

What is a virus?
How does a virus invade a cell?
What’s the difference between a virus and bacteria?
What are some common viruses?
Why are antibiotics powerless against viruses?
What are antiviral agents?
In their earliest forms, viruses were harmless messengers delivering hereditary information from newly developed life to its offspring in plants, fungi, protozoa, animals, and eventually people.
As viruses evolved and adapted to environmental changes around them, they ceded their messenger roles to cells and took on a more sinister role of infecting genes. In fact, virus is the Latin word for poison.
Some viral infections are short-lived: colds, the flu, sore throats. Others are lifelong: hepatitis and AIDS (caused by the human immunodeficiency virus). Collectively, viral infections represent the prime reason people visit doctors for medical care.
Throughout history, viral epidemics have plagued mankind and proven more powerful than the mightiest of armies. A flu epidemic wiped out Charlemagne’s army in 876 A.D. Thousands of American colonists in the 1720s died after being exposed to a flu virus. The Spanish flu of 1918 killed more than 22 million people worldwide. The Hong Kong flu killed more than 70,000 Americans in the late 1960s. In the early 1980s, a new viral disease surfaced that still plagues us today: AIDS. In the late 1990s, a lethal, fast-killing virus garnered headlines: Ebola. Like AIDS, there is still no cure for Ebola. Today hepatitis has become a major concern as well.
A virus is really little more than a clump of genetic material (DNA or RNA) bunched inside a protein packet. It needs a host cell to survive. Without one, it lies dormant. However, once it infiltrates a living cell within a person, it taps into that cell’s reproductive equipment to duplicate itself. It makes thousands of copies of itself and, in the process, damages or destroys the host cells.
All this cellular debris and loose viral particles signals your immune system to fight back. White blood cells zoom to the infected scene, releasing chemical toxins, fever stimulators, and other agents built to fight invading viruses. Viruses test your body’s infection-fighting capacity. As a consequence, symptoms including pain, redness, swelling, heat, fever, and rash often result. Because a virus is essentially composed only of genetic material, you can see how destroying it can be so challenging.
Fear not. Natural medicine features an arsenal of many solutions. Several years ago, Dr. Yuanhai He, a medical colleague of mine, expressed surprise while watching the television news. Airing was a story about a famous singer who had contracted hepatitis C. After attempts using conventional medicine didn’t ease her symptoms, she said she was too weak to continue and was announcing her retirement from show business. She was frustrated because conventional medicine offered no solutions. This situation startled Dr. He. “That’s so strange. Why didn’t they try Chinese herbs and acupuncture to help her?” he asked. “In China, we routinely treat viral infections like hepatitis with these methods.”
Why indeed. This book teaches you how to take a more active role in maintaining good health. The first step is achieved by understanding how a virus forms. I’ve provided cartoon illustrations in this chapter to help with the explanation. Subsequent diagrams will demonstrate how a virus duplicates, how it differs from bacteria, and how it can elude the immune system. The chapter concludes by providing you with insight into some of the more common and prevalent types of viruses affecting us today.
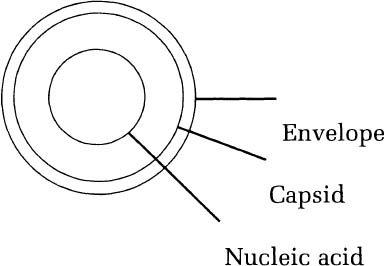
The basic structure of a virus is quite simple. Viruses consist of a nucleic acid (DNA or RNA) enclosed within a protein coat (capsid) and they may or may not be enclosed by a cellular envelope.
The virus, though simple in structure, entirely depends on our cells to supply the machinery necessary to produce more viruses.
1. A virus has a special structure located on its outer surface that allows it to attach to our cells at special sites (receptors).
2. Once the virus attaches to the cell, the virus then enters the cell.
3. Within the cell, the virus sheds its capsid. Then nucleic acid is released into the cell.
4. The virus then uses the cell’s components to replicate viral parts and to aid in the virus assembly.
5. After the new viruses are assembled, they can exit the host cell by one of three ways: by budding off the cell membrane (enveloped virus), cellular destruction (non-enveloped virus), or crossing junctions between cells.
6. The new viruses are now ready to infect other cells.3
It is easy to confuse a virus with bacteria, but they are different types of foreign invaders. True, both have the power to cause an infection. Viral infections tend to be more widespread. Bacterial infections usually are more localized. A middle-ear infection is a common example of a bacterial infection. So is that redness and swelling you notice on a finger cut that was not properly cleaned.
In most cases, your immune system cells quickly fend off a bacterial invasion by simply surrounding and engulfing the bacteria (a process called phagocytosis). Then these cells release chemicals that kill and dissolve the bacteria. Victory is obvious when the site has completely healed.
