8
HOPE ON THE HORIZON
The Promise of New Treatments
The latest research is the latest hope.
—Michael J. Fox
THERAPEUTIC PROGRESS AGAINST PARKINSON’S HAS BEEN SLOW. In the last twenty years, the Food and Drug Administration (FDA) has approved about a dozen new drugs for Parkinson’s (Table 1).1 Nearly all of them, however, are only incremental advances on existing therapies. Three of the new drugs are just different formulations of levodopa, the dopamine precursor.2 Others treat the increased involuntary movements that levodopa causes. Some decrease the symptom fluctuations that can develop after long-term use of the drug—there can be periods when levodopa works well and other times when it does not.
In this century, only two new drug classes—therapies that take a different approach to tackling the disease—have come on the US market. However, both only treat symptoms that affect a subset of individuals: pimavanserin for hallucinations and droxidopa for lightheadedness. Fortunately, in addition to the gene-targeting treatments likely on the way, innovative surgeries, possible immunizations, and other new therapies are emerging.
THE POTENTIAL OF DEEP BRAIN STIMULATION
Frida Falcon, a successful Peruvian sculptor in her fifties, and her husband, Marcus, a multinational businessman, were enjoying a good life together. Then “Mr. Parkinson,” as they came to refer to the disease, knocked at their door. As the illness took increasing control over Frida, her ease of movement and artistry disappeared. Medication helped but only temporarily. When her levodopa kicked in, her tremors would fade away. But over time she needed to take the drug every hour.
Then she developed new, more disabling movements. These writhing motions prevented her from sculpting or even sitting still. The more levodopa she took, the worse the movements became. When she took less, she stiffened and moved more slowly.
The Falcons were fortunate enough to have the resources to fly around the world and meet with different doctors. Eventually, they decided to pursue deep brain stimulation surgery at the University of Florida under the guidance and care of one of our authors, Dr. Michael Okun, and his colleague, Dr. Kelly Foote. During a four-hour procedure that requires the patient to be awake, wires that produce electrical impulses are implanted in the brain. The thought of sticking metal into her head was obviously not appealing to Frida, but in select individuals, the surgery can reduce the involuntary movements caused by levodopa, decrease the symptoms of Parkinson’s, and improve quality of life.15
Surgery as a treatment option for Parkinson’s first emerged over one hundred years ago.16 Doctors noticed on rare occasions that a stroke or brain tumor in specific locations—parts connected to the substantia nigra where dopamine-producing nerve cells are located—could relieve the symptoms of Parkinson’s. Based on these observations, surgeons in the 1930s and 1940s began damaging (usually by burning with an electric current) specific areas of the brain to try to alleviate tremors. Not surprisingly, slight errors had profound consequences. Missing the target by even a millimeter or two led to visual loss, problems with speech, or paralysis. When the surgeons hit their target, a patient’s tremor, though, could magically disappear. With the arrival in the 1960s of levodopa, which was safe and effective, risky surgeries for Parkinson’s soon fell out of favor.17
In the 1970s, interest in surgery was renewed when Dr. Mahlon DeLong, a gifted researcher at Johns Hopkins, began to map the brain circuits important to Parkinson’s disease. DeLong created a model of the brain circuitry that showed connections between the substantia nigra and many other parts of the brain.
DeLong identified brain areas that were responsible for movement. Other brain circuits are responsible for seeing or speaking, for example. With a model of the movement network, DeLong and other scientists could then predict what might happen from a loss of nerve cells in the substantia nigra. This loss would decrease its output and affect other parts of the brain circuit that then might become under- or overactive.18 These areas could then be targets for surgical treatment that would usually decrease the output from regions that were hyperactive.
With DeLong’s map of the brain circuits, surgeons could now explain why earlier surgeries that quieted certain targets worked. They could also surmise why other surgeries did not. The time was ready for a more refined surgical approach. In 1987, Dr. Alim Benabid in Grenoble, France, came up with one. Rather than destroying nerve centers, he suggested using electrical current to change their output. This approach was called deep brain stimulation.19
This new surgery uses a small electricity-conducting wire to stimulate a targeted area of the brain. The wire is connected to a battery that is placed under the skin on a patient’s chest much like a pacemaker for the heart. The battery-powered wire can then provide electrical current to change the nerve cell activity in the targeted region. This stimulation actually decreases or blocks the output of the target.20
However, rather than irreversibly destroying the nerve cells like earlier surgeries, this stimulation can be modified based on a patient’s symptoms. Like a television, the stimulator can be adjusted with a wireless remote control device. In the clinic, when a patient’s stimulator is first turned on, the results can be dramatic. Tremors can vanish, stiffness can disappear, walking can become normal, and hidden smiles can reappear.
