13
INTEGRATION OF THE SCIENCES BASIC TO MEDICINE AND THE WHOLE OF THE CURRICULUM
Stewart Mennin
A number of programmes have successfully brought together the sciences basic to medicine and clinical practice.
Integration is a keystone in the arc of medical education that warrants a much deeper understanding of its interdependence with the purpose and function of the curriculum. As Beane (1997) notes in the following quotation, claims are often made of integrated curriculum.
(Beane 1997: 2)
What works for the integration of the sciences basic to medicine1 and the whole curriculum has been, is now, and will continue to be challenging as new information, ideas, experiences and approaches to learning emerge. Integration in the present context refers to the interactions, exchanges and interrelationships that unify different subjects and objects forming a whole. The perception of the ‘whole’ is relative to the scale at which observations and measurements occur. The whole that comes from curriculum integration exists, and is co-embedded at multiple levels of an even larger and greater whole. This chapter argues that an awareness of different levels of integration, the whole (e.g. the curriculum), the part (e.g. individual learners, patients and teachers) and the greater whole (the university, the health system and the well-being of society), is fundamental for the emergence of an ecology of medical education that fulfils its social contract with society. Integration of the sciences basic to medicine and the whole involves complex interrelationships that necessarily function within and across constraints that serve to organise, liberate and optimise a self-organising, learning curriculum. Integration occurs within, and as a consequence of, conditions and constraints that are a variable consequence of the circumstances. It is the author’s contention that it is the qualities of sensitivity and adaptive responsiveness to variations in local conditions that produce a coherent sustainable adaptive whole, i.e. fit for function.
The present chapter begins with a view of integration expressed in terms of the recent history of medical education. The focus then turns to the ability of integration of the sciences basic to medicine to exist at many levels of curriculum and the organisation. Finally, a perspective view of an adaptive integrated curriculum is considered that can be relevant to the needs of society while conditions and problems continue to evolve and change (Doll 1993; Beane 1997; Fogarty and Pete 2009; Mennin 2010a; Bleakley et al. 2011; Patterson et al. 2013).
Integration: where are we and how did we get here?
The story of the integration of the sciences basic to medicine with the whole of the medical curriculum is one of episodic evolution of new concepts, pedagogies, methods and technologies at every level (Papa and Harasym 1999). Over 100 years ago Flexner sought to bring together and integrate research in the basic sciences with hospital-based care to reconstitute the whole of medical education with the basic sciences taught separately as a necessary prerequisite to clinical studies (Flexner 1910). Over 40 years later, Case Western Reserve University, USA, loosened the constraints on single-subject-specific curricula by integrating (co-mingling) the basic science disciplines within patterns of organ systems (Patterson 1956). McMaster University, Canada, went even further in the mid-1960s, significantly reducing the constraints on curriculum integration using ‘authentic’ clinical cases in small-group, problem-based learning (PBL) tutorials promoting integration and relevance among and across the basic and clinical sciences (Neufeld and Barrows 1974). The primary driving force for learning in their PBL approach was the ‘need to know’, derived from students’ systematic inquiry and questions created by them at the frontier of their understanding in the context of a particular problem (Barrows and Tamblyn 1980; Schmidt 1993). PBL popularised and made accessible the integration of self-directed ‘independent’ study, collective elaboration and the reflective application of what was being learned to ‘more realistic’ problems; initially in the sciences basic to medicine and later in the greater whole of health professions education and beyond. It also promoted greater collective accountability for what and how sense making occurred in small-group learning and cleared the way for the emergence of increased reflection, feedback and formative assessment in medical education. Small-group, problem-oriented learning promoted more equity in the curriculum for areas such as professionalism, ethics and communication, among others. Maastricht University, the Netherlands, since the early 1980s, has had a major integrative role nationally and internationally, promoting the development of research in medical education and the dissemination of PBL (van der Vleuten et al. 2004; Mennin 2010b). The University of New Mexico (USA) School of Medicine’s parallel curriculum track, the Primary Care Curriculum (1979–94), further decreased constraints on the teaching and learning of the sciences basic to medicine by integrating community-oriented learning and PBL together, focusing on early and sustained clinical skills as the nidus around which the sciences basic to medicine, community-oriented learning, clinical experiences and PBL were oriented (Kaufman 1985; Kaufman et al. 1989). A focus on the whole, the part and the greater whole was further strengthened by the publication of two reports by the Association of American Medical Colleges (AAMC) General Professional Education of the Physician (GPEP) (AAMC 1984) and Assessing Change in Medical Education – The Road to Implementation (ACME-Tri) (Anderson and Swanson 1993), and the adoption of the General Medical Council’s (GMC’s) Tomorrow’s Doctors (GMC 2003, 2009) and ‘the Scottish doctor’ (Simpson et al. 2002).
Significantly, a loosening of constraints around the concept and purpose of assessment brought a greater emphasis on formative assessment as integrative and co-embedded with learning (Schuwirth and van der Vleuten 2006; Hodges 2013). The rise of portfolio assessment as part of learning further integrated and legitimised narrative and qualitative perspectives in the lexicon of curriculum and research in medical education (Friedman Ben-David et al. 2001). Progress testing deepened the temporal dimensions of assessment and integration in medical education (Wrigley et al. 2012).
Many other significant integrative advances in medical education included the classification of knowledge into hierarchies and sequences from least to most complex, with workplace authenticity being defined as the greater whole (Bloom et al. 1956; Miller 1990). The advent of simulated and standardised patients (Stillman et al. 1986; Barrows et al. 1987) and the explosion of technologies for low- and high-tech simulation fostered the integration of clinical skills, clinical care, assessment and the sciences basic to medicine in ways not previously possible (Motola et al. 2013).
The relatively recent emphasis on outcomes and competency-based curricula is influencing medical education by integrating the emphasis on the process of learning with clearly defined and measurable learning outcomes (Harden et al. 1999; Morcke et al. 2013). The rise of interest in ethics, professionalism and communication, among other complex capabilities, required integration with the whole of the curriculum, including the basic sciences (Epstein and Hundert 2002; Stepien and Baerstein 2006; O’Sullivan et al. 2012). Sustained clinical and community experiences were recognised as authentic opportunities for the integration of the sciences basic to medicine across a wide spectrum of healthcare and workplace scenarios. Assessment and learning in the workplace extended our experiences and ideas of how the whole of integrated learning looked (Norcini and Burch 2007).
