
I present the philosophy, rationale, and benefits of eating Primal Blueprint style, emphasizing the importance of moderating insulin production and improving insulin sensitivity by limiting the intake of processed carbohydrates, which means not only sugars, but also cultivated grains (yep, even whole grains). This simple dietary modification—perhaps the single most critical takeaway action item from the Primal Blueprint—will allow you to avoid the unpleasant physical and mental effects of modern high-carbohydrate eating, succeed with long-term weight-loss goals, and prevent the most common lifestyle-related health problems and diseases.
You will learn why the conventional wisdom assertion that cholesterol is a direct heart disease risk factor is deeply flawed. The true culprits that trigger the development of atherosclerosis are oxidation and inflammation, created largely by the Standard American Diet of processed carbohydrates and refined industrial vegetable/seed oils and partially hydrogenated oils. I detail the dietary steps you can take to prevent systemic inflammation and virtually eliminate your risk of heart disease.
The concept of “eating well” means more than just making healthy food choices; it means eating sensibly and intuitively, in a relaxed environment conducive to maximum appreciation of food, and it means avoiding regimented, restrictive diets that lead to negativity, guilt, rebellion, and usually failure. Finally, I offer tips on how to succeed in converting to Primal Blueprint-style eating without causing the stress or disappointment that are so common with unrealistic diet programs.
I bought a talking refrigerator that said “Oink” every time I opened the door. It made me hungry for pork chops.
—Marie Mott
Primal Blueprint-style eating offers many health benefits, which served Grok and his ancestors well for 2.5 million years. The most important goal of eating like Grok is to minimize the wildly excessive insulin production caused by the Standard American Diet. Making this simple change will allow you to lose unwanted fat, maintain an ideal body composition for the rest of your life, and virtually eliminate the major disease risk factors that will kill more than half of all Americans. Here are some other major benefits of the Primal Blueprint eating style:
Becoming a Fat-Burning Beast: When you reduce your consumption of grains, sugars, and other simple carbohydrates in favor of plants and animals, you will optimize your level of insulin production, enabling you to utilize fatty acids from both food intake and stored fat as your preferred fuel source. Being insulin-balanced helps regulate daily energy levels, even if you skip meals. In contrast, excess insulin production from a sugar-burner diet requires that you eat every few hours to bump up blood glucose levels that have crashed.
Effortless Weight Management: Plants and animals are much more nutritionally dense than processed-carbohydrate foods and refined vegetable oils, which comprise a large percentage of calories in the Standard American Diet. Eat like Grok, and you’ll meet your nutritional needs with fewer calories and dramatically boost your antioxidant intake. Moreover, the protein and fat you will be eating provide deeper and longer-lasting satisfaction levels—more satiety—than you get from a diet high in refined carbs. Finally, consuming fewer processed carbohydrates results in less insulin production, thus causing your hunger and cravings to moderate. Remember, the crash-and-burn effect is due to your body constantly cycling back and forth from consuming carbohydrates, burning it as glucose, then kicking out insulin to moderate blood glucose, which results in you feeling lethargic, hungry, and looking for a quick fix. Stopping that cycle by reducing the intake of carbs, especially simple carbs, is important to moderate your energy and hunger levels so that you can eat intuitively rather than in response to the crash-and-burn effect of the Standard American Diet.
Enhanced Cellular Function: The high-quality fats found in primal foods provide structural components for cell membranes and encourage your body to convert stored fat efficiently into energy. This includes the well-known omega-3s (mainly from oily, cold-water fish); monounsaturated fats from avocados, macadamia nuts, olives, and extra virgin olive oil; strategically-chosen polyunsaturated fats from nuts and seeds; and even the saturated fats from animal and coconut products that conventional wisdom has warned us to avoid.
Lean Muscle Development and Maintenance: The high-quality protein found in primal foods will help you build lean muscle mass, achieve healthy bone density, and control your body’s day-to-day repair and renewal requirements. When you moderate insulin production, exercise sensibly, and eat adequate amounts of protein, you become more insulin sensitive. This means the receptor sites in your muscle cells can assimilate amino acids and glucose efficiently, which is the key to muscle building and recovery.
Reduced Disease Risk Factors: Ditching grains, sugars, other simple carbs, and processed foods, especially “bad fats” (refined vegetable/seed oils and trans and partially hydrogenated oils), will reduce your production of hormone-like messengers that instruct genes to make harmful pro-inflammatory protein agents. These agents increase your risk for arthritis, diabetes, cancer, heart disease, and many other inflammation-related health problems.
Obesity is really widespread.
—Joseph O. Kern II
A SEPARATE SHELF FOR THE BLUEPRINT
You may be familiar with the decades-old Atkins diet program named after Dr. Robert Atkins, the original proponent of “low-carb” dieting. Over the years, numerous other programs (e. g., South Beach and the Zone) have battled for shelf-space supremacy Diet best-sellers have varied from mostly credible to completely ridiculous propositions. Followers of Atkins and other low-carb diets will indeed lose fat by strictly limiting carbohydrates and thus moderating insulin production. However, an obsessive ultra-low-carb strategy can be unhealthy over an extended time period because it limits your intake of some of the most nutritional foods known to humans—vegetables and fruits. Furthermore, high-calorie-burning, low-body-fat, highly insulin sensitive folks, as well as females with certain hormonal irregularities, might not respond well to one-size-fits-all carb restriction protocols.
While the Primal Blueprint also advocates eliminating the extremely harmful processed carbohydrates and sugars from your diet, vegetables and (some) fruits are central components of the Primal Blueprint eating strategy. Vegetables and fruits (which consist mainly of carbohydrates) are nutrient dense yet calorically sparse, so even generous portions of these foods will not provoke a high insulin response. What’s more, the extra energy required to digest the complex carbohydrate and highly fibrous nature of vegetables is such that you need not even count the carbohydrate grams in vegetables toward your daily goals based on the Primal Blueprint Carbohydrate Curve. Fruits are a bit different and require a bit of moderation in today’s world of year-round availability and excess dietary carb intake in general—especially if you are trying to reduce excess body fat. I discuss this topic in detail in the next chapter.
One of the online Primal Blueprint appendices at MarksDailyApple.com compares and contrasts the Primal Blueprint with popular diets such as Atkins, Low Fat (e.g., Ornish, McDougall, Pritikin), Metabolic and Blood Typing, paleo-themed diets, South Beach, Vegetarian, and the Zone. Of all these mentioned, the paleo eating approach is the most similar to the Primal Blueprint However, I refrain from even calling the Primal Blueprint a “diet” due to its comprehensive nature. The Primal Blueprint is a lifestyle—with some important but extremely flexible eating guidelines. I prefer to apply the eating laws in conjunction with the other eight Primal Blueprint lifestyle laws for best results.

The Primal Blueprint eating philosophy might seem a little unusual at first for those trying to do the right thing by conventional wisdom. After all, here’s a plan that suggests that healthy fat should be the centerpiece of your diet, while supposedly “healthy” whole grains should be eliminated. In fact, one might describe the Primal Blueprint as a high-fat, moderate-protein, fairly low-carb diet—particularly in comparison to the exceedingly grain-heavy diet that has been endorsed for years by the USDA Food Pyramid and Food Plate visuals, the American Heart Association, and the American Medical Association.
We now know that the outdated and unwarranted recommendation to eat 300 or more grams of (mostly grain-based) carbohydrates each day has contributed greatly to the destruction of human health. It’s not unusual for an average American, and for people in other countries following a Western-style diet, to consume 500 or 600 grams of insulin-generating, fat-promoting carbohydrates daily. Furthermore, a large proportion of these carbohydrates are likely refined, meaning they have been processed in some way that increases the severity of the glucose spike and requisite insulin response. White flour and high fructose corn syrup are two prominent examples of refined carbohydrates that are rampant in the Standard American Diet. They have no real nutritional value and can promote inflammation and oxidative damage when they are consumed regularly.
Keep in mind that Grok and his clan probably worked hard to gather natural carbohydrates like fruits, vegetables, and starchy tubers—unrefined, fibrous, slow-burning food with excellent nutritional value. While intake likely fluctuated greatly by season, our ancestors rarely ate over 100 grams of carbs per day, and in some cases/locations, they were able to survive for long periods of time on extremely minimal carbohydrate intake (for unlike fat and protein, carb consumption is not required for human survival).

By averaging between 100 and 150 grams daily (certain folks may adjust this upward, which I’ll discuss later) of vegetable- or fruit-based carbs; high-nutrient-value carbs like sweet potatoes, wild rice, and quinoa; and incidental carbs from nuts, seeds, and moderation foods such as high-fat dairy and high-cacao dark chocolate, you can achieve stable levels of insulin and other appetite and metabolic hormones, enjoy sustained energy levels, reduce excess body fat, and maintain a healthy weight. If you want to accelerate your fat loss for a period of time, lowering your average carb intake to 50 to 100 grams or less per day will allow you to easily drop an average of one to two pounds (one-half to one kilogram) of body fat per week. We will discuss this strategy in detail in Chapter 9. And you can do all this while eating until you’re satisfied—no suffering!
MARK TALK

