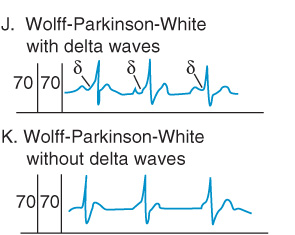
FIGURE 132-1 Tachyarrhythmias. (Modified from BE Sobel, E Braunwald: HPIM-9, p. 1052.)
• Obtain long rhythm strip of lead II, aVF, or V1. P waves can be made more evident by intentionally doubling the ECG voltage.
• Place accessory ECG leads (e.g., right-sided chest leads) to help identify P waves. Record ECG during carotid sinus massage (Table 132-1). Note: Do not massage both carotids simultaneously.
• For intermittent symptoms, consider 24-h Holter monitor (if symptoms occur daily), a pt-activated or continuously recording event monitor over 2–4 weeks, or, if symptoms are very infrequent but severely symptomatic, an implanted loop monitor. A standard exercise test may be used to provoke arrhythmias for diagnostic purposes.
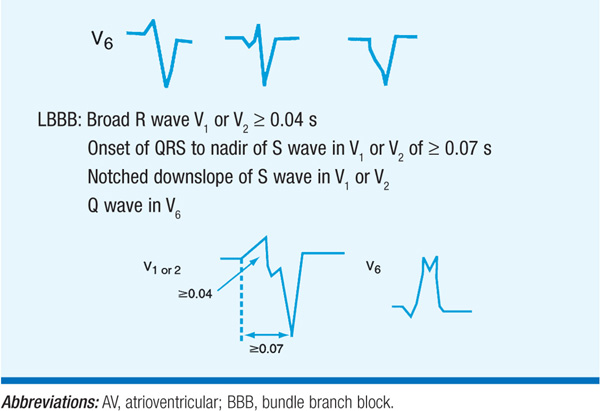
Tachyarrhythmias with wide QRS complex beats may represent ventricular tachycardia or supraventricular tachycardia with aberrant conduction. Factors favoring ventricular tachycardia include (1) AV dissociation, (2) QRS >0.14 s, (3) rightward and superior QRS axis, (4) no response to carotid sinus massage, (5) morphology of QRS unlike typical RBBB or LBBB, and similar to that of previous ventricular premature beats (Table 132-2).
TABLE 132-2 WIDE COMPLEX TACHYCARDIA
TREATMENT Tachyarrhythmias (Tables 132-1 and 132-3)
Precipitating causes (listed above) should be corrected. If pt is hemo-dynamically compromised (angina, hypotension, CHF), proceed to immediate cardioversion.
Do not cardiovert sinus tachycardia; exercise caution if digitalis toxicity is suspected. Initiate drugs as indicated in the tables; follow ECG intervals (esp. QRS and QT). Reduce dosage for pts with hepatic or renal dysfunction as indicated in Table 132-3. Drug efficacy is confirmed by ECG (or Holter) monitoring, stress testing, and, in special circumstances, invasive electrophysiologic study.
TABLE 132-3 ANTIARRHYTHMIC DRUGS
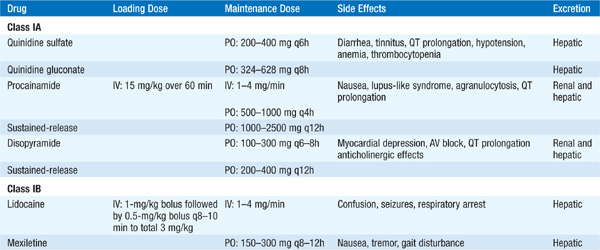
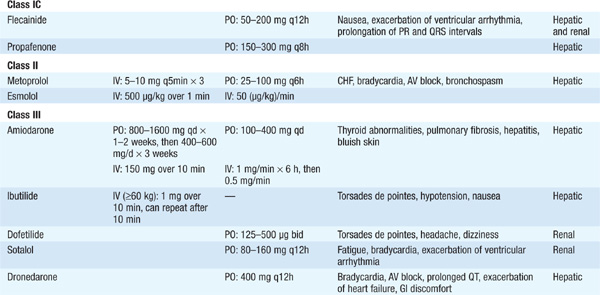
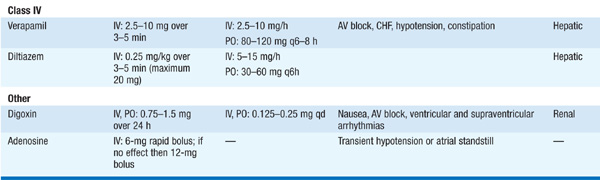
Antiarrhythmic agents all have potential toxic side effects, including provocation of ventricular arrhythmias, esp. in pts with LV dysfunction or history of sustained ventricular arrhythmias. Drug-induced QT prolongation and associated torsades de pointes ventricular tachycardia (Table 132-1) is most common with class IA and III agents; the drug should be discontinued if the QTc interval (QT divided by square root of RR interval) increases by >25%. Antiarrhythmic drugs should be avoided in pts with asymptomatic ventricular arrhythmias after MI, since mortality risk increases.
