Most authors of textbooks are very proficient in their field, as should be expected. However, this depth of knowledge creates a language and concept barrier between them and beginners who, by definition, do not understand the material fully. This “language difficulty” creates a feeling of helplessness and insecurity that overwhelms many beginners at first. As mentioned in the Foreword, the Beginner’s Perspective boxes have been created as a way for me, recently a beginner myself, to reach out to those just starting and share some of my trials and tribulations. I will focus on key pearls or take-home messages that I found important to develop a deeper understanding of the topic. I hope that by sharing this journey together, we can make the learning process less difficult.
I would sum up this chapter with the expression, “A picture is worth a thousand words.” The strength of this chapter is in its graphics. They help clarify and simplify various difficult concepts. As an example, consider Figure 1-5. I was originally taught the traditional way that focuses on two circulatory systems (pulmonary and somatic) that function in sync with each other to circulate blood. My original impression was of two systems connected at the heart, but the route the blood had to take in this system was difficult to conceptualize. Only after looking at Figure 1-5 and seeing how the blood is actually routed did I realize there is one true nonstop route with “tubing” crossing over itself at the level of the heart, like a figure eight.
By altering our thinking just a bit, we can see how backups in one section affect the rest of the system. Perhaps unknowingly, we have worked with related concepts all our lives. Take for example a simple hose. We’ve all seen how a kink in the hose causes increased pressure in the section of the hose before the kink and, ultimately, decreased flow out of the hose. We’ve seen how partial obstructions affect the fluid dynamics of the system, how different nozzles affect it, how increases or decreases in water pressure affect it, how the width of the hose affects it, and so forth. Once we understand the system as a continuing circuit, then break it down into the pulmonary and somatic systems, it makes sense.
