This chapter focuses on the practical aspects of providing transcranial magnetic stimulation (TMS) in the clinical setting. Prior to establishing a clinical TMS program, practitioners need to understand a host of issues. These include space and facility requirements and equipment used in performing TMS. Also, because TMS is often done in collaboration with nurses or medical assistants, personnel and training issues are covered. How patients are selected, evaluated, and managed for TMS is reviewed, and patient education and the consent process are explained. Consistency for any team of clinicians performing a procedure is important in order to provide safe and effective care for patients and to enhance outcomes. To facilitate this consistency and TMS program development, TMS policy and standard operating procedure topics are discussed. Finally, billing and reimbursement issues are identified and reviewed.
Adequate space is needed for equipment and staff who provide TMS. In the treatment room, enough space should be allowed for the TMS device, a comfortable chair for the patient, and workspace for the treater (typically a desk, work computer, and chair). Storage space for supplies and TMS device–related items, patient charts, and other work items is important. The size of the room is not standard; one manufacturer suggests a room size of 12′ × 15′ for their device, which includes an electrical reclining chair and computer console (Neuronetics I, 2012). A dedicated electrical outlet should be available.
In the room where TMS is performed, sound may be an issue. The TMS coil can produce loud intermittent clicking. The walls of the treatment room provide an adequate sound barrier so as not to disturb other activities in the building. Extra insulation or thicker doors could be considered. Also, due to the intense intermittent sound of the device, a supply of foam hearing protection for both the treater and patient should be available (Rossi, Hallett, Rossini, & Pascual-Leone, 2009).
Medical crises with TMS are rare. The most serious known complication of TMS is seizure during a treatment session (Rossi et al., 2009). This emergency necessitates that the TMS program clinicians be aware of what equipment is required by their local facility administrators and policies. At a minimum, the treater should have ready access to a telephone in the room to call for immediate help and alert emergency medical services (EMS). Other equipment that is not mandatory but is useful for managing a seizure and maintain airway include an ambu bag or wall suction.
A number of TMS devices are produced by various manufacturers. These devices vary in the shape of coil used, but most use focal stimulation of the superficial cortex to either activate or inhibit neuronal function. Other forms of transcranial magnetic stimulation technology are emerging. A newer type of “deep” TMS device may soon be commercially available. It uses a different coil shape and technology to stimulate deeper brain structures more globally (Rosenberg, Shoenfeld, Zangen, Kotler, & Dannon, 2010). Another device made by Neosync, Inc. (Waltham, MA) uses a form of “synchronized” TMS to target the brain’s natural alpha electroencephalographic (EEG) rhythm; it is currently undergoing investigational study for depression (Clinicaltrials.gov, 2013).
Only two devices are US Food and Drug Administration (FDA) approved for major depression. The Neurostar system by Neuronetics, Inc. (Malvern, PA) was the first TMS device to be approved specifically for the treatment of major depression in 2008. More recently, the novel design of the Brainsway, Inc. (Jerusalem, Israel) deep TMS device was approved in 2013 using the FDA 510(k) mechanism of showing substantial equivalence in efficacy and safety to the Neuronetics, Inc. (Malvern, PA) device (Brainsway, 2013). MagVenture, Inc. (Atlanta, GA) and Magstim, Inc. (Whitland, United Kingdom) both produce TMS devices that are FDA approved for use in diagnostic testing, such as peripheral nerve stimulation/evoked potential tests, but do not carry an indication specifically for depression (MagVenture, 2012; Magstim, 2012). Nonetheless, some clinics use these devices for therapeutic purposes.
Factors that influence the choice of a device for use in the clinical setting include cost, equipment included with the system, and ease of use. For example, the Neurostar system comes with an electric reclining chair for comfort, a patient record computer system, the TMS device, and a touch screen console to manipulate settings. However, added costs are required for disposal sensors that ensure good coil contact with the scalp and mitigate surface sensations or pain from the stimulation. As newer TMS technologies become available, clinicians need to learn more about the pros and cons of each device in terms of safety and tolerability, efficacy, and space/facility requirements.
As a medical procedure, it is recommended that a licensed physician prescribe TMS. Properly trained non-physician personnel can administer TMS under the direction of the physician prescriber (Rossi et al., 2009). Commonly, the treater is a registered nurse, but some clinics use qualified medical assistants who are well supervised and trained. During the daily treatment sessions, the physician does not need to be present in the treatment room. However, due to the possibility of tolerability issues, medical emergencies such as a seizure, and even psychiatric emergencies, the physician should be in close proximity to the treatment room, either in the same building or on the same floor.
When initiating a course of TMS, a physician typically completes the motor threshold procedure at the first session. Training should be extensive enough to establish proficiency in mapping the motor cortex, identifying the target muscle movement, and determining the motor threshold level. The physician should be aware of dosing strategies and safety risks associated with various device parameter options. Specifically, clinicians must be aware of the risks with increased intensity, frequency, and shorter decreased intertrain intervals of the TMS stimulus, such as pain, facial muscle contractions, and elevated risk of seizure.
Team members who provide the treatments also need adequate training that includes use of the TMS device and placement of the coil at the target treatment site. Understanding how to optimize patient comfort is important as well. During each session, the patient is monitored directly in the treatment room. The patient must be observed for any abnormal reactions that could indicate dangerous side effects, such as abnormal motor activity, which could place the patient at risk of developing a seizure. TMS team members should be knowledgeable about what questions to ask patients upon arrival that may affect seizure threshold, such as medication changes, decreased sleep, and increased caffeine use. Changes should be communicated to the physician lead. In the event of a seizure, treatment nurses or assistants need to fully understand what the protocol is for managing this complication and how and when to call for emergency services and help.
Currently there are no credentialing programs for physicians and team members who administer TMS. Many attend educational training courses and workshops to enhance their knowledge about TMS. The International Society for ECT and Neurostimulation offers this type of course (Neurostimulation, 2013). Alternatively, well-established device manufacturers provide training programs. Regardless of the training strategy used, TMS program medical directors and administrators need to develop procedures for training team members and establish the frequency of training. Privileging to conduct TMS may also require special approval from local hospital or clinic administrators.
Prior to prescribing TMS, clinicians should complete a thorough assessment of the patient to ensure that a treatable condition likely to respond to TMS is present. Generally, TMS is only FDA approved for depression. The implications of using TMS off label are discussed below in the reimbursement section of this chapter. In addition to the psychiatric assessment of the patient, the pre-TMS consultation should include a review of medical problems, with an emphasis on conditions that may put patients at greater risk with TMS. As with any assessment, physicians should look for medical and neurological comorbidities that may mimic the condition being considered for treatment. Findings from this evaluation may lead the clinician to obtain a more complete physical exam/neurological exam, laboratory tests, or neuroimaging. Because TMS is not associated with cognitive side effects and may actually positively affect cognition (Guse, Falkai, & Wobrock, 2010), pretreatment neuropsychological tests are not necessary. Currently there are no required pre-TMS exams or tests, and performance of any laboratory tests should be driven by a clinical indication or concern.
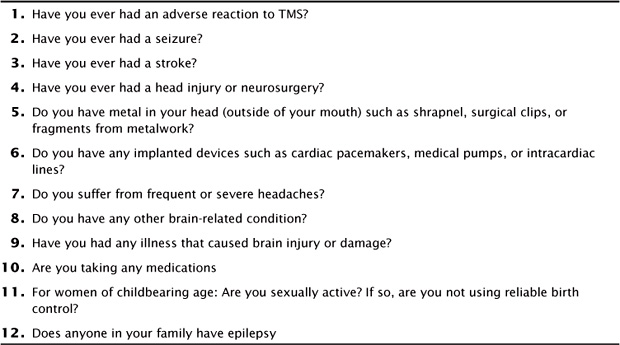
A simple screening tool proposed by Keel et al. (2001) can be used to screen for a number of possible issues prior to the start of TMS (Figure 6.1). If questions are answered with a yes, then further exploration is warranted, but may not necessarily preclude a patient from receiving TMS (Keel et al., 2001). These screening questions focus on neurological conditions, risk of metal or medical implants, and medications that could impact safe delivery of TMS and increase risks.