Longitudinal integrated clerkships decreased the constraints on clinical education, breaking new ground in what had previously been clerkship-dominated specialties, taught separately and sequentially. Entrustable professional activities (EPA) established the capacity for mutual interrelated responsibility and accountability (integration) in the clinical setting with high degrees of freedom for the learner and preceptor, further decreasing the constraints on the concept of curriculum and medical education (Worley et al. 2000; ten Cate 2005).
What’s next for integration in medical education? It’s not possible to predict. It does seem clear that ‘what works,’ and what will continue to work in the future, requires an increased awareness, recognition, acceptance and understanding of the role of constraints on the dynamics of the interrelationships among educational activities, programmes, curricula and practices. Current trends in medical education towards earlier authentic learning experiences change the fundamental nature of learning as the problems and issues selected as learning activities become more immediately meaningful for learners both in the here and now and in their future careers.
In summary, the evolution of contemporary medical education has been marked by a progressive decrease of constraints (conversely, a progressive increase in the degrees of freedom) around how the sciences basic to medicine fit with the whole of the curriculum, and a progressive revision of how the whole of medical education has been perceived, understood and influenced during the last 50 years. The organisation of curriculum activities based on real-life problems that involve the learners in the here and now, rather than learning something that will be useful at some time in the future, is a fundamental change that has enhanced meaningful and coherent integration necessary for capacity building (Beane 1997).
The landscape of curriculum integration
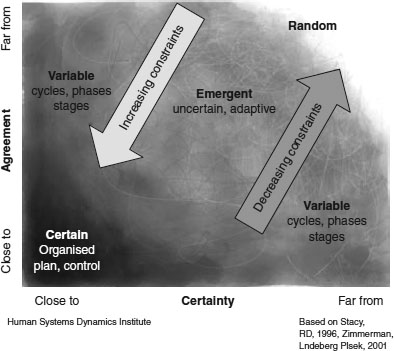
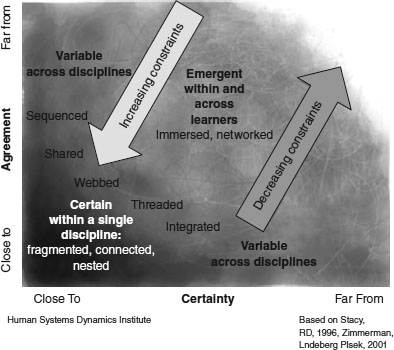
How to make sense of changes in curriculum integration in the face of varying degrees of freedom and constraints? The adaptive action landscape diagram (Figure 13.1) is one way to visualise relationships and interactions in a complex environment (Kauffman 1993). It has been widely adopted in the field of leadership, organisational development and adaptive action (Stacy 1996; Zimmerman et al. 2001; Eoyang and Holladay 2013) and more recently in education (Patterson et al. 2013) and curriculum integration.
The horizontal (x) axis in Figure 13.1 is the degree of certainty in any system (e.g. curriculum) along a continuum from close to certainty on the left to far from certainty on the right. The closer to certainty, the more predictable, stable and controllable are the patterns of connections, interactions and teaching, assessing and integration in the curriculum. The further from certainty, the greater the unpredictability and the weaker and more short-lived are the patterns of connections and integration in the curriculum. For example, vaccine production and use, pacemakers and insulin pumps have to be very stable, accurate, reproducible and predictable. High-stakes assessments are highly constrained and need to be accurate, reliable and controlled.
By contrast, far from certainty is privileged when what has worked in the past isn’t working now; when expertise is not useful and when you’re stuck and not sure what to do. Under these conditions, creativity, innovation and educated trial and error with reflection and feedback are fit for function. Integrated curricula with low constraints (far from certainty) accumulate tension and are sensitive and responsive to small changes in the environment that affect learning, integration and the curriculum. Examples are found in entrustable activities for residents (ten Cate 2005), longitudinal clerkships (Worley et al. 2000) and community-based medical education (Mennin and Petroni-Mennin 2006).
The vertical (y) axis in Figure 13.1 represents agreement in a curriculum (system) along a continuum from close to agreement to far from agreement. When teachers and students are close to agreement, things are predictable; there is a strong similarity in ways that teachers and students respond to challenges and stimulation. Clearly defined specific objectives and outcomes indicate to both students and teachers exactly what to expect. Close to agreement, disagreements are minimised. When a system is far from agreement, everyone does their own thing; there is little to no coordination and agreement among teachers and students; satisfaction with and productivity of the learning environment are low. Here one finds a large gap between what is taught, assessed and actually done in practice (Hafferty 1998).
The sciences basic to medicine: day-to-day integration within a phase of a curriculum
A coherent curriculum is one in which the patterns of practice and understanding present across the whole of any given education programme are similar, without losing the richness of difference at the same time (Eoyang and Holladay 2013). Four case studies from medical schools in Malaysia, Argentina, Saudi Arabia and the USA respectively illustrate how integration of the sciences basic to medicine are shaped by constraints at different levels of the whole. The case studies also illustrate and reinforce the organising effect of constraints on the interrelationships of different elements, parts and subjects, and how they combine and coordinate to form a more complete, harmonious and emergent whole (Beane 1997; Harden 2000; Fogarty and Pete 2009; Mennin 2010a; Eoyang and Holladay 2013).
