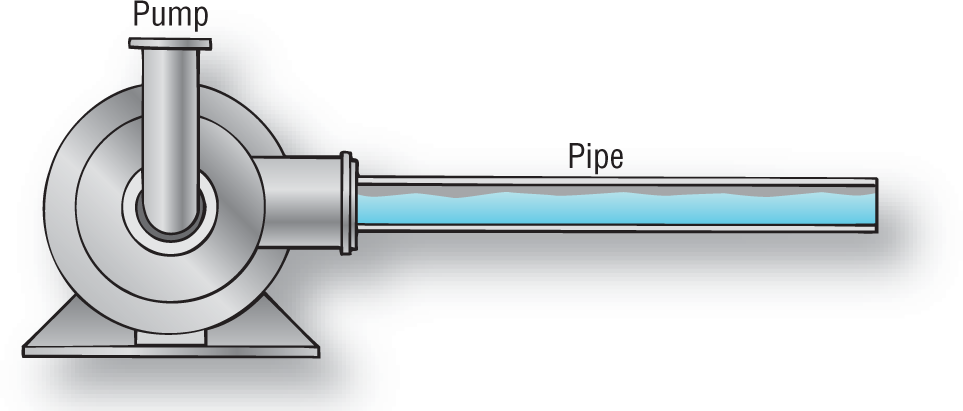
Figure 1-6 Rigid tube system.
© Jones & Bartlett Learning.
Blood pressure is critical to life. We need blood pressure to act as the driving force to move blood through the circulatory system in order to deliver oxygen and nutrients to every cell. How does the body maintain blood pressure? It is maintained by both passive and active means. In this section, we will first go over the passive system and then we will discuss the active system.
Suppose you put an extra 70 mL of fluid into a fluid-filled, solid-walled pipe such as a PVC or copper pipe (Figure 1-6). What changes would the extra fluid create in the tube? The pressure in the tube would build up dramatically with every cc of fluid you put into it (Figure 1-7). The pressure would force fluid to run out the open end of the pipe in order to relieve the pressure. That system works well when you have a short amount of pipe and a strong pump. The longer the pipe, the stronger the pump needed.
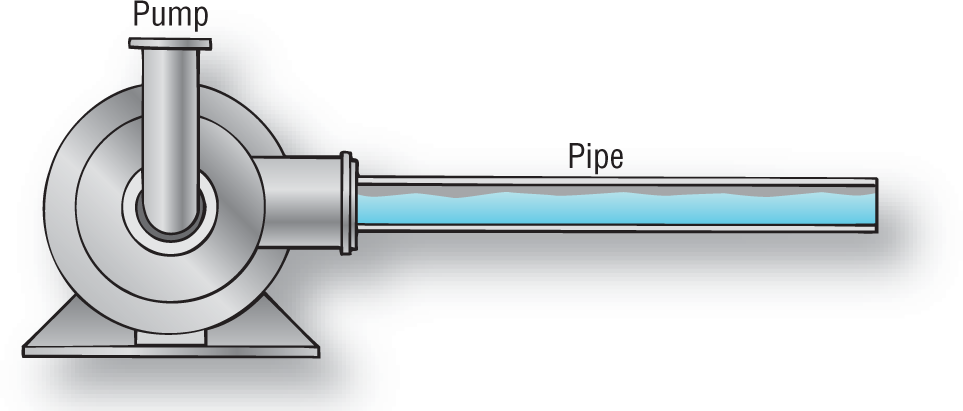
Figure 1-6 Rigid tube system.
© Jones & Bartlett Learning.

Figure 1-7 Pressure inside the pipe.
© Jones & Bartlett Learning.
In one pound of fat tissue in the human body there is one-quarter mile of tubing (Figure 1-8). We can assume that this is true for other types of tissue as well.

Figure 1-8 Every pound of fat has about one-quarter mile of vascular tubing in it to allow perfusion of every cell.
© Jones & Bartlett Learning.
DescriptionHow many miles of tubing are in your entire vascular system? A lot! The pump needed to push blood through such a tubing system, if it were rigid, would need to be very strong indeed. What do you suppose such strong forces would do to your red cells, white cells, and platelets? They would destroy them. Therefore, this type of system would not work in our bodies.
Instead of rigid tubing, the human body is composed of elastic tubing. Elastic tubing can bend and allow us to move without any difficulty. It is compressible, allowing external muscle movement to help pump the blood by compressing or milking the tube, causing the fluid to be pushed along. The main advantage to this type of tubing, however, is its elastic properties. Its elasticity allows the blood vessel to simply distend in order to accommodate for the extra fluid whenever the heart pumps (Figure 1-9).