The acute TMS course often consists of Monday through Friday daily TMS sessions for 4–6 weeks. A plan should be designed for how patients will be monitored during this critical time. An assessment every 1–2 weeks is reasonable. In treating depression, rating scales, whether clinician rated or patient rated, can be helpful in measuring outcome. Regular visits during the TMS course also allow the TMS team to evaluate tolerability issues and changes in medical status or medications. Information gathered from the assessments informs the team whether a repeat motor threshold procedure is necessary or changes in dosing of the TMS may be beneficial.
Patients should be given clear information to ensure they understand the risks and benefits of the TMS procedure. Commonly, general patient education information is presented in a pamphlet or in web page materials to facilitate discussion. If both clinician and patient agree to pursue TMS as a therapeutic modality, a detailed consent form should be reviewed and signed. Figure 6.2 provides a consent form sample that can be adapted to meet your needs.
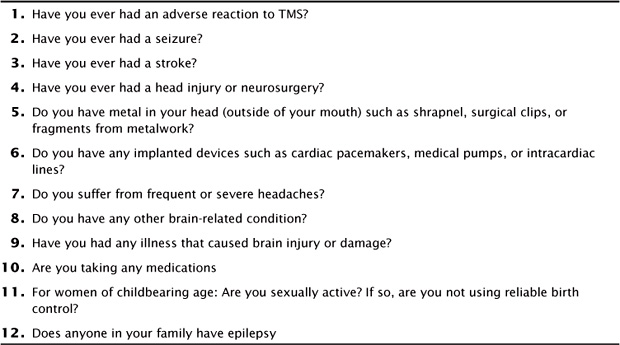
FIGURE 6.1 TMS Adult Safety Screen Questions.
If you answer yes to any questions, further exploration by a TMS physician should be done. Source: Keel, 2000.
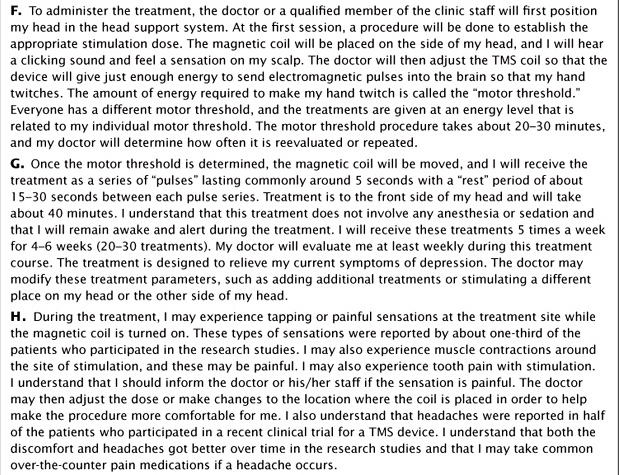
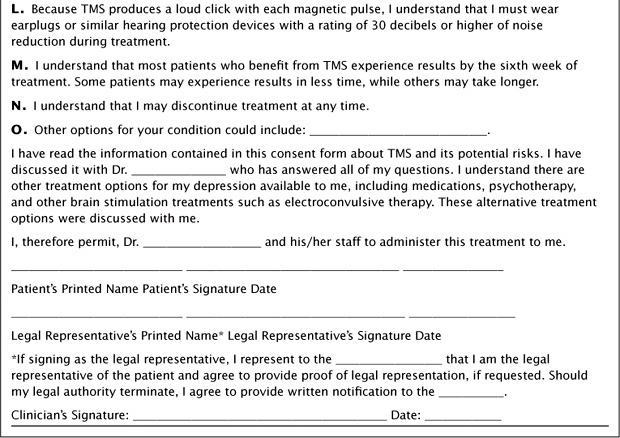
FIGURE 6.2 Consent for Transcranial Magnetic Stimulation
Items covered in the consent form include who the prescribing doctor is and the condition being treated. The consent details how the target location is obtained during the motor threshold procedure, what to expect during this session, and how long this first session will last. Patients are educated that after a motor threshold is established, a brain region is targeted and the treatment coil is placed.