Sitting down? Here’s another zinger that will blow your mind and set you straight about the secret to weight loss and long-term body composition success: Eighty percent of your ability to reduce excess body fat is determined by how you eat, with the other 20 percent depending on proper exercise, other healthy lifestyle habits, and genetic factors.
It’s as simple as this: if you have excess body fat, it’s directly reflective of the amount of insulin you produce from your diet combined with your familial genetic predisposition to store fat. In plain-speak, if you eat like crap and have bad (genetic) luck, you’ll get fat and sick and you’ll probably die early. On the other hand, having a bad diet and good luck (carrying the “skinny gene”) might allow you to avoid a plump figure, but it also might result in a physique that health experts refer to as “skinny fat”—having minimal subcutaneous fat, minimal lean body mass, and poor muscle definition, but with dangerous amounts of visceral fat surrounding the organs.
Furthermore, skinny fat folks can and do get heart disease, hypoglycemia, arthritis, sarcopenia (loss of muscle mass), chronic fatigue, compromised immune function, exhausted stress-management mechanisms, and a host of other adverse health consequences heavily attributed to diet. A slender type 2 diabetic might experience an even greater risk for serious disease because he or she is less able to activate the so-called “thrifty genes” that efficiently store excess dietary glucose in fat cells, and as a result, that glucose floats around in the bloodstream causing intense cellular damage. While the overall impact of poor lifestyle habits, including outward physique, vary widely due to luck of the draw, we all share an evolutionary genetic predisposition to suffer chronic disease when we eat foods that are misaligned with our genes.
On the positive side, if you eat right, you can look your absolute best even if you possess a genetic predisposition to store more fat than your workout partner. Your ability to reduce excess body fat and maintain desirable body composition is directly related to your ability to moderate insulin production with healthy dietary habits, to reduce inflammation (a contributor to insulin resistance), and, to a lesser extent, follow a sensible exercise program that combines extensive low-level cardio, frequent brief, intense strength-training sessions, and occasional all-out sprints. We can’t all have Gisele Bündchen’s or David Beckham’s body, but we can all unlock the best versions of ourselves by making good—and relatively easy—lifestyle decisions. Even if you have struggled with excess body fat for your entire life, you can quickly and dramatically alter your destiny by following the simple laws of the Primal Blueprint.
I’m not talking about achieving “success” with a short-term crash program. The Primal Blueprint is based on eating as much as you want, whenever you want, choosing your favorites from a long list of delicious approved foods, and simply avoiding eating foods from a different list. When I say you will notice quick and dramatic results, I’m referring primarily to the immediate increase and stabilization of energy levels, reduced hunger and fewer mood swings related to “bonking” (running low on blood glucose), improved immune function, and a reduction in the symptoms of allergies, arthritis, and other inflammatory conditions exacerbated by the anti-nutrients in a grain-based diet.
Regarding weight loss, we must recognize that our views are so messed up on this topic that it’s hard even to have a sensible conversation about it. The stories of losing massive amounts of weight in a short time are so commonplace that we seem to expect nothing less when we pursue weight-loss goals. First, the Primal Blueprint is really about optimizing body composition, instead of just reducing your weight on the scale. For most, this means a reduction in body fat percentage and an increase or maintenance of muscle or lean body mass. Clearly, gaining muscle and losing fat produces more impressive appearance changes than dropping 20 quick pounds on a crash diet that depletes muscle mass and water retention. Lean body mass (muscle, skeleton, and all the rest of you that is not fat) is also directly correlated with “organ reserve,” the highly desirable ability of all your vital organs to function effectively beyond basal level (the minimum functional or effective level; for example, when your heart rate elevates during exercise). We’ll discuss this critical longevity component in Chapter 7.
When you trigger your genes to stop storing body fat and start burning it, as well as to build or maintain an optimal amount of muscle mass, you can sensibly and realistically lose a pound or two of body fat per week if you are currently storing excess body fat. You can even do this with minimal exercise, but the fat loss (and the gaining, sculpting, or toning of lean muscle) will be accelerated significantly when you choose the right exercise regimen. Mostly, your success depends on how diligent you are in keeping your insulin levels moderated, thereby allowing your body to obtain more of your caloric needs from your stored body fat.
You can alter your biochemistry at each meal—to stimulate a fat-burning metabolism and maintain consistent energy levels, or to do the opposite with poor food choices.
Not a day goes by without a friend, client, or MarksDailyApple.com commenter relating to me how he or she notices improvements within days of switching to the Primal Blueprint eating style. As I will detail in this chapter, you have the chance to alter your biochemistry at each meal—to stimulate a fat-burning metabolism and maintain consistent energy levels, or to do the opposite with poor food choices. The momentum you build with good choices will make it easier to discard old habits because you experience instant gratification from satisfying meals and stable energy levels, as well as positive long-term health and metabolic consequences.
MORE THAN ONE WAY TO SKIN A CAT: THE PARADOXICAL SUCCESS OF LOW-FAT EATING
At this point in history, it’s clear that the type of low-fat diet prescribed by the USDA, American Heart Association, and similar organizations has been a dismal failure. Heart disease remains a potent killer, diabetes rates continue to climb, and America—and the West at large—is no closer to beating the obesity epidemic than we were 40 years ago (actually, the population is fatter than ever), when low-fat advisories became public policy. Pushing our fat intake down to 30 percent of total calories has, it seems, done more harm than good.
Yet there remains a paradox in the nutrition community’s ongoing macronutrient wars: the success of extremely low-fat diets such as those espoused by Dean Ornish, John McDougall, Rip and Caldwell Esselstyn, Nathan Pritikin, and Neal Barnard. By keeping fat intake to a rigid 10 percent of calories or lower (and emphasizing whole, unprocessed plant foods as dietary staples), these low-fat proponents claim success in treating obesity, heart disease, diabetes, and other modern chronic diseases, with a fair amount of published research supporting as much Hold the toast! How could extremely low-fat diets yield any success when moderately low-fat diets have been so disastrous?
The answer lies in the intriguing ability for extreme fat restriction to improve insulin sensitivity and reduce the chance of post-meal fat storage. For one, in the context of a nearly fat-free meal, the insulin spikes following carbohydrate ingestion don’t have any dietary fat to shove into cells, making fat gain less likely Second, when dietary fat is combined with a hefty carbohydrate intake, the result can be that it takes more insulin to result in fat storage for that particular meal Take away the fat in these instances, and carbohydrate metabolism improves.
Does this mean that extremely low-fat diets are a smart move for your health? Not so fast While these diets do claim some clinical success in terms of weight loss, they’re also low in (or devoid of) the important fat-soluble vitamins A, D, and K2. They can also result in essential fatty acid deficiency, are scarce in animal-based nutrients, and aren’t anywhere near as satiating as a higher-fat, real-food primal diet. Likewise, their efficacy may be limited to a small number of individuals who are highly responsive to low-fat diets. And finally, a recent review of 53 published scientific studies orchestrated by researchers at Brigham and Women’s Hospital and the Harvard School of Public Health found that low-fat diets were not more effective than other types of dietary interventions in terms of long-term (greater than one year) weight loss.
That being said, short-term bouts of very low-fat, high-carbohydrate eating—especially when those carbs are of the nutrient-dense primal variety—can work as a “hack” to break through weight-loss stalls, restore some insulin sensitivity, reboot hormone levels, and flood gut flora with beneficial starches and fibers. The so-called “Potato Hack,” for instance, has gained popularity on Mark’s Daily Apple forums This consists of eating two to three pounds of cooked and cooled potatoes (and little else—sorry, no butter on those spuds) for several days or a week as a way to rapidly shed body fat Along with serving as a carb refeed after periods of lower carbohydrate intake, this type of strategy can provide healthy gut microbes with an abundance of resistant starch (discussed in Chapter 5), helping rekindle the beneficial bacterial strains whose food source dwindles on a low-carb menu.
All in all, I am still convinced that a primal eating strategy containing plenty of healthy fats from both animal and plant sources is your best bet for long-term health However, the human body is adapted to—and even expects—sporadic changes in dietary patterns Brief windows of very low-fat eating (or its inverse, ketosis, which we’ll cover in chapter 4) can be a fine component of a primal eating framework, and may even offer some benefits.