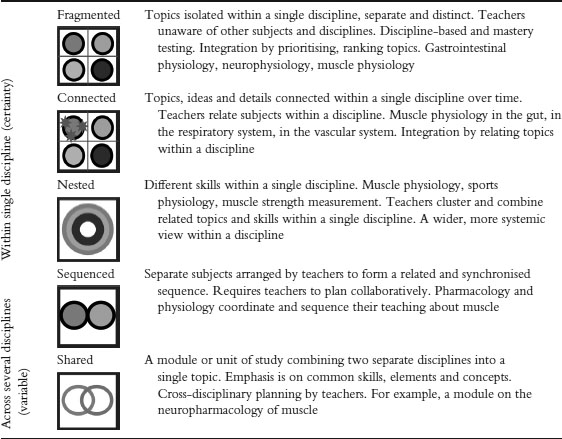
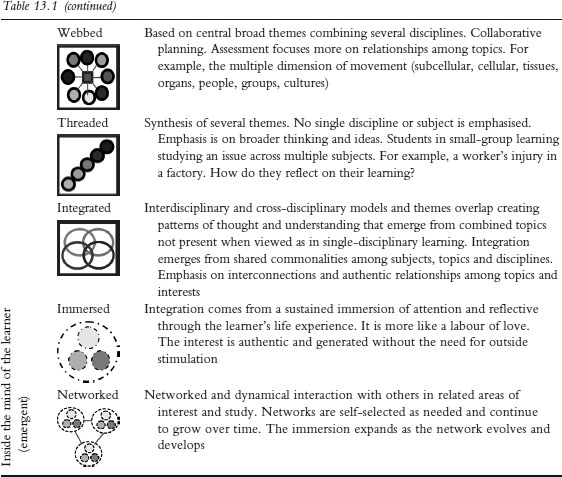
The organisational framework for the discussion of the case studies is based on and adapted from the work of Beane (1997), Fogarty (1991), Fogarty and Pete (2009) and Harden (2000). Fogarty’s classic work proposed three dimensions of curriculum integration: (1) within a single discipline; (2) across disciplines; and (3) within and across learners; and ten models of integration within the three dimensions (Fogarty and Pete 2009) (Table 13.1). The reader is referred to these authors for a more indepth explanation of the models.
The first case study focuses on integration within a single discipline, anatomy.
Table 13.1 Summary of three domains (within a single discipline, across several disciplines and inside the mind of the learner) and ten models of curriculum integration
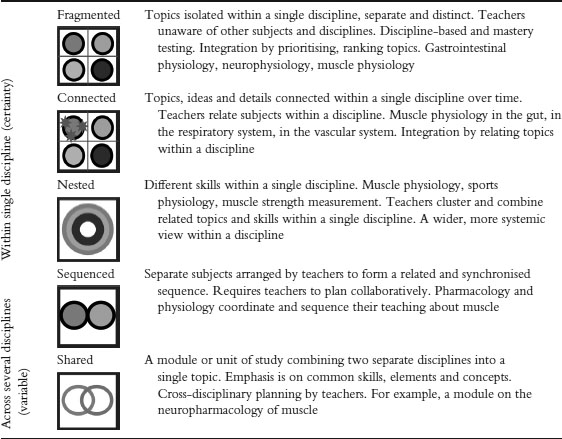
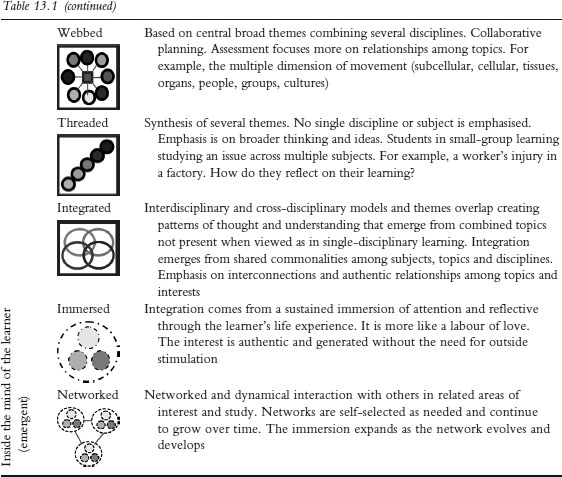
Source: Adapted from Fogarty and Pete (2009). See Harden (2000) for specific examples applied to medical education.
Case study 13.1 Integration of simulation-based clinical correlation pedagogy within an anatomy curriculum, Kuala Lumpur, Malaysia
Nicole Shilkofski and Carmen Coombs
Perdana University Graduate School of Medicine (PUGSOM) in Kuala Lumpur is the first graduate-entry medical school in Malaysia, developed in collaboration with Johns Hopkins University School of Medicine (JHUSOM) to introduce the American-style 4-year medical curriculum in Southeast Asia. Simulation-based clinical correlation pedagogy was integrated into the Introduction to Human Anatomy course for Year 1 medical students at PUGSOM, which, unlike at JHUSOM, is non-cadaveric in its pedagogy as a result of resource and cultural constraints. Cadavers for purposes of dissection are not widely available in Malaysia, necessitating a novel pedagogy to teach surgical and radiological approaches to anatomy.
A simulation-based curriculum was designed to teach the clinical relevance of anatomical principles and surface anatomy correlates utilising high-fidelity mannequin simulators, partial task trainers and standardised/simulated patients (SPs). Modules were designed around the major anatomical regions studied concurrently in the course, with specific measurable learning objectives related to clinically relevant anatomy. Students rotated each week between simulation stations in small groups, overseen by a faculty preceptor. For example, students encountered a high-fidelity mannequin simulating tension pneumothorax. They discussed the simulator’s clinical findings of decreased breath sounds, hypoxia and tachypnoea, requested diagnostic studies and made a provisional diagnosis. Faculty reviewed radiological images and discussed treatment options in light of the relevant anatomical concepts, emphasising surface anatomical landmarks for the procedure of needle decompression. Students practised the procedure on the mannequin under faculty supervision and guidance. Additional stations included clinical anatomy procedures for the thorax, abdomen, extremities and head and neck regions. Engagement, self-assessed pragmatic learning and knowledge retention were evaluated favourably by students. Knowledge of clinically related anatomical concepts was assessed as significantly better after participation in the curriculum.
This type of applied simulation is feasible and effective for integration into pre-clinical sciences such as anatomy, particularly in settings where access to cadaveric specimens for dissection may be limited.
This case study presents integration using aspects of the ‘nested’ and ‘shared’ curriculum models in collaborative planning with clinical skills and anatomy as required (Table 13.1), in which multiple skills such as needle decompression of a tension pneumothorax are used to enhance the relevance of the anatomy of the thorax (Fogarty and Pete 2009). Integration of knowledge is the primary focus, with some ‘social integration’ in working with peers and teachers around case diagnosis and treatment (Beane 1997).
Constraints that organise the integration include the lack of cadavers, a single discipline sequenced early in a new 4-year curriculum, organisation by disciplines and specific anatomical regions, defined problems and diagnoses, radiological correlates and surgical procedures. Advantages of this approach to integration include enhancing the relevance of specific anatomical regions, hands-on simulation, practical procedures and clinical radiological and surgical skills stimulating interest in the subject.