Patients are given information about the duration of each TMS treatment and how they may experience the stimulation, for example, “you will feel a tapping sensation on your scalp for 5 seconds followed by a pause for 25 seconds. This cycle will continue for about 40 minutes.” A review of the number of anticipated TMS sessions for a treatment course is discussed.
Potential side effects such as scalp pain, headache, and muscle/facial twitching are noted. Reviewing the risks of having any magnetic-sensitive metal in or around the head should be highlighted. With seizure risk being very low, yet still the most severe potential adverse event, a special section about this risk should be listed. During the procedure, a loud clicking sound occurs, and patients should be expected and instructed to use ear protection. Finally, patients are educated to report mood changes, including worsening of mood.
A policy may be defined as a high-level overall plan of acceptable procedures and strategies. Standard operating procedures (SOPs) are detailed written instructions that help ensure uniformity in the performance of a plan or procedure. Often, hospitals, administrative departments, or facilities require at least general policies and guidelines in conducting a procedure such as TMS. However, SOPs can be further developed to enhance consistency for all team members in the administration of TMS treatments. These SOPs can operationalize strategies to assist in compliance with regulations, improve safety, and increase better outcomes. Both policies and SOPs can be developed simultaneously and often complement each other.
Definitions and standards are outlined in a policy. The TMS procedure is generally defined and explained, including how the motor threshold is defined and what generally consists of the typical course of treatments. Standards that the TMS program will adhere to are established and may include who conducts the motor threshold procedure and treatments, general patient selection, consent process, and the fact that team members are appropriately trained. Finally, policies may also include a general description of items relevant to patient clinical management and the type of documentation performed.
SOPs can be further designed to provide more details on how TMS is delivered and the roles and responsibilities of each team member. One strategy for keeping both policies and SOPs together for quick referencing is to create a manual or binder for all documents. Copies of the manual can be made readily available to the team in various locations or offices. The manual can be divided into many sections (Figure 6.3). The first section would include the general policy document available for review. A section for TMS documents would include medical chart templates (motor threshold procedure and daily treatment notes), ratings scales, and any other assessment tools implemented by the team. The patient education materials section would include items shared with patients and families, such as TMS pamphlets and a copy of the TMS consent form.
FIGURE 6.3 Sections for a TMS Program Manual
The privileging and training section highlights how all team members are approved to engage in the clinical tasks assigned to them and who is responsible for the privileging approval. The privileging procedure may specify how long privileges are permitted or how often renewal is required. For physicians, proficiency in the motor threshold procedure may need to be demonstrated on regular intervals, and details of retraining for those clinicians who become inactive in their skills can be outlined. Nurses or medical assistants who provide the daily treatments should be trained to be proficient in use of the TMS device, coil placement, and monitoring of tolerability issues with TMS and should demonstrate an understanding of seizure protocols. Training and privileging requirements vary from site to site, and these procedures may need to be developed and reviewed with local administrators.
To provide consistency for the motor threshold procedure and duties of the team members conducting the daily treatments, a TMS procedure section should be developed. In this section, specific procedures of how the motor threshold is obtained are detailed for all physicians. The motor threshold is done at the start of the TMS course to establish a dosing strategy and target site. The threshold appears to not change much over time (Zarkowski, Navarro, Pavlicova, George, & Avery, 2009); however, outlining when a repeat threshold is considered can be detailed. Reasons for redoing a motor threshold include dose tolerability, pain at the treatment site, and changes in medication that potentially could alter threshold. In addition, the coil placement strategy used to target the treatment site and approximate the left dorsolateral prefrontal cortex (DLPFC) should be outlined. In the TMS pivotal trial for depression, this placement was 5 cm anterior from the motor threshold spot (O’Reardon et al., 2007). Data support that this “5-cm rule” may not be optimal and that the actual treatment target site may be better estimated by a coil placement more anterior (Herbsman et al., 2009). Today, current recommendations are for the coil to be placed 5.5–6 cm anterior from the motor threshold location. Other strategies of targeting the left DLPFC are available including use of the F3 EEG location (Beam, Borckardt, Reeves, & George, 2009) or neuro-imaging strategies (Fitzgerald et al., 2009).
