Figure 6-8 An escape complex.
© Jones & Bartlett Learning.
An escape complex is almost the opposite of a premature complex. Instead of occurring early in the cadence of the rhythm, it occurs late in the cadence (Figure 6-8). In order to understand how an escape complex occurs, remember that all cardiac tissue has the ability to function as a potential pacemaker for the heart. The sinus node has the fastest pacing cycle; the ventricular muscle has the slowest (Figure 6-9). When the primary pacemaker fails for whatever reason, the next one in succession will take over the main role.
Figure 6-8 An escape complex.
© Jones & Bartlett Learning.
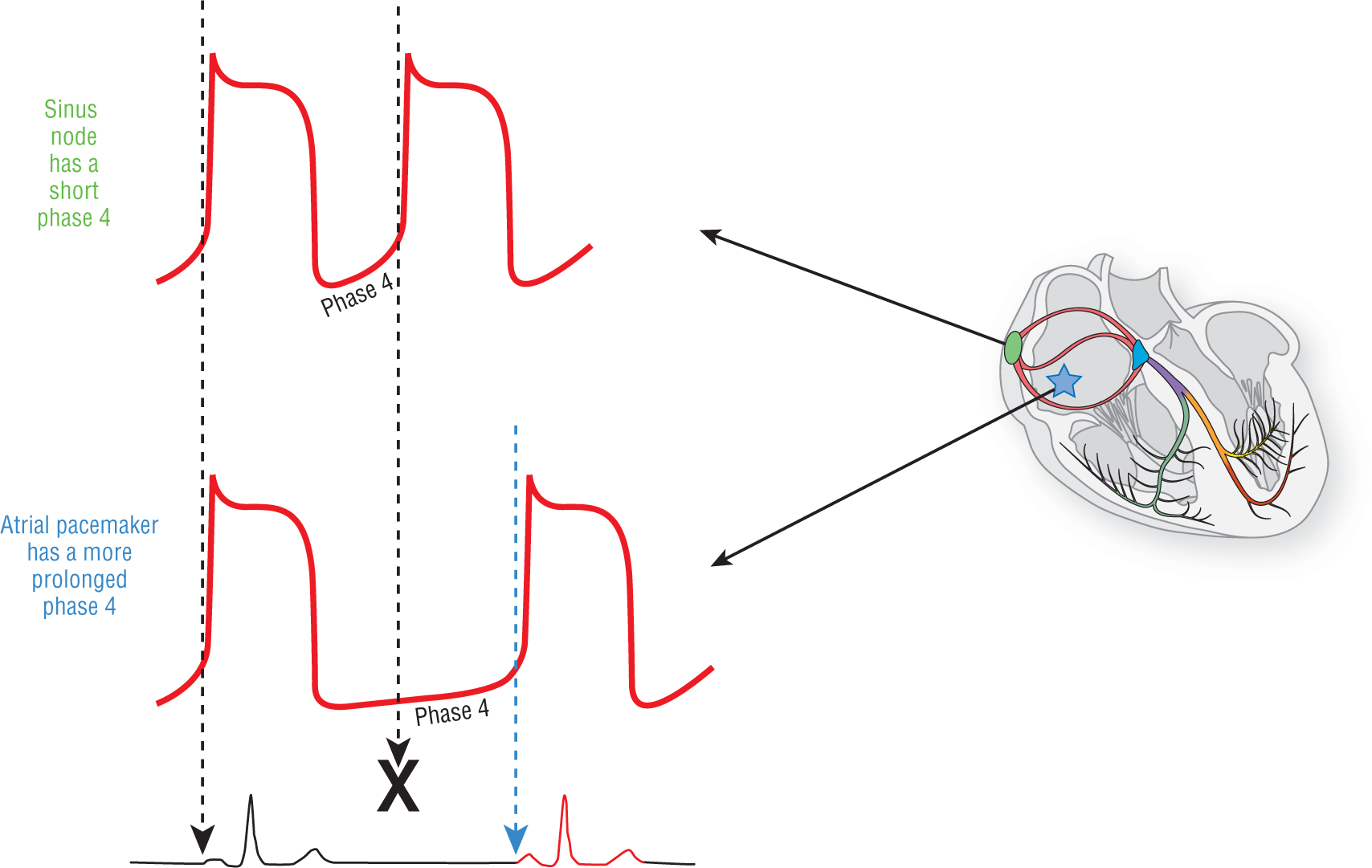
Figure 6-9 When the atrial pacemaker fails to pace at the expected time, the next pacemaker will fire according to its schedule. This creates an escape complex (see blue arrow).
© Jones & Bartlett Learning.
DescriptionAdditional Information
An Arrhythmia Versus an Event
At this point, we need to review some terminology. A cardiac rhythm refers to the cadence or sequence of how the cardiac complexes occur. Cardiac rhythms can be normal or abnormal and do not necessarily refer to a pathologic process. Normally, the sinus node acts as the pacemaker and the impulse proceeds down the normal electrