Respiration
RespirationIN THIS CHAPTER:
 Respiration
Respiration
 Components of the Respiratory System
Components of the Respiratory System
 Mechanics of Breathing
Mechanics of Breathing
 Respiratory Volumes
Respiratory Volumes
 Gas Transport
Gas Transport
 Regulation of Respiration
Regulation of Respiration
 Solved Problems
Solved Problems
All cells require a continuous supply of oxygen (O2) and must continuously eliminate a metabolic waste product, carbon dioxide (CO2). On the macroscopic level, the term respiration simply means ventilation, or breathing. On the cellular level, it refers to the processes by which cells utilize O2, produce CO2, and convert energy into useful forms.

The major passages of the respiratory system are the nasal cavity, pharynx, larynx, and trachea. Within the lungs, the trachea branches into bronchi, bronchioles, and finally pulmonary alveoli. While the primary function of the respiratory system is exchange of gasses for cellular metabolism, portions of the respiratory system also function in sound production, abdominal compression, and coughing and sneezing. The conducting division of the respiratory system includes all cavities and structures that transport gases to and from the pulmonary alveoli.
Structures: nasal superior septum; middle and inferior nasal conchae.
Tissues: pseudostratified ciliated columnar epithelium; olfactory epithelium
Warms and moistens the inspired air, also functions in olfaction.
Nasopharynx: auditory (eustachian) canals, uvula, pharyngeal tonsils Oropharynx: palatine and lingual tonsils
Laryngeopharynx: larynx
The oropharynx and laryngopharynx have respiratory and digestive functions, while the nasopharynx serves only the respiratory system.
Structures: anterior thyroid cartilage, epiglottis, cricoid cartilage, arytenoid cartilages, cuneiform and corniculate cartilages, and the glottis. The larynx forms the entrance into the trachea. Its primary function is to prevent food or fluid from entering the trachea and lungs during swallowing. A secondary function is sound production.
Structures: trachea branches into right and left primary bronchi, further branching into secondary bronchi, tertiary bronchi, and bronchioles.
Tissues: cartilaginous rings; lined with mucous-secreting pseudostratified ciliated columnar epithelium.
Serves as a conducting system for air. Cartilaginous rings hold passages open.
Structures: continued branching into terminal bronchioles, alveolar ducts, alveolar sacs, pulmonary alveoli.
Tissues: Simple cuboidal epithelium in alveolar ducts, simple squamous epithelium in pulmonary alveoli.
Gas exchange occurs in the pulmonary alveoli, external respiration. Septal cells, which secrete a surfactant that lower the surface tension, and alveolar macrophages that remove foreign debris from the alveolus are found in the alveolar walls.
The paired lungs are contained within the thoracic cavity, separated from each other by the mediastinum (Figure 18-1). Each lung is composed of lobes, and these, in turn, of lobules that contain the alveoli. The left lung has a cardiac notch on its medial surface. It is subdivided into two lobes by a single fissure and contains eight bronchial segments. The right lung is subdivided into three lobes by two fissures, and contains ten bronchial segments.
The lungs are surrounded by a two-layered serous membrane, the pleurae. The inner layer, visceral pleura, is attached to the surface of the lungs; the outer layer, parietal pleura, lines the thoracic cavity. Between the visceral and parietal pleura is a moist potential space, the pleural cavity. Air pressure in the pleural cavity (intrathoracic pressure) is slightly lower than atmospheric pressure in resting lungs. This negative pressure is critical for the thoracic cavity to “pull out” on the lungs causing them to inflate.
Inspiration occurs when contraction of the inspiratory muscles causes an increase in thoracic volume, with expansion of the lungs and a decrease in intrathoracic and intrapulmonic (alveolar) pressures. Air enters the lungs when intrapulmonic pressure falls below atmospheric pressure (760 mmHg at sea level). Expiration follows passively, causing thoracic volume to decrease and intrapulmonic pressure to rise.