The same can be said for Figure 1-9 and the concept of afterload, a critical concept discussed in later chapters. It is one thing to talk about how cardiac contraction causes blood to circulate throughout the body; it is another thing to understand how it does so. Figure 1-9 shows us that the left ventricle contracts and the amount of blood held in that chamber is pushed out into the aorta. That volume of blood dilates the aorta by expanding its elastic muscular wall. The pent-up tension in the elastic muscular wall, in turn, increases the internal pressure within the aorta as the walls try to return to a normal relaxed state. Since the valves of the heart are one-way valves and blood cannot return to the ventricles, the blood has only one way to go: forward. It is that steady pressure on the blood, caused by the release of the elastic muscular tension in the walls of the aorta, that slowly pushes the blood forward throughout the rest of the body and creates circulation. The role of the heart is just to start the process by ejecting that bolus of blood into the aorta; most of the process of circulation takes place after the heart. The passive elastic property built into the arterial walls actually propels the blood to circulate through the brain, the heart itself (through the coronary arteries), and the rest of the body.
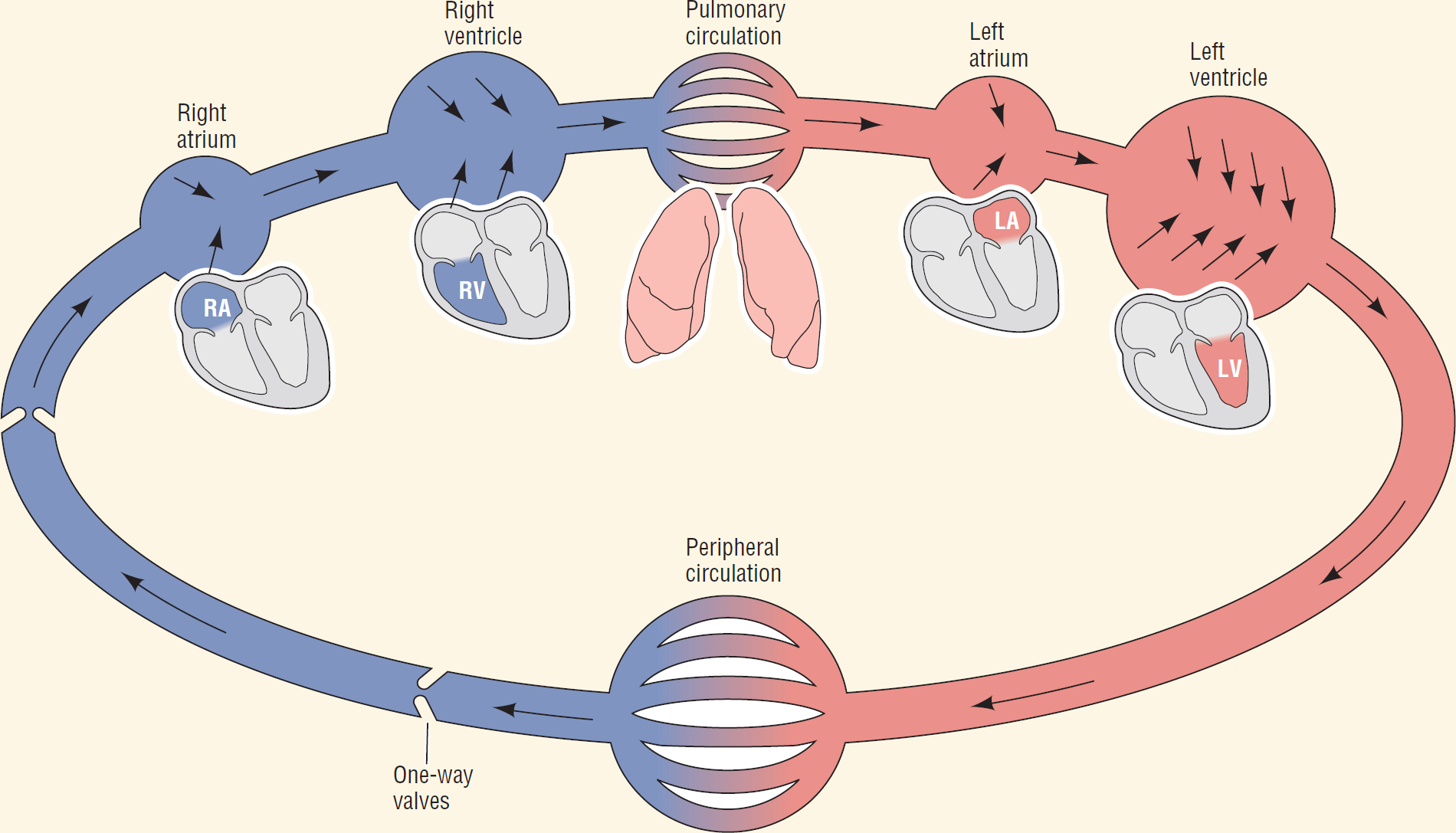
Inset of Figure 1-5.
© Jones & Bartlett Learning.
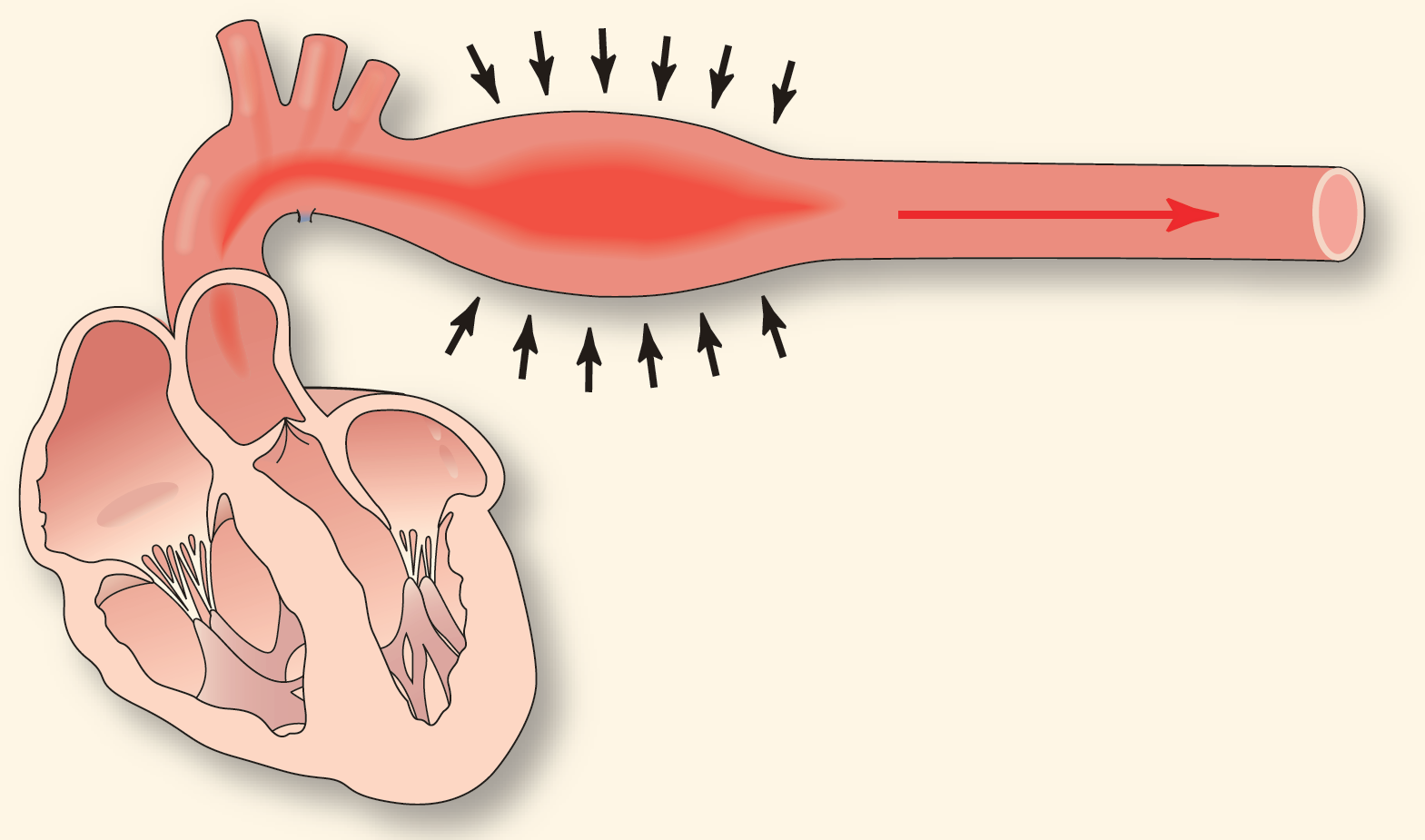
Inset of Figure 1-9.
© Jones & Bartlett Learning.
Knowing this information is really cool. What else can we derive from it? Well, now we understand where systolic and diastolic pressures come from. Systolic blood pressure is the amount of pressure within the artery immediately after receiving the blood bolus from the heart; it starts the process of moving the blood forward. Diastolic blood pressure is the pressure within the artery when the muscular walls are in a relaxed state—in other words, when there is a marked decrease in the forward flow of the blood.