CHRONIC ATRIAL FIBRILLATION (AF) Evaluate potential underlying cause (e.g., thyrotoxicosis, mitral stenosis, excessive ethanol consumption, pulmonary embolism). Pts with risk factors for stroke (e.g., rheumatic mitral valve disease, history of cerebrovascular accident or transient ischemic attack, hypertension, diabetes, heart failure, age >75, left atrial diameter >5.0 cm) should receive anticoagulation with either warfarin (INR 2.0–3.0) or, for AF not associated with valvular disease, newer agents that do not require prothrombin time monitoring—e.g., dabigatran 150 mg bid [75 mg bid for creatinine clearance (CrCl) 30–50 mL/min; avoid if CrCl <30] or rivaroxaban 20 mg daily with the evening meal (15 mg daily for CrCl 15–50 mL/min; avoid if CrCl <15). Substitute aspirin, 325 mg/d, for pts without these risk factors or if contraindication to systemic anticoagulation exists.
Control ventricular rate (60–80 beats/min at rest, <100 beats/min with mild exercise) with beta blocker, calcium channel blocker (vera-pamil, diltiazem), or digoxin.
Consider cardioversion (100–200 J) after ≥3 weeks therapeutic anticoagulation, or acutely if no evidence of left atrial thrombus by transesophageal echo, especially if symptomatic despite rate control. Initiation of class IC, III, or IA agents prior to electrical cardioversion facilitates maintenance of sinus rhythm after successful procedure. Class IC (Table 132-3) drugs are preferred in pts without structural heart disease, and class III drugs are recommended in presence of left ventricular dysfunction or coronary artery disease (Fig. 132-2). Anticoagulation should be continued for a minimum of 3 weeks after successful cardioversion.
Catheter-based ablation (pulmonary vein isolation) can be considered for recurrent symptomatic AF refractory to pharmacologic measures.
Conduction occurs through an accessory pathway between atria and ventricles. Baseline ECG typically shows a short PR interval and slurred upstroke of the QRS (“delta” wave) (Fig. 132-1J). Associated tachyarrhythmias are of two types:
• Narrow QRS complex tachycardia (antegrade conduction through AV node). Treat cautiously with IV adenosine or beta blocker, verapamil, or diltiazem (Table 132-2).
FIGURE 132-2 Recommendations for the selection of antiarrhythmic medications to prevent the recurrence of atrial fibrillation. See Table 132-3 for definition of class IA and IC drugs. An atrioventricular nodal blocking agent (i.e., beta blocker, calcium channel blocker, or digoxin) should be added to all class IC and IA agents as well as to dofetilide. LVEF, left ventricular ejection fraction; CHF, congestive heart failure; CAD, coronary artery disease; EF, ejection fraction.
• Wide QRS complex tachycardia (antegrade conduction through accessory pathway); may also be associated with AF with a very rapid (>250/min) ventricular rate, which can degenerate into VF. If hemodynamically compromised, immediate cardioversion is indicated; otherwise, treat with IV procainamide or ibutilide (Table 132-3), not digoxin, beta blocker, or verapamil.
Consider catheter ablation of accessory pathway for long-term prevention.

For a more detailed discussion, see Marchlinski F: The Tachyarrhythmias, Chap. 233, p. 1878, in HPIM-18.