Four major classes are commonly used in adults: (1) antidepressants, (2) anxiolytics, (3) antipsychotics, and (4) mood stabilizing agents. Nonpsychiatric physicians should become familiar with one or two drugs in each of the first three classes so that the indications, dose range, efficacy, potential side effects, and interactions with other medications are well known.
1. Most treatment failures are due to undermedication and impatience. For a proper medication trial to take place, an effective dose must be taken for an adequate amount of time. For antidepressants, antipsychotics, and mood stabilizers, full effects may take weeks or months to occur.
2. History of a positive response to a medication usually indicates that a response to the same drug will occur again. A family history of a positive response to a specific medication is also useful.
3. Pts who fail to respond to one drug will often respond to another in the same class; one should attempt another trial with a drug that has a different mechanism of action or a different chemical structure. Treatment failures should be referred to a psychiatrist, as should all pts with psychotic symptoms or who require mood stabilizers.
4. Avoid polypharmacy; a pt who is not responding to standard mono-therapy requires referral to a psychiatrist.
5. Pharmacokinetics may be altered in the elderly, with smaller volumes of distribution, reduced renal and hepatic clearance, longer biologic half-lives, and greater potential for CNS toxicity. The rule with elderly pts is to “start low and go slow.”
6. Never stop treatment abruptly; especially true for antidepressants and anxiolytics. In general, medications should be slowly tapered and discontinued over 2–4 weeks.
7. Review possible side effects each time a drug is prescribed; educate pts and family members about side effects and need for patience in awaiting a response.
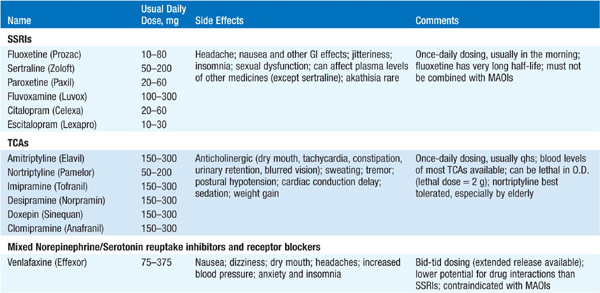
Useful to group according to known actions on CNS monoaminergic systems (Table 209-1). The selective serotonin reuptake inhibitors (SSRIs) have predominant effects on serotonergic neurotransmission, also reflected in side-effect profile. The TCAs, or tricyclic antidepressants, affect noradrenergic and, to a lesser extent, serotonergic neurotransmission but also have anticholinergic and antihistaminic effects. Venlafaxine, desvenlafaxine, duloxetine, and mirtazapine have mixed noradrenergic and serotonergic effects. Bupropion is a novel antidepressant that enhances noradrenergic function. Trazodone, nefazodone, and amoxapine have mixed effects on serotonin receptors and on other neurotransmitter systems. The MAOIs inhibit monoamine oxidase, the primary enzyme responsible for the degradation of monoamines in the synaptic cleft.
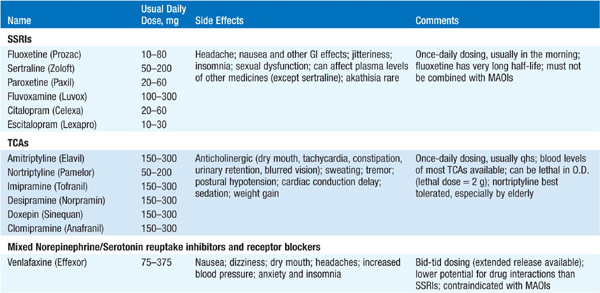
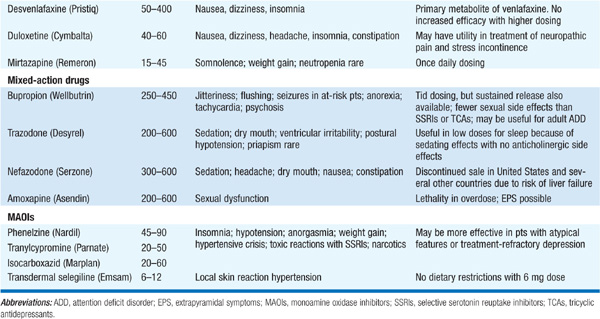
ADs are effective against major depression, particularly when neuro-vegetative symptoms and signs are present. Despite the widespread use of SSRIs, there is no convincing evidence that they are more efficacious than TCAs, although their safety profile in overdose is more favorable than that of the TCAs. ADs are also useful in treatment of panic disorder, post-traumatic stress disorder, chronic pain syndromes, and generalized anxiety disorder. The TCA clomipramine and the SSRIs successfully treat obsessive-compulsive disorder.
All ADs require at least 2 weeks at a therapeutic dose before clinical improvement is observed. All ADs also have the potential to trigger a manic episode or rapid cycling when given to a pt with bipolar disorder. The MAOIs must not be prescribed concurrently with other ADs or with narcotics, as potentially fatal reactions may occur. “Withdrawal syndromes” usually consisting of malaise can occur when ADs are stopped abruptly.
