![]()
HYPNOTIC ANALGESIA: PSYCHOLOGICAL AND NEURAL MECHANISMS
![]()
THOUGH THERE IS no question that the phenomenon of hypnotic analgesia is real, there continue to be intriguing questions about its nature: How does hypnotic analgesia work? What is the psychological mechanism of its action? What is the biological mechanism of its action? What does knowledge of the mechanisms tells us about its use in clinical circumstances? Inquiry into these questions has absorbed and challenged investigators for some time. Their work has been fruitful and their questions have begun to yield answers. This chapter explores these questions, the method of their scientific investigation, and the clinical implications of answers that have emerged thus far.
Studies of hypnotic analgesia have labored under a double burden. Both the independent variables of hypnotic treatments and the multiple components of pain experience, which are the dependent variables, are subjective phenomena. Partly as a consequence, measurements of subjective independent and dependent variables of hypnotic analgesia experiments are seen as lacking the precise control that may be present in physiological or pharmacological studies.
This chapter presents an alternative view of the possibility of precise analysis and measurement of both the independent and dependent variables of hypnotic analgesia studies. In the context of providing this alternative view, a preliminary explanation of the neural and psychological mechanisms that may underlie hypnotic analgesia will be presented. Finally, the implications of understanding the neural and psychological mechanisms of hypnotic analgesia for the treatment and management of clinical pain will be elaborated.
THE INDEPENDENT VARIABLES OF HYPNOTIC ANALGESIA
The logistics and intent of hypnotic analgesic interventions are sometimes quite simple, particularly for acute pain. The clinician induces a hypnotic state in the patient, makes suggestions for reduced pain or the absence of pain, and then both the clinician and patient enjoy the consequences of hypnotically induced pain control. The problem becomes enormously complicated the moment one begins asking questions about the factors that evoke and maintain pain reduction, as well as about the nature of the pain reduction itself. The factors that evoke pain reduction range from psychosocial, including interactions between clinician and patient, to psychophysiological ones that influence the actual transmission of pain signals within the patient. The factors that maintain pain reduction differ; they seem to be largely dependent on an interaction among the patient’s personality, environmental contingencies, and the efficacy of treatment. It is these factors and their relationships that effective treatment must address, even more than basic factors such as nociception.
The following discussion will consider: (1) the demand characteristics of the hypnotic analgesia situation; (2) the role of the hypnotic state; and (3) the possible interactions between hypnotic state and incorporation of hypnotic suggestions.
This discussion will be followed by a consideration of how hypnotic interventions influence the multiple dimensions of pain and, at least in a general sense, the neurophysiological processing of pain.
Demand Characteristics and Role Enactment Theory
One school of thought about the nature of hypnotic analgesia is that this phenomenon merely represents compliance with demand characteristics of the experimental or clinical situation and does not involve a genuine alteration in an individual’s experience of pain. This model suggests that, after being given hypnotic induction and suggestions, subjects or patients cognitively relabel their reports of pain as less intense not because they perceive them to be less intense but because social expectations require that they act in the role of someone who has less pain (Spanos, 1986). In other words, while they continue to feel pain, they pretend that they do not.
There are two interrelated claims in this explanation. The first is that the hypnotic situation does not create a change in state of consciousness and that such a change is not required to respond to hypnotic suggestion. The second related claim is that there is nothing special about the hypnotic response of reducing one’s pain rating. This response does not necessarily involve an actual reduction in pain, but rather a willingness to invent lowered ratings to describe unaltered sensory pains, in order to behave “as” if one were actually experiencing less pain. According to the “role enactment” theorists, the elaborate process of hypnotic induction serves only to strengthen the demand characteristics of the situation and encourage subjects to follow instructions and emit the desired behavior. (A corollary assumption underlying this theory is that self-report is an unreliable means of knowing what an individual is experiencing.)
Support for the claim that change in state of consciousness is neither necessary for nor contributory to hypnotic analgesia comes from studies that show no difference in analgesia levels between two groups of subjects given analgesia suggestions, with and without an induction of a hypnotic state (T. Barber & Hahn, 1962; T. Barber & Wilson, 1977; Evans & Paul, 1970). On the other hand, there are considerably more studies that demonstrate that greater analgesia occurs when subjects experience a hypnotic state, and that hypnotic responsivity is at least somewhat predictive of hypnotic analgesia (see references in Hilgard & Hilgard, 1994).
The related claim that hypnotically induced reports of reduced pain do not necessarily reflect actual reductions in perceived pain is perhaps best supported by observations that physiological responses to pain, such as increased heart rate and blood pressure, often still occur at the same time hypnotized subjects provide reports of greatly reduced pain (Hilgard & Hilgard, 1994). This issue will be further discussed when we consider dependent variables of hypnotic analgesia.
The Role of a Hypnotic State in Hypnotic Analgesia
If a hypnotic state is not required to evoke reductions in pain report, and if subjects of hypnotic analgesia experiments are simply enacting an elaborate role, then subjects who are deliberately instructed to simulate analgesia—to pretend not to hurt—should be able to tolerate intense pain—while pretending that they do not hurt—as well as those who undergo the allegedly unnecessary ritual of hypnotic induction.
An elaborate experiment designed to test this hypothesis was carried out by Greene and Reyher (1972). They randomly assigned highly responsive subjects to the hypnotized and simulating groups. They instructed the simulators to remain unhypnotized, while deceiving the experimenter into believing they were hypnotized. They were also told to react to the painful stimulus as if they were analgesic. Increasing intensities of electric shock served as the painful stimuli, and pain tolerance and pain intensity reports served as dependent measures.
Despite the attempt to behave like hypnotized subjects while not, in fact, hypnotized, the simulators were clearly less tolerant of the pain during each of the several experimental conditions than were the hypnotized subjects. For example, the hypnotized and the simulators increased their tolerance of pain by 45 percent and 16 percent, respectively, a difference that was statistically highly reliable. Apparently, the shocks were more bearable for the hypnotized than for the equally responsive, but unhypnotized, role enactors. This experiment and similar others cast doubt on the idea that hypnotized subjects feel pain but report less pain to satisfy the demand characteristics of the situation.
Interactions Between a Hypnotic State and the Incorporation of Hypnotic Suggestions
Since it is clear that a hypnotic state is not in itself sufficient to produce analgesia, and since there is reasonable evidence that analgesia is greater in the context of a hypnotic state than without one (Hilgard & Hilgard, 1994), it is reasonable to conclude that a hypnotic state facilitates the analgesia induced by suggestions. This brings us to the general question of how a hypnotic state does this.
Two investigations have directly addressed this question. In the first (Price & Barrell, 1990), a group of 21 graduate students and faculty members participated in an experiential-phenomenological study of the common elements that comprise the experience of a hypnotic state, using the approach and method the investigators had previously described (Price & Barrell, 1980). First, through direct experience of several hypnotic inductions, each participant-observer identified the common elements that were present in most or all inductions used for analysis. Second, a group consensus identified the common elements that were necessary or sufficient for a hypnotic state. These elements included the following:
1. a feeling of relaxation (a letting-go of tensions or becoming at ease)
2. an absorbed and sustained focus of attention on one or a few targets
3. an absence of judging, monitoring, and censoring
4. a suspension of usual orientation toward time, location, and/or sense of self
5. experience of one’s own responses as automatic (i.e., without deliberation and/or effort)
It was evident from descriptions of the observers’ direct experiences of the hypnotic state that some of the common elements were necessary for the emergence of other elements and that, in general, strong interrelationships existed among these elements. Thus, element 1 (“relaxation, becoming at ease”) appeared to provide a supportive general background for element 2 (“absorbed and sustained focus”), which in turn appeared to affect elements 3 (“absence of judging, monitoring, censoring”) and 4 (“suspension of usual orientation toward time and location”). The latter two elements, in turn, appeared to maintain element 5 (“automaticity”). Finally, it was agreed by all observers that elements 4 (“suspension”) and 5 (“automaticity”) directly contributed to perceived hypnotic depth. A tentative model of these interrelationships was then formulated as shown in Figure 4.1A.
This model was subsequently tested in a second study in which 62 participants rated their perceived magnitudes of these elements on visual analogue scales during normal waking, mild, and deep hypnotic states (Price, Barber, & Harkins, 1988). As can be discerned from Figure 4.1B, path analysis provided at least a general statistical confirmation of the validity of the model. Only the hypothesized influence of element 3, “lack of monitoring,” on element 4, “disorientation,” was not confirmed. The experiential and conceptual basis for this model is generally supported by the work of others who have independently arrived at many of these same common elements (Bowers, 1978; Pekala & Kumar, 1984).
