Proteins play a myriad of roles in your body. Not only do they serve as building blocks for many of your tissues, but as enzymes, they catalyze the billions upon billions of reactions taking place inside you every second. Proteins consist of hundreds or thousands of smaller units called amino acids, and the order in which these amino acids are strung together dictates a protein’s function. Your body uses 20 different amino acids to make thousands of proteins and polypeptides (small strands of amino acids) that do such wondrous things as stimulate growth (somatotropin), metabolize sugars (insulin and glucagon), tell you when you’re hungry and sated (ghrelin and cholecystokinin), and help you achieve orgasmic bliss (oxytocin). Nine of the amino acids that we humans use to make proteins must be consumed in the diet because we are incapable of producing them—these nine are referred to as essential amino acids.
While most of the average human’s body is actually water, a considerable chunk (15–20 percent) is protein. To get all this protein into you, your gut must first digest intact proteins from food. This process is sort of like taking apart a sectional couch so that it can get through the front door of your house and then reassembling it once it’s in your living room. Along the same lines, your gut must first deconstruct proteins until they are small enough to be absorbed through your intestine’s epithelial cells. Once inside you, most of these remnants of digestion eventually get repackaged into intact proteins.
You might recall from Chapter 1 that your stomach is a hot spot of protein digestion. Pepsinogen is secreted from specialized cells there, and its discharge is accompanied by the release of hydrochloric acid, which converts pepsinogen to pepsin. Hydrochloric acid also unravels proteins, which allows pepsin to split apart proteins into smaller molecules. Upon arriving in your small intestine lumen, the pancreatic enzymes trypsin and chymotrypsin continue working on the intermediates of protein digestion (polypeptides and peptones) until they are obliterated into individual amino acids or very small peptide chains. (Figure 6.1 provides an overview of protein digestion.)
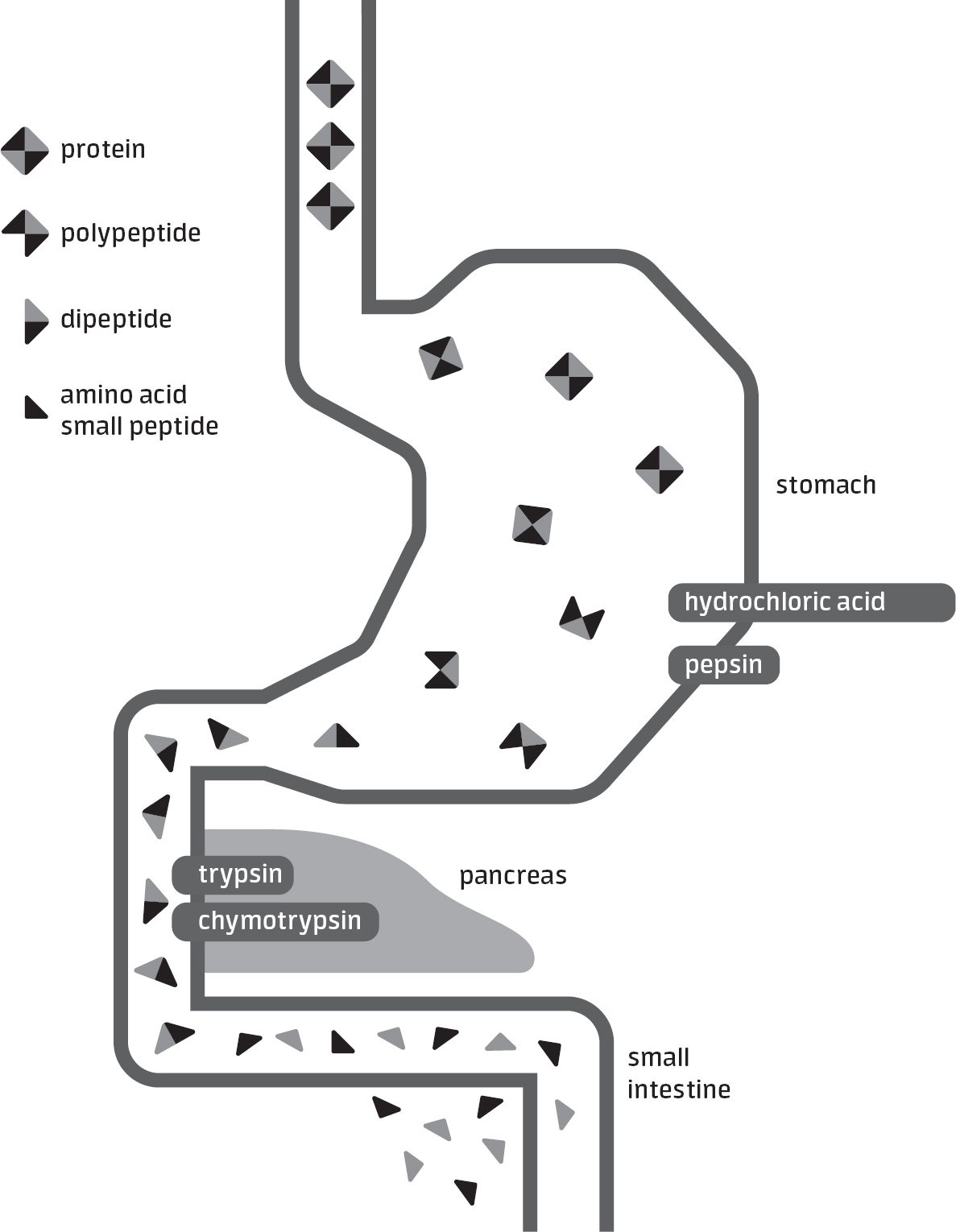
figure 6.1PROTEIN DIGESTION

The digestion of protein kicks off in the stomach via hydrochloric acid and the enzyme pepsin and continues in the small intestine through the actions of several enzymes released from the pancreas.