You Need to Know 
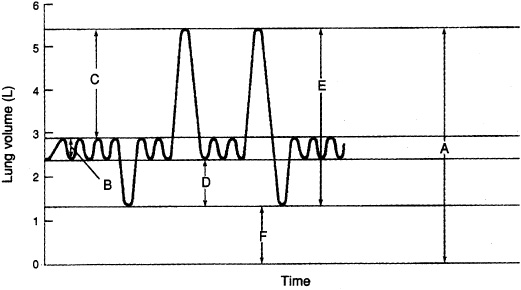
Total lung capacity may be expressed as the sum of four volumes (Figure 18-1): tidal volume, the volume of air moved into and out of the lungs during normal breathing; inspiratory reserve, the maximum volume beyond the tidal volume that can be inspired in one breath; expiratory reserve, the maximum volume beyond tidal volume that can be forcefully exhaled following a normal expiration; and residual volume, the air that remains in the lungs following a forceful expiration. Respiratory air volumes are measured with the spirometer.
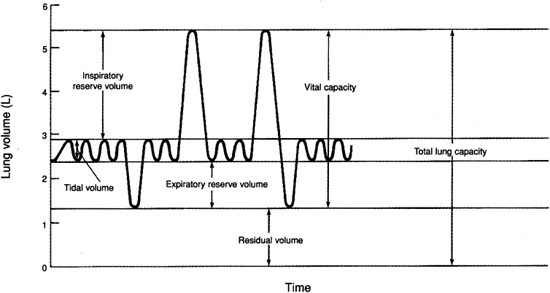
Figure 18-1. Respiratory air volumes.
Minute respiratory volume is the volume of air moved in one minute. A normal value is 6 L/sec. Alveolar ventilation is the volume of air exchanged in 1 minute in the pulmonary alveoli.
Minute respiratory volume = (tidal volume) x (respiratory rate)
Alveolar ventilation = [(tidal volume) - (dead space)] x (respiratory rate)
Dead space is the volume of air in the conducting division, typically 150 ml in an adult.
Up to 99 percent of O2 in the blood is transported on hemoglobin molecules in erythrocytes. CO2 in blood is mostly converted to bicarbonate ions in erythrocytes and released into the blood plasma.
In a mixture of gases, each component gas exerts a partial pressure that is proportional to its concentration in the mixture. For example, air is 21 percent O2, this gas is responsible for 21 percent of air pressure. Twenty-one percent of 760 mmHg = 160 mmHg, the partial pressure of O2. The difference in partial pressures in the alveolus and in the pulmonary capillaries favors diffusion of O2 from the alveolus into the blood and CO2 from the blood into the alveolus.
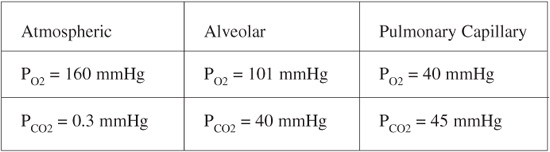
The presence of the enzyme carbonic anhydrase in erythrocytes causes about 67 percent of the CO2 in blood to combine quickly with water to form carbonic acid, most of which dissociates into bicarbonate and hydrogen ions:
CO2 + H2O ↔ H2CO3 ↔ HCO3- + H+
Bicarbonate ions (HCO3-) make up a large part of the blood buffer system. Respiratory acidosis (blood pH below 7.35) occurs when CO2 is not eliminated from the body at a normal rate, increasing vascular PCO2. This can be caused by lung disease or hypoventilation. Respiratory alkalosis (blood pH above 7.45) occurs when CO2 is eliminated too rapidly, decreasing vascular PCO2. This may result from hyperventilation or certain drugs that affect the respiratory control center of the brain.
Control of respiration occurs in the expiratory and inspiratory centers of the rhythmicity area of the medulla oblongata of the brain. When the inspiratory neurons are excited, the respiratory muscles are stimulated to produce inhalation and the expiratory neurons are inhibited. After about 2 seconds the reciprocal process occurs. The medulla also contains chemoreceptors concerned with respiration as do the carotid bodies in the carotid arteries and aortic bodies in the arotic arch. These receptors respond to increased PCO2 by initiating inspiration.
_____ 1. Total lung capacity (a)
_____ 2. Expiratory reserve volume (d)
_____ 3. Vital capacity (e)
_____ 4. Residual volume (f)
_____ 5. Tidal volume (b)
_____ 6. Inspiratory reserve volume (c)