Benzodiazepines bind to sites on the γ-aminobutyric acid receptor and are cross-tolerant with alcohol and with barbiturates. Four clinical properties: (1) sedative, (2) anxiolytic, (3) skeletal muscle relaxant, and (4) antiepileptic. Individual drugs differ in terms of potency, onset of action, duration of action (related to half-life and presence of active metabolites), and metabolism (Table 209-2). Benzodiazepines have additive effects with alcohol; like alcohol, they can produce tolerance and physiologic dependence, with serious withdrawal syndromes (tremors, seizures, delirium, and autonomic hyper-activity) if discontinued too quickly, especially for those with short half-lives.
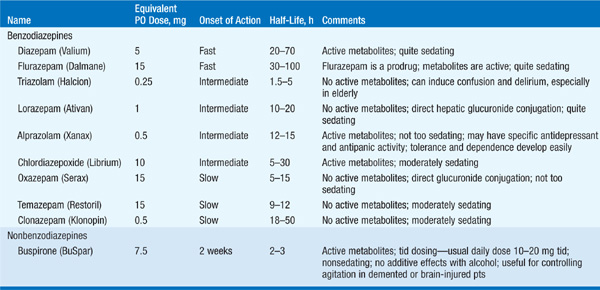
Buspirone is a nonbenzodiazepine anxiolytic that is nonsedating, is not cross-tolerant with alcohol, and does not induce tolerance or dependence. It requires at least 2 weeks at therapeutic doses to achieve full effects.
These include the first-generation (typical) neuroleptics, which act by blocking dopamine D2 receptors, and the second-generation (atypical) neuroleptics, which act on dopamine, serotonin, and other neurotransmitter systems. Some antipsychotic effect may occur within hours or days of initiating treatment, but full effects usually require 6 weeks to several months of daily, therapeutic dosing.
Useful to group into high-, mid-, and low-potency neuroleptics (Table 209-3). High-potency neuroleptics are least sedating, have almost no anticholinergic side effects, and have a strong tendency to induce extrapyramidal side effects (EPSEs). The EPSEs occur within several hours to several weeks of beginning treatment and include acute dystonias, akathisia, and pseudo-parkinsonism. Extrapyramidal symptoms respond well to trihexyphenidyl, 2 mg twice daily, or benztropine mesylate, 1 to 2 mg twice daily. Akathisia may respond to beta blockers. Low-potency neuroleptics are very sedating, may cause orthostatic hypotension, are anticholinergic, and tend not to induce EPSEs frequently.
TABLE 209-3 ANTIPSYCHOTIC AGENTS


Up to 20% of pts treated with conventional antipsychotic agents for >1 year develop tardive dyskinesia (probably due to dopamine receptor supersensitivity), an abnormal involuntary movement disorder most often observed in the face and distal extremities. Treatment includes gradual withdrawal of the neuroleptic, with possible switch to a novel neuroleptic; anticholinergic agents can worsen the disorder.
Rarely, pts exposed to neuroleptics develop neuroleptic malignant syndrome (NMS), a life-threatening complication with a mortality rate as high as 25%; hyperpyrexia, autonomic hyperactivity, muscle rigidity, obtundation, and agitation are characteristic, associated with increased WBC, increased creatine phosphokinase, and myoglobinuria. Treatment involves immediate discontinuation of neuroleptics, supportive care, and use of dantrolene and bromocriptine.
A new class of agents that has become the first line of treatment (Table 209-3); efficacious in treatment-resistant pts, tend not to induce EPSEs or tardive dyskinesia, and appear to have uniquely beneficial properties on negative symptoms and cognitive dysfunction. Main problem is side effect of weight gain (most prominent in clozapine and in olanzapine; can induce diabetes). The CATIE study, a large-scale investigation of antipsychotic agents in the “real world,” revealed a high rate of discontinuation of all medications over 18 months; olanzapine was modestly more effective than other agents but with a higher discontinuation rate due to side effects.
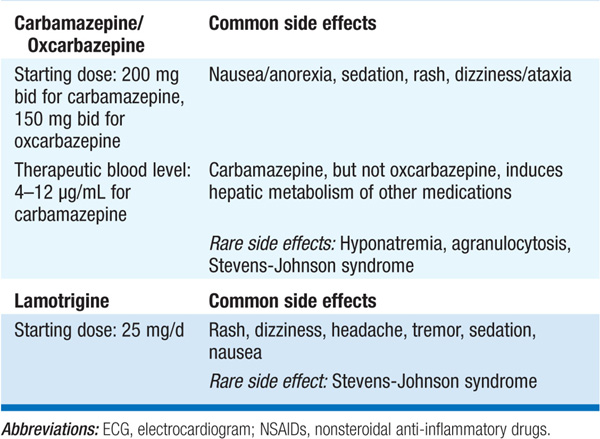
Four mood stabilizers in common use: lithium, valproic acid, carbamazepine/oxcarbazepine, and lamotrigine (Table 209-4). Lithium is the gold standard and the best studied, and along with carbamazepine and valproic acid, is used for treatment of acute manic episodes; 1–2 weeks to reach full effect. As prophylaxis, the mood stabilizers reduce frequency and severity of both manic and depressed episodes in cyclical mood disorders. In refractory bipolar disorder, combinations of mood stabilizers may be beneficial.
TABLE 209-4 CLINICAL PHARMACOLOGY OF MOOD STABILIZERS