The insulin story is perhaps the most health-critical concept in the book, so I want you to fully understand it on both a practical and a biochemical level. A primary goal of the Primal Blueprint is to help you moderate insulin production and improve insulin sensitivity, both markers of metabolic health that will help you avoid many of the health scourges of modern society. To understand insulin, you first have to understand blood glucose. When you eat carbohydrates (starches: grains and legumes, and sugars: both processed sugars such as granulated sugar and sugars naturally occurring in fruits and vegetables), your digestive system breaks them down into their components, one of which is glucose. Glucose is delivered from your stomach and small intestine into the bloodstream, where it travels around providing fuel for your cells. When you hear the term “blood sugar,” this actually refers to the amount of glucose in your blood (which is why I use the term “blood glucose” to be more accurate). Your body can burn glucose quickly and efficiently for energy, so it is the first choice for fuel when it is available. While glucose is a critical component of the body’s energy system, it is toxic if it remains in the bloodstream for too long and in quantities that are too high, so it must be moved to its destination quickly. Insulin is quite literally the key to this system.
Insulin is a hormone secreted by beta cells in the pancreas in response to elevated blood glucose (as happens after a meal containing carbohydrates). Cell receptors use insulin as a key to unlock glucose channels in the membrane of each cell. With the cell “door” open, glucose can be stored inside the cell (along with other nutrients whose transport into the cell is potentiated by insulin). Any glucose that isn’t needed immediately for energy is shuttled into storage for future use, first in muscle or liver cells as glycogen, or in adipose (fat) cells as triglycerides. It’s an elegant way for cells to gather the fuel they need while eliminating excess glucose from the bloodstream. It’s also how the body prepares itself to have sufficient energy supplies even in times of famine (which would have been inevitable for Grok, but for most of us, not so much).
In order to stay healthy and to avoid medical problems that are rampant in modern society such as heart disease, Metabolic Syndrome, obesity, type 2 diabetes, certain cancers, and hyperglycemia or hyperinsulemia, it is absolutely critical that you remain insulin sensitive. That simply means that insulin is able to do its job opening the figurative cell doors for glucose.
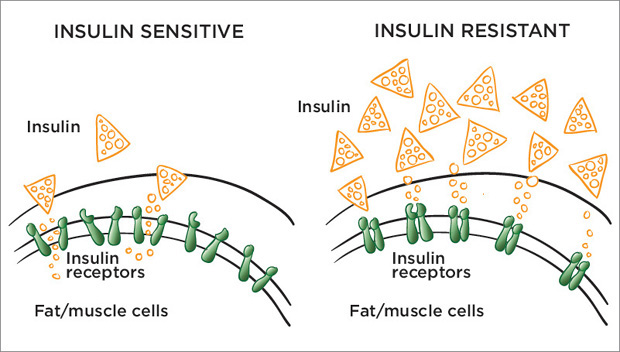
Insulin works on cell receptors to deliver precious cargo including glycogen that is frequently depleted by exercise.
To promote insulin sensitivity, the most important factor is a diet such as the one laid out in this book that helps the body maintain relatively stable, moderate insulin levels. Unfortunately, the typical modern diet is basically made up of one glucose bomb after another, in the form of breads, pastas, cereals, pastries, sweets, and even supposedly healthy foods like smoothies, trail mix, and meal replacement bars, many of which contain tons of added sugar, milk chocolate, processed corn products, and so on. Bombarding their systems in this way has many Americans on a glucose-insulin roller coaster that results in the short term in glucose spikes and crashes, increased insulin production, cravings, irritability, and weight gain, and in the long term, chronic disease.
Exercise is also instrumental for promoting insulin sensitivity, and this is another area where too many people fall short. The average person can only store a total of about 400 grams (less than one pound) of glycogen in liver and muscle tissue. (Even a highly trained athlete can only store perhaps 600 total grams.) If you frequently empty your liver and muscle cells of glycogen with brief, intense workouts, frequent low-level movement, and structured aerobic sessions, you become adept at not only burning stored energy, but also replenishing glycogen (as well as amino acids, whose metabolism is also facilitated by insulin). In this case, insulin will deliver nutrients to your liver and muscles instead of just having them go straight to fat. If you are sedentary and eat a moderate- or high-carbohydrate diet, there is no selection pressure (to borrow an apropos term from our evolution discussion) to be insulin sensitive. My foolproof prevention plan or, dare I say, cure for those with type 2 diabetes, obesity, and heart disease, no matter how overwhelming their genetic predisposition to these conditions, is to moderate dietary insulin production and exercise according to the Primal Blueprint laws.
Sadly, a grain- and sugar-heavy diet coupled with chronic inactivity has put many people on the path to insulin resistance instead of insulin sensitivity. The human body simply is not designed to process the amount of glucose most people dump into it day after day. For a little while, your system can cope with a poor diet and bad (or non-existent) exercise routine, although you might not like its coping strategy: converting excess ingested glucose into triglycerides in the liver and storing these triglycerides in fat cells throughout the body. Remember, although the first thing insulin wants to do with any glucose that your body doesn’t immediately need is to store it as glycogen in muscle and liver cells, that has a finite capacity. That has a finite capacity. Inactive folks generally have plenty of muscle and liver glycogen stored at all times, so insulin takes any carbs they ingest on an express train to their ultimate destination in fat cells. On top of that, when blood insulin levels are high, those same fat cells store not only excess glucose (as triglycerides) but also the fat you ate at your last meal.
Eventually, the strain of having chronically high glucose and insulin circulating around leads to the problem of insulin resistance, wherein cells (first muscle and liver, and then fat cells) are not receptive to insulin trying to unlock them in order to shuttle glucose out of the bloodstream. The pancreas then has to pump out even more insulin to try to get the job done, leading to a harmful cycle of insulin overproduction (resulting, eventually, in chronic hyperinsulinemia). Just as blood glucose is desirable as long as it is regulated but can be toxic if it exceeds normal levels, a moderate amount of insulin in the bloodstream is good, but a lot can be bad... very bad. The more insulin your pancreas produces to deal with excessive carbohydrate intake, the more resistant your muscle and liver cells can get. This happens because the genes responsible for these receptor sites turn themselves off, or “downregulate,” in response to—and in defense against—the excessive energy that insulin is trying to shuttle into your cells. This is all part of the body’s quest for balance and your genetic response to environmental signals.
Furthermore, the “do not enter” sign hanging on the liver due to insulin resistance tricks some cells in your liver into believing they are starved for glucose (which, if it were true, would be a big problem because the brain preferentially uses glucose for fuel, and a few specific types of cells, such as red blood cells, rely exclusively on glucose). In response to the liver’s storage cells refusing to accept glucose, your genes signal other specialized liver cells to commence gluconeogenesis (the conversion of lean muscle tissue or ingested protein into glucose for quick energy) and dump more glucose into the bloodstream, despite the fact that there’s already plenty there. Talk about a communication breakdown! Of course, your resistant muscle cells are deaf to insulin signaling as well, so the new, extra glucose your liver just made is also diverted to the eager fat cells, unless they, too, are overgorged with fat.
Taken to the extreme, as with a morbidly obese individual, even fat cells become resistant to further storage, because we only have a fixed number of fat cells. At that point, the body’s last line of defense against the damage inflicted (quickly) by excess blood glucose has maxed out, in which case the glucose stays in your blood stream. Consequently, all hell breaks loose in terms of blood glucose toxicity and insulin damage, leading to even greater risk for type 2 diabetes (if it hasn’t already developed, which it likely has), heart attack, blindness, the need for limb amputation, and other disasters.
Carbs are treated differently in the body depending on whether you’re insulin resistant (insufficient exercise and movement, dietary energy excess, surplus of processed carbohydrates) or insulin sensitive (regular exercise, active lifestyle, healthy weight, moderated carb intake).
This doesn’t mean your daily PowerBar is going to lead to limb amputation any time soon, but as you gain further understanding of the insulin story, it becomes clear how the shocking statistic of the average American gaining one and a half pounds of fat (two-thirds of a kilo) a year for 30 years is achieved. It is quite easy to slide down the slippery slope of insulin resistance and end up with a host of medical problems, many of which doctors are just coming to understand are tied to insulin resistance.
In case you aren’t already convinced, let’s take a look at some more of the unpleasant consequences of having chronically elevated blood glucose and insulin levels and of becoming insulin resistant:
Fat cells get bigger, and you get fatter. In addition to glucose and dietary fat being delivered straightaway to adipose tissue deposits, you become less able to burn fat for energy. Insulin inhibits the fat-burning enzyme lipase, so fat cells can’t release their stored energy into the bloodstream where the fatty acids could be used as fuel. So not only do you store more fat, the fat remains locked in storage.
Advanced glycation end products (AGEs) result from chemical reactions that occur when blood-borne glucose molecules bind randomly with important structural proteins used by your organs and systems, causing long-term damage. A familiar example is the wrinkling of the skin. Yes, aging and sun damage are factors, but so are AGEs. AGEs are also culprits in increased inflammation and risk of heart disease, as well as the circulation problems and neuropathies (nervous system disorders) that characterize type 2 diabetes. When glucose is not efficiently shuttled out of the blood, AGE damage can result.
Pancreatic beta cells start facing glucolipotoxicity from being overexposed to chronically high levels of glucose and free fatty acids. This leads to impaired insulin secretion, beta cell death (apoptosis), and—when other genetic and environmental factors are in place—the progression of type 2 diabetes.
Accelerated aging is associated with chronically excessive insulin production, which is dangerously pro-inflammatory and can wreak havoc throughout the body. Scientists know that within any species, those that produce the least amount of insulin over a lifetime generally live the longest and remain the healthiest.
Excessive insulin is also now believed to be a central catalyst in the development of atherosclerosis. Insulin promotes platelet adhesiveness (sticky platelets clot more readily) and the conversion of macrophages (a type of white blood cell) into foam cells, which are the cells that fill with cholesterol and accumulate in arterial walls. Eventually, a cholesterol and fat-filled “tumor” blocks circulation in the artery, a situation further aggravated by increased platelet adhesiveness and thickness of the blood. In addition, insulin and the aforementioned AGEs interfere with the production and activity of a compound called nitric oxide (NO). NO performs the critical function of keeping the endothelial cell wall—the lining of your arteries—relaxed and flexible, as well as inhibiting platelet adhesion and other mechanisms that contribute to atherosclerosis. Low NO causes your artery walls to become more rigid, which drives up blood pressure and increases the sheer force of blood against the arterial wall, further exacerbating the atherosclerotic condition. I will further detail the chain of events causing atherosclerosis and what you can do to prevent it in the cholesterol section later in this chapter.
Levels of growth hormone and other important health-enhancing hormones are also adversely affected by insulin resistance. The pituitary gland makes growth hormone, which is then sent to the liver to signal the production of insulin-like growth factors (IGFs). Many of our cells have surface receptors for IGFs. Because of its similar structure, insulin binds to IGF receptors and prevents growth-hormone-stimulated IGFs from doing their job.
High insulin levels over long periods of time also hamper sex hormone synthesis, causing levels of testosterone, DHEA, and other sex hormones to decline steeply as we age. Hormone levels naturally decline over time, but this flagship premise of the multi-billion-dollar anti-aging industry is very likely exacerbated by insulin resistance as opposed to the mere passing of the seasons. Remember, if Grok was lucky, he could enjoy dramatically better health and physical fitness into his seventies than most of today’s baby boomers. Sex hormones are supposed to be transported through the bloodstream by globulin (a blood protein) to act upon target organs and tissues. When excessive insulin is present, these hormones can stay bound to globulin instead of getting dropped off at the target cells (e.g., the adrenal glands, sex organs, and brain). Even an expensive anti-aging hormone regimen cannot override this undesirable condition caused by excessive insulin.
Thyroid function is disrupted by excessive insulin. The thyroid gland produces a hormone called T4 which is converted in the liver to T3, the primary hormone that controls energy metabolism. When your liver becomes insulin resistant, conversion of T4 to T3 declines drastically. This leads to a decrease in metabolic rate, increased fat storage, and diminished energy levels and brain function.
Hopefully by now you are convinced of the importance of insulin sensitivity and are sufficiently troubled by the possibility of becoming insulin resistant. Clearly, insulin is absolutely essential to life; it’s just that chronic overproduction of insulin turns a good thing into a bad thing. Luckily, research suggests that insulin resistance can be addressed quickly by reducing carbohydrate intake and increasing activity levels. It’s as simple as this: when you eat the Primal Blueprint-style foods that fit your genes, you’ll be able to fit into your jeans!
If these clinical details about the long-term damage from a high-insulin-producing diet are not sufficient to get you to change your breakfast order today, consider the short-term unpleasant effects of high-carbohydrate, insulin-producing meals and snacks (on otherwise healthy, non-diabetic folks).
Ingesting high-carbohydrate food (sugary foods and beverages, desserts, processed grains, etc.) generates an immediate increase in blood glucose levels, which has the short-term effect of elevating your mood, energy level, and alertness. In a matter of minutes, however, your pancreas secretes a requisite amount of insulin to quickly remove any excess glucose from the bloodstream before it becomes toxic. Depending on the type and amount of carbs you consumed and your degree of insulin sensitivity, this insulin rush can eventually cause your blood glucose levels to decline so much that your glucose-dependent brain soon becomes low on fuel. As a result, you may feel sluggish, foggy, and cranky, and have trouble focusing. While this explains the familiar post-lunch afternoon blues and grogginess, extensive data also suggest a strong link between processed carbohydrate consumption/insulin production and attention deficit/hyperactivity disorder (ADHD) and assorted other cognitive disorders.
Additionally, the ingestion of lots of carbohydrates, followed by the secretion of lots of insulin (and, subsequently, low blood glucose levels), is interpreted as a stressful event by the hypothalamic-pituitary-adrenal (HPA) axis. This homeostasis-monitoring part of your endocrine system (responsible for the fight or flight response) signals your adrenal glands to release epinephrine (adrenaline) and cortisol (the “stress hormone”) into your bloodstream to cope with the perceived stress. Cortisol breaks down precious muscle tissue into amino acids, some of which are sent to the liver and converted into glucose through gluconeogenesis. The ensuing blood glucose rush gives you the boost your brain thinks you need—commonly at the expense of your muscle tissue.
Depending on your individual sensitivity to glucose and insulin, the stress response to this seesaw process may make you feel amped, jittery, edgy, or hyper, and you may experience a racing heartbeat. Others may not experience any stress-hormone buzz, likely because years of abusing this delicate life-or-death energy boosting mechanism (thanks to high-carbohydrate eating, chronic cardio, excessive artificial light/insufficient sleep, and high-stress lifestyle) have exhausted your fight or flight hormonal mechanisms. Instead, they’ll just feel like taking a nap after high-carb meals. Consequently, their roller coaster ride will consist of a brief glucose high after meals, followed by a crash and carb/sugar cravings (to bring their energy levels back up) and/or a desire for a nap once insulin starts going to work. However your particular daily energy level and appetite fluctuations play out, all roads in this saga lead to burnout and elevated risk of disease and dysfunction.
Besides the unsettling energy swings and added physiological stress, sugar also seriously hampers immune function as soon as it’s ingested. We know that excessive and/or prolonged production of cortisol is a potent immune suppressor (the fight or flight mechanism diverts resources to provide an immediate energy boost). Research also shows that sugar itself can impair the function of immunity-related phagocytes (immune system cells that remove bacteria or viruses from the bloodstream) for at least five hours after ingestion. This impairment happens through a process known as competitive inhibition, when excess glucose prevents all-important vitamin C from being transported inside certain immune cells. Because both molecules use the same mechanism and entry point to gain access to the inside of the immune cells, the presence of excessive glucose can overwhelm the transporter sites and block vitamin C from entering. Furthermore, your blood thickens as a response to these immune stressors, which is why heart attacks (in people predisposed to them) tend to occur after a meal.
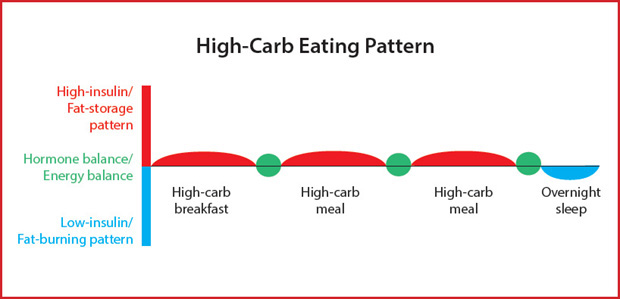
The high-carb eating pattern requiring excess insulin production causes a roller coaster of glucose spikes and dips, overstress (leading to burnout), increased appetite/caloric intake, mood/energy level swings, and lifelong insidious weight gain.
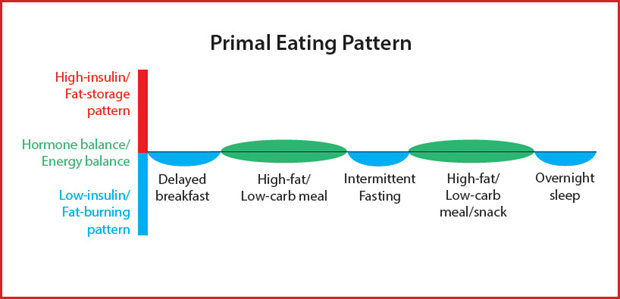
Energy balance happens from becoming fat-adapted and eating low-insulin-producing meals. Appetite, mood, energy, caloric intake, and blood glucose are stabilized, leading to effortless weight maintenance.
Putting yourself through the roller coaster of sugar-spiking meal  insulin response
insulin response  blood glucose crash
blood glucose crash  stress-induced gluconeogenesis feels like a life-or-death matter to your primal genes. Getting the afternoon blues and brain fog and making mistakes on spreadsheets is very bad news, but low blood sugar in primal times might have spelled doom at the hands of the nearest predator. Fortunately, our highly sensitive fight or flight response can turn muscle into glucose quickly when we need energy.
stress-induced gluconeogenesis feels like a life-or-death matter to your primal genes. Getting the afternoon blues and brain fog and making mistakes on spreadsheets is very bad news, but low blood sugar in primal times might have spelled doom at the hands of the nearest predator. Fortunately, our highly sensitive fight or flight response can turn muscle into glucose quickly when we need energy.
On an extreme scale, you might harness this system during times of personal or family crisis where your appetite and food intake is suppressed for days on end but you are still wired on nervous energy. Cortisol will stimulate gluconeogenesis, breaking down muscle into the sugar your brain and body need to go. On a minor scale, a high-carbohydrate eating pattern will chip away at the stress response by repeatedly tapping into gluconeogenesis to boost up sagging blood sugar levels. When coupled with other forms of chronic stress in modern life (including chronic exercise especially), the fight or flight response can easily become exhausted and send you into a state of burnout.
Note that the chain of events described here happens routinely in a normal, healthy person who overindulges in carbohydrates. Experiencing these high-low cycles is no fun, but it does mean you still have some sensitivity to the negative effects of carbohydrate ingestion and insulin production. If you don’t experience significant noticeable symptoms after eating lots of carbohydrates (particularly sugar), you are likely well on your way to, or have already developed, the extremely problematic condition of insulin resistance. The analogy of a smoker feeling minimal ill effects from his or her habit applies here. I’d argue that a vast majority of the population is somewhere on this continuum, far outside of the healthy ideal of a diet that moderates carb intake and insulin production in line with our genetic requirements for health.
Your goal should be to maintain stable, healthy insulin levels through sensible diet and exercise choices. This does not mean cutting all carbohydrates out of your diet, but rather preferentially eating reasonable amounts of carbohydrates from vegetables and fruits that produce a much more moderate insulin response than that caused by grains or sugars. Bear in mind that while it’s obviously preferable to mute insulin spikes and crashes, your diet’s total insulin production is the most important element to consider. If you are routinely eating excessive carbohydrates (especially in the context of an inactive lifestyle), even if they come from “healthy” sources, you will likely gain weight and increase your risk of developing other associated health problems including the “oxidation and inflammation” syndrome that is the major culprit behind heart disease.
The debate over the theory known as the lipid hypothesis of heart disease has raged for years. Big Pharma and your helpful friends at the FDA, AMA, and other respected health agencies have done a great job of vilifying cholesterol and saturated fat as the major causes of atherosclerosis and heart disease. You know their story by now. Your arteries are like pipes. Cholesterol is the fatty, sticky gunk that clogs them up if you eat too many high-cholesterol animal products (meat, eggs, butter) or saturated fats in general. According to conventional wisdom, you should eat a low-fat, low-cholesterol, high-complex-carbohydrate diet. If your diet or genetic bad luck results in a total cholesterol level of over 200, you simply take cholesterol-lowering statin medicines to “safely” reduce your risk.
In recent years, many elements of conventional wisdom’s stance on cholesterol have been called into question. While there is significant dispute and uncertainty about the issue among respected experts, there is compelling evidence that freely dispensing powerful statin medications to reduce all forms of cholesterol offers minimal to no protection from heart disease and stroke. Furthermore, it’s almost universally agreed that lifestyle modifications such as losing weight, reducing intake of processed carbs and refined vegetable oils, consuming omega-3 oils, exercising, and managing stress levels can do a much better job than statins in terms of eliminating the major heart disease risk factors.
Fortunately, the tide is slowly turning as the cracks in conventional wisdom’s armor are beginning to show. A June 2014 cover of TIME bore the command “Eat Butter,” with the headline “Scientists labeled fat the enemy. Why they were wrong”—a striking follow-up to the magazine’s iconic 1984 cover illustrating a frowning eggs-and-bacon face with the words, “Cholesterol. And now the bad news... .” In September 2015, the peer-reviewed British Medical Journal even published an editorial chastising the less-than-scientific underpinnings of the US Dietary Guidelines, calling for a more rigorous, less biased evaluation of the evidence (particularly that condemning saturated fat and dietary cholesterol).
Finally, in December 2015, the U.S. Department of Health and Human Services (HHS) released the new 2015-2020 Dietary Guidelines for Americans report (available on health.gov) and did away with the recommended maximum of 300 mg/day of dietary cholesterol from the 2010 guidelines. The report goes on to say that Americans should “eat as little dietary cholesterol as possible,” but then states that high-cholesterol eggs and shellfish are an acceptable part of a healthy diet. So it seems that HHS doesn’t know quite where it stands on cholesterol at the moment, although the report strongly implies that cholesterol probably isn’t that bad, and saturated fat is the real enemy—another claim I strongly dispute. (In fairness, the report does call for more research into the relationship between dietary and serum—blood—cholesterol; but you will know by the end of this section that I’m not impressed by serum cholesterol as a health risk marker, to say the least). In an interesting behind-the-scenes look, the committee that makes recommendations to the HHS when preparing the new guidelines asserted, “[A]vailable evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol.. Cholesterol is not a nutrient of concern for overconsumption.” Obviously the HHS wasn’t ready to make such a bold statement.
While the new guidelines are a step in the right direction, they fall short of admitting that the fearmongering around cholesterol is largely unwarranted. Moreover, there is still the hurdle of getting this accepted by medical practitioners who have been bombarded with the message that elevated cholesterol is the root of all heart disease. We may have a way to go before mainstream medicine is fully on board with evolutionarily health-aligned principles, but the trend, however slow, is at least moving in the right direction. Because I highly respect the valiant battle medical professionals are fighting with today’s heart disease pandemic (after all, they often have little or nothing to do with patients until they show up in the waiting room with clogged pipes), I’d like to assert here that this is not a “Mark versus your doctor” battle of the egos. Rather, I believe this is an unbiased interpretation of cutting-edge data that extends beyond the narrow and dated “eating fat drives cholesterol drives heart disease” story that most of us are familiar with, including physicians. Remember, physicians don’t necessarily have any specialized knowledge about the link between diet and heart disease from their medical training. Or if they do, it might be very outdated information. Like your plumber, their expertise is in dealing with already-clogged pipes.
For now, the best we can do is educate ourselves while the rest of the world gradually catches up. This discussion will give you a deeper understanding of exactly what causes heart disease (hint: it’s oxidation and inflammation driven primarily by poor food choices, excessive insulin production, and all forms of stress in excess, including overexercising) and help you do a better job minimizing heart disease risk than just following the party line of “don’t eat cholesterol—and take drugs if your numbers are high.”
Using total cholesterol level—or even your LDL cholesterol value—is irrelevant in the absence of further context, such as Metabolic Syndrome and other accomplices to heart disease.
Among the most notable research refuting the cholesterol story is the highly respected Framingham Heart Study. The study (which I reference often at MarksDailyApple.com) has followed the dietary habits of 15,000 participants, residents of Framingham, Massachusetts, over three generations. It is widely regarded as the longest (it began in 1948 and is still going strong!), most comprehensive study of health and illness factors on a population in medical history. It has led to the publication of more than 1,200 research articles in leading journals. Study director Dr. William Castelli summarized the issue unequivocally when he said, “Serum cholesterol is not a strong risk factor for coronary heart disease.” Among the study’s highlights are:
There is no correlation between dietary cholesterol and blood cholesterol levels.
Framingham residents who ate the most cholesterol, saturated fat, and total calories actually weighed the least and were the most physically active.
Luckily for us, over the past decade, hundreds of bright, clear-thinking researchers have reexamined old data, conducted new research, and written extensively on how and why the conventional wisdom lipid hypothesis of heart disease is deeply flawed. (There’s even an organized group called the International Network of Cholesterol Skeptics, populated by over a hundred leading M.D.’s and Ph.D.’s from across the globe, dedicated to countering the argument that animal fat and cholesterol cause atherosclerosis and heart disease.) Their research shows that atherosclerosis is caused mainly by excessive oxidation (and the ensuing inflammation) of a certain type of cholesterol that constitutes a small fraction of the mostly good stuff” flowing through your bloodstream.
Ironically, in many cases, it appears that this oxidation might be made worse by consuming the very cholesterol-free, polyunsaturated fats in vegetable and grain oils that the medical establishment led us to believe were healthier than animal fats! Furthermore, the drugs often prescribed to lower cholesterol have done little or nothing to improve the health of most of the people taking them, while the side effects and expense have been devastating to millions more.
Cholesterol is a little waxy lipid (fat) molecule that happens to be one of the most important substances in the human body. (Actually, there are many types of cholesterol, but for the moment I will lump them together.) Every cell membrane has cholesterol as a critical structural and functional component. Brain cells need cholesterol to make synapses (connections) with other brain cells. Cholesterol is a precursor molecule for important hormones such as testosterone, estrogen, DHEA, cortisol, and pregnenolone. Cholesterol is needed for making the bile acids that allow us to digest and absorb fats. Cholesterol is converted by UVB energy in sunlight into the all-important vitamin D. You can’t survive or thrive without cholesterol, which is why your liver actually makes up to 1,400 milligrams a day regardless of how much food-borne cholesterol you consume—or how much you avoid it like the plague—in your diet.
Because cholesterol is fat-soluble and does not dissolve in water, but must travel to and from cells in the watery environment of the bloodstream, it needs to be carried by special spherical particles called lipoproteins (the name means “part protein and part lipid [fat]”). There are several varieties of lipoproteins with different transporting functions—chylomicrons, LDLs, IDLs, HDLs, and VLDLs (as well as subfractions of those)—but the three we are concerned with here are VLDLs, LDLs, and HDLs (very low-density, low-density, and high-density lipopro-teins, respectively). Each of these lipoproteins carries a certain percentage of cholesterol, triglycerides, and other minor fats. Your blood test values for triglycerides and HDL, LDL, and VLDL cholesterol represent the combined total in your bloodstream of what all the lipoproteins are transporting.
VLDLs, the largest of these cholesterol complexes, are manufactured in the liver in the presence of high levels of triglycerides. Hence, VLDLs are comprised of 80 percent triglyceride and a little cholesterol. After leaving their birthplace in the liver, these lipoproteins deliver their cargo to fat and muscle cells for energy. Once these VLDLs have deposited their triglyceride load inside a fat or muscle cell, their size decreases substantially and they convert into either large, fluffy LDLs or small, dense LDLs—in both cases bearing mostly cholesterol and a little bit of remaining triglyceride. Large, fluffy, or “buoyant” LDLs are the more innocuous form of LDL, as they go about their assigned task of delivering cholesterol to the cells that need it.
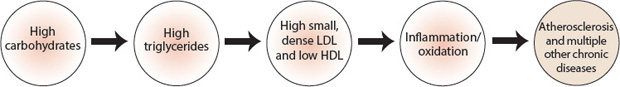
The real trouble starts when triglycerides are unusually high in the bloodstream, causing your body to convert VLDLs into small, dense LDLs. This condition can occur routinely when you eat a high-carb diet (even if it’s a low-fat diet), because excessive insulin production drives the conversion of ingested carbohydrate into fat (triglycerides). Obviously, the condition can also occur when you eat a moderate-carb, high-fat diet, because insulin will see to it that both excess carbs and fat get circulated in the bloodstream and stored in fat cells.
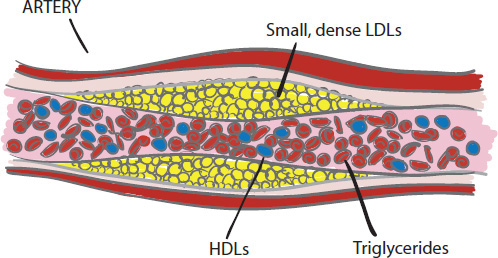
When the bloodstream is overloaded with triglycerides due to high-carb eating, VLDLs convert into the more problematic small, dense LDLs. This sets the stage for atherosclerosis.
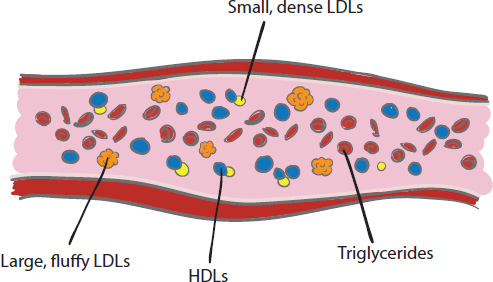
Primal eating lowers triglycerides and raises HDL. VLDLs convert into large, fluffy LDLs. HDLs—“nature’s garbage trucks”—remove problematic agents from the bloodstream, keeping arteries clean.
Dr. Dean Ornish and other proponents of low-fat eating will tell you that reducing fat intake quickly reduces cholesterol and triglyceride levels. This is absolutely true, as confirmed by numerous best-selling books as well as newspaper and magazine feature stories touting quick and dramatic results (lowered cholesterol and triglyceride levels) from fat-restrictive diets. But the reason is twofold: one, triglycerides will initially drop on any diet that triggers weight loss (which extremely low-fat diets can do because they dramatically reduce food options and cause an initial reduction in energy intake—but long-term sustainability is another issue entirely); and two, your liver makes cholesterol as a raw material for the bile salts that help you digest fat, so if you aren’t eating much fat, your genes will be given the signal to downregulate cholesterol production.
However, low-fat eating requires you to consume a high level of carbs, by default, to obtain your daily energy requirements. While this can work for some highly active populations that haven’t been exposed to the atrocities of the Western diet and lifestyle (such as some Pacific Islander tribes and traditional Asian communities), for the rest of us, this can lead to excessive insulin production and kick-start the cycle that eventually leads to heart disease. Any way you slice it, consuming more carbs than you need sooner or later leads to high triglycerides (not to mention the other risk factors detailed in the upcoming sidebar “How to Sneeze at Heart Disease”).
With high triglycerides in your blood, VLDL production skyrockets to handle the extra load, and these particles can be altered into the small, dense LDLs that appear to be a bigger factor in atherosclerosis and heart disease than large, fluffy LDLs. Being small and dense, these small, dense LDLs (why can’t all medical nomenclature be this easy?) can become stuck in the spaces between cells lining the arteries and then become oxidized. This is compounded by the fact that small, dense LDLs do not bind to LDL receptors (receptors on the surface of cells, especially liver cells, that remove LDLs from the bloodstream) as easily as the larger LDL particles do. That means the small, dense LDLs stay in circulation longer, increasing the chance that they will get stuck in the arterial wall and oxidize. This oxidative damage causes inflammation and begins a process of destruction that I will detail shortly.
Small, dense LDLs are small enough to get stuck In the endothelial lining of the blood vessels and become oxidized, while large, fluffy LDLs sail along unscathed.
Another issue to be aware of is the difference—tragically, one rarely discussed by doctors when delivering your cholesterol results—between calculated LDL (“LDL-C”) and LDL particle number (“LDL-P”). LDL-C is the value reported on most blood tests, unless you’ve specifically requested otherwise. It’s simply a measure of the cholesterol mass within your LDL particles, calculated indirectly based on your total cholesterol, your HDL, and your triglycerides. (For people with triglyceride levels below 100, the formula used to calculate LDL-C tends to significantly overestimate LDL levels.) By contrast, LDL-P is a direct measure of the number of LDL particles in your bloodstream. As with small, dense LDL, LDL particle count is more highly correlated with heart disease than calculated LDL, since a large number of LDL particles—by sheer probability—have a greater chance of facing oxidative modification in the bloodstream and ending up embedded in artery walls.
This distinction matters significantly when it comes to gauging your disease risk. If your blood is host to a party of large, fluffy LDL particles carrying plenty of cholesterol in each lipoprotein “vehicle,” LDL-C will tend to be high (especially if your triglycerides are also low), even if the actual number of LDL particles is in a healthy range. Meanwhile, if your bloodstream is full of small, dense LDL packing less cholesterol in each lipoprotein, your LDL-C may appear lower, even though the number of particles is dangerously high. In other words, LDL-C can be wildly misleading; knowing your LDL particle count, and whether small or large particles predominate, is much more valuable.
The remaining cholesterol complex with which you might be familiar is the high-density lipoprotein (HDL), which takes cholesterol back to the liver for recycling. These tiny but powerful cholesterol complexes are often called the “good cholesterol” or “nature’s garbage trucks” because HDLs also clean up any damaged or oxidized cholesterol that might cause problems later. They are particularly important for their role in preventing atherosclerosis, a build-up of plaque in your arteries that is often a precursor to heart attack or stroke. Atherosclerosis can occur when those small, dense LDLs get stuck in the arterial walls and oxidize, and the immune system fights back with macrophages (white blood cells) that scavenge the oxidized LDL. The macrophages end up converting into foam cells—fat-laden cells that themselves build up in the artery, causing or exacerbating atherosclerosis. HDL can remove cholesterol from these foam cells. Scientists generally agree that the more HDL you have, the lower your risk for heart disease. That’s why Big Pharma has tried—so far unsuccessfully—to create an effective drug to raise HDL and address existing atherosclerosis. (Some physicians prescribe the combination of prescription fibrates and over-the-counter niacin to raise HDL, but this treatment can be problematic and is not widely used.)
Research has shown that people with Metabolic Syndrome or type 2 diabetes all have elevated levels of both triglycerides and small, dense LDL particles. As you might have imagined, they also typically have high triglycerides and low levels of beneficial HDL. Of course, these same people have substantially increased risks for heart disease and stroke. Exercise is one of the cheapest, easiest, and most effective ways to raise HDL. Consuming saturated fat is another!