Over time, Parkinson’s progresses, and adjustments to the deep brain stimulator are required. And unfortunately, over enough time the miraculous effects tend to disappear. Still, Dr. David Marsden, the late British neurologist and one of the founders of the movement disorders field, called deep brain stimulation one of the two miracles in Parkinson’s disease (levodopa was the other).
Numerous studies have demonstrated the benefits of the surgery, which has become part of standard Parkinson’s care in many regions of the world.21 There are risks, including bleeding, infection, misplacement of the electrode, and, very rarely, death. To date, over 200,000 patients worldwide, including Frida Falcon, have received the surgery.
For Frida, the surgery was a success. She is back to sculpting and jokes that she has divorced “Mr. Parkinson.” The improvement in her movements and quality of life are not permanent but can last from five to ten years.22 She is among the lucky ones.
Many people in most of the world lack access to these expensive surgical techniques—even in the United States. In 1997, the FDA approved the surgery for the treatment of Parkinson’s disease that is not well controlled by medications.23 Deep brain stimulation costs about $65,000, which is generally covered by insurance and Medicare. But the surgery is primarily performed at major medical centers—in the United States and in other high-income nations—which often leaves people living in rural areas at a disadvantage.24 Those who do have access to the surgery usually have to go back every few months to have their stimulators adjusted. Doctors reprogram the stimulators—almost like changing the television channel—to find the settings that best relieve a patient’s symptoms.
New advances are enabling physicians to make these adjustments remotely, which, as it sounds, does not require the patient to travel to the medical center. Doctors in China are already doing this while video conferencing with their patients. The physician cycles through many possible settings until the neurologist and patient find an optimal one that, for example, helps minimize tremors while avoiding side effects from excessive stimulation.
In the future, patients will be able to wear a watch or sensors that can passively monitor their movements. Data from these sensors will be automatically sent to clinicians who can use the information to adjust medications or stimulator settings. The information may even be able to bypass the physician altogether. Like glucose sensors for insulin pumps, the data could guide the stimulator to optimal settings directly. Studies testing this technology have already begun, and Okun along with Dr. Christopher Butson at the University of Utah have been working with the National Institutes of Health to make home-based adjustments in Parkinson’s devices a reality.25
Also on the horizon are more sophisticated stimulators that will be able to predict, rather than react to, tremors. Dr. Helen Brontë-Stewart, a neurologist at Stanford University, and Dr. Peter Brown, a neurologist at the University of Oxford, are now using the wire electrode not only to send electrical impulses but also to sense abnormalities in a brain’s natural rhythm. These blips can indicate the onset of a tremor or can identify when someone’s walking is about to be interrupted by a freezing episode. In two proof-of-concept studies, Brontë-Stewart and her colleagues demonstrated that this adaptive form of deep brain stimulation that responds to a patient’s own signaling can reduce tremors and improve walking.26 So symptoms can be prevented before they even occur.
TURNING CELLS ON WITH A FLICK OF A SWITCH
The emerging field of optogenetics offers more promise for Parkinson’s. As the name suggests, the idea is to activate certain genes and the proteins they command using light (“opto”). The work is still in very early stages and has only been tested on animals, but the approach is fascinating.27
Here is how it works. A virus is used to insert specific genes into nerve cells in the brain. The most important of these genes tells the body to make a protein that turns on—starts working—in response to light. In the 1970s, researchers found this unique light-activated protein in the tiniest of organisms.28 This class of small living creatures is found in very salty environments, such as the Dead Sea. Most remarkably, unlike almost all organisms, these creatures do not require sugar for energy. Instead, they can use light.29
Putting a light inside a human brain is not yet feasible. However, scientists can use light to study the circuitry that DeLong modeled in the brains of animals with Parkinson’s.30 A fiber-optic light source is either mounted onto the skull or placed deep within the brain. When the light is turned on, so is the activity of the protein in the cell. Turning on the light turns on the protein. Turning off the light turns off the protein.