The aim of this chapter is to identify the ways in which ingesting protein affects your gut. In addition, given the popularity of protein and amino acid supplements, I also detail how these products can impact gut symptoms.
PROTEIN CONSUMPTION BEFORE EXERCISE
When it comes to eating protein before a game or race, the American College of Sports Medicine states that foods high in protein may need to be avoided to prevent gut issues.1 However, this recommendation is based largely on theoretical grounds. Specifically, researchers and practitioners who recommend avoiding protein before exercise usually claim that it impedes stomach emptying, but, in truth, different types of protein vacate from the stomach at different rates. Intact milk protein and solid forms of animal protein (beef, chicken, etc.), for instance, typically leave from the stomach more slowly than processed sources like whey, and therefore may be more likely to cause upper gut problems if eaten in close proximity to exercise.
There are anecdotal accounts of athletes eating large amounts of protein before competition and experiencing gut distress. In one such case, Scottish-American runner Jock Semple ate a thick, juicy steak an hour or so before the 1934 Boston Marathon; despite being considered a favorite to win, things did not go swimmingly for Semple, thanks in large part to crippling nausea. To be clear, few studies have fed athletes relatively large amounts of protein before exercise and quantified its effects on gut symptoms or rates of gastric emptying. One such study, though, conducted out of the University of Otago in New Zealand, provides some justification for the recommendation to avoid loads of protein.2 For the study, basketball players were fed meals 90 minutes before completing a high-intensity, 90-minute basketball-specific exercise protocol on two occasions. On one occasion, the players consumed a roughly 600 kcal meal that had a measly 6 grams of protein, while on the other occasion, the 600 kcal meal contained a hefty 69 grams of protein, primarily in the form of whey. Notably, athletes experienced more nausea and burping during exercise after they consumed the high-protein meal, although the symptoms didn’t seem to be severe enough to impact sprinting and jumping performance.
