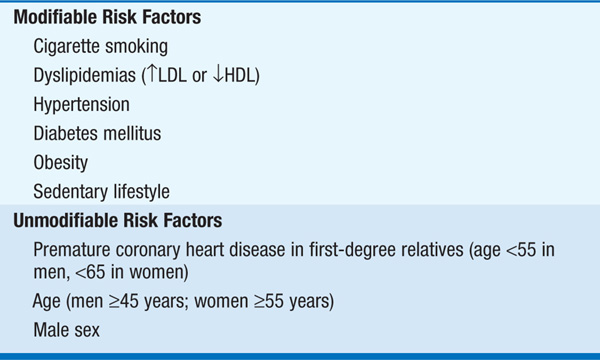
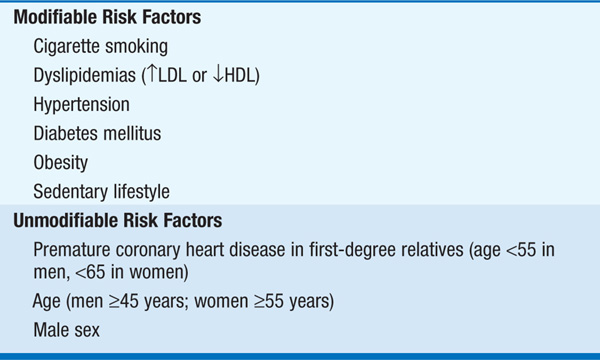
Cardiovascular disease is the leading cause of death in developed nations; prevention is targeted at modifiable atherosclerosis risk factors (Table 215-1). Identification and control of these attributes reduce subsequent cardiovascular event rates.
TABLE 215-1 ESTABLISHED ATHEROSCLEROTIC RISK FACTORS
Cigarette smoking increases the incidence of, and mortality associated with, coronary heart disease (CHD). Observational studies show that smoking cessation reduces excess risk of coronary events within months; after 3–5 years, the risk falls to that of individuals who never smoked. Pts should be asked regularly about tobacco use, followed by counseling and, as needed, antismoking pharmacologic therapy to assist cessation.
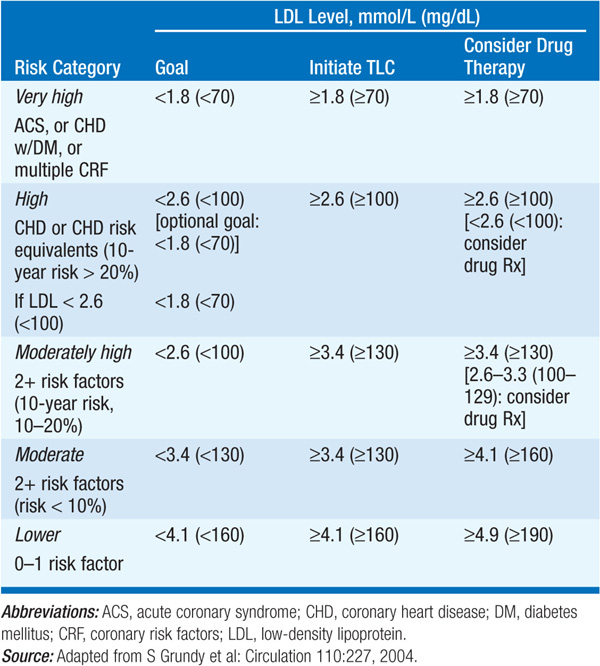
(See Chap. 189) Both elevated LDL and low HDL cholesterol are associated with cardiovascular events. Each 1-mg/dL increase in serum LDL correlates with a 2–3% rise in CHD risk; each 1-mg/dL decrease in HDL heightens risk by 3–4%. ATP III guidelines advise a fasting lipid profile [total cholesterol, triglycerides, HDL, LDL (calculated or directly measured)] in all adults, repeated every 5 years. Recommended dietary and/or pharmacologic approach depends on presence or risk of coronary artery disease (CAD) and the LDL level (Table 215-2); treatment should be most aggressive in pts with established CAD and in those with “equivalent risk” (e.g., presence of peripheral arterial disease or diabetes mellitus). Drug therapy is indicated when LDL level exceeds goal in Table 215-2 by 30 mg/dL (0.8 mmol/L). If elevated triglyceride level [>200 mg/dL (> 2.6 mmol/L)] persists after control of LDL, secondary goal is to achieve non-HDL level (calculated as total cholesterol minus HDL) ≤30 mg/dL (0.8 mmol/L) above the target values listed in Table 215-2. In pts with isolated low HDL, encourage beneficial lifestyle measures: smoking cessation, weight loss, and increased physical activity. Consider addition of fibric acid derivative or niacin to raise HDL in pts with established CAD (see Chap. 189).