The following table and diagrams help illustrate the distinctive differences between a virus and bacteria:


Viral Structure
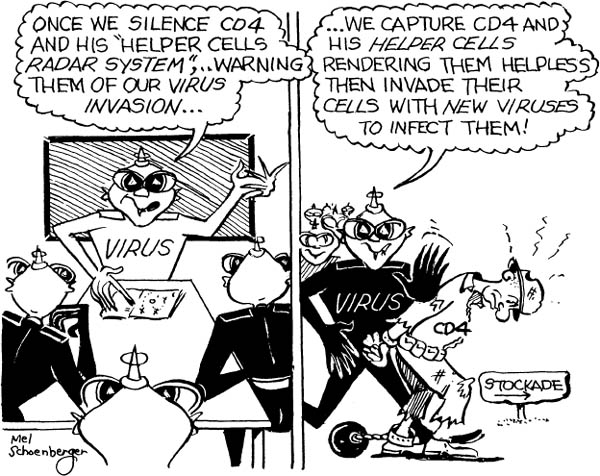
Viruses are stubborn and sneaky and possess a keen sense of survival. The following chart demonstrates how a virus attempts to bypass your body’s built-in alarm system—the immune system.
Viruses can avoid the immune system by several means:
Growing in areas where the immune system has limited access. Viruses grow or are shed into areas that are less accessible to the immune system (i.e., cytomegalovirus [CVM] and the poliovirus in the digestive tract).
Surface antigen changes (mutations). Antigens are found on the cell membranes and tell the immune system which cells are infected. Viruses can alter their antigens, resulting in a delayed response by the immune system. This delay allows the virus time to replicate and assemble new viruses and increases its chances of further spreading the infection. Antigenic changes due to mutation result in a new infection from a different strain of the original viral infection. The new virus strain is relatively unsusceptible to the antibodies of the original viral strain. Mutation can also trigger latent or non-dangerous viruses to become lethal through alterations in the virus’s nucleic acid. Persistence of a viral infection can be due to its ability to mutate into new strains and evade the immune system.

Suppression of the immune system. HIV and Epstein-Barr virus (EBV) infect the immune system, cause direct damage, and lead to the development of other infections [i.e., HIV to AIDS).
Viral infections range from the common cold to the nearly always fatal Ebola. This outline identifies some of the prevalent viruses we face today.
I. Rhinovirus (common cold): The rhinoviruses (over 100 strains) consist of a single-stranded RNA nucleic acid molecule and are not surrounded by an envelope. This virus is responsible for approximately 50 percent of common colds and only infects the upper respiratory tract. Once infected, our bodies make a specific antibody to avoid re-infection by this strain.
II. Hepatitis viruses: These viruses cause inflammation of the liver.
A. Hepatitis A:
1. incubation period: 30 (15–50) days [self-limiting infection]
2. severity: mild to moderate
3. chronicity: no
4. mode of spread: fecal-oral contamination and close personal contact
5. carrier state: none
6. chronic hepatitis development: no
B. Hepatitis B:
1. incubation period: 90 (21–180) days
2. severity: moderate to severe
3. chronicity: yes
4. mode of spread: blood (can live up to 2 weeks outside of body), blood products, sexual intercourse, close personal contact
5. carrier state: yes (10 percent of infected)
6. chronic hepatitis development: yes (5–10 percent of infected)
1. incubation period: 20–90 days
2. severity: moderate to severe
3. chronicity: yes
4. mode of spread: blood, blood products, sexual intercourse, close personal contact
5. carrier state: yes
6. chronic hepatitis development: yes (greater than 50 percent of infected)
D. Hepatitis D:
1. incubation period: 30–50 days (requires Hepatitis B co-infection)
2. severity: moderate to severe
3. chronicity: yes (mainly due to Hepatitis B)
4. mode of spread: blood, blood products, sexual intercourse, close personal contact
5. carrier state: yes
6. chronic hepatitis development: yes
III. Epstein-Barr virus (EBV): EBV is responsible for infectious mononucleosis (IM). The virus has an affinity for the B-lymphocytes of the immune system. In IM, the infected individual has a fever, sore throat, enlarged lymph nodes throughout the body, enlargement of the spleen, and some liver impairment.
IV. Ebola Virus: Ebola hemorrhagic fever was first discovered in Africa, in 1976. There are four types of Ebola virus that cause disease in humans. The Ebola Zaire strain is the most virulent, which is fatal in 90 percent of infected persons. Transmission of the virus is dependent on direct contact with bodily fluids of individuals or contaminated objects such as needles. The virus’s incubation period is approximately 2 to 21 days; it will infect faster if there is a direct route to the bloodstream (e.g., sexual contact). The primary response by the immune system is to produce anti-viral antibodies; unfortunately, they are relatively ineffective, and death results within 7 to 16 days. The specific cause of death is shock, often accompanied by severe blood loss.
V. Hantavirus: Hantavirus was discovered in 1993 after outbreaks of an unidentifiable illness occurred in southwestern areas of the United States. It was found that people became seriously ill through rodents (mainly the deer mouse) that were infected by the hantavirus. The virus is excreted through rodent droppings, urine, and saliva. Thus, any contact with these contaminated substances can make one prone to infection. Direct contact with the virus can also occur through air that has been contaminated by the rodent droppings. The infected rodents have mainly been identified in rural areas.