Returning then to the question of how a hypnotic state facilitates the incorporation of suggestions for analgesia, this model implicitly provides a basis for increased responsiveness to suggestion that is unique and distinguishable from other types of psychologically mediated increases in responsiveness to suggestion (e.g., placebo). This basis is directly evident in the phenomenology of the interrelationships between the common elements of this model and can be described as follows:
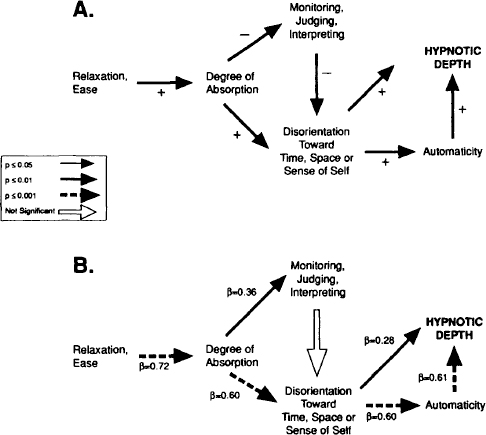
FIGURE 4.1. Models of How a Hypnotic State Facilitates Analgesia Induced by Suggestions
A hypnotic state begins with an absorbed and sustained focus on something. It can occur naturally during periods of fascination, for instance while watching an absorbing movie or ripples in a stream. The experience captures us. At first, it may take effort to develop this absorption. With time, however, one proceeds from an active form of concentration to a relaxed, passive form.
There is often (though perhaps not necessarily) an inhibition or reduction in the peripheral range of one’s experience. At the same time, this relaxation and/or reduction in range of attention supports a lack of monitoring and censoring of that which is allowed into one’s experience. Hence, inconsistencies are now more tolerable. Contradictory statements, which once arrested attention and caused confusion or disturbance, now no longer do so. The uncensored acceptance of what is being said by the hypnotist is not checked against one’s own associations. Consequently, one no longer chooses or validates the correctness of incoming statements. This allows thinking and meaning-in-itself that is disconnected from active reflection.
From this way of experiencing, there emerges the sense of automaticity, wherein thought doesn’t precede action but action precedes thought. Thus, if the hypnotist suggests a bodily action, a sensation, or a lack of sensation (e.g., analgesia), there is no experience of deliberation or effort on the part of the subject. The subject simply and automatically identifies with the suggested action, sensation, or lack of sensation, whatever is suggested. The possibility of not carrying out the action or experiencing the suggested changes in sensation is not considered, or is considered very little. In this way, a hypnotic state facilitates the incorporation of suggestions, including that of analgesia.
It must be noted that the automatic identification with the suggested action or sensation (or lack thereof) that occurs during the hypnotic experience shares some common principles with other types of psychologically mediated forms of responses to suggestion. To take just one of many possible examples, Kojo (1988) has suggested that the imagination of heat evokes actual increases in blood flow and skin temperature by creating a psychological set wherein the subject allows the feeling of warmth to be there without deliberation or effort.
It may well be that what is unique about hypnotic suggestions is not the effect of the suggestions themselves, such as pain relief, but the way in which the suggestions implicitly or explicitly refer to the source of experiential change—it is both effortless and automatic. This deceptively simple idea may, in fact, provide a rich source of understanding by clinicians of how to create effective suggestions for analgesia.
This uniqueness can perhaps be illustrated by comparing the nature of hypnotic suggestions with those that occur during placebo administration. The “suggestion” provided in the case of placebo analgesia can readily be distinguished from that provided during hypnotic analgesia, in that the former refers to an outside authoritative source as the origin of the pain relief. For example, injections or tablets provided by a health-care professional indicate that the agency of therapeutic relief comes from a medicine and a person experienced in the knowledge of the efficacy of the treatment. Within the placebo literature, there exists considerable evidence that greater placebo effects are achieved by more believable and technically convincing agents. Thus, placebo injections are more effective than placebo pills, and placebo morphine is more effective than placebo aspirin (Traut & Passarelli, 1957).
Implicit in the overall suggestion inherent to a placebo analgesic manipulation is the idea that in the absence of this outside authoritative agent there would be unrelieved pain. The nature of hypnotic suggestions for analgesia, on the other hand, refers to a more innate and self-directed capacity to alter one’s own experience, often to the effect that one can experience sensations differently and including the possibility that there is no pain to be experienced (Barber, 1982). The source of experiential change, in the case of hypnotic analgesia, is perceived as occurring automatically and from within.