The proteins that are turned on or off by the light control the activity or electrical firing of the nerve cell. Light can activate or excite these now light-sensitive cells. The scientists can see what happens in the circuits that are responsible for movement as well as speech or thinking.31 They can test to see whether activating certain nerve centers in the brain improves or worsens the gait of a parkinsonian mouse all with just light. In essence, they can try to mimic the effects of deep brain stimulation without the surgery.
Researchers at Stanford used light to study the function of different nerve cells in animal models of Parkinson’s disease. Nerve cells that had the light-sensitive protein were turned on or off at the discretion of the researchers. They found that light, depending on which cells it turned on, could worsen or improve Parkinson’s symptoms in mice.32 For example, shining the light on certain nerve cells “elicited a parkinsonian state”—the mice’s movements and walking were slowed.33 By contrast, using a light to turn on dopamine-producing nerve cells “completely rescued” animals from their parkinsonian symptoms.34 In essence, light, and not a medication like levodopa or a surgery like deep brain stimulation, could restore function to animals with Parkinson’s disease.
In the short term, light can help us understand how nerve cells control movement. In the long term, the hope is that surgical treatment with light or optogenetically inspired therapies could alleviate the symptoms of Parkinson’s disease.
TARGETING GENES TO TREAT THE UNDERLYING CAUSE
In 2008, Patti Meese, an effervescent fifty-six-year-old human resources director, developed a shuffling gait and stooped posture and “was pretty much a mess,” she said, when she was diagnosed with Parkinson’s. Receiving that news sent her into what she later described as a “huge depression.” She went into isolation, which she now says is the worst thing that you can do with the disease.
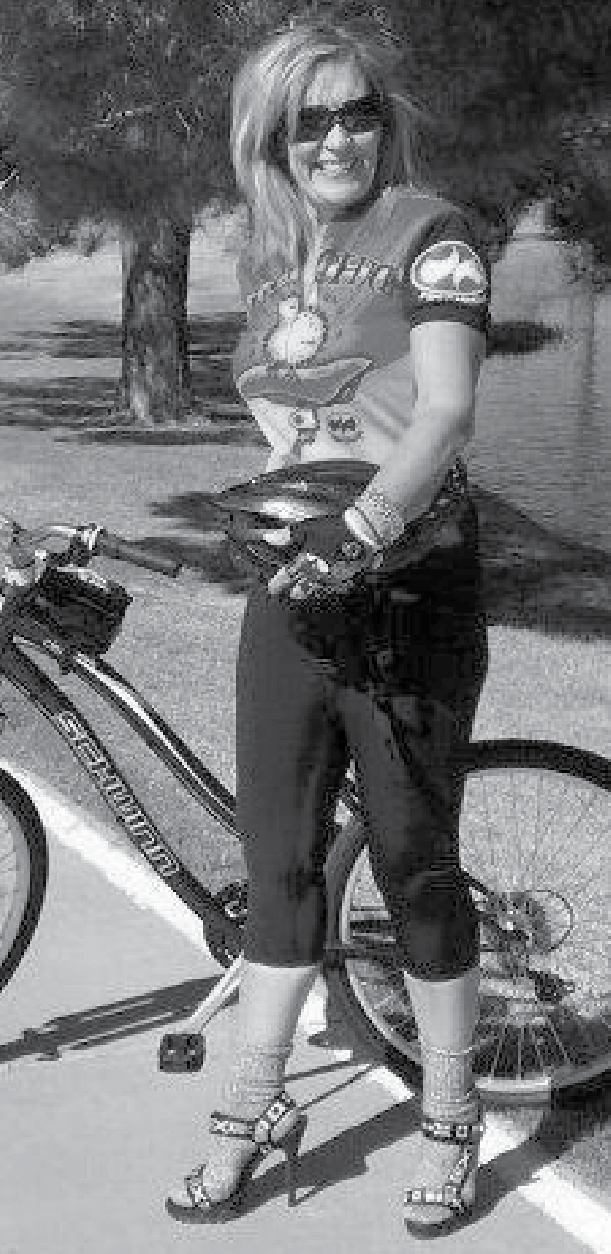
Patti Meese, though, is not one to let anything keep her down. She rebounded from her depression and started doing water aerobics and using a stationary bicycle for up to two hours a day. Soon, she entered El Tour de Tucson, Arizona’s largest bicycling event. To raise money and awareness, she formed her own group of competitors, called “Team Foxy Heels,” and completed a ten-mile ride in six-inch stilettos (Figure 1). She also started volunteering for every research study that she could. By her count, she has participated in more than one hundred in the ten years since her diagnosis.