Figure 1-9 Imagine that the bolus of blood that shoots out of the heart is the red area in this figure. Notice how the aorta is distended outward by the additional bolus. As the bolus begins to mix with the rest of the blood, the built-up pressure on the arterial walls is pushing the walls inward. This happens because the elastic walls want to go back to their resting state of relaxation. This pressure causes the blood to move forward smoothly and continuously. The process is repeated over and over with each cardiac contraction.
© Jones & Bartlett Learning.
What would happen to the pressure inside the tube now? It would build up inside the tube, but the distention would distribute the pressure a bit more smoothly. What happens to an elastic band when you stretch it? It wants to go back to its original shape. This built-up energy places constant, smooth pressure on the blood, causing it to flow forward in a smooth fashion, avoiding high shearing pressures and turbulence (Figure 1-9). The distended arterial walls are, in essence, acting like an additional pump helping to push the blood forward through the circulatory system.
The slow, constant pressure of a distended elastic arterial system wanting to return to normal is the passive way in which the circulatory system functions. Now let’s go over the active system that causes the arterial distention in the first place.
The blood pressure is maintained actively by the amount of blood that the heart pumps out into the vascular system every minute—in other words, the cardiac output. Cardiac output is, in turn, composed of two variables: the stroke volume and the heart rate. The stroke volume is the amount of blood that the heart ejects during any one contraction. This amount is usually around 70 cc of blood per contraction. Heart rate, as you can imagine, refers to the number of times the heart beats in one minute.
Cardiac output is mathematically calculated by taking the amount of blood that the heart can eject in one contraction and then multiplying this by the number of contractions per minute. In other words:
Cardiac Output = Stroke Volume × Heart Rate
In order to maintain a good hemodynamic balance, the cardiac output has to be within the normal range. Notice however, that you can maintain an adequate cardiac output by altering the two variables. For example, suppose that the stroke volume was 40 cc/min (instead of the normal 70 cc/min). Can you figure out a way that the cardiac output for the heart can be maintained within the normal range? One way would be by increasing the heart rate. That is the reason why, when someone has lost a significant amount of blood (resulting in decreased stroke volume because there is less blood to pump), a tachycardia develops as a compensatory mechanism. The body tries to overcome the deficiency in blood and stroke volume by increasing heart rate.
Now let’s take a closer look at the concept of stroke volume. At the end of systole, the ventricles have just emptied their contents into the arterial system (Figure 1-10). How does the heart fill up the ventricles again? If you remember from basic physiology, the largest amount of ventricular filling occurs during early diastole, when the atrioventricular (AV) valves open up and a rush of blood floods the ventricular chamber (Figure 1-11). This is known as the rapid filling phase of diastole.

Figure 1-10 This Figure shows the heart in late systole. The atria are full but the ventricles are empty.
© Jones & Bartlett Learning.

Figure 1-11 In early diastole, the AV valves open, allowing a large amount of blood to rush into the ventricles. This is the rapid filling phase of diastole.
© Jones & Bartlett Learning.
After the rapid ventricular filling phase of diastole, the ventricles are full with blood. If the ventricles were to contract at this point, the stroke volume of the heart would be at the lower end of normal for most people. Why? Because the ventricles are filled, but not overfilled. It is a well-known fact in muscle physiology that a muscle contracts much more efficiently if it is stretched just a bit (see the Additional Information box). So, how can we overfill the ventricles to allow a bit of muscle stretching? Passive inflow of blood just wouldn’t do it. The answer is made clear when we think about atrial contraction.
If you look at Figure 1-12, you will notice that the atria are completely full of blood during the middle of diastole. They have been filled by the venous blood that is constantly flowing back to the heart. At the end of diastole, when the ventricles are almost full, the atria contract and push the extra blood into the ventricles in order to overfill them (Figure 1-13). The overfilling provided by the atrial contraction stretches the ventricular muscle, allowing for maximal contractility and maximal stroke volume. Better stroke volume means better control over the cardiac output.

Figure 1-12 In mid-diastole, the ventricles are full. Notice that the ventricular walls, however, are not distended in any way.
© Jones & Bartlett Learning.

Figure 1-13 The atrial contraction allows an extra amount of blood to enter the ventricles, causing them to stretch and overfill. The slight stretch in the ventricular muscle caused by the atrial kick will maximize stroke volume and cardiac output.
© Jones & Bartlett Learning.
You may be asking why we are spending so much time on basic physiology when this is a book on arrhythmias. The reason is that the heart rate is one of the most important variables in the maintenance of cardiac output. As we saw earlier, the other main variable is the stroke volume. In many cases, arrhythmias will affect either one or both of these variables profoundly. In order to understand the clinical implications of arrhythmias, you need to understand the concept of cardiac filling and cardiac output very clearly. We will constantly refer back to this section throughout the book.
Additional Information
Muscle Tension
When a muscle is at its normal length (Figure 1-14), the amount of tension that it can produce is a set amount. In other words, a muscle can only produce just so much tension. On the other hand, if the muscle were stretched, the amount of tension that it could produce would be increased (Figure 1-15).

Figure 1-14 Unstretched muscle has less tension than stretched muscle.
© Jones & Bartlett Learning.

Figure 1-15 Stretched muscle has better functionality.
© Jones & Bartlett Learning.
The heart muscle is no exception to this rule. If the heart were allowed to fill only by passive means such as the inflow of blood, the heart muscle would not be stretched. The amount of force that the heart could use to contract would be less than if the muscle were stretched somewhat. (Textbooks on physiology refer to this finding as the Frank-Starling mechanism or law.) The atrial kick allows the heart to “overfill” a bit and stretch the muscle, maximizing myocardial contraction.
Now let’s take a closer look at how heart rate affects stroke volume. What do you think happens to the stroke volume of the heart at very fast heart rates? Remember from our previous discussion on the rapid filling phase that most of the blood volume entering the ventricle occurs during very early diastole right after the AV valves open up (Figure 1-16). At very fast ventricular rates, the ventricles do not have time to fill adequately because the rapid filling phase is shortened (Figure 1-17). The net result is that the ventricles are not filled to capacity or overfilled at the end of diastole. Now when they contract, the amount of blood that is expelled is less than optimal. Less than optimal ejection means a decrease in cardiac output. In other words, the cardiac output will diminish because the stroke volume will be greatly decreased. Decreased cardiac output could very easily cause or lead to hemodynamic instability. That is how and why a tachycardia or rapid heart rate can kill.

Figure 1-16 Normal rapid filling phase and the overfilling caused by atrial contraction during normal heart rates.
© Jones & Bartlett Learning.
Description
Figure 1-17 Impaired rapid filling phase is shown on Examples A to C. The small amount of blood added by the atrial kick is not enough to overcome the decreased blood volume in the ventricles. The net result is that the stroke volume, and hence the cardiac output, will be greatly decreased.
© Jones & Bartlett Learning.
Description