This experiential distinction between hypnotic and placebo analgesia may at least partly account for the complete lack of relationship between the magnitude of hypnotic analgesia and the magnitude of placebo analgesia tested in subjects of both high and low responsiveness (Hilgard & Hilgard, 1994). It has been determined that, for subjects not responsive to hypnotic suggestions, about the same modest degrees of analgesia are achieved through hypnotic suggestion and placebo administration. For highly responsive subjects, pain reduction evoked by hypnotic suggestion is far greater than the negligible or even negative effects produced by placebo. Therefore, hypnotic analgesia is more than a placebo and very likely different with respect to psychological mechanisms.
The considerations raised so far indicate that multiple factors within the psychosocial context and within the experience of subjects influence the alteration of pain as a result of hypnotic suggestions for analgesia. The influences of individual factors on responses to various types of hypnotic suggestion—other than hypnotic responsiveness perse—have received relatively little explicit recognition. However, the relative influence of elements within the hypnotic state on analgesic responses to suggestions could be tested in experiments wherein participants provide judgments of their experienced magnitudes. For example, self-ratings of such elements as “automaticity” and “depth of hypnotic state” could constitute independent variables in investigations of the relationship between depth of hypnotic state and responsiveness to analgesic suggestions.
THE DEPENDENT VARIABLES OF HYPNOTIC ANALGESIA
The suggestions for alteration of the experience of pain in studies of hypnotic analgesia relate closely to the dimensions of pain and to the psychological stages of pain processing. Thus, there are suggestions that specifically target the affective dimension of pain as distinguished from the sensory dimension. These include suggestions for reinterpreting sensations as pleasant rather than unpleasant or for reducing or eliminating the implications of threat or harm from the sensations. Then there are suggestions designed specifically to alter the quality and/or intensity of sensations so that they become less painful, not at all painful, or absent altogether. These include suggestions for substituting sensations of numbness, warmth, or other sensations for that of pain and suggestions for the complete absence of sensation. The latter include suggestions for dissociation, wherein subjects do not feel parts of their bodies that would otherwise be painful or subjects experience themselves in another location and context altogether. In addition to studies to assess the role of hypnotic depth and individual components of hypnosis on pain, we need studies of differential effects of various types of suggestion on sensory and affective dimensions of pain experience. For example, what are the effects on pain of suggestions exclusively designed to reinterpret the meanings of the sensations so that they are less threatening or unpleasant?
Just as there exist multiple psychological dimensions that contribute to hypnotic analgesia, analgesia itself is also likely to be comprised of multiple dimensions. As Barber described in Chapter 1, the experience of pain has both sensory and affective dimensions. The strategy discussed above for characterizing and measuring the factors in hypnotic treatments could be interfaced with one that assesses how these factors influence the different dimensions of pain, as well as the different neurological stages of pain processing (i.e., spinal, cortical, etc.).
Maximizing this strategy requires accurate, sensitive, and valid methods of pain measurement. This may be accomplished by using pain measurement methods that fulfill criteria for ideal pain measurement (Gracely & Dubner, 1981; Price & Harkins, 1992b). Direct magnitude scaling of sensory and affective dimensions of pain would seem essential, especially if hypnotic suggestions differentially influence the two dimensions of pain. Tursky (1985) has recommended the use of more sophisticated scaling methods and has identified the deficiencies of certain quantitative methods as they relate to the assessment of analgesia.
Since pain is comprised of sensory and affective dimensions, a number of questions can be raised about how a hypnotic intervention influences the various dimensions and stages of pain processing:
1. Does hypnotic analgesia reduce the affective dimension more than the sensory dimension of pain?
2. To what extent does hypnotic analgesia involve descending inhibition of pain transmission at spinal cord levels or intracortical mechanisms that prevent awareness of pain?
3. Does hypnotic analgesia utilize an endogenous opiate system?
As surprising as it may seem, these questions are at least partly answerable in experiments that utilize multiple measures of pain experience and, in some cases, physiological indices of pain processing at different levels of the nervous system.