Dr. Cate Shanahan hanging around Lakers headquarters, ready to plan healthier road trip meals.

Dr. Ronesh Sinha lectures to physician groups about ancestral health principles. His success in expanding traditional treatment perspectives is bolstered by the awesome results he gets with his high-risk patients, without drugs.

Dr. Doug McGuff urges you to get fit and take responsibility for your own health—so you don’t have to meet him in the ER someday!
It follows from our discussion of the various lipoproteins that the blood value we’ve been obsessed with for decades—total LDL cholesterol (irrespective of particle size)—is only a small part of the heart disease risk story. A slew of other blood markers may better predict your potential for inflammation and LDL oxidation and the chronic diseases that occur as a result. Dr. Cate Shanahan—author of Deep Nutrition and Food Rules, nutrition director for the Los Angeles Lakers, Primal Blueprint Podcast recurring guest, and family physician in Denver, CO, specializing in medically supervised weight loss through primal-style eating—suggests that your triglycerides-to-HDL ratio is perhaps the best way of monitoring heart disease risk It’s critical to get your ratio to 3. 5:1 or better, and 1:1 or better is considered superior. Remember, high triglycerides suggest the body’s cholesterol processing system is overwhelmed, and you likely have an abundance of small, dense LDL loitering around, ready to cause trouble. Meanwhile, a high level of HDL arms your vascular system for battle, while suboptimal levels of HDL leave your body vulnerable to oxidation and inflammation.
Regarding the folly of tracking total LDL without respecting particle size or looking at the bigger picture of inflammation markers, Dr. Ronesh Sinha, author of The South Asian Health Solution and internal medicine specialist in Silicon Valley, references a UCLA meta-analysis (which synthesizes the results of many independent studies) showing that 75 percent of patients hospitalized for a heart attack had an LDL of less than 130 mg/dl (widely accepted as “safe”), and that half of the victims had an LDL under 100, widely considered “ideal.” Unfortunately, as Dr Sinha explains, instead of taking a holistic view of how all risk factors interplay, “[M]any physicians and drug companies are interpreting the results of the UCLA meta-study to mean we should set our LDL targets even lower.”
Dr. Doug McGuff, a South Carolina emergency room physician, co-author of The Primal Prescription and fitness expert advocating high-intensity exercise to optimize health and delay aging, reminds us that the “beast” that is mainstream health and medicine moves very slowly, and it’s up to us to think critically about the latest research and take personal responsibility for our health. “It’s certain that the science will reshape conventional wisdom (to honor many of the evolutionary health-based notions presented in this book and elsewhere), but it’s going to take 20 years. Personally, I don’t feel like waiting that long.”
It’s heartening to see pioneers like Drs Shanahan, Sinha, and McGuff making their valiant efforts to reshape culture and improve the lives of the patients they treat directly, and also to observe mainstream media beginning to investigate ideas that counter the dogma we’ve been fed for many decades Indeed, it will take many more years for the masses to come around, for the random passenger next to you on the airplane to eagerly join the conversation instead of drawing a blank when you say the word “primal” (not to mention, request a gluten-free airline meal instead of mowing down on snack pretzels). When you experience stunning health and body-composition breakthroughs from primal living, it’s easy to allow your enthusiasm to overwhelm others who have not yet “seen the light.” I want to caution you against evangelism when it comes to any kind of lifestyle change. This area tends to be a sore spot for many people, dredging up years of weight-loss failures and frustration. The best approach is to set an example of healthy living with a willingness to think critically in the face of irresponsible or dated dogma (e.g., “I’ve decided to reduce my intake of carbs to get my triglycerides down and eventually go off statins. How does that sound doc?”).

While cholesterol in and of itself is popularly blamed for heart disease, we should really be pointing fingers at oxidative damage as the proximal cause. Because lipoproteins have a lipid surface, they are subject to oxidation. Like oils left open in your kitchen, they can go rancid when they come in contact with oxygen. When this happens, lipoproteins—and the cholesterol inside—can become damaged. As mentioned previously, small, dense LDLs are small enough that they can get trapped in the spaces between endothelial cells lining the arteries (sometimes called gap junctions). Even if they are not oxidized to begin with, once trapped, LDLs can oxidize in place because they are sitting there continually exposed to oxygen passing by that’s attached to hemoglobin in the red blood cells.
Either way, this oxidation eventually causes injury and inflammation to the arterial wall, prompting the body’s immune system to send macrophages (scavenging white blood cells) to gobble up the oxidized LDLs. The immune system tries hard to do its job, but the macrophages can become overwhelmed by absorbing so much oxidized LDLs. The consumption of oxidized LDLs causes certain genes to convert these macrophages into foam cells that attach to the arterial lining, laying the foundation for future trouble. The damaged area, known as a lesion, prompts more macrophages to come to the rescue. They try to gobble up more and more oxidized LDLs floating by, increasing the severity of the lesion over time. This is how plaques accumulate on the arterial wall, a saga with which you are no doubt familiar thanks to the myriad Big Pharma drug ads aimed at this problem. Arterial plaques grow and eventually compromise the inner diameter of the artery. If allowed to continue, this process can eventually occlude blood flow, or plaques can rupture and release clots into the bloodstream, preventing blood—and oxygen—from reaching a vital organ. This describes your classic heart attack or stroke. (By the way, atherosclerosis occurs in the arteries and not the veins because venous blood has very little oxygen.)
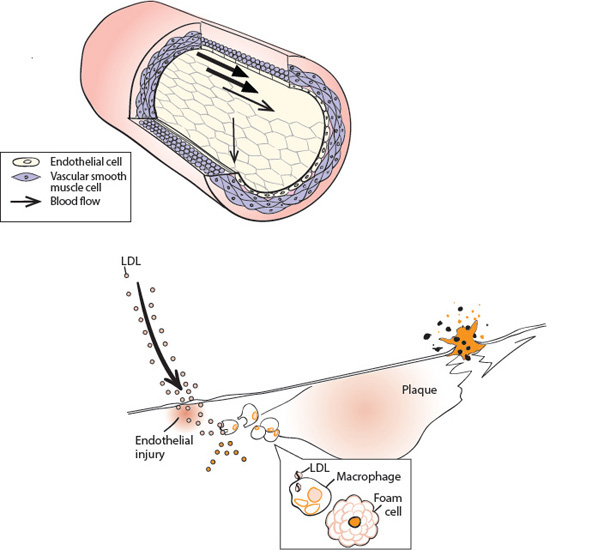
Small, dense LDL lodge on the endothelial cell layer; macrophages come to the rescue and blow up into foam cells; plaque forms, leading to heart attack or stroke.
Of course, oxidation happens all the time throughout the body, and we have evolved some effective antioxidant systems (namely catalase, superoxide dismutase, and glutathione) to prevent too much of this damage from getting out of control. Furthermore, consuming ample levels of high-antioxidant foods (vegetables, fruits, nuts and seeds, and dark chocolate) and antioxidant supplements (such as vitamin E, CoQ10, beta-carotene, and lycopene) can help mitigate some of the damage. It’s also extremely convenient that HDLs can remove some of the damaged cholesterol and take it back to the liver for recycling. Your cholesterol processing system has evolved to expect a certain range and quality of dietary fat, protein, carbohydrate, and antioxidants, as well as a certain level of exercise (to help promote insulin sensitivity in the muscles and maintain high levels of HDL) to provide appropriate gene signals and avoid artery disease. The cholesterol processing system has served humans and most other mammals well for millions of years—until recently.
The oxidation of small, dense LDLs—and the concomitant inflammation and disease that are so now common—most likely happens for a variety of reasons that have to do with modern dietary habits more than anything else. A major culprit is a high intake of unstable high polyunsaturated fats from vegetable oils in the diet. (High polyunsaturated fats incorporated into the lipid layer are much more prone to oxidation than are saturated fats.) Due to vegetable/seed oils’ high-temperature processing methods involving toxic chemical solvents—combined with these oils’ extreme sensitivity to heat, light, and oxygen—they are essentially a bottled source of free radicals. They accelerate aging, are directly linked to assorted cancers, hamper immune and cardiovascular function, and can severely compromise your ability to remove excess body fat. Dr. Shanahan asserts that the direct and immediate damage that industrials oils inflict at the cellular level makes them “literally no different than eating radiation.”
Potential damage is exacerbated by the Standard American Diet, with its focus on consuming (insulin-promoting) whole grains and reducing healthy fats from animal sources and nuts. Diets rich in processed carbs are often also low in natural antioxidants, which would otherwise mitigate oxidation. High-carb diets have also been implicated in low HDL cholesterol readings, and remember that HDL can removed oxidized lipids and combat oxidative damage.
Unfortunately for some of us, poor diet, lack of exercise, stress, certain drug therapies, and, yes, family genetic history can all contribute to the increased production of the dangerous small, dense LDL particles. Your doctor can test for them if you ask, but most common blood tests don’t yet distinguish between the benign “fluffy” forms of LDL, sometimes called pattern A, and the small, dense particles, called pattern B. A comprehensive lipid blood panel such as the Berkeley HeartLab test will typically provide values for total cholesterol, HDL, LDL, VLDL, and triglycerides and indicate relative particle sizes.
It is important to remember that the oxidation and inflammation process described has little or nothing to do with your total cholesterol or even your total LDL cholesterol levels. In most cases, atherosclerosis is a result of the oxidation of a small fraction of the total amount of LDL in your blood—the small, dense LDL particles. If you have low triglycerides and high HDL (indicative of minimal small, dense LDL), your risk of heart disease drops dramatically. Also, if your HDL is high, it’s very unlikely that you’ll encounter a problem, because HDL does such a great job of scavenging the oxidized cholesterol from LDL in the bloodstream.
A physician will generally dispense medication if your total LDL levels exceed a certain figure (this varies by doctor and individual patient profile), knowing your body will respond to the statins with a quick overall reduction regardless of particle size. This will indeed lower all forms of LDL (including both the neutral and harmful kind), but a much more sensible—and safer—option is simply to alter dietary and exercise habits and minimize insulin production, thereby preventing excess accumulation of triglycerides in the blood and allowing the cholesterol system to work as intended. In fact, the combination of low carbs and good fats in primal foods will generally raise HDL and lower both triglycerides and small, dense LDL.
Meanwhile, compelling evidence suggests that Primal Blueprint-style eating and exercising will allow you, regardless of your genetic predisposition, to essentially have no participation in this heart disease saga whatsoever. If you feel any hesitation here, go get a “before” blood panel, eat primally for 21 days, and then get another panel. It’s virtually certain you will see an impressive alteration of unfavorable numbers, giving you the motivation and clarity you need to plunge wholeheartedly into primal eating.
Now that you know more about the different types of cholesterol, isn’t it disappointing to discover that statins and other cholesterol-lowering meds do not have any ability to influence LDL particle size and can only lower total LDL by reducing both the neutral and harmful versions? The fact that some people taking statins experience a dramatic reduction in total cholesterol or in LDL means very little in the context of the true oxidation- and inflammation-based nature of heart disease. To be clear, statins do slightly reduce the risk of heart attacks among men under the age of 65 who have had a prior heart attack. However, many doctors now believe that these benefits are independent of their “cholesterol-lowering” properties and instead come from an anti-inflammatory effect that addresses the more proximate cause of heart disease. A cheaper and more effective anti-inflammatory effect can be achieved for most people by eating foods high in omega-3 or taking fish oil supplements, exercising sensibly instead of chronically, and getting more sleep if you are deprived.
HDL does a great job of scavenging the oxidized cholesterol from LDL in the bloodstream…. If your HDL is high, it’s much less likely you’ll encounter a [heart disease]problem.
By simply adopting the Primal Blueprint laws, you can enjoy superior results without the perilous side effects and huge expense of drug therapy. In the case of statins, known side effects include chronic fatigue, tendon problems, cognitive problems, impotence, blood glucose elevations, and muscle pain, weakness, and numbness. Recent data even suggests an increased risk of developing diabetes as a result of taking statins. These side effects are believed to be due in large part to statins’ interference with the normal production of a critical micronutrient known as coenzyme Q10 (CoQ10). CoQ10 is essential to healthy mitochondrial function (energy production) and defending your cells against free radical damage. Statin therapy is believed to lower CoQ10 levels by up to 50 percent. Ironically, CoQ10 plays a particularly important role in the healthy function of the cardiovascular system, and heart attack patients show depressed levels of CoQ10! Some researchers suggest that statins’ depletion of CoQ10 may nullify any potential benefits of statin therapy.