From one of the studies, she learned that, like Google cofounder Sergey Brin, she carried a mutation in the LRRK2 gene, which can raise the risk of developing Parkinson’s by 20% or more.35 Mutations in the LRRK2 gene increase the activity of the LRRK2 protein.36 Researchers are developing new therapies to reduce its activity.
In an early study of one such drug, researchers at Denali Therapeutics, a biotechnology company in Silicon Valley, found that the drug was safe and well tolerated in healthy volunteers. In the fluid surrounding the brain, high levels of the drug were found, suggesting that the drug is able to get where it needs to go.37 The next step is to test the drug in people with Parkinson’s to make sure it is safe—work that is now underway.38
Denali is not alone in pursuing treatments aimed at LRRK2. Multiple companies, including Biogen, Cerevel Therapeutics, GlaxoSmithKline, and Merck, have all created drugs that target LRRK2.39 For the 1% to 2% of individuals who have Parkinson’s due to mutations in the LRRK2 gene, the drug could slow the progress of the disease.40 For those who carry a mutation but do not have Parkinson’s, the hope is that the gene-targeted treatments could delay or even prevent the disease’s occurrence. Recent research indicates that the LRRK2 protein is inappropriately active in individuals with Parkinson’s even if they do not carry the LRRK2 mutation.41 Consequently, these drugs, if effective, may be beneficial for many people with Parkinson’s.42
Patti Meese hopes to participate in upcoming clinical trials of LRRK2-targeted therapies. She will keep helping further science, she says, “so that no one ever has to hear those four terrible words again: ‘You have Parkinson’s disease.’”
LRRK2 is not the only genetic target for new therapies. In 2004, National Institutes of Health researchers discovered mutations in a gene called GBA that can be found in about 5–10% of individuals with Parkinson’s.43 Those who develop the disease at a younger age are more likely to carry them.44 How the mutations lead to Parkinson’s is under investigation.45 However, these mutations, or changes, in the GBA gene decrease the activity of a protein. This protein is responsible for helping break down alpha-synuclein and other proteins in a part of the cell that acts like a garbage incinerator. The less active the protein that is controlled by the GBA gene, the less well the incinerator works. When this is the case, more garbage bags of alpha-synuclein accumulate in cells. Indeed, Lewy bodies, the garbage bags of alpha-synuclein, are found in the substantia nigra of individuals with GBA mutations.46
A major investor in gene-targeted therapies is one of the world’s leading venture capitalists—and someone who stands to benefit personally from advances. In 2017, Jonathan Silverstein had just made Forbes magazine’s “Midas List” of dealmakers for the sixth time when he noticed a tremor in his left leg. He was forty-nine. His subsequent Parkinson’s diagnosis was attributed to a GBA mutation.47
Silverstein was at first reluctant to disclose his illness publicly. He said, “No one wants to be known as a sick person.… Everyone wants to be known as a Super Bowl–winning quarterback.” He realized, though, that he had the resources to accelerate efforts to find a cure. “I knew I could put a spotlight on [Parkinson’s disease],” he said.
Given his work as a prominent venture capitalist in the biotech and medical devices sectors, Silverstein was well positioned to help advance new treatments for his disease. Companies that he and his firm have backed have received FDA approval for over eighty devices, diagnostics, and therapeutics for a wide range of conditions.
Silverstein started by mailing 1,000 letters to fellow financiers, drug developers, and scientists asking them what were the most promising areas of research and treatment for Parkinson’s due to GBA mutations. The responses came back with many ideas. Given his high profile and appearances on CNBC, in Forbes, and in numerous other media outlets, Silverstein received unsolicited letters as well.48 Among them was one from a man in Ohio with GBA-associated Parkinson’s disease who sent a check for $18.49
Armed with guidance from the people on the cutting edge of Parkinson’s research, Silverstein and his wife created the Silverstein Foundation for Parkinson’s with GBA. The group aims to educate people about the disease (most people with Parkinson’s due to GBA mutations are unaware of the cause) and to develop new therapies to both treat and prevent the disease in those who carry the mutation.50 “If I don’t do it,” Silverstein said, “who does?”51 In its first year, the foundation and its partners launched Prevail Therapeutics, a biotechnology company that has since raised $129 million for the development of gene therapies.52 In 2018, Silverstein was recognized on the “Midas List” for a seventh time.