It is worth noting that the integration is geared towards future practice rather than application now, to real problems of consequence that could be within the skill level of first-year students. For example, it might be possible to decrease further the constraints on learning anatomy by extending learning activities to include basic screening history interviews with simulated and real patients whose problems require sense making with knowledge of anatomical correlates related to the story of the present illness and its history. Most history questions have anatomical and other sciences basic to medicine underlying their purpose. For example, ‘How often, if at all, do you wake up at night to go to the bathroom (heart, pulmonary, kidneys, urogenital diaphragm, drug-induced, etc.)? What is the anatomical structure of the heart and lung sounds you are hearing in this person? How do they relate to the person’s chief complaint? What is the structural explanation for wheezing in this person? Is your pain localised (patient points to area with one finger) or diffuse (patient moves the whole hand over a region)?’ In this way, typical history questions can be interpreted anatomically as well as with most of the sciences basic to medicine. The basic screening history and physical examination provide all the anatomical correlations students need in the here and now as they learn and practise basic clinical skills early in their education. It is also possible to be multidisciplinary, to add other disciplines sequenced within the basic screening clinical skills approach. It could even lead to a sequenced and shared integration (Table 13.1) with planning between the anatomy and clinical skills teachers.
The next case study combines several basic science disciplines with clinical correlations in a slightly different way.
Case study 13.2 Clinical odontologists teaching basic sciences for health, integrating basic/clinic, different methodologies and disciplines in Argentina at the National University of Rio Negro Dental School – why it works
Elena I. Barragán
A multidisciplinary course comprised of anatomy, histology, embryology, physiology, biochemistry and biophysics involved 60 students in the second year of a 6-year course at the Dental School in the National University in Patagonia, Argentina. The purpose was to use clinical correlations to engage clinical practitioners and enhance teaching.
The teachers of the basic sciences are practising dental health professionals. They apply examples and metaphors from their everyday practice to their teaching. The integration is between the disciplines involved in the course and the practical applied experience of the teachers. Teachers also emphasise and highlight relevant content from the appropriate texts related to professional practice. Students identify with practising odontologists. They see themselves in the future with the help of a teacher who can translate clinical situations for students and use clinical examples to explain the importance of concepts to both the present course and to their future practice. This motivates students to integrate the complex arena of the basic sciences with the management of clinical situations. In return, the reward of engaging students in significant learning is an important motivation for teachers learning new methodologies and seeking to enhance their capability as teachers. Pedagogy is integrated by mixing teacher- and student-centred methods. In addition, internet platforms, email, PowerPoint and communication contribute to the course.
One problem encountered is that professionals and teachers have become specialised and, consequently, someone who teaches anatomy may have difficulty teaching embryology or physiology. Similarly, dentists who practise orthodontics may not be familiar with mandible junction problems. The challenge is to build teams that know how to work together, support each other and give the ability to someone else to take the lead when their expertise is required. Knowing when and how to shift roles to be supportive of someone else’s abilities is very important for effective teamwork (Arrow and Henry 2010). Without this ability among the teachers, students find it difficult to learn from and within teams and struggle to develop their own collaborative and collective integrated vision of effective teamwork.
What works with students is centring education where it is fit for purpose, sometimes on students, sometimes on teachers and at other times on texts, internet materials, community-based experiences, field-based practice and family practice. A dynamic approach blends teaching methodologies that are responsive to the variable mix of the disciplines. Teachers use real situations to integrate content and practice and students find this effective for their learning and professional growth.
The integration described crosses disciplines and could combine aspects of Fogarty’s ‘sequenced’ and ‘shared’ models of curriculum (Table 13.1). ‘Sequenced’ refers to topics and ideas arranged serially to coincide with one another, i.e. practising dentists bringing practical experiences and metaphors to particular disciplines and content. ‘Shared’ refers to planning in two disciplines organised around shared concepts or ideas (Fogarty and Pete 2009). The integration described in the dental school could also have aspects of the ‘webbed’ model that presents a central theme linked to different subject areas (Table 13.1). It is not clear to what extent teachers are using their practical experience and metaphors to organise the course content or whether the subject content is the organisational centre around which practice themes and metaphors are selected; probably some of both, depending on individual teachers, the conditions and their comfort with the subject. ‘Knowledge integration’ and ‘social integration’ (Beane 1997) are expressed by practising dentists serving as role models for early socialisation of students into the profession. In addition, there is some ‘integration’ in curriculum design as knowledge is developed and used to address both basic sciences and practical applications. The motivation for and relevance of learning the basic sciences are enhanced by clinically relevant examples, stories and metaphors. As with the case study from Malaysia, the application of what is being learned is deferred to the students’ future, a constraint on the continuity of learning and coherence across the curriculum.
The example from Saudi Arabia seeks to integrate learning across the entire curriculum rather than within a particular subset of disciplines.
Case study 13.3 Basic science integration into the whole curriculum at the Faculty of Medicine, King Abdulaziz University, Saudi Arabia
Abdulmonem Al-Hayani
The medical curriculum at Abdulaziz University begins with and follows an outcome-based approach linked to the attributes students must have at graduation. Two phases are described:
• Phase I (first 2 years) includes core courses in the basic medical sciences and system-based modules, such as musculoskeletal, immune-blood-lymph. Basic sciences are integrated horizontally at different levels of Harden’s ladder of integration (Harden 2000). In addition, some clinically relevant topics are included in different modules, promoting vertical integration among basic and clinical sciences.
• Phase II includes core clerkships and subspecialties, special clinical, biomedical and ethics electives. Special study modules promote self-directed, indepth learning in various fields as students explore their career preferences and/or remedy deficiencies in a subject or specialty. Extended elective modules provide students with opportunities to acquire research abilities, to enhance skills in collection, evaluation, synthesis and presentation of evidence and to participate in community services.
Different teaching approaches and strategies include lectures, tutorials, self-directed learning, student-prepared presentations, practical learning and PBL. PBL emphasises the elaboration of learning goals and discussion in small groups across disciplines. Formative and summative assessment methods include: written examinations, multiple-choice questions, matching, short and long essay, Objective Structured Practical Examination (OSPE) and Objective Structured Clinical Examination (OSCE). Central management of the curriculum is overseen by Phase I and II committees and a main curriculum committee that oversees the whole curriculum.