Differential Effects of Hypnotic Suggestions
on Sensory and Affective Dimensions of Pain
The question of whether hypnotic suggestion has differential effects on sensory and affective dimensions was addressed in an investigation of the factors that contribute to the magnitudes of reduction in pain following indirect hypnotic suggestions (Price & Barber, 1987). Two groups of human volunteers made responses on extensively validated visual analogue scales of sensory pain intensity (sensory VAS) and pain unpleasantness (affective VAS) to noxious skin temperature stimuli (44.5 to 51.5°C) before and after hypnotic suggestions were given for analgesia. Group 1 was given suggestions for developing a hypnotic state only once, just before analgesic testing, and did not have significantly reduced VAS responses to experimental pain after hypnosis. The experimenter remained with Group 2 and provided cues for maintaining a hypnotic state during their analgesic testing session. This group developed a 44.5 percent mean reduction in sensory pain intensity and a 87.4 percent mean reduction in affective pain. As shown in Table 4.1, the reduction in affective pain was much larger and more consistent across Group 2 subjects than the reduction in sensory pain intensity. A small but statistically reliable correlation was found between hypnotic responsiveness and overall magnitude of reduction in VAS sensory ratings but not VAS affective ratings.
It is not immediately apparent why hypnotically induced reductions in VAS affective ratings to experimental pain were greater and more consistent than reductions in VAS sensory ratings. Affective responses to experimental heat pain were reduced even in participants who had low responsivity scores and who showed very little change in perceived sensation intensities (see, for example, subjects 2 and 5 in Table 4.1). A possible answer to this question may be obtained through consideration of the nature of sensory and affective responses to experimental pain and of the degree of hypnotic involvement required to experience alterations in these pain dimensions.
Table 4.1
Hypnotic Susceptibility and Analgesia in Group 2
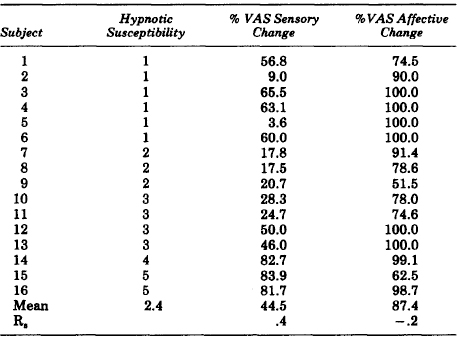
Affective responses associated with pain are more influenced by the perceived context of the experimental situation than are sensory responses (Price, 1988). Thus, factors related to the psychological context of the person can selectively and often powerfully reduce affective responses to experimental pain (Price, 1988; Price, Barrell, & Gracely, 1980). Hypnotic suggestions in this experiment were directed toward
1. experiencing the testing situation as more pleasant.
2. experiencing the heat stimuli as more pleasant.
3. experiencing the heat stimuli as less intense.
It is clear that these three alterations in experience would require different degrees of hypnotic involvement (Shor, 1965; Weitzenhoffer, 1957). Experiencing the testing situation and test stimuli as less unpleasant would require less hypnotic involvement than experiencing direct reductions in sensations evoked by noxious heat stimuli. In some instances, selective reduction in affect could occur without a hypnotic state. Therefore, one component of a hypnotic intervention may involve responses to suggestion for reduced unpleasantness that do not require a hypnotic state. This explanation is consistent with the result that reductions in unpleasantness were not at all correlated with hypnotic responsiveness.
The reduction in pain-related unpleasantness beyond that accountable by a simple reduction in sensory pain intensity, and in some cases without any reduction in sensory pain, is not likely the result of reduction of the pain signal at peripheral or even spinal levels. Rather, it is likely the result of alteration in the meanings that normally attend painful experience. As such, the selective reduction in affective pain by cognitive mechanisms is likely to reflect neural events at higher levels of pain processing, including intracerebral mechanisms.
MECHANISMS OF REDUCTIONS IN SENSORY PAIN INTENSITY
Although it is clear that hypnotic suggestions may exert a more powerful reduction of affective pain than of sensory pain, it is also quite apparent that both dimensions are reduced. This has been amply demonstrated in several experimental laboratories (see Hilgard & Hilgard, 1994, and Price, 1988, for reviews). Moreover, it is the reduction in sensory pain itself that is statistically correlated with hypnotic responsivity, albeit at modest levels. Therefore, the hypnotic intervention that relies on hypnotic ability and a hypnotic state is the one most influential in reducing sensory pain intensity. Interestingly, the correlation becomes stronger with increasing levels of pain intensity, as shown in Table 4.2.