Clinical trials of treatments aimed at GBA have recently begun. One of the first drugs to be evaluated is called ambroxol.53 It could improve the function of the protein that is altered in people who have Parkinson’s due to GBA mutations.
In 2017, the biotechnology company Sanofi Genzyme launched a clinical trial of another drug aimed at treating Parkinson’s due to the GBA mutation.54 It was designed to lower the levels of a fatty substance that builds up as result of the GBA mutation.55 The study, which is seeking to enroll 243 participants, is expected to end in 2022.56 Prevail Therapeutics is hoping to take up to four drugs into clinical trials in 2019.
Therapies directed at these various mutations mark the beginning of an era of personalized medicine for Parkinson’s—an advance that is long overdue. The Parkinson’s Foundation is helping prepare for this step toward individualized treatment. Formed in 2016 following a merger of two foundations, the Parkinson’s Foundation seeks to improve care and advance research toward a cure.57 In 2018, the Parkinson’s Foundation launched “PD GENEration: Mapping the Future of Parkinson’s Disease” to offer genetic testing and genetic counseling to up to 15,000 people diagnosed with Parkinson’s disease.58 While genetic therapies are not yet available, genetic information about what is or is not causing a person’s Parkinson’s is useful. With appropriate support, people can learn more about their prognosis—genetic causes of Parkinson’s have different rates of progression. Genetic testing also opens the door to participating in certain research studies and, if desired, informing family members about their own risk.59
EMPOWERING THE IMMUNE SYSTEM TO FIGHT PARKINSON’S
Immunization, the same tool that we use to fight infectious diseases, is now being tested as a possible treatment for Parkinson’s (Box A). When we are infected with a virus, such as chicken pox or the flu, our immune systems produce antibodies to kill it off. Our immune system also reacts to foreign proteins. This is convenient in the case of Parkinson’s because misfolded forms of the alpha-synuclein protein—that major factor in the disease—could be targeted. Unfortunately, the human immune system, for uncertain reasons, does not clear the misfolded protein. Scientists are now experimenting with ways to immunize people with the disease so that the misfolded protein is removed or at least does not spread.
Before polio vaccines were developed to prompt people’s immune systems to make their own antibodies, Dr. William Hammon of the University of Pittsburgh had a different idea. He wanted to give individuals existing antibodies against polio to see if they would protect against future infection. Hammon first obtained antibodies from people who had been infected with polio and recovered on their own. He then injected these personalized fighters into children who had not been infected. The children received modest benefit—fewer of them got polio than those who were not immunized. However, Hammon knew the approach had limitations.60 The antibodies were in short supply and insufficient to immunize entire communities. The other issue was that the effects tended to wane, so repeated injections were required. When Jonas Salk and Albert Sabin developed effective vaccines, Hammon’s treatment fell out of favor.61
In October 2018, researchers tried Hammon’s approach against Parkinson’s.62 They gave eighty people three monthly infusions of an antibody directed against the toxic misfolded forms of the alpha-synuclein protein. The antibodies did lower the levels of these proteins in the blood and in the fluid surrounding the brain, where it matters most. Many companies are now pursuing this approach for Parkinson’s.63 While promising, the approach requires much more investigation.64 As with polio, vaccines against these malformed alpha-synuclein proteins is an exciting prospect.
Vaccine studies have recently begun. In 2017, an Austrian biotechnology company called AFFiRiS announced that in an early study of thirty-six people with Parkinson’s, its vaccine did not result in serious safety concerns and was tolerated well.65 The vaccine also resulted in the production of antibodies against alpha-synuclein in about half the participants. However, their antibody levels declined over time and required a later booster injection.66 These results are encouraging, but much more work remains, including a demonstration that the vaccine reduces symptoms in those with the disease.