Integration occurs within a curriculum organisation constrained in two phases in a ‘2 + 2’ Flexnerian organisation with clinical correlates in core courses and systems-based modules in the first 2 years (Phase I). Phase II resembles Fogarty’s ‘shared’ and ‘threaded’ curriculum integration model (Table 13.1), with teaching organised around connected sections, such as core clerkship topics, where the final outcome competencies are defined within and across all sections. Electives can be understood to function as both a ‘webbed’ and a ‘themed’ curriculum model, allowing deeper development of a particular area of interest (Fogarty and Pete 2009). Electives that are extended over a long period of time allow for more ‘immersion’ (Table 13.1), with aspects of the third of Fogarty’s categories: integration within and across learners. The curriculum described has an overall ‘threaded’ and ‘webbed’ theme (Table 13.1) with a progressive decrease in constraints on student learning over the 4 years. Integration works to the extent that it is present across the curriculum (coherence) rather than within particular subsections.
A further case study of relevance to this chapter (‘The Primary Care Curriculum at the University of New Mexico School of Medicine’ by S. Scott Obenshain) can be found in Chapter 15. This New Mexico case study illustrates aspects of ‘webbed’, ‘threaded’ and ‘integrated’ models (Table 13.1) in which clinical skills and community are the organising focus around which the rest of the curriculum is organised, including the sciences basic to medicine. There were also some aspects of the ‘immersed’ and ‘networked’ model (Table 13.1) in that the primary care curriculum remained responsive to real-time health issues and to the growing needs of the community. Networking also promoted responsiveness to students as they participated in decision making about the programmes itself (Beane 1997).
Assessment and integration of the sciences basic to medicine
The assertion that assessment of learners and learning are co-embedded, interrelated and interdependent (Schuwirth and van der Vleuten 2004, 2006; Dijkstra et al. 2010; Schuwirth et al. 2011; Hodges 2013) specifies that the level of complexity of the assessment must match the level of complexity of the teaching conditions of the whole for which the assessment is valid. Another way to say this is that the assessment is ‘fit for function’. What might this look like in the sciences basic to medicine?
Imagine you are at the end of your first year of a 4-year, or the end of the second year in a 6-year, medical curriculum. You are in an anatomy laboratory practical examination with a series of timed stations, one of which has a bisected human heart with an arrow pointing to a part of it (in this example the arrow points to a hole in the interventricular septum). The question reads, ‘Describe the chief complaint that brought this person to seek assistance from their health provider. Explain how it is interrelated with the structure indicated by the arrow.’ Students have to recognise the interventricular septum and know its structure, embryology and function. They would need to understand the dynamics of pressure in the heart chambers during the cardiac cycle and how this hole in the interventricular septum is a difference that makes a difference. Many of the sciences basic to medicine are integrated with the whole of this ‘simple short question’ and it is relevant to early clinical experiences in the curriculum.
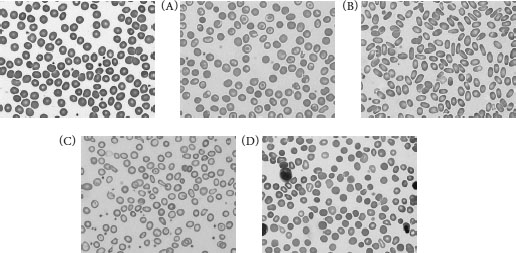
Another example of an assessment question for integrating sciences basic to medicine at a higher dimension of interrelationships comes from a pilot assessment written collaboratively by the author and the late Miriam Friedman Ben-David in 1991 for what was to become an integrated Student Progress Assessment of the Primary Care Curriculum at the University of New Mexico School of Medicine. The question was developed for students at the end of their second year of their study in that programme. The question begins with a brief problem that Mrs Pereira brings to her physician, followed by some history about her problem, some physical examination data, and laboratory data and images (Box 13.1).
Box 13.1 Sample question illustrating an approach to assessing the integration of the sciences basic to medicine and clinical skills
History
Regina Pereira is a 48-year-old woman who visited her family physician, Dr Wernicke, complaining of increasing fatigue and shortness of breath on minimal exertion (such as carrying the groceries from the car). She has noted progressive worsening of her symptoms over the previous few months. She had no history of heart or lung problems. Her husband has noticed that she is pale.
Review of symptoms is notable for many months of menstrual irregularity with quite heavy menstrual flow. She has not had this problem previous to this year and has no history of other bleeding problems or easy bruising.
Past medical history is negative for rheumatic fever, hypertension and diabetes. She has had three pregnancies that were uncomplicated.
Social history: non-smoker, works in the home, married 15 years.
A) Physical examination
• Mrs Pereira is a pleasant but somewhat apprehensive woman who appears pale.
• Temperature 37.2°C; blood pressure 120/55 mmHg; pulse 110 beats/minute; respiration 16 breaths/minute.
• Sclera anicteric. Neck: No jugular venous distension.
• Heart. Prominent point of maximal impulse, S1, S2, no S4 or S3, a systolic murmur was heard.
• Lungs. Normal to percussion. No rales or rhonchi noted.
• Abdomen. Normal bowel sounds, no hepatosplenomegaly. Stool Hemoccult negative.
• Extremities. No cyanosis or oedema.
• Neurological exam: Normal.
B) Laboratory data
| White blood cells 5.5 × 109 litre |
(Normal 4.8 × 109 litre) |
| Differential: 74% neutrophil; 21% lymphocyte; 4% monocyte; 1 % eosinophil |
| Red blood cells 3.0 × 1012/litre |
(Normal 4.7–6.1 × 1012/litre) |
| Haemoglobin 7.0 g/dl |
(Normal female 12.0–16.0 g/dl |
| Haematocrit 23.0% |
(Normal female 37–47%) |
| Platelet count 450 × 109/litre |
(Normal 150–400 × 109/litre) |
| Mean cell volume 76.6 fl |
(Normal 81–99 fl) |
| Mean cell haemoglobin concentration 30.4 g/dl |
(Normal 31.5–36.6 g/dl) |
| Reticulocyte count (uncorrected) 2.8% |
(Normal 0.5–1.5%) |
| Total bilirubin 1.1 mg/dl |
(Normal 0.2–1.2 mg/dl) |
| Direct bilirubin 0.2 mg/dl |
(Normal 0. –3 mg/dl) |
| Lactate dehydrogenase 361 IU/ml |
(Normal 300–600 IU/ml) |
| Task 1: |
Using the figures below, choose a letter of the blood smear which illustrates the red blood cell morphology that is most consistent with this patient’s situation (1 point) and then explain your choice (2 points). |
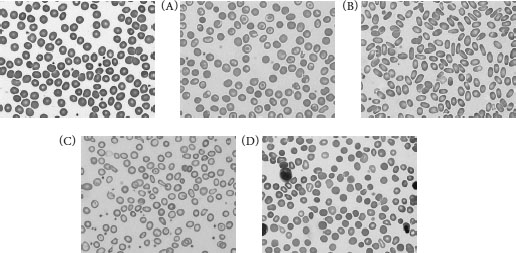
Source: Images provided by Carla S. Wilson MD PhD, Department of Pathology, University of New Mexico School of Medicine.