There are some additional concepts that I used to think were not important for me—that is, until I understood how circulation actually works. Take the advanced concept of afterload, for example. Afterload is defined as the pressure against which the heart must pump to eject blood. If the pressure in the aorta is high, the heart has to work harder to pump the same amount of blood into it. Now that we understand circulation, we can see how this scenario can be a big problem. Less blood could be ejected from the heart, leading to less blood being circulated; increased tension on the heart could lead to ischemia or dilation of the ventricles, and less blood reaching the organs of the body, such as the brain and the heart itself.
You may be saying, “I’m just a [state your clinical title here]. I don’t need to know about afterload. How does this information affect me?” My question to you is, do you ever give your patient a drug? Drugs alter the tension in the muscular walls. For example, this process is how antihypertensives work, and, to a great extent, how nitroglycerin works. Furthermore, it is a factor in the lack of blood volume in the circulation due to trauma. And those are only a few implications.
The bottom line is, the field of clinical medicine works on mechanics. Arrhythmia recognition is no exception to this rule. Learning should be simple, exciting, and interesting, not to mention fun. Our goal is to provide you with that opportunity; your goal should be to have an open mind.
In closing, when you begin to learn a new subject, you should look for simple descriptions of how things work. There is always time for complexity later. By understanding the simple principles, you are about 95% of the way there. It is the other 5% that require a lifetime to master.
—Daniel J. Garcia