It makes sense that reduction of more intense pain requires more hypnotic ability than reduction of less intense pain. However, the overall modest strength of correlation between hypnotic responsivity and sensory analgesia and the complete absence of a significant correlation between hypnotic ability and reductions in affective pain ratings (Table 4.2) strongly indicate that multiple factors are involved. When analgesia results from a hypnotic intervention, it can also include factors that are unrelated to hypnotic responsivity and even to a hypnotic state. Such potential multiple factors are closely related to different proposed mechanisms of hypnotic analgesia as discussed below.
Table 4.2
Hypnotic Susceptibility and Analgesia
| Stimulus Temperature | Spearman Correlation Coefficient | |
| Sensory Analgesia | Affective Analgesia | |
| 44.5°C | +0.04 | -0.23 |
| 47.5°C | +0.21 | -0.11 |
| 49.5°C | +0.43* | -0.08 |
| 51.5°C | +0.56* | +0.10 |
| * P < 0.01 | ||
Neodissociation and “Intracerebral” Mechanisms
At present, there are two general mechanisms by which sensory pain can be reduced in intensity during hypnosis. The neodissociation theory (Hilgard & Hilgard, 1994) proposes that during hypnotic analgesia there is reduced awareness of pain, which normally occurs when nociceptive information has reached higher centers. According to this theory, pain is registered by the body and by covert awareness during hypnotic analgesia, but it is masked by an amnesia-like barrier between dissociated streams of consciousness. This dissociation in awareness has been demonstrated through “automatic writing” and through the phenomenon of the “hidden observer” (Hilgard, 1977; Hilgard & Hilgard, 1994; Hilgard et al., 1975).
Hilgard and his colleagues (1975) instructed subjects to report covert levels of cold pressor pain through automatic key pressing ratings of pain while their overtly experienced pain produced by the same cold pressor was reported through magnitude estimation. The result was that during nonhypnotic suggestions for analgesia there was about a 40 percent reduction in both overtly and covertly reported pain intensity. Suggestions for analgesia after inducing a hypnotic state produced an additional reduction in overtly reported pain, but not in covertly reported pain. This additional reduction is said to reflect dissociative mechanisms that are available for manipulation only when a hypnotic state is induced. A component of the perception of pain may be immediately forgotten or otherwise diverted from conscious awareness.
This interpretation of hypnotic analgesia as a dissociation in consciousness suggests an explanation for the paradox that physiological indices of stress often continue during hypnotic analgesia, even though the subject consciously feels little or no pain. Interestingly, Hilgard and his colleagues found that, with highly responsive subjects, the rise in heart rate caused by cold pressor pain was somewhat less during the hypnotic experience than during waking nonhypnotic control conditions, but that some increase in heart rate still occurred (Hilgard & Hilgard, 1994). This partial reduction is consistent with Hilgard’s observation of two components of pain reduction (sensory and affective). The reduction of pain during nonhypnotic conditions may be accompanied by reductions in autonomic and reflex responses to pain, whereas the reduction in pain associated with dissociative mechanisms would not likely be accompanied by decreases in autonomic responses.
Descending Spinal Cord Inhibitory Mechanisms
A second general mechanism by which hypnotic suggestions could reduce pain is by activation of an endogenous pain inhibitory system that descends to the spinal cord, where it prevents the transmission of pain-related information to the brain. There are multiple lines of indirect evidence for and against such a mechanism.
The question of whether hypnotic analgesia involves a brain-to-spinal-cord descending control mechanism is indirectly related to another question: whether endogenous opiates mediate hypnotic analgesia. If they do, then it would be likely that a descending control system is involved, since it has been well established that opiate analgesic mechanisms rely heavily on a brain-to-spinal-cord descending control system. A number of observations indicates that hypnotic analgesia does not depend on endogenous opiate mechanisms. First, different groups of investigators have found that naloxone hydrochloride, an opiate antagonist, does not reverse analgesia produced by hypnotic suggestions. For example, Barber and Mayer (1977) found that hypnotic suggestions elevated pain thresholds produced by tooth-pulp stimulation, and that these elevations in threshold were completely unaffected by naloxone hydrochloride. Similar negative results were obtained by Goldstein and Hilgard (1975).