| Task 2: |
Calculate the corrected reticulocyte count (1 point) and then explain its significance in this patient (2 points). |
| Task 3: |
Explain what the bilirubin value tells you about this patient’s problem (2 points). |
| Task 4: |
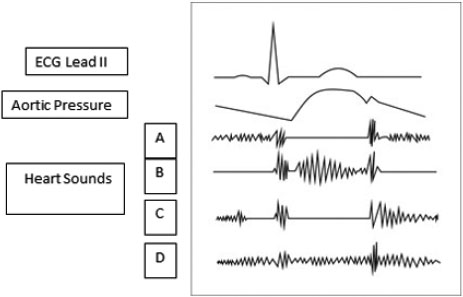
Below are several tracings synchronised in time; ECG lead II, aortic pressure and four heart sounds: A, B, C and D. Using this illustration (below), choose the one tracing, A, B, C or D, that most accurately represents the heart sounds for this patient (1 point) and explain your choice (2 points). |
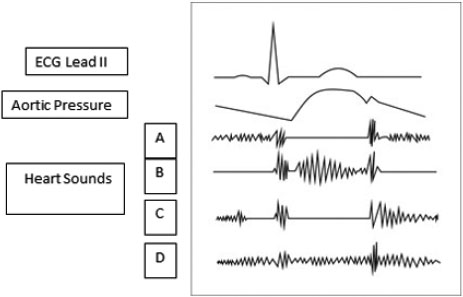
Mrs Pereira’s story cannot be understood without making some sense of the relationships among the sciences basic to medicine. The question is still somewhat discipline-oriented and can fit with ‘webbed’ and ‘integrated’ models of curriculum (Table 13.1). The question is derived from a need to understand a real problem in the here and now rather than at some time in the future. Furthermore, it is not possible to receive a passing mark on this question by only correctly identifying structures, as explanation is worth twice as much as identification. This gives a strong message to students and teachers about the relevance of integration to understanding health problems and the need for understanding that informs actions.
The integration of the sciences basic to medicine is an interactive process of interrelating, combining, forming, emerging and working together to form a whole. The perception and understanding of an ‘integrated whole’ of the curriculum are relative to the scale at which it is observed and measured. Thus, curriculum integration can be viewed at multiple levels: the whole (a module or unit, the curriculum), the part (a single event, discipline or subject, a person), and the greater whole (the university, the hospital, the health system and society). The expression of what works with respect to the integration of the sciences basic to medicine, and its integration across the continuum of possibilities, can be understood as a function of the limits and constraints (degrees of freedom) affecting the interactions and exchanges among people, ideas, things and environments. Learning situations close to certainty and agreement are organised and integrated as single disciplines with linear, additive, reliable and replicable characteristics. A little further away from certainty and agreement, learning situations exhibit more variations and possibilities organised and integrated in predictable phases, steps and cycles – a main theme in contemporary medical education. Still further from certainty and agreement, when there are too many factors involved in the learning situation to control in a predictable way, the conditions become complex and unpredictable and are far from equilibrium.
Tension builds up in the system and its release functions to reorganise the structure of the situation (self-organisation) spontaneously such that a new structure emerges that is more appropriate, i.e. a better fit for function. This is a fundamental mechanism and explains why complex adaptive systems are learning systems (Davis et al. 2008). Examples are seen in the nervous and immune systems, socio-cultural interactions with health systems, collective problem solving through group and teamwork, authentic educational settings, complex health professional–patient relationships, and the process of learning to become a practising health professional.
It is in this context that the integration of the sciences basic to medicine into the whole of the curriculum can be understood and explained. The adaptive action landscape diagram (Figure 13.1) combined with Fogarty’s dimensions and models of curriculum integration (Tables 13.1 and 13.2) (Fogarty 1991; Fogarty and Pete 2009), as seen through the lens of the case studies from Malaysia, Argentina, Saudi Arabia and the USA, can be used to visualise the dynamics of the relationships between learning situations far from certainty and agreement (emergent) and those closer to certainty and agreement (certain and variable) (Figure 13.2).
It also suggests a meaningful strategy for change through modification of the conditions (constraints) in the workplace to which people respond rather than directly persuading and pressuring people to change (Heifetz 1994; Heifetz et al. 2009; Eoyang and Holladay 2013).
The significance of the proposed synthesis of levels of curriculum organisation and the continuum of integration of learning situations as a function of agreement and certainty is that both linear and non-linear conditions can be embraced without the necessity of resorting to reductionism and fragmentation when confronted with complex high-dimensional learning, teaching, assessment and research situations. To go further in medical education, to achieve a responsive, integrated curriculum across the full spectrum of learning and practice situations, requires seeing, understanding and influencing both linear (additive) and non-linear (multiplicative) learning situations (West 2010).