Obviously, 69 grams of protein is a whopping dose (it’s almost as much as what the average American eats in an entire day), so it would be unfair to extrapolate these findings to situations where athletes consume moderate portions of protein. Take for example an investigation of female cyclists which found that consuming a dairy-based meal with about 35 grams of protein didn’t lead to more gut discomfort during 90 minutes of cycling than a nondairy meal that contained about 12 grams of protein.3 Of note, the meals were consumed approximately two hours before cycling, which should have provided sufficient time for much of the food to exit the participants’ stomachs. Undoubtedly, dosage and timing of ingestion are important factors that determine how well your gut will respond to pre-exercise protein consumption. Eating a jumbo-sized serving of protein-rich food 30 to 90 minutes before intense exercise—much like Jock Semple did—is basically asking for nausea and reflux. But consuming more moderate doses (say, 20–40 grams found in 10 ounces of low-fat Greek yogurt or 4 ounces of chicken breast) two to four hours before exercise seems unlikely to induce gut problems in most athletes.
There may also be a potential downside to completely avoiding or heavily restricting protein prior to exercise: increased hunger. On a per-gram basis, protein elicits somewhat greater feelings of fullness and declines in hunger than carbohydrate.4 As a result, athletes who eat their final meal three to four hours before exercise may end up feeling famished if they choose a high-carbohydrate meal that’s also very low in protein. This problem may be further exacerbated if the athlete also curbs fiber intake, which also increases satiety. While limiting fat, fiber, and protein to modest amounts one to two hours before competition is a prudent approach to preventing gut issues, the recommendation to drastically restrict these nutrients for three to four hours beforehand is probably overkill.
Like other nutrients, the likelihood that protein will give you gut troubles depends on a host of factors including the type, quantity, and timing of ingestion, as well as the intensity and duration of exercise you engage in. Accordingly, each athlete should experiment during training to determine how these factors influence their gut symptomology. If eating solid protein like chicken, fish, beef, or tofu one to four hours before exercise causes you considerable gut issues, you might consider switching to faster-digesting sources like whey or soy protein supplements or simply eating those same foods well in advance of exercise. Also, the presence of large food particles in the stomach can modestly slow gastric emptying,5 so make sure to chew well when you’re eating solid protein-rich foods in close proximity to exercise. (It turns out your mom’s scolding reminders to chew your food served a purpose after all!)
PROTEIN CONSUMPTION DURING EXERCISE
During the 19th century and even into the early 20th century, many scientists believed that protein breakdown was what primarily fueled physical work, an idea popularized by German chemist Justus von Liebig.6 This view originated, in part, from his observations that the analysis of animal muscles failed to reveal any trace of fat or carbohydrate. As a result, protein recommendations at the turn of the 20th century were quite high for the average man, ranging from 110 to 150 grams per day depending on activity levels.7 (That’s roughly what you’d get from eating an entire 16-ounce sirloin steak from Texas Roadhouse.) As time went on, work from a variety of physiologists and chemists challenged Liebig’s views, and today it’s widely acknowledged that protein contributes to only a small fraction (a few percent) of the energy needed for exercise. A poorly fueled athlete who engages in prolonged exercise may see this relative contribution of protein increase to 10–15 percent near the end of exercise,8 yet even during the most arduous endurance events, fat and carbohydrate supply the lion’s share of the ATP needed for muscular contraction.
Because protein isn’t a primary source of fuel during exercise, it isn’t surprising that most contemporary physiologists focus on carbohydrate ingestion as a strategy for improving endurance. Nevertheless, protein ingestion during exercise has received an increasing amount of scientific attention, and although several experiments have shown improvements in endurance when protein is added to carbohydrate beverages, these benefits were likely due to the extra energy and not the protein itself.9 In fact, investigations comparing carbohydrate drinks against carbohydrate-protein drinks have consistently found that the addition of protein offers no performance edge when the energy content of the beverages is matched.