Statins are prescribed freely despite meta-study data suggesting that low LDL levels are not protective against heart attacks, and despite energy-sapping, health-compromising drug side effects.
The long and short of it is, statins offer only a small degree of protection against heart attack and stroke (and only in some segments of the population), little or even no apparent benefits in terms of life span (especially among those who don’t already have heart disease), and significant side effects in a larger percentage of the patient population than they help. So why are millions being advised to take dangerous, powerful drugs when lifestyle intervention is more effective and less expensive and has no side effects? Perhaps we like to search for easy answers with quick results, and statins produce a graphic and quick decline in blood cholesterol levels. Like other elements of conventional wisdom, there are billions of dollars invested and powerful market forces pushing us in the direction of swallowing drugs and their side effects, while the full story is lost amidst the hype of “lower your numbers quickly!”
If you are currently taking statins or other medications, I realize that asking you to question conventional wisdom and the specific recommendations of your trusted physician can put you in a very uncomfortable position. I strongly urge you to engage in lifestyle modification (after all, there are no side effects or potential compromises to your drug regimen when you improve your diet), while concurrently addressing the possibility with your doctor of gradually reducing your dependence on medication based on the ensuing favorable blood test results.

HOW TO SNEEZE AT HEART DISEASE
The catchall term Metabolic Syndrome is used to describe an assortment of heart disease risk factors widely attributed to today’s prevailing poor dietary and exercise habits. The highly respected Cleveland Clinic states that “the exact cause of Metabolic Syndrome is not known... [but] many features are associated with insulin resistance.” The following five markers are universally used as reliable indicators of Metabolic Syndrome:
1. Elevated fasting blood glucose of 100 mg/dl or greater.
2. Blood pressure of 130/85 mm Hg or greater.
3. Waistline measurement of 40 inches or more for men and 35 inches or more for women.
4. HDL of less than 40 mg/dl for men and less than 50 mg/dl for women.
5. Triglycerides of 150 mg/dl or greater.
Individuals with three or more of these markers are said to have Metabolic Syndrome. The U. S. government and other sources report that some 47 million Americans—that’s one in five!—meet the conditions to be diagnosed with Metabolic Syndrome It’s a chronic condition that develops and worsens over time (with no discernible physical symptoms, except that expanding waistline...) unless you take dramatic steps to alter your lifestyle. The Cleveland Clinic and Journal of the American Medical Association report that more than 40 percent of Americans in their 60s and 70s have this condition.
A routine physical exam and blood panel will give you an indication of your Metabolic Syndrome status. Many experts recommend a few additional blood tests to assess overall health and risk factors, including:
C-Reactive Protein: High sensitivity C-reactive protein (hs-CRP) is produced by your liver as part of an immune system response to injury or infection. In the absence of other acute infections, high levels of hs-CRP in your blood are indicative of systemic inflammation. Because atherosclerosis is primarily a disease of inflammation, some researchers contend that hs-CRP is a strong predictor of your heart disease risk, and indeed elevated hs-CRP is associated with an increased risk of heart attack, stroke, and sudden cardiac death. Given that cholesterol tests have become less reliable in predicting risk, especially among those with normal or low cholesterol levels, hs-CRP seems to be a good alternative.
Lp2A: Another key inflammation marker associated with small, dense LDL particles.
A1c (estimated average glucose): A1c measures how much glucose is attached to a hemoglobin molecule, a reliable marker for the dangers of elevated blood glucose levels over an extended time period. This is a good companion test to the aforementioned fasting blood glucose readings (the first Metabolic Syndrome indicator above).
Fasting Blood Insulin Levels: High fasting insulin levels are indicative of prediabetic conditions.

HEART DISEASE PREVENTION TIPS
If you are diagnosed with (or are on the cusp of) Metabolic Syndrome, following the Primal Blueprint for 21 days can turn four of the five Metabolic Syndrome markers around (it might take a bit longer to get your waistline back in the safe zone) and cause your heart disease risk to plummet—even if you have a family history of obesity, high cholesterol, and heart disease Here are some specific recommendations and corresponding benefits of following the Primal Blueprint:
Ditch Industrial Oils: Eliminating consumption of processed sources of polyunsaturated fats—namely the refined vegetable/seed oils and margarines we’ve been told to use in lieu of butter—gives you a greater proportion of saturated (and therefore oxidation-resistant) fats in lipoprotein lipid layers and fatty membranes. Increased consumption of omega-3 oils—best sourced from oily, cold-water fish like sardines and wild salmon—helps control inflammation, the precursor for atherosclerosis and virtually all other metabolic diseases.
Exercise Primal Blueprint Style: A sensible blend of low-level cardio, regular strength training, and occasional all-out sprints helps lower LDL and raise HDL. On the flip side, chronic cardio can cause you to lose these benefits and actually increases heart disease risk factors!
Increase Antioxidant Intake: If your antioxidant intake is appreciable (eating your vegetables?), you’ll help boost your natural defenses against oxidation.
Reduce Carb Intake, Especially Refined Carbs: Dr. Richard Fein-man, one of the most frequently published and highly regarded researchers in the fields of nutrition and metabolism, has suggested that “Metabolic Syndrome may be defined by the response to carbohydrate restriction” (meaning that if you restrict carbs and your symptoms are improved or alleviated, carb intake is the defining variable in Metabolic Syndrome). Reducing your carb intake will help lower your production of triglycerides, raise HDL, lower LDL, and dramatically reduce your level of small, dense LDL (because it is high levels of triglycerides that prompt small, dense LDL production).

A major feature of Primal Blueprint eating is that it provides high levels of healthy saturated and unsaturated fats. While conventional wisdom generally contends that saturated fats should be diligently restricted, they are an excellent energy source and offer a variety of nutrients critical to health. Consuming ample amounts of saturated fat helps prevent direct oxidative damage to your cells. (Saturated fat is an integral part of cell membranes.) While your eyes might bug out at the following statement, it’s virtually irrefutable and proven by many respected long-term studies:
Eat (healthy) fat to help prevent cancer and heart disease. Avoid fat and increase your risk of cancer, heart disease, and even obesity.
Fortunately, omega-3 polyunsaturated fatty acids don’t have an image problem and are universally regarded as healthy. Adequate omega-3 consumption supports healthy cardiovascular, brain, skin, and immune function. By turning on genes that improve blood circulation, reducing inflammation, and supporting healthy cholesterol and triglyceride levels, omega-3s help reduce the risk of high blood pressure, blood clots that cause heart attacks, arthritis, autoimmune disorders, and cognitive problems such as depression, Alzheimer’s, and even ADHD. The important role of omega-3s in supporting cognitive function is made even more evident by the fact that half the brain consists of fat, including concentrated levels of the omega-3 docosahexanoic acid, or DHA.
Another form of polyunsaturated fat called omega-6 plays a vital role in our health as well, but its extreme prevalence in the Standard American Diet—from undesirable sources like vegetable oils, grain-fed animal fats, bakery items (donuts, cookies), and processed snacks that almost universally contain soybean oil or corn oil—leads to a dangerous imbalance of excessive omega-6 and deficient omega-3. The ideal omega-6:omega-3 balance (O6:O3) is 1:1 or 2:1, ratios that Grok likely met with ease. Even 4:1 is okay today, but the typical modern eater has an O6:O3 ratio of 20:1, or even 50:1! Imbalanced fatty acid intake can exacerbate the insulin resistance problem discussed earlier. Omega-6 fats (particularly arachidonic acid) suppress expression of the insulin receptor gene GLUT4 (promoting more fat storage), while omega-3 fats increase expression of GLUT4 (promoting insulin sensitivity and less fat storage).
High carbohydrate intake increases your risk of cancer, heart disease, and obesity. Cutting carbs and increasing intake of (healthy) fat lowers your disease risk and helps you maintain healthy body composition.
For years, the O6:O3 ratio has been a popular discussion topic in the primal and paleo scenes, and unfortunately, the message has become oversimplified and distorted to omega-3s are anti-inflammatory—“good”—while omega-6s are pro-inflammatory—“bad.” This had led savvy enthusiasts to scale back consumption of healthy foods like nuts, most of which are predominantly omega-6. However, more recent research has shown that the concerns about O6:O3 imbalance stem mainly from the ingestion of heavily processed, high-omega-6 oils in junk foods—vegetable oils, margarine products, and processed, packaged, or frozen meals or snacks—that inflict oxidative damage on the body. (It’s also possible that if you aren’t eating much oily, cold-water fish, you could fall a little short of optimal omega-3 intake. More on this in Chapter 5.)
When you consume a diet laden with oxidized oils and introduce other inflammatory influences into daily life (such as insufficient sleep, overly stressful work patterns, and chronic cardio exercise habits), your genes respond by doing what they’re told to do according to these signals and you experience a programmed inflammation response throughout the body. Under normal circumstances, inflammation is your body’s highly desirable first line of defense against pain, injury, and infection. Inflammation processes detect and destroy toxic material in damaged tissue before it can spread to the rest of the body. Consider examples like a bee sting, taking an elbow to the face, or turning an ankle on a hiking trail. The reddened skin, black eye, and ballooned ankle help your body quarantine the damage from the trauma to the inflamed areas instead of letting toxins run wild through the bloodstream.
Unfortunately, an out-of-control inflammation response (also known as systemic inflammation)—resulting from stress and imbalanced dietary and exercise habits—confuses your body into thinking it’s under assault from destructive, infectious foreign agents or that a major trauma has just occurred. That’s when the disease process begins.
In my own athletic example, the extreme stress of my chronic cardio training regimen coupled with my highly inflammatory grain-based diet led to excessive and prolonged inflammation throughout my body as evidenced by repeated injuries and illnesses I couldn’t shake. What I should have been seeking was a more desirable temporary state of moderate inflammation (pumped muscles, elevated heart rate, oxygenated lungs) from a Primal Blueprint-aligned training regimen and plenty of recovery time for my body to return to homeostasis. The systemic inflammation I experienced from overtraining tore down my muscles, joints, and immune system.
Interestingly, after extreme endurance events like a marathon or iron-man triathlon, blood levels of CPK (creatine phosphokinase, an enzyme that leaks into the bloodstream when muscle, heart, or brain tissue is traumatized) can be elevated for weeks. In fact, if you ran a marathon and then—just for kicks—immediately headed over to a hospital emergency room for a blood draw, a doctor might think you were suffering from a heart attack! In my case, when I adjusted my diet and training habits, virtually all my inflammatory and immune-suppressing conditions vanished.
We know that most forms of systemic inflammation have a strong dietary component and can usually be resolved with a few dietary modifications. Nevertheless, conventional wisdom within the medical community has recommended fighting our widespread inflammation-related health problems with corticosteroids, COX-2 inhibitors such as Vioxx and Celebrex, and other nonsteroidal anti-inflammatories. (Asthma meds work on a similar chemical pathway.)
I have a nonscientific name for this approach: digging a hole to install a ladder to wash the basement windows. As you might imagine, because these medications interfere with normal hormone pathways and gene expression, they almost never address the underlying cause of inflammation. They simply mask the pain in the short term—if they mask it at all. Dietary modification (and exercise modification if you are currently overdoing it) is almost always a superior method of treatment and protection against pain and serious diseases triggered by systemic inflammation.
I have a nonscientific name for treating lifestyle-related health problems with pharmaceuticals: digging a hole to install a ladder to wash the basement windows.