Table 13.2 The relationship between landscape categories and Fogarty’s three stages and ten curriculum models
| Landscape diagram (Figure 13.2) |
Fogarty’s ten curriculum models (Fogarty and Peat 2009) |
| |
| Certain |
Within a single discipline |
Highly constrained curriculum integration patterns and activities. Predictable, reliable, reproducible |
Fragmented, connected, nested |
| Variable |
Across disciplines |
Moderately constrained curriculum integration patterns and activities expressed as recognisable variations in phases, cycles, stages and steps. Variations on the theme are common |
Sequenced, shared, webbed, threaded, integrated |
| Emergent (uncertain) |
Within and across learners |
Very low constraints on curriculum integration; patterns are complex and unpredictable. Innovation and creativity in response to changing conditions |
Immersed, networked |
Non-linear, complex adaptive situations are essential to creativity and innovation and are especially useful when what has worked before is no longer working. What is needed is integration of the full range of learning conditions in the curriculum from day one to the last day and beyond, so students learn and become more comfortable with the different conditions that favour certainty, variability and emergent complex adaptive situations. The presence of integration of certain, variable and emergent learning situations from day one of the curriculum until graduation and beyond contributes to a comfort and capacity building among students of their ability to deal with the sticky reality of uncertainty much earlier, and therefore have more experience learning about and with it during their professional education. This proposed approach to integration keeps learners, teachers and the curriculum continuously curious about, and sensitive and responsive to, variability, creativity and innovation while assuring the quality of knowledge, skills and attitudes for what needs to be learned, understood and embedded through authentic experiences as a way to move forward in the dynamic context of 21st-century health professions education.
Take-home messages
• Integration in the curriculum is the combination and coordination of separate and diverse elements into a more complete and harmonious whole.
• The recent history of medical education is one of progressive decreases in the level of constraints on integration in the curriculum.
• There are different degrees of integration of the sciences basic to medicine depending on the constraints and conditions that can be visualised in an adaptive action landscape diagram of close to certainty and agreement (certainty), further from certainty and agreement (variable) and far from certainty and agreement, depending on the number of factors involved.
• Three stages of integration (within a single discipline, across disciplines, across learners) and ten curriculum models are described.
• Integration of the sciences basic to medicine applies equally to assessment of learners, and the level of complexity of the integration questions must match the level of complexity of the teaching conditions for the assessment to be valid.
• A curriculum model is proposed in which curriculum constraints can be illustrated within a landscape diagram with axes of certainty and agreement, upon which Fogarty’s three forms and ten methods of integration are superimposed.
Note
1 The concept of the sciences basic to medicine is preferred as it provides a more expansive, inclusive and relevant framework (i.e. the physical, biological, social, political sciences and more) than the concept of the basic sciences (i.e. traditionally limited to anatomy, physiology, biochemistry, microbiology, pharmacology and pathology).
Bibliography
Anderson, M.B. and Swanson, A.G. (1993) ‘Educating medical students – the ACME-TRI report with supplements’, Academic Medicine, 68(6, Suppl.): S1–46.
Arrow, H. and Henry, K.B. (2010) ‘Using complexity to promote group learning in healthcare’, Journal of Evaluation in Clinical Practice, 16(4): 861–6.
Association of American Medical Colleges (1984) ‘Physicians for the twenty-first century: Report of the project panel on the general professional education of the physicians and college preparation for medicine’, Journal of Medical Education, 59(11, Part 2): 1–208.
Barrows, H.S. and Tamblyn, R.M. (1980) Problem-based learning: An approach to medical education, New York, NY: Springer Publishing.
Barrows, H.S., Williams, R.G. and Moy, R.H. (1987) ‘A comprehensive performance-based assessment of fourth-year students’ clinical skills’, Journal of Medical Education, 62(10): 805–9.
Beane, J. (1997) Curriculum integration: Designing the core of democratic education, New York, NY: Teachers College Press.
Bleakley, A., Bligh, J. and Browne, J. (2011) Medical education for the future: Identity, power and location, Dordrecht: Springer.
Bloom, B.S. (ed), Engelhart, M.D., Furst, E.J., Hill, W.H. and Krathwohl, D.R. (1956) Taxonomy of educational objectives: The classification of education goals. Handbook I: Cognitive domain, New York, NY: David McKay.
Davis, B., Sumara, D. and Luce-Kapler, R. (2008) Engaging minds: Changing teaching in complex times, New York, NY: Routledge.
Dijkstra, J., van der Vleuten, C.P.M. and Shuwirth, L.W.T. (2010) ‘A new framework for designing programmes of assessment’, Advances in Health Sciences Education, 15(3): 379–93.
Doll Jr, W.E. (1993) A post-modern perspective on curriculum, New York, NY: Teachers College Press.
Eoyang, G.H. and Holladay, R. (2013) Adaptive action: Leveraging uncertainty in your organisation, Stanford, CA: Stanford University Press.
Epstein, R.M. and Hundert, E.M. (2002) ‘Defining and assessing professional competence’, Journal of the American Medical Association, 287(2): 226–35.
Flexner, A. (1910) Medical education in the United States and Canada: A report to the Carnegie Foundation for the Advancement of Teaching, bulletin no. 4, New York, NY: The Carnegie Foundation for the Advancement of Teaching.
Fogarty, R. (1991) ‘10 ways to integrate curriculum’, Educational Leadership, 49(2): 61–5.
Fogarty, R. and Pete, B.M. (2009) How to integrate the curricula (3rd edn), Thousand Oaks, CA: Corwin.
Friedman Ben-David, M., Davis, M.H., Harden, R.M., Howie, P.W., Ker, J. and Pippard, M.J. (2001) ‘AMEE medical education guide no. 24: Portfolios as a method of student assessment’, Medical Teacher, 23(6): 535–51.
General Medical Council (2003) Tomorrow’s doctors, London: General Medical Council.
General Medical Council (2009) Tomorrow’s doctors: Outcomes and standards for undergraduate medical education, London: General Medical Council. Online. Available HTTP: www.gmc-uk.org/New_Doctor09_FINAL.pdf_27493417.pdf_39279971.pdf (accessed 10 June 2014).
Hafferty, F.W. (1998) ‘Beyond curriculum reform: Confronting medicine’s hidden curriculum’, Academic Medicine, 73(4): 403–7.
Harden, R.M. (2000) ‘The integration ladder: A tool for curriculum planning and evaluation’, Medical Education, 34(7): 551–7.
Harden, R.M., Crosby, J.R. and Davis, M.H. (1999) ‘AMEE guide no. 14: Outcome-based education: Part 1 – An introduction to outcome-based education’, Medical Teacher, 21(1): 7–14.
Heifetz, R.A. (1994) Leadership without easy answers, Cambridge, MA: Belknap Press of Harvard University Press.
Heifetz, R.A., Grashow, A. and Linsky, M. (2009) The practice of adaptive leadership: Tools and tactics for changing your organization in the world, Boston, MA: Harvard Business Press.
Hodges, B. (2013) ‘Assessment in the post-psychometric era: Learning to love the subjective and collective’, Medical Teacher, 35(7): 564–8.