On the other hand, these studies haven’t shown any detriments from adding a little protein to a sports drink, and even suggest there’s a benefit if you’re ingesting carbohydrate in smaller amounts (less than 30–45 grams per hour). Furthermore, adding some protein to a sports beverage could speed post-exercise recovery. It’s worth noting that the majority of studies adding protein to sports beverages used whey, in large part due to its solubility in water; therefore, athletes looking to use this strategy should probably stick with preformulated beverages or use whey if they plan to make their own concoctions.
CHRONIC HIGH-PROTEIN DIETS
The current minimum recommendation for daily protein intake from the Institute of Medicine is 0.8 grams per kilogram of body mass, or just under 0.4 grams per pound. For a 150-pound runner, that equates to a little over 50 grams of protein per day, or about an 8-ounce chicken breast’s worth. For a 250-pound footballer, that equals 90 grams of protein, or roughly the amount in a 12-ounce steak. To put these numbers in perspective, most American adults consume somewhere between 50 and 100 grams of protein per day.10
Regrettably, the Institute of Medicine’s recommendation for protein is almost certainly suboptimal for a few populations, including athletes. (Note that this isn’t because a huge amount of protein is burned during exercise, as Liebig thought, but is instead largely due to an increased demand from tissue remodeling and building.) Based on an array of research since the Institute of Medicine came up with its initial guidelines, it’s now recognized that intakes of 1.2–1.6 grams of protein per kilogram of body mass (or roughly 0.5–0.7 grams per pound) are more optimal for serious athletes, individuals losing weight, and perhaps even the elderly.11 That’s not to say that eating an amount closer to the Institute of Medicine’s recommendation will cause someone to literally wither away, but it does mean that some people are losing out on important health and performance benefits because of a dietary protein shortfall.
What are these benefits of consuming additional protein above the Institute of Medicine’s recommendation? To be sure, there’s ample science showing that, at least in the short term, high-protein diets help people shed extra pounds, sometimes even more effectively than other energy-restricted diets.11 Moreover, elevating protein intake aids in the retention of lean body tissue as one loses weight. As an example, a 2010 study examined the effects of differing protein intakes while athletes followed one of two energy-restricted diets for two weeks.12 A group consuming 1 gram of protein per pound of body weight lost significantly less lean tissue as compared to a group that ate only 0.45 grams of protein per pound.
Despite some potential advantages of protein-abundant diets, there are concerns that these regimens could be detrimental to your gut over the long term. When people drastically up their intakes of protein, consumption of either carbohydrate or fat is sometimes pared down. Carbohydrate is curtailed more heavily than fat in many of these cases, and as a result, intakes of fiber and other fermentable carbohydrates can drop quite dramatically. When fewer of these fermentable carbohydrates make it to your colon, the populations of microorganisms there begin to shift, leading to changes in the metabolic milieu of the large bowel.
In one study, feeding obese men a high-protein, low-carbohydrate diet for four weeks reduced the amount of butyrate appearing in their stools;13 remember, butyrate is a by-product of carbohydrate and fiber fermentation in the gut, and, as it so happens, it’s an important energy source for your intestinal cells and may even promote the death of colorectal cancer cells. Interestingly, including moderate amounts of carbohydrate in the diets (181 grams) was enough to offset much of this decline in butyrate production. The high-protein diets used in this study also amplified the appearance of so-called N-nitroso compounds in the stool, which are known carcinogens. While these sorts of short-term studies cannot tell us whether these metabolic changes lead to more cases of colon cancer or other gut problems, individuals following high-protein diets should think about including at least modest amounts of carbohydrate and fiber in their nutritional plans.