The illness has an incubation period of 1 to 6 weeks. Symptoms of fever, headache, abdominal pain, muscle pain, nausea, vomiting, cough, and shortness of breath usually develop 1 to 5 days after the onset of symptoms. Respiratory failure and heart failure due to fluid buildup in the lungs can occur. A high fatality rate, of 49 percent nationwide, is reported.
VI. Influenza (Flu): There are three classifications of the influenza virus-A, B, and C. The most common cause of the flu is influenza A. It often occurs in epidemics during the late fall or early winter. The highest incidence of the flu is in schoolchildren. The incubation period is 48 hours. Acute symptoms usually subside in 2 to 3 days. Chills, fever, headache, and muscular aches and pains are the most common initial symptoms, followed by a severe cough. Persons at risk for serious complications include those with chronic pulmonary disease, valvular heart disease, or heart disease.
VII. Human immunodeficiency virus (HIV): HIV specifically attacks the immune system and allows other infections
and/or diseases to develop (e.g., AIDS, fungal infections, pneumonia, etc.). HIV is known as an RNA retrovirus. It uses its RNA to make a double stranded DNA that then becomes part of the infected cell’s DNA. Most viruses do not become part of the cell’s DNA; instead, they use the cell’s components/machinery to manufacture new viruses. The newly incorporated HIV DNA will then be used to make new viruses, but it can be latent for months to years before the development of an HIV infection occurs. HIV depletes CD4+ T-helper cells, which are crucial in avoiding other opportunistic infections that will destroy other cells. Therefore, HIV sets the body up to be attacked by other infections, and with a very low CD4+ count, the development of AIDS results.
Treatment of HIV can be very difficult for two reasons:
HIV’s RNA to DNA incorporation into the cell’s DNA. The virus can be latent for months to years and then suddenly erupt.
HIV’s immunosuppressive effect. HIV lowers immune system response and allows the expression of other infections and disease to arise. How can one increase immune system response when it is under attack?
What about antibiotics? Antibiotics cannot be used for viral infections since they work by destroying the cell walls of bacteria or by inhibiting protein synthesis within bacteria so they cannot multiply. Viruses do not have cell walls. (The envelopes and capsids are not cell walls).
There are many problems with the development of antiviral drugs:
• Viruses live within the cells. It is difficult to get high levels of antiviral agent activity without damaging/destroying non-infected host cells.
• Timing. When symptoms of a viral infection appear, the viruses have gone through at least several cycles of replication. Therefore, the best time for antiviral therapy is at the initial stages of infection.
• Difficulty diagnosing viral infections. Viral infections can have vague symptoms, making it hard to decipher what type of infection is present.
• Many viral infections are relatively benign and self-limiting. It is important to weigh the effectiveness verses the toxicity of treatment in order to make the use of such agents acceptable.
One approach for drug antiviral therapy is to block the virus from penetrating the cell membrane. An example of a drug that is thought to have this action is amantadine. Although its exact mechanism is unknown, it is thought to prevent the virus from entering susceptible host cells. It has a specific use for the flu virus (influenza A). It must be given within 48 hours of the onset of symptoms to have any benefit.
These types of drugs are designed to work in the same fashion as your immune system’s antiviral agents to inhibit viral replication. To date, they are not anywhere near as effective as the chemicals naturally occurring in your immune system. Examples include:
Acyclovir—herpes, chicken pox, and shingles
Ganciclovir—herpes, cytomegalovirus
Ribavirin—respiratory syncytial virus
Vidarabine—herpes, chicken pox, and shingles
Another class of pharmaceutical antiviral medications are known as reverse transcriptase inhibitors. These are the drugs used for retroviruses like HIV. As explained on page 23, retro-viruses like HIV are unlike most viruses in that they use the host-cell DNA (genetic material) to manufacture new viruses. Examples of drugs for retroviruses include zidovusine (Retrovir), didnanosine (Videx), zalcitibine (Hivid), lamivudine (Epivir), and stavidine (Zerit).
The following are important components of your body’s immune response to viruses:
Interferons (INFs) are found in the natural response by the immune system. They are messengers within the cell and have antitumor, antiviral, and immunomodulating effects. INFs’ mechanism of action on viruses begins with binding to the cell membrane, in which it then stimulates the production of new cellular protein with an antiviral effect. INFs also inhibit cellular growth, enhance the cytotoxic effect of immune cells, and support antigen expression on the cell membrane.
Immunoglobulins (IMG) are the antibodies used to inactivate “free” viruses.
Researchers are trying to develop more specific agents that will affect viral replication mechanisms and are less toxic than present antiviral pharmaceuticals. One area of focus has been the viral DNA polymerase, which is required in order for the virus to replicate within the host cell. Studies of the effects of combinations of drugs are also being evaluated.4