Kauffman, S. (1993) The origins of order: Self-organization and selection in evolution, New York, NY: Oxford University Press.
Kaufman, A. (ed.) (1985) Implementing problem-based medical education: Lessons from successful innovations, New York, NY: Springer.
Kaufman, A., Mennin, S., Waterman, R., Duban, S., Hansbarger, C., Silverblatt, H., Obenshain, S.S., Kantrowitz, M., Becker, T., Samet, J. and Wiese, W. (1989) ‘The New Mexico experiment: An educational innovation and institutional change’, Academic Medicine, 64(6): 285–94.
Mennin, S. (2010a) ‘Self-organization, integration and curriculum in the complex world of medical education’, Medical Education, 44(1): 20–30.
Mennin, S. (2010b) ‘Sustainability of PBL and innovation in medical education at Maastricht University’. In: H. van Berkel, A. Scherpbier, H. Hillen and C. van der Vleuten (eds) Lessons from problem-based learning, Oxford: Oxford University Press.
Mennin, S. and Petroni-Mennin, R. (2006) ‘Community-based medical education’, The Clinical Teacher, 3(2): 90–6.
Miller, G.E. (1990) ‘The assessment of clinical skills/competence/performance’, Academic Medicine, 65(9 Supp): S63–7.
Morcke, A., Dornan, T. and Eika, B. (2013) ‘Outcome (competency) based education: An exploration of its origins, theoretical basis, and empirical evidence’, Advances in Health Sciences Education, 18(4): 851–63.
Motola, I., Devine, L.A., Chung, H.S., Sullivan, J. and Issenberg, S.B. (2013) ‘Simulation healthcare education: A best evidence practical guide. AMEE guide no. 82’, Medical Teacher, 35(10): e1511–30.
Neufeld, V.R. and Barrows, H.S. (1974) ‘The ‘McMaster philosophy’: An approach to medical education’, Journal of Medical Education, 49(11): 1040–50.
Norcini, J. and Burch, V. (2007) ‘Workplace-based assessment as an educational tool: AMEE guide no. 31’, Medical Teacher, 29(9): 855–71.
O’Sullivan, H., van Mook, W., Fewtrell, R. and Wass, V. (2012) ‘Integrating professionalism into the curriculum: AMEE guide no. 61’, Medical Teacher, 34(2): e64–77.
Papa, F.J. and Harasym, P.H. (1999) ‘Medical curriculum reform in North America, 1765 to the present: A cognitive science perspective’, Academic Medicine, 74(2): 154–64.
Patterson, J.W. (1956) ‘Weston Reserve interdepartmental and departmental teaching of medicine and biological science in four years’, Journal of Medical Education, 31(4): 521–9.
Patterson, L., Holladay, R. and Eoyang, G.H. (2013) Radical rules for schools: Adaptive action for complex change, Circle Pines, MN: Human Systems Dynamics Institute.
Schmidt, H.G. (1993) ‘Foundations of problem-based learning: Some explanatory notes’, Medical Education, 27(5): 422–32.
Schuwirth, L.W.T. and van der Vleuten, C.P.M. (2004) ‘Changing education, changing assessment, changing research?’, Medical Education, 38(8): 805–12.
Schuwirth, L.W.T. and van der Vleuten, C.P.M. (2006) ‘A plea for new psychometric models and educational assessment’, Medical Education, 40(4): 296–300.
Schuwirth, L., Colliver, J., Gruppen, L., Kreiter, C., Mennin, S., Onishi, H., Pangaro, L., Ringsted, C., Swanson, D., van der Vleuten, C. and Wangner-Menghin, M. (2011) ‘Research in assessment: Consensus statement and recommendations from the Ottawa 2010 conference’, Medical Teacher, 33(3): 224–33.
Simpson, J.G., Furnace, J., Crosby, J., Cummings, A.D., Evans, P.A., Friedman Ben-David, M., Harden, R.M., Lloyd, D., McKenzie, H., McLachlan, J.C., McPhate, G.F., Percy-Robb, I.W. and MacPherson, S.G. (2002) ‘The Scottish doctor – learning outcomes for the medical undergraduate in Scotland: A foundation for competent and reflective practitioners’, Medical Teacher, 24(2): 136–43.
Stacy, R.D. (1996) Strategic management and organizational dynamics, London: Pitman Publishing.
Stepien, K.A. and Baerstein, A. (2006) ‘Educating for empathy: A review’, Journal of General Internal Medicine, 21(5): 524–30.
Stillman, P.L., Swanson, D.B., Smee, S., Stillman, A.E., Ebert, T.H., Emmel, V.S., Caslowitz, J., Greene, H.L., Hamolsky, M., Hatem, C., Levenson, D.J., Levin, R., Levinson, G., Ley, B., Morgan, J., Parrino, T., Robinson, S. and Willms, J. (1986) ‘Assessing clinical skills of residents with standardized patients’, Annals of Internal Medicine, 105(5): 762–71.
ten Cate, O. (2005) ‘Entrustability of professional activities and competency-based training’, Medical Education, 39(12): 1176–7.
van der Vleuten, C.P.M., Dolmans, D.H.J.M., de Grave, W.S., van Luijk, S.J., Muijtjens, A.M.M., Scherpbier, A.J.J.A., Schuwirth, L.W.T. and Wolfhagen, I.H.A.P. (2004) ‘Education research at the Faculty of Medicine, University of Maastricht: Fostering the interrelationship between professional and education practice’, Academic Medicine, 79(10): 990–6.
West, B.J. (2010) ‘Homeostasis and Gauss statistics: Barriers to understanding natural variability’, Journal of Evaluation in Clinical Practice, 16(3): 403–8.
Worley, P., Silagy, C., Prideaux, D., Newble, D. and Jones, A.H. (2000) ‘The parallel rural community curriculum: An integrated clinical curriculum-based in rural general practice’, Medical Education, 34(7): 558–65.
Wrigley, W., van der Vleuten, C.P.M., Freeman, A. and Muijtjens A. (2012) ‘A systematic framework for the progress test: strengths, constraints and issues: AMEE guide no. 71’, Medical Teacher, 34(9): 683–97.
Zimmerman, B., Lindberg, C. and Plsek, P. (2001) Edgeware: Insights from complexity science for health care leaders, Irving, TX: VHA Publishing.