You might also be wondering what impact loading up on protein has on the incidence and severity of gut symptoms. Regrettably, this is an area bereft of research. This isn’t because of a lack of studies on high-protein diets, but is instead due to their failure to collect meaningful information on gut symptoms. Despite the limited data, a handful of studies suggest that several gut symptoms are more prevalent on high-protein diets. In a study published in the Journal of the American Medical Association, bloating and fullness were twice as prevalent (12 percent versus 6 percent) when participants were on a higher-protein diet (about 25 percent of energy) than when they followed either a carbohydrate-rich diet or a diet rich in unsaturated fats.14 That said, most of the extra protein came from dairy and plant sources (legumes, nuts, seeds, etc.), so it’s possible that other components of these foods (lactose and fiber, for example) could have triggered the bloating. Another study, published in the Annals of Internal Medicine around the same time, found that in comparison to those following a low-fat diet, overweight adults who were following a very-low carbohydrate, high-protein diet (which contained about 30 more grams of protein on average) experienced more constipation (68 percent versus 35 percent) and diarrhea (23 percent versus 7 percent).15 It’s nearly impossible to tell if these bowel problems were due to the additional protein, additional fat, or because the low-carbohydrate diet was also likely lower in roughage. Perhaps the most likely explanation is that these extra gut symptoms arose from a combination of these factors.
At the end of the day, the effects of a high-protein diet on gut symptoms depend on which foods and supplements are consumed to boost protein intake, as well as which foods are restricted as a consequence of including extra protein in the diet. Dramatically increasing the consumption of protein-rich milk and yogurt, for example, could increase bloating and flatulence in a person who is lactose intolerant. Likewise, even though they’re relatively good sources of protein, eating loads of garbanzo and kidney beans could trigger gas and bloating because they’re also rich in fermentable fibers. For these reasons, athletes considering adding extra protein-rich foods to their diets should put some serious thought behind the sources of protein they choose, as well as the gut symptoms they’re most concerned with preventing or managing. If constipation is your main concern, following a meat-laden, low-carbohydrate, low-fiber diet is probably not your best choice. Alternatively, eating an abundance of legumes, nuts, and seeds may not be the best approach if you wish to avoid gas and bloating.
PROTEIN SUPPLEMENTS
Besides vitamins and minerals, protein is one of the most widespread types of supplements used by athletes. Gym bros and bodybuilders are not the only ones crushing protein supplements these days, as one analysis of surveys published in the journal Sports Medicine estimated that 25–49 percent of all male athletes and 7–22 percent of female athletes use protein supplements, and an additional 10–15 percent use individual amino acid supplements.16 Probably the most popular protein supplement is whey. As it relates to gut function, whey empties from the stomach rather rapidly, whereas other supplemental forms like casein tend to leave somewhat more slowly (casein curdles in the acidic environment of the stomach, which delays emptying).17 Regardless of how quickly they’re digested and absorbed, most supplemental forms of protein are well tolerated and have relatively few digestive side effects.
One exception to this general rule is if an athlete is lactose intolerant and consumes a large amount of whey protein concentrates. Because whey comes from milk, it typically contains lactose and can trigger symptoms like gas, bloating, and loose stools in those of us who aren’t efficient at breaking down lactose. For lactose-sensitive athletes, whey protein isolates are a better choice because they have undergone additional processing that removes almost all lactose.
Beyond whey concentrates, another possible gut-offending category of supplements is that of amino acid products like arginine and branched-chain amino acids. Arginine serves as a precursor for nitric oxide synthesis, and because nitric oxide regulates blood flow in tissues such as the skeletal muscle, arginine is frequently used as a pre-workout supplement in an attempt to, as your typical gym bro would say, “get my muscle pump on.” Despite the positive anecdotes you may hear at the gym, much of the research on arginine and athletic performance is lackluster.18 In addition, clinical trials that have rigorously collected information on the adverse effects of arginine supplements often report diarrhea as a side effect, particularly when 9 grams or more are taken in a single sitting.18, 19
Branched-chain amino acids are another popular supplement used by serious athletes and weekend warriors alike, and as with arginine, the hype surrounding them exceeds their true benefits, at least in terms of muscle-building potential.20 And just as with arginine, side effects like diarrhea and nausea have been reported in some studies of branched-chain amino acids.21, 22