The Primal Blueprint eating style, with its emphasis on nutritious, inflammation-reducing foods and its aversion to processed, pro-inflammatory foods, will help you naturally avoid the systemic inflammation that is now believed to be the root cause of the major health problems affecting modern humans.
The Primal Blueprint is about enjoying a healthy, happy, balanced lifestyle. As Dr. Andrew Weil said in describing the title of his book Eating Well for Optimum Health, “eating well” refers not only to choosing natural, nutritious foods, but also to enjoying the experience as one of the great pleasures of life. It’s likely that Grok appreciated food much more than we do today because he had to work so hard for his meals and was never assured of success. Throughout history, food has represented a centerpiece of cultural celebration—let’s not kill the momentum now! The key to eating well is to eliminate distractions and negative influences while you are eating. This will allow the physical sensations of hunger and the simple pursuit of pleasure to have predominant influence on your dietary habits.
If you wish to succeed with healthy dietary habits, it’s important that you discard any negative emotions you have toward eating and embrace each meal as an opportunity to enjoy yourself. I strongly recommend that you give yourself permission to eat as much as you want, whenever you want, for the rest of your life. While this suggestion might scare the heck out of you, releasing yourself from restriction and deprivation enables you to become more connected with your physical nutritional needs rather than being driven by emotional triggers.
Take notice of that point in every meal where you have attained satisfaction and feel comfortable stopping—not the point at which you are stuffed full and need to take your belt out a notch, but the point at which you are no longer hungry for the next bite—knowing that you can eat again whenever you like. If you wish to enjoy a treat once in a while, choose with discretion and enjoy it with full attention and awareness to the pleasure that every single savored bite gives you. Reject feelings of anxiety, guilt, or rebellion connected to your food choices, and replace them with the idea that you deserve to eat the most delicious, nutritious foods possible.
When it comes to what to include or exclude, or how to dial in the perfect food choices for you, I prefer to let my taste buds guide me to the most enjoyable and nourishing food choices within the broad guidelines of the Primal Blueprint. Forget the scientifically unproven admonitions to eat certain macronutrient combinations at certain times, or to align your food choices with your racial heritage or blood type, for example. Despite whatever percentages your genetic heritage test from ancestry.com reveals, we are all East African Homo sapiens for purposes of eating foods that promote optimal gene expression.
There are foods that are unhealthy for all humans (e.g., refined carbohydrates and industrial oils) and other foods that are more problematic for certain humans than others (e.g., sensitivity to fat storage with carbohydrate intake). While not every primal-approved food will be healthy for every human (e.g., some have allergies or autoimmune responses to certain vegetables, nuts, or even eggs), all humans can craft an enjoyable, varied, and healthy diet from the list of primal-approved foods.
Essentially, my goal is for you to become a modern forager with a keen sense of what you need to do (or not do) to thrive day in and day out. When you eat Primal Blueprint style, there is no city to which you can’t travel, no restaurant at which you can’t eat, no grocery store in which you can’t shop, and no family holiday you can’t endure!
While those immersed in carbohydrate dependency from SAD eating patterns will become hungry and irritable when missing even a single meal, you can free yourself from dependency on regular meals when you become fat-adapted through a sustained period of primal-aligned eating. Our ancestors ate sporadically—with continually varied mealtimes and food choices. Given seasonal variables and hunting success or failure, they didn’t always have enough food or a varied diet. Our genes thrive on intermittent scarcity and can even handle occasional excess. In fact, they expect it.
Our genetic ability to thrive on intermittent eating habits is an important concept to grasp, because it unburdens you of having to eat every meal on a set schedule, to balance food groups (meat with starch, grains with protein, etc.), or to align your foods with time-of-day traditions (cereal for breakfast, sandwich for lunch, etc.). Skipping meals, fasting briefly, and simply freeing yourself from an obsessive need to eat three squares or six small meals a day when the clock strikes a particular hour will most definitely benefit your body by improving your ability to tap into stored body fat for energy, optimizing cellular repair, moderating your appetite, and enhancing your appreciation for the meals you eat when you’re actually a little, or a lot, hungry! Unburdened by the strict and ill-advised “rules” of conventional wisdom, eating becomes much simpler and more intuitive, relaxing, and enjoyable.
On this topic, it’s interesting to note that your need to consume calories on a regular schedule will diminish substantially when blood glucose levels are moderated and you start burning fat and ketones (as discussed in Chapter 4) more efficiently through low-insulin Primal Blueprint dietary choices. By contrast, if you eat the typical Western diet of 300 to 500 grams of carbohydrates per day (instead of the 100 to 150 from high-nutrient plant sources as suggested by the Primal Blueprint), you are going to experience significant blood glucose fluctuations and corresponding cravings for quick-energy, high-carbohydrate foods. This is perhaps the single quickest and most exciting revelation for converts to the Primal Blueprint eating style. By eliminating sweetened beverages, sugars, grains, and highly refined vegetable or seed oils from your diet and emphasizing primal foods, you will experience more consistent energy levels and a comfortably diminished appetite. You’ll become a fat-burning beast!
By eliminating sugars, grains, and legumes from your diet and emphasizing primal foods, you will experience more consistent energy levels and a comfortably diminished appetite.
These benefits will be long lasting, but they might take a bit of time to realize. Every once in a while, people commenting on MarksDailyApple.com mention difficulties with energy level swings during the first three weeks of their transition to a primal eating style. During this transition period, your body expects sugar as fuel (of which it’s probably getting considerably less) but hasn’t rediscovered yet how to get the most out of its fat reserves. Don’t worry, it will. By limiting carbs (and, hence, lowering insulin) you are sending a new series of hormonal signals to your genes. In turn, they are downregulating their sugar-burning systems and upregulating their fat- and keto-burning machinery.

I love my morning routine as much as any breakfast enthusiast; there Is just no food Involved. Instead, I take a cold plunge for a brief, natural stressor and then enjoy a deliberate cup of coffee.
While you may experience a few episodes of lightheadedness during your transition (because your body is relearning how to sustain energy without constant carb infusions), rest assured that the shift will be complete in a few weeks. Energy levels, appetite, mood, and cognitive ability will stabilize even when you eat sporadically. During your transition from carb dependency to fat-adaptation, you can do everything possible to make things smooth and comfortable. Going primal is not about struggling, suffering, starving, or fighting through cravings with willpower. Instead, you can surround yourself with satiating, high-fat foods to enjoy whenever you feel an energy dip or have a hankering for one of your old standby snacks. These primal food choices will totally satisfy you without bringing about a sugar crash later, as will happen when you reach for a bagel or energy bar. This is due to the high caloric density and slow burn rate of foods high in fat and/or protein (such as meat, fish, fowl, eggs, avocados, butter, coconut products, nuts and seeds, olives, and high-fat dairy products) and the high water and fiber content of vegetables and fruits.
Because modern life is all about schedules, we often find it convenient and enjoyable to eat regular meals. This is fine. I’m simply suggesting you pay more attention to your hunger levels than to the clock. For example, over the years of primal living I have become accustomed to skipping breakfast and eating in a compressed time window of around noon to 7 P.M. each day. I’m not doing this for weight loss or to save money on eggs; it’s simply a routine I’ve arrived at that gives me the most pleasure. By the time lunchtime rolls around, I’m ready to enjoy my biggest meal of the day. I might even enjoy a “breakfast” offering like a world-famous MarksDailyApple.com Big Ass Omelet (three eggs, cheese, chopped mushrooms, peppers, onions, and tomatoes, and topped with some bacon and avocado), or a Big Ass Salad with assorted fresh veggies, nuts, and steak, chicken, or tuna. Other days, especially when I’m traveling, I’ll just have a Primal Fuel smoothie during the day and carry on until dinner.
When your food choices and meal times are flexible, you feel less stress and more pleasure from your diet. The key is to make informed choices that minimize your exposure to toxic foods and, when you indulge or get off track, allow your body to return quickly to balance. If you enjoy a decadent dessert or a weekend away from healthy food options, simply eat a few low-insulin-producing meals in a row and return to regulated energy levels and optimal metabolic function. Even a short walk, or a quick set of squats or pushups, after a big meal and rich dessert can mitigate the insulin response by diverting glucose from the bloodstream into working muscles.

ONE SMALL SCOOP FOR MANKIND
When you eat Primal Blueprint style, the consequences of your food choices become crystal clear. Eat right and you have discernibly more energy and health. Stick with it, and altering your body composition happens with much less effort than the dated calorie-counting strategies. Slide a little bit, and you might get halfway to your goal, have a little less energy, and maybe catch an extra cold or two due to compromised immune function (due in part to insulin-driven sugar crashes and cravings).
And with this goes my chances for a dairy council endorsement deal...
Every once in a while, I’ll give in to temptation and indulge in something like a small scoop of gourmet ice cream. It tastes delicious for the few minutes it takes to eat it (though not quite up to par with a bowl of fresh blueberries and raspberries with homemade whipped cream), but invariably I experience bloating and gas in the ensuing hour as well as a discernible sugar crash When I lay down at bedtime, I can detect a slightly elevated heart rate and have some difficulty falling asleep normally. Because these lapses are out of my normal pattern, I am highly sensitive to the consequences of choices like these. Heaven knows that back in the day I could polish off an entire half-gallon of ice cream over the course of a leisurely evening to no ill effects—that I was conscious of at the time.
The important point here is that I enjoy the taste of ice cream as much as anyone, but I will reassert my position that after eating primally for some time, even the occasional treat that’s not Primal Blueprint approved isn’t worth it for me once I weigh the fleeting pleasure against the lingering post-consumption effects on my body. You may feel like you can handle your routine of lime mojitos, strawberry daiquiris, high-carb finger foods, or occasional rich desserts on the holiday party circuit with no ill effects. But it’s only when you eliminate these indulgences for a significant time period that you are truly able to compare and contrast the negative impacts on your body from these influences. Over time it becomes easier to stay the course, or to recalibrate quickly when you do decide to occasionally indulge yourself.
What’s more, you’ll soon learn that much of the emotional comfort related to eating comes not from the food itself, but rather from the rituals surrounding it. Primal enthusiasts discover how easy it is to separate an offensive food from the overall experience Barbequing burgers can still be fun if you opt for a lettuce wrap You can make a tasty soda with carbonated water, some vanilla, big squeezes of lemon and lime, and perhaps a pinch of stevia extract. Heck, there are entire books, like Primal Cravings, dedicated to recipes that replace offensive ingredients with primal-friendly alternatives so you can still enjoy your pancakes, muffins, lasagna, and gelato! There are many ways to enjoy all the pleasures we have learned to associate with food while still making optimal food choices.