MAKING NEW THERAPIES ACCESSIBLE TO ALL
In the United States, prescription drugs account for only 5% of health-care expenditures on Parkinson’s compared to 14% for all conditions.67 That is largely because levodopa is a generic drug and is cheap compared to most medications. New treatments, as some patients are discovering, are much more costly.
Four years ago, Karen Blair (not her real name), a seventy-year-old architect, was diagnosed with Parkinson’s. Her neurologist prescribed a medication called rasagiline (brand name Azilect) that improves the symptoms of the disease modestly.68 Studies in laboratory animals suggest that, unlike levodopa, the drug also slows disease progression.69 However, demonstrating such effects in humans is very difficult in the absence of a reliable measurement of its advance.70 Still, Blair was eager to start the drug. When she did, she got a shock.
Despite having prescription drug coverage through Medicare, the medication cost Blair $600 a month. She tolerated it well and liked the idea of taking something that might slow her disease. But the cost was eating away at her retirement savings. She did not feel much better taking the drug, so she stopped it. In doing so, Blair joined the 45 million Americans who forego medications because they are too expensive.71
To be sure, developing safe and effective drugs requires a huge investment. The Tufts Center for the Study of Drug Development and its collaborators estimate that the research and development costs for a new therapy are as high as $2.6 billion.72 Other estimates are lower but of similar magnitude.73 Regardless of the exact numbers, drug development is a risky business. Up to 90% of drugs that show benefit in laboratory animals and are then tested in humans fail.74
Some drugs have enormous health and economic value. Drugs for HIV changed the infection from a death sentence into a manageable disease. As we know, drugs can cure infectious conditions and even some cancers. In the absence of other treatments, many of these medications justify their high price. The problem is that in the United States, most do not. Instead, pricing is based on what pharmaceutical companies can charge in a very imperfect market.75 And when their prices are astronomical—justified or not—Medicare and other insurers do not pick up enough of the cost.
The 2019 closure of Medicare’s “doughnut hole,” a previous gap in the program’s coverage of expensive drugs, will help some.76 The real solution is universal health insurance coupled with caps on total expenses that patients pay. If someone is sick and a highly effective therapy is available, a country that is as wealthy as ours can afford to cover the cost of that therapy.
For high-priced therapies that offer the promise of great benefit, new models are emerging. One, for example, requires insurers to pay only if a drug works (e.g., a cancer therapy cures cancer).77 Highly effective treatments for Parkinson’s should reduce the estimated $25 billion annually that is spent on medical care, mostly by Medicare, for the disease. A cure, of course, would eliminate such expenditures.
To lower overall drug spending, Medicare (paid for by taxpayers) could use its purchasing power to negotiate lower prices, especially for drugs that have high prices but only modest value.78 In addition, generic drugs should be permitted rapid entry once drug patents expire, and anticompetitive behavior that delays entry should not be tolerated.79 All these approaches have limitations, but new ideas and more work are needed to ensure that future effective therapies for Parkinson’s can help everyone.
EXTENDING LEVODOPA’S REACH
Even current inexpensive medications—the generic levodopa can cost as little as $11 a month—are unattainable for most patients.80 The main reason is that the drug is not available in all countries. A 2004 report by the World Health Organization found that 40% of countries lacked access to levodopa, still the gold standard treatment.81 Not surprisingly, access varied by a country’s income. While 84% of high-income countries had access to levodopa, only 17% of low-income countries did.
The World Health Organization includes levodopa on its list of “essential drugs.”82 The list is supposed to help countries and their departments of health prioritize their spending on medicines.83 However, many countries have yet to make purchasing levodopa a priority.
Given limited access to medications for Parkinson’s, individuals in some countries are left to utilize alternative sources for levodopa. It turns out that a bean plant called Mucuna pruriens is an excellent source of the dopamine precursor. The plant (Figure 2) is found in many tropical and subtropical areas where access to medications is limited, and in some countries, such as India, it is used as a treatment for Parkinson’s.84 Clinical trials suggest that Mucuna pruriens may have comparable benefits to medical preparations of levodopa.85 However, the plant is not available everywhere levodopa is needed. Over-the-counter formulations are available in the United States, but dosing and formulations are widely variable. In addition, levodopa alone can cause nausea and other side effects. In most medical formulations, levodopa is combined with another drug to reduce these side effects. Fifty years after its development, we need to ensure that the miraculous levodopa is available to all.