TABLE 215-2 LDL CHOLESTEROL GOALS AND CUTPOINTS FOR THERAPEUTIC LIFESTYLE CHANGES (TLC) AND DRUG THERAPY IN DIFFERENT RISK CATEGORIES
(See Chap. 126) Systolic or diastolic bp > “optimal” level of 115/75 mmHg is associated with increased risk of cardiovascular disease; each augmentation of 20 mmHg systolic, or 10 mmHg diastolic, above this value doubles the risk. Treatment of elevated blood pressure reduces the rate of stroke, congestive heart failure, and CHD events, with general goal of bp <140/85 mmHg or <130/80 in pts with diabetes or chronic kidney disease. Cardiovascular event rates in elderly pts with isolated systolic hypertension (systolic ≥140 but diastolic <90) are also reduced by antihypertensive therapy.
See Chap. 126 for antihypertensive treatment recommendations. Pts with “prehypertension” (systolic bp 120–139 mmHg or diastolic bp 80–89 mmHg) should receive counseling about beneficial lifestyle modifications such as those listed below (e.g., low-fat diet replete with vegetables and fruit, weight loss if overweight, increased physical activity, reduction of excessive alcohol consumption).
(See Chaps. 127 and 184) Pts with diabetes most often succumb to cardiovascular disease. LDL levels are typically near average in diabetic pts, but LDL particles are smaller, denser, and more atherogenic; low HDL and elevated triglyceride levels are common. Tight control of serum glucose in type 2 diabetics reduces microvascular diabetic complications (retinopathy, renal disease), but a decrease in macrovascular events (CAD, stroke) has not been shown. Conversely, successful management of associated risk factors in diabetics (e.g., dyslipidemia and hypertension) does reduce cardiovascular events and should be vigorously pursued. Antilipidemic (i.e., statin) therapy should be used to lower LDL to <100 mg/dL in diabetics, even if pt has no symptoms of CAD.
Individuals without overt diabetes but who have “metabolic syndrome” (constellation of insulin resistance, central obesity, hypertension, hypertriglyceridemia, low HDL—see Chap. 127) are also at high risk of cardiovascular events. Dietary counseling, weight loss, and increased physical activity are important in reducing the prevalence of this syndrome.
Coronary risk is greater in men compared to that of premenopausal women of same age, but female risk accelerates after menopause. Estrogen-replacement therapy lowers LDL and raises HDL in postmenopausal women and in observational studies has been associated with reduced coronary events. However, prospective clinical trials do not support such a benefit and hormone-replacement therapy should not be prescribed for the purpose of cardiovascular risk reduction, especially in older women.
May be assessed selectively in pts without above traditional risk factors who have premature vascular disease or strong family history of premature vascular disease.
There is a graded correlation between serum homocysteine levels and risk of cardiovascular events and stroke. Supplemental folic acid and other B vitamins lower serum levels, but prospective clinical trials have not shown that such therapy reduces cardiac events.
Inflammatory serum markers, such as high-sensitivity C-reactive protein (CRP), correlate with the risk of coronary events. CRP prospectively predicts risk of MI and outcomes after acute coronary syndromes; its usefulness and role in prevention as an independent risk factor is currently being defined.
Potential benefits of assessing other emerging risk factors [e.g., lipoprotein(a), fibrinogen] remain unproven and controversial.
Thrombosis at the site of disrupted atherosclerotic plaque is the most common cause of acute coronary events. In primary prevention trials, chronic low-dose aspirin therapy has reduced the risk of a first MI in men and the risk of stroke in women. The American Heart Association recommends aspirin (75–160 mg daily) for men and women who are at high cardiovascular risk (i.e., by Framingham Study criteria, for men with ≥10% 10-year risk, or women with ≥20% 10-year risk).
Encourage beneficial exercise habits (>30 min moderate intensity physical activity daily) and sensible diet (low in saturated and trans fat; 2–3 servings of fish/week to ensure adequate intake of omega-3 fatty acids; balance caloric consumption with energy expenditure). Advise moderation in ethanol intake (no more than 1–2 drinks/day).

For a more detailed discussion, see Libby P: The Pathogenesis, Prevention, and Treatment of Atherosclerosis, Chap. 241, p. 1983; Gaziano TA and Gaziano JM: Epidemiology of Cardiovascular Disease, Chap. 225, p. 1811; and Martin GJ: Screening and Prevention of Disease, Chap. 4, p. 29; in HPIM-18.