Other characteristic differences also exist between opiate analgesia and hypnotic analgesia. Once it is repeatedly established in a highly responsive subject, hypnotic analgesia can be induced again very quickly (sometimes within seconds) in the same subject, and can also be very quickly terminated. Endogenous opiate mechanisms, by contrast, typically have a delayed onset to maximum effect (e.g., several minutes), and the effect is predictably slow to dissipate.
However, the lack of demonstration of an endogenous opiate mechanism involved in hypnotic analgesia does not exclude the possibility of a descending control system, only the possibility of an opiate descending control mechanism. Nonopiate brain-to-spinal-cord descending control mechanisms are known to exist (Price, 1988).
Although physiological investigations have addressed the possibility that hypnotic analgesia involves a brain-to-spinal-cord descending inhibitory mechanism, nearly all studies have focused on autonomic (T. Barber & Hahn, 1962), neurochemical (Barber & Mayer, 1977; Goldstein & Hilgard, 1975; Mayer, Price, Barber, & Rafii, 1976), or electrocortical changes associated with hypnotic analgesia (Crawford & Gruzelier, 1992).
A limitation common to all of these studies is the difficulty of identifying the general neuroanatomical sites at which the relevant modulatory mechanisms take place. Evidence that hypnotic analgesia involves a descending inhibition at spinal levels could be simply provided if some measure of spinal nociceptive function and pain perception could be simultaneously provided during hypnotic analgesia. The feasibility of such an approach is strongly indicated by Wilier (1977, 1984, 1985), who has demonstrated that different types of somatosensory stimulation and attentional manipulations simultaneously reduce pain and the electrically evoked flexion reflex. He has also demonstrated that graded doses of morphine reduce the electrically evoked flexion reflex and pain intensity on a near equal percentage basis, thereby providing a standard for assessing descending pain inhibitory mechanisms. All of these observations suggest the possibility of simultaneous measurement of pain and the flexion reflex during hypnotic analgesia. Indeed, this idea may have originated in Hagbarth and Finer’s (1963) preliminary demonstration of marked suppression of the flexion reflex in a few subjects during hypnotic analgesia. Though this result is very interesting, its meaning is difficult to interpret, partly because the suppression of the reflex was demonstrated in subjects who were aware of the physiological response that was being measured (and may have, unwittingly, complied in a nonhypnotic fashion).
A more recent and extensive analysis of the question of a possible descending inhibitory mechanism of hypnotic analgesia was made by examining changes in the R-III, a nociceptive spinal reflex, during hypnotic reduction of sensory pain and unpleasantness (Kiernan, Dane, Phillips, & Price, 1995). The R-III was measured in 15 healthy volunteers who gave VAS sensory and VAS affective ratings of an electrical stimulus during conditions of resting wakefulness without suggestions and during hypnosis with suggestions for hypnotic analgesia. A critically important feature of this study was that subjects were blind to the physiological index being measured and, later, when informed that measurements were being made of the R-III flexion reflex, failed to intentionally reduce the magnitude of this reflex. (This controls for both expectancy and compliance effects that had not been controlled in the earlier demonstration by Hagbarth and Finer.)
Hypnotic sensory analgesia was partially, yet reliably, related to reduction in the R-III (R2 = .51, p < .003), suggesting that hypnotic sensory analgesia is at least in part mediated by descending antinociceptive mechanisms that exert control at spinal levels in response to hypnotic suggestion. Hypnotic affective analgesia was not quite significantly related to reduction in R-III (p = .053). Reduction in R-III was 67 percent as great as reduction of sensory pain, and accounted for 51 percent of the variance in reduction in the affective component. In turn, reduction in sensory pain was 75 percent as great as, and accounted for 77 percent of the variance in, reduction of unpleasantness.
The results suggest that three general mechanisms may be involved in hypnotic analgesia: The first, implicated by reductions in R-III, is related to spinal cord antinociceptive mechanisms. The second, implicated by reductions in sensory pain over and beyond reductions in R-III, may be related to brain mechanisms that serve to prevent awareness of pain once nociception has reached higher centers, as predicted by Hilgard’s neodissociation theory (Hilgard & Hilgard, 1994). That the percent reduction in sensory pain intensity was greater than that of the R-III is consistent with Hilgard’s and others’ finding that some autonomic responses to pain remain even under conditions of profound hypnotic analgesia. The third, implicated by reductions in unpleasantness above and beyond reductions in sensory pain, may be related to selective reduction in the affective dimension, possibly as a consequence of reinterpretation of meanings associated with the painful sensation, as previously suggested by Price and Barber (1987).