For daily treatments, a dosing strategy needs to be selected. Currently, the most common strategy is to start with device settings that reflect similar parameters used in FDA approval studies. Specifically, the starting point tends to be stimulation of the left DLPFC at 120% motor threshold at a frequency of 10 Hz for 3000 pulses per session (O’Reardon et al., 2007). However, over time, other dosing strategies that are based on new research findings will emerge as alternatives. These strategies include increasing the number of pulses to 5000-6000 per session (George & Post, 2011), using right-sided low-frequency (1 Hz) stimulation (Fitzgerald et al., 2009), or combining low-frequency right-sided TMS with high-frequency left-sided TMS (McDonald et al., 2006). More research on these dosing strategies is needed in order to better evaluate outcomes (George, 2010). If a physician uses a dosing strategy that is different from what is approved by the FDA or that targets a different brain region, patients should be apprised of any potential added risks. Details of how any alternate strategy is used should be described in the SOPs and may be justified on clinical judgment of tolerability, patient symptoms, level of improvement, and advancements supported in the research literature that shift standards of care. Daily tasks of nurses or assistants can also be outlined and include how patients are greeted and assessed, treatment room preparation, removal of jewelry or metal from around the head, use of hearing protection, patient positioning for comfort, coil placement and coil repositioning for stimulation discomfort, end of session assessments for side effects, discharge to home instructions, and medical record charting duties. Based on the TMS device used or as other TMS devices (using newer technology) are developed and/or become FDA approved, details of the TMS procedure may change over time. Consequently, treatment protocols should be reviewed routinely.
For clinical management, details of the patient selection and evaluation process, including who conducts the interview, documentation of a TMS responsive condition and rationale for treatment, and recording of assessment tools and scales, can be listed. Although there are no current mandatory laboratory or imaging tests required before TMS, each program should consider whether there are any pre-TMS tests required or if tests are strictly driven by indication or medical condition. A physical exam is also not required prior to TMS, and programs need to decide when or what type of exam is done. If there are any concerns regarding history of a suspected neurological condition, a thorough neurological exam should be considered. Because TMS patients undergo a course of treatment over a number of weeks, details of how patients are followed during this time should be outlined. As noted earlier, one option is to ensure that patients are seen by the prescribing physician at least every 1–2 weeks to evaluate outcome and tolerability so that changes can be made in the treatment plan if needed. Also, nurses or assistants involved in the routine care of TMS patients during the week should have a mechanism to communicate any concerns to the physician in charge, and this expectation should be explicitly clear to team members to ensure safety of TMS patients. Finally, this section should contain procedures on how to manage side effects such as pain. Most importantly is a description of the program’s seizure protocol and how this rare but potential adverse event is managed locally. This protocol may include basic physical management to protect the patient’s airway and breathing, who to call for medical assistance, instructions to contact EMS, and what to document (abnormal preseizure activity, detail seizure/motor activity, duration of seizure, any injuries sustained, and clinical status after the seizure). This seizure protocol can also be posted in the treatment room for quick reference.
A TMS manufacturer section includes information about the maker of the TMS device. This section contains contact information and procedures for ordering supplies and who to call for maintenance and trouble-shooting. Finally, the important TMS literature section is used as a resource for all team members to stay abreast of new advancements in the clinical practice of TMS.