Primal Cravings’ Strawberry Shortcake Waffles and Cherry Almond Streusel Muffins
Granted, major lifestyle changes and habit modifications can be a struggle, but the first step toward transformation is to clearly understand the consequences of each and every food (and lifestyle) choice that you make, whether they are aligned with your primal genes or not It is then that you accept personal responsibility for your health instead of hiding behind rationalizations and defense mechanisms like “Everything in moderation,” “You only live once,” “Things are too hectic this month to worry about my diet; I’ll start the program next month,” or “My grandfather smoked and drank and still lived to 98, so I have good genes.” When you tell yourself such stories, you gloss over the fact that the years and decades of those little ice cream outings and extra servings from the bar can literally add up to hundreds of pounds of ingested substances that are toxic to your body. Furthermore, as unhealthy food choices ingrain themselves (pun intended) into your daily life, I believe you become desensitized to the negative effects they have on your health This concept is illustrated by the tolerance levels of heavy tobacco or caffeine users who are able to function somewhat normally (that’s not saying much) with volumes of chemicals in their bloodstream that would floor the casual user or teetotaler.
The complete lack of regimentation or caloric deprivation in the Primal Blueprint eating style (I refuse to use the word diet because it implies regimentation and calorie counting) is the secret to its long-term success You don’t have to force yourself to go hungry or to feel deprived or negative about eating Simply make sensible choices by welcoming the abundant selection of delicious foods whenever you want, and transition out of habitually consuming foods that may taste great for a brief moment but make your body feel bad or create long-term metabolic stress.


While I take great pains to emphasize a relaxed, intuitive approach to primal eating, we have to face the reality that carbohydrate dependency has serious hormonal and psychological underpinnings that require dedication to overcome. Sugar and wheat both have addictive properties, and the insulin roller coaster is difficult to dismount if you allow doses of carbs to leak into the picture here and there... and there... and here. If you adopt an extremely disciplined approach for the first 21 days to ditch sugars, grains, and bad oils, you will build momentum toward fat-adaptation. This will make it much easier over the long term to avoid the backsliding that is so common among dieters, and I fear among primal/paleo enthusiasts who “try” instead of commit. Remember once you become fat-adapted (when you notice your energy levels stabilize throughout the day, and you can skip a meal—or two!—with no ill effects because you are burning off stored body fat for energy), minor departures from primal eating are easily handled by the body because your genes are calibrated to burn fat instead of carbohydrates.
If you argue that life will never be the same without your bowl of Raisin Bran or a heaping plate of pasta and garlic bread, try these suggestions:
80 Percent Rule: When you first make the switch to primal eating, I recommend following the Primal Blueprint recommendations as closely as possible for the first 21 days. That is how long it will probably take initially to break the cycle of carb addiction and to set you on the right path. That is not to say that you will never be tempted by a cupcake or a plate of pasta again—you will. Do the best you can, and relieve yourself from the pressure of perfection. If you make departures from primal-aligned choices, make sure you get back on track quickly to minimize the damage. Over time, as you experience the benefits of making healthy changes, you will naturally and comfortably become more compliant, particularly with the restriction and elimination of grains, sugars, and toxic vegetable oils.
Build Momentum: As you continue to make progress eating the way you were designed to eat, you will notice a heightened sensitivity to how food affects your body, both positively and negatively. During my years as an athlete, I thought my recurrent digestive bloating and post-meal fatigue were due to hard training or simply the end of a long day—not from subclinical allergic reactions to excessive processed carbohydrates and/or dairy products.
Can you relate to that hyper, racing-heart sensation that comes after consuming a sugary dessert? It’s probably something that we’ve been aware of since childhood—a little annoying but no big deal, right? It was only when I started to aggressively clean up my diet a decade ago that my sensitivity went to the next level. What a pleasure it was to leave the dinner table feeling totally satisfied, yet alert and energetic! Passing on dessert took a little getting used to, but I noticed that the sacrifice of a few moments of instant gratification paled in comparison to not having to deal with sugar highs and sugar crashes. Plus, grains and sugars are confirmed to have significant addictive properties. So when you cut them out, you begin to lose your craving for them. (Really!) Hence, you escape the vicious cycle that befalls even those with tremendous willpower trying to do the right thing but eating the wrong stuff.
Five Favorite Meals Strategy: Pick your five favorite Primal Blueprint-approved meals and rotate them for the first three weeks of your transition to Primal Blueprint eating. Maybe it’s broiled salmon with lemon butter and a heaping plate of steamed broccoli or Brussels sprouts loaded with butter. (Sorry Weight Watchers, but eating more fat is how you lose weight and keep it off!) Or lamb chops with grilled zucchini and summer squash (loaded with butter). Maybe rotisserie chicken (with the skin, preferably organic) and a large steamed vegetable (again, loaded with butter) is your cup of tea. Eat as many colorful, creative salads as you want, drizzled with healthy olive oil or avocado oil dressings. Snack liberally on Primal Blueprint-approved snacks. Yes, you are removing the baked potato, corn on the cob, Cheerios, baguettes, and other beige staples from the picture, but the discomfort of a habit change can be greatly minimized when you can look forward to as much as you want of your favorite primal foods during this crucial transition period to the Primal Blueprint eating lifestyle.
Never Struggle, Suffer, or Go Hungry: Surround yourself with Primal Blueprint-approved foods and enjoy them as much and as often as you like. Always have primal snacks nearby to help you through the transition period. That said, pay close attention to your hunger levels, and eliminate emotional triggers that lead to unhealthy eating. Eat because you are hungry, not because you are bored, tired, or stressed. Stop eating when you are no longer hungry, rather than when you feel full, because by then you’ve likely over eaten.
Substitute: Consider whether you can switch out some of your old favorite meals, snacks, and even treats for interesting new Primal Blueprint options. I used to be a big blueberry pancakes and granola guy, but whatever deprivation I might have felt at first in eliminating the “stack” from my life was more than made up for by a dozen bites of a delicious primal omelet. Consider the overall impact of your current favorite foods on your body and if they are all truly worth it. A fine Italian meal of pasta and gelato will please most any palette, but if you feel bloated, gassy, jittery, and then groggy in the hours afterward, a better strategy might be to consider some of the many other delicious, Primal Blueprint-approved items on the menu (or off it, but likely available by polite request) at the same restaurant.
1. Primal Blueprint Benefits: Benefits of Primal Blueprint eating include becoming fat-adapted instead of carbohydrate dependent, enhancing cellular function, improved immune and antioxidant functioning, optimal development and repair of muscle tissue, reduced disease risk factors, and stabilization of daily appetite and energy levels. While primal eating is low-carb in comparison to the Standard American Diet, it advocates abundant consumption of nutritious carbs in the form of all vegetables and some fruits. For body composition goals, 80 percent of your success is dependent upon what you eat, particularly when moderating the wildly excessive carbohydrate intake of the Standard American Diet.
2. Insulin Is the Master Hormone: Perhaps the most important health benefit of eating primally is moderating the wildly excessive insulin production associated with the Standard American Diet. Eighty percent of your ability to achieve your preferred body composition is determined by what you eat, specifically the level of insulin you produce as a consequence of your carbohydrate intake and insulin-desensitizing lifestyle factors. When you moderate insulin production and maximize insulin sensitivity, you access and burn stored body fat for energy, preserve or build muscle, and reduce disease risk factors.
When the delicate insulin balance is abused by years of consuming too many carbs (especially heavily processed ones), havoc ensues: cells become insulin resistant, excess glucose is present in the bloodstream, and more fat is stored, making it increasingly difficult to mobilize that fat as an energy source. This sets the stage for the development of serious conditions such as Metabolic Syndrome, type 2 diabetes, and heart disease. Synthesis of important hormones, including thyroid hormones, testosterone, and human growth hormone is also hindered by excessive insulin production, creating an accelerated aging effect that has more to do with your breakfast choices than chronology. While the long-term effects of excess insulin production are dire, there are also serious immediate drawbacks to consuming high-carb snacks or meals. The sugar high/insulin release/stress response cycle causes problems with fatigue, mental focus, mood swings, and jitters, resulting in burnout.
3. Cholesterol: Cholesterol is critical to healthy cell structure and numerous metabolic functions. Conventional wisdom’s lipid hypothesis of heart disease is now widely acknowledged as a flawed and oversimplified view of the risk factors that contribute to heart disease. The lipid hypothesis has been refuted in recent years by the Framing-ham Heart Study and many other respected studies and experts. The true risk factors for heart disease are best characterized by the common health condition known as Metabolic Syndrome—oxidization and inflammation in the cardiovascular system—which is prompted largely by the ingestion of sugars, grains, and refined vegetable oils. When tracking heart disease risk, blood values like high triglycerides, low HDL, high glucose values, and other inflammation markers are more relevant than the oversimplified obsession with total cholesterol values and the subsequent routine dispensation of statin drugs to lower that number.
What triggers Metabolic Syndrome and other adverse blood values is excessive intake of processed carbs and easily-oxidized fats (trans and refined polyunsaturated fats such as canola, safflower, and soybean oil). Poor exercise habits (either sedentary or too chronically stressful) also promote the inflammation and oxidation symptomatic of Metabolic Syndrome. Raising HDL through consumption of saturated fat and engaging in sensible exercise can help mitigate the potential threat of small, dense LDL becoming oxidized. Conversely, the primary function of statin drugs—lowering cholesterol levels—does not directly address these risk factors. Statins’ purported anti-inflammatory benefits can be easily achieved through diet, exercise, and supplementation, saving the expense and harmful side effects of prescription statin therapy.
The key to preventing heart disease is to ditch toxic vegetable fats, exercise according to the Primal Blueprint plan, increase antioxidant intake, and reduce your intake of grains and sugars.
4. Healthy Fats: Primal foods provide high levels of nutritious saturated, monounsaturated, and omega-3 fatty acids. A diet with ample amounts of these healthy fats supports cardiovascular, brain, skin, and immune functioning as well as increases dietary satiety. Unfortunately, the Standard American Diet features excessive levels of unhealthy oxidized fats and insufficient intake of nutritious fats. This leads to the condition of systemic inflammation, which is a catalyst for many disease processes.
5. Eating Well: Enjoy your meals without deprivation, restriction, emotional stress, or other negativity. Choose your favorite foods from the broad list of Primal Blueprint-approved choices and don’t obsess about calories, nutrient ratios, regimented mealtimes, or food combinations. Eat until you feel satisfied instead of habitually stuffing yourself until you are full (or depriving yourself in the name of weight loss). Realize that your genes evolved to easily handle sporadic eating habits without energy lulls or metabolic slowdowns and can do so after 21 days of reprogramming, allowing you to become a fat- and keto-burning beast!
6. Transitioning to the Primal Blueprint: When adjusting to the Primal Blueprint eating style, choose primal foods that appeal to you (you can rotate them over and over if you like) and discover desirable substitutes for non-primal options to avoid feelings of deprivation from discarding old meal choices. Have plenty of Primal Blueprint-approved foods available for snacks and meals so you don’t suffer, feel depleted, or “cheat” for lack of good options. Be strict in the first 21 days so you can build momentum toward fat-adaptation and make it easier to stay the course over the months, and years, ahead. In the big picture, follow the 80 Percent Rule by being compliant 80 percent of the time and not stressing about perfection. Notice your heightened sensitivity to how foods affect your body, and leverage that awareness to stay on the path of high energy, effortless weight management, and optimal gene expression with Primal Blueprint foods.