This study by Kiernan and his colleagues provides crucial confirmation that hypnotic analgesia (1) is a measurable psychophysiological phenomenon and (2) has measurable effects on spinal reflexes.
The analytic strategy provided in this study is very useful for two reasons: (1) It conceptualizes the possible multiple actions of a hypnotic pain control intervention; (2) it provides a strategy for independent evaluation of multiple stages of pain processing. Similar to the work of Hilgard and Hilgard (1994), this study shows that multiple components of pain reduction are produced by a single hypnotic intervention. Most critically, the study demonstrates that the hypnotic experience has some measurable effect on a person beyond that suggested by role-enactment theory.
CLINICAL IMPLICATIONS
Taken together, investigations about the psychological and neural mechanisms of reduction of pain by hypnotic interventions strongly indicate the existence of multiple factors and mechanisms. These mechanisms include factors that evoke the development of a hypnotic state and incorporation of suggestions for analgesia, as well as multiple dimensions of pain experience and behavior.
Future studies of hypnotic analgesia should be designed to better assess the experiential factors and psychosocial contextual factors that influence changes in self-reported pain intensity that occur as a result of a hypnotic intervention. New approaches and methods are available to measure experiential factors such as “perceived automaticity” and “degree of absorption” (cf. Bowers, 1978; Pekala & Kumar, 1984; Price & Barrell, 1990). Using these methods, the factors that optimally influence responses to hypnotic suggestions for analgesia could be identified and utilized by both patients and clinicians. The concept of “hypnotic therapeutic manipulations” could shift in emphasis from reliance on outside authority to the patient’s active participation in developing psychological conditions for therapeutic effects. (Many effective clinicians already utilize this concept, if only intuitively.)
More precise analysis of different components of hypnotic analgesic effects also has important therapeutic implications. These components include:
1. Selective reduction of pain-related affect (i.e., unpleasantness) through changes in the meaning of sensations and of the contexts in which they occur. It is possible that little or no hypnotic state is required for this type of influence, even though it may be an integral part of a hypnotic intervention.
2. Reductions in sensory pain by mechanisms that divert pain from conscious awareness once nociceptive information has reached higher centers. To the extent that this component is manifested within an individual, the normal somatomotor reflexes and autonomic, neuroendocrine, and neuroimmunological consequences of pain are not attenuated. Thus, stress-related reponses associated with pain still occur, often to the physiological detriment of the individual.
3. Inhibition of pain signals at the spinal level of processing. In contrast to the mechanism just described, negative physiological consequences of pain would be attenuated by this mechanism, since inhibition of pain signals would interrupt the supraspinal activation of brain structures involved in autonomic and neuroendocrine responses to pain.
Different individuals may utilize different proportions of these mechanisms, as has been suggested previously (Kiernan et al., 1995; Price, 1988). For example, considerably different proportions of reduction in both affective pain and sensory pain were found among subjects in the Price and Barber experiment (1987), as indicated in Table 4.1.
Knowledge about the prevalence of these multiple mechanisms and the factors that influence them has far-reaching implications for treatment of various medical conditions, as well as pain. For example, the discovery that reductions in affective pain are larger and more prevalent than reductions in sensory pain, and that such reductions in affective pain are unrelated to hypnotic responsiveness, suggests that a large percentage of people could benefit from a hypnotic intervention (rather than only highly responsive individuals). Furthermore, hypnotic responsiveness does not appear to be a critically limiting factor in determining which patients could benefit from a hypnotic intervention.
To take another example, suppose certain types of hypnotic suggestions or treatments optimally activate cognitive dissociative mechanisms, whereas others activate descending spinal inhibitory mechanisms. The latter may be accompanied by reduced physiological consequences of pain, such as reduced immune response and reduced healing time. This specific type of hypnotic intervention may have a significant therapeutic advantage over hypnotic mechanisms that only involve cognitive dissociative mechanisms or selective reductions in affective pain, since the latter two mechanisms would not reduce the centrally mediated physiological responses that accompany pain, such as release of stress-related hormones and cardiovascular response. Clearly, further precise analysis of factors that contribute to hypnotic analgesia, as well as the components of analgesic responses themselves, offer possibilities for improved therapeutic effects of hypnotic interventions.