The spread of insurance coverage for TMS has been a slow process since the FDA approved the first TMS device for depression in 2008, and this coverage has been sporadic over the last five years in the United States. Costs of providing TMS encompass the facility overhead, staffing, physician time, and TMS device costs. The fee charged for a TMS session is in the range of $300–$400 (Reti, 2013). Without insurance coverage, many clinicians charge a fee for service, and in many areas, access to TMS is limited. Those covered by Medicare also have few options to receive TMS. Since there is no national coverage determination for TMS by Medicare, TMS can be covered at the discretion of individual Medicare contractors based on a local coverage determination (LCD; Services CfMM, 2013). There is a growing number of Medicare contractors in certain regions of the United States that are developing policies for TMS as a covered benefit. In early 2013, three Medicare contractors had TMS policies that covered Alabama, Delaware, the District of Columbia, Georgia, Maine, Maryland, Massachusetts, New Hampshire, New Jersey, Pennsylvania, Rhode Island, Tennessee, and Vermont (CMS, L32055 (2013); CMS, L32228 (2012); CMS, L32834 (2012)). In addition, a number of other commercial healthcare providers across the United States have written TMS policies.
The language for the FDA-approved TMS device and the indication of depression focuses on a narrow window of only one failed antidepressant in the current episode indicating early or mild treatment resistance (Neuronetics I, 2010). Interestingly, the criteria in many policies vary and may actually require more severe treatment resistance before allowing TMS. As an example, the LCD Medicare policies mentioned above list lack of significant response to four medications from two antidepressant classes (CMS, L32055 (2013); CMS, L32228 (2012); CMS, L32834 (2012)) as a criterion. For clinicians, it is important to fully understand any TMS coverage provided by patients’ insurance policies and to review this before prescribing TMS. If no coverage benefit is available, physicians and TMS team members need to discuss fees and possibly even payment plan options for those who wish to proceed but pay out of pocket. Even if a policy covers TMS, it is advisable to also obtain preauthorization approval from the insurer, as this may further help clarify the actual TMS benefit for patients and clinicians.
To facilitate billing of TMS, the American Medical Association (AMA) has assigned Current Procedural Terminology (CPT) category I codes for TMS. Three codes are available (see Table 6.1; American Medical Association, 2013). CPT code 90867 is used for the initial TMS session when the motor threshold procedure is done, the treatment target is identified, and dosing strategy is determined. In addition, this code is used for the entire first treatment session. CPT code 90868 is used for subsequent daily treatment sessions. If a repeated motor threshold is done for clinical reasons or per local protocol, CPT code 90869 is used to indicate this procedure and for the entire treatment session that day. Both motor threshold codes (90867 and 90869) should not be used in conjunction with each other or with the daily treatment code (90868). Since 1992, the Centers for Medicare & Medicaid Services (CMS; formerly Health Care Financing Administration) has used the resource-based relative value scale model to quantify and reimburse for physicians services (Johnson & Newton, 2002). The model allows for the calculation of relative value units (RVUs) for every CPT code. As of 2013, RVUs have not been assigned for TMS, but clinicians should monitor when the RVUs become available.
Beyond depression, emerging clinical research has suggested that TMS might have a role in a number of psychiatric and medical conditions such as anxiety disorders, bipolar disorder, dementia, schizophrenia, pain, and tinnitus. However, more research is needed to establish clear benefit for many of these conditions (Praharaj, Ram, & Arora, 2009; Vercammen et al., 2009; Wassermann & Zimmermann, 2012). Any use of TMS for these clinical situations would be deemed off label. TMS practitioners who venture into targeting different brain regions or treating different disorders other than those approved may face difficulties similar to those faced by prescribers of expensive medication for an off-label use. Preauthorization may be needed or the treatment may not be covered at all.
Two strategies will help with changing policies. If TMS is prescribed even if the treatment is not covered, use of the appropriate CPT codes when billing patients contributes to the database on the use of TMS. This type of information is used by CMS and insurers and can potentially impact policy development. Second, advocating for the safe and effective use of TMS locally is a strategy to consider. Examples of advocacy that can be done include educating the public about TMS and providing letters of support for the use of TMS to local insurers.
TABLE 6.1 CPT Codes for TMS
CPT Code |
Details |
90867 |
Therapeutic repetitive transcranial magnetic stimulation (TMS) treatment; initial, including cortical mapping, motor threshold determination, delivery and management of treatment |
90868 |
Therapeutic repetitive transcranial magnetic stimulation (TMS) treatment: subsequent delivery and management, per session |
90869 |
Therapeutic repetitive transcranial magnetic stimulation (TMS) treatment; subsequent motor threshold re-determination with delivery and management (Do not report 90869 in conjunction with 90867 or 90868) |
CPT is copyrighted by the American Medical Association.
When developing a TMS program, it is not sufficient to simply learn about the biological mechanisms of TMS and the basic procedure. Much planning is involved to successfully provide the best care and service for patients. Design of an excellent program entails creating thorough administrative protocols, policies, and operating procedures that become the framework for all that TMS team members do. Finally, the use of TMS technology in clinical situations appears to be a rapidly evolving field, with newer TMS strategies and devices on the horizon. TMS program leaders must be constantly vigilant of the latest advances.
American Medical Association. (2013). CPT: current procedural terminology, professional edition. Chicago, IL: American Medical Association.
Beam, W., Borckardt, J., Reeves, S., & George, M. (2009). An efficient and accurate new method for locating the F3 position for prefrontal TMS applications. Brain Stimulation, 2(1), 50–54.
Brainsway. (2013). Press release: Brainsway Receives FDA Approval. Retrieved from http://www.brainsway.com/Brainsway/Templates/showpage.asp?DBID=1&LNGID=1&TMID=178&FID=565&PID=0&IID=3442. Clinicaltrials.gov. (2013). Synchronized Transcranial Magnetic Stimulation (sTMS) in Major Depressive Disorder - Full Text View - ClinicalTrials.gov. Retrieved from http://clinicaltrials.gov/show/NCT01370733 [Accessed: 28 Sep 2013].
CMS L32055 (2013). Transcranial Magnetic Stimulation (TMS) for the Treatment of Depression. Retrieved from http://www.novitas-solutions.com/webcenter/content/conn/UCM_Repository/uuid/dDocName:00007677 CMS L32834 (2012). Local Coverage Determination (LCD): Medicine: Repetitive Transcranial Magnetic Stimulation (rTMS) for Resistant Depression (L32834). Retrieved from http://www.cms.gov/medicare–coverage–database/details/lcd–details.aspx?LCDId=32834&ContrId=213&ver=4&ContrVer=1&articleId=51982&CntrctrSelected=213*1&Cntrctr=213&name=Cahaba+Government+Benefit+Administrators%24*%24sup*%24*%c2%ae%24*%24%2fsup*%24*%2c+LLC+(10102%2c+MAC+–+Part+B)&IsPopup=y&.
CMS L32228 (2012). Local Coverage Determination (LCD): Repetitive Transcranial Magnetic Stimulation (rTMS) (L32228). Retrieved from http://www.cms.gov/medicare–coverage–database/details/lcd–details.aspx?LCDId=32228&ContrId=210&ver=3&ContrVer=1&CntrctrSelected=210*1&Cntrctr=210&name=NHIC%2c+Corp.+(14402%2c+MAC+–+Part+B)&DocType=Active&DocStatus=Draft&s=47&bc=AggAAAIAAAAAAA%3d%3d&.
Fitzgerald, P., Hoy, K., Mcqueen, S., Maller, J., Herring, S., Segrave, R., … Daskalakis, Z. (2009). A randomized trial of rTMS targeted with MRI based neuro-navigation in treatment-resistant depression. Neuropsychopharmacology, 34(5), 1255–1262.
George, M. (2010). Transcranial magnetic stimulation for the treatment of depression. Expert Review Neurotherapeutics, 10(11), 1761–1772.
George, M., & Post, R. (2011). Daily left prefrontal repetitive transcranial magnetic stimulation for acute treatment of medication-resistant depression. American Journal of Psychiatry, 168(4), 356–364.
Guse, B., Falkai, P., & Wobrock, T. (2010). Cognitive effects of high-frequency repetitive transcranial magnetic stimulation: a systematic review. Journal Neural Transmission, 117(1), 105–122.
Herbsman, T., Avery, D., Ramsey, D., Holtzheimer, P., Wadjik, C., Hardaway, … Nahas, Z. (2009). More lateral and anterior prefrontal coil location is associated with better repetitive transcranial magnetic stimulation anti-depressant response. Biological Psychiatry, 66(5), 509–515.
Johnson, S., & Newton, W. (2002). Resource-based relative value units: a primer for academic family physicians. Fam Med, 34(3), 172–176.
Keel, J. C., Smith, M. J., & Wassermann, E. M. (2001). A safety screening questionnaire for transcranial magnetic stimulation. Clinical Neurophysiology, 112(4), 720.
Magstim. (2012). Retrieved from http://www.magstim.com/products–and–applications.
MagVenture. (2012). Retrieved from http://www.magventure.com/en–gb/products.aspx.
McDonald, W., Easley, K., Byrd, E., Holtzheimer, P., Tuohy, S., Woodard, J., … Epstein, C. (2006). Combination rapid transcranial magnetic stimulation in treatment refractory depression. Neuropsychiatric Disease Treatment, 2(1), 85–94.
Neuronetics I. (2010). NeuroStar TMS Therapy System User Manual. Retrieved from http://www.neurostar.com/wp–content/uploads/2010/11/PrescribingInformation.pdf.
Neuronetics I. (2012). NeuroStar TMS Therapy System Version 1.7 Technical Data Sheet. Retrieved from http://neurostar.com/wp–content/uploads/2012/04/80–50101–002–NeuroStar–TMS–System–Version–1.7–Technical–Data–Sheet.pdf.
Neurostimulation, IISfEa. (2013). Retrieved from https://www.isen–ect.org/node/936.
O’Reardon, J. P., Solvason, H. B., Janicak, P. G., Sampson, S., Isenberg, K. E., Nahas, Z., … Sackeim, H. A. (2007). Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biological Psychiatry, 62, 1208–1216.
Praharaj, S., Ram, D., & Arora, M. (2009). Efficacy of high frequency (rapid) suprathreshold repetitive transcranial magnetic stimulation of right prefrontal cortex in bipolar mania: a randomized sham controlled study. Journal Affective Disorders, 117(3), 146–150.
Reti, I. M. (2013). A rational insurance coverage policy for repetitive transcranial magnetic stimulation for major depression. Journal ECT, 29(2), e27–28.
Rosenberg, O., Shoenfeld, N., Zangen, A., Kotler, M., & Dannon, P. (2010). Deep TMS in a resistant major depressive disorder: a brief report. Depression Anxiety, 27(5), 465–469.
Rossi, S., Hallett, M., Rossini, P. & Pascual-Leone, A. (2009). Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clinical Neurophysiology, 120(12), 2008–2039.
Services CfMM. Medicare Determination Process. (2013). Retrieved from http://www.cms.gov/Medicare/Coverage/DeterminationProcess/index.html?redirect=/DeterminationProcess/.
Vercammen, A., Knegtering, H., Bruggeman, R., Westenbroek, H., Jenner, J., Slooff, C., … Aleman, A. (2009). Effects of bilateral repetitive transcranial magnetic stimulation on treatment resistant auditory–verbal hallucinations in schizophrenia: a randomized controlled trial. Schizophrenia Research, 114(1), 172–179.
Wassermann, E., & Zimmermann, T. (2012). Transcranial magnetic brain stimulation: therapeutic promises and scientific gaps. Pharmacology Therapeutics, 133(1), 98–107.
Zarkowski, P., Navarro, R., Pavlicova, M., George, M., & Avery, D. (2009). The effect of daily prefrontal repetitive transcranial magnetic stimulation over several weeks on resting motor threshold. Brain Stimulation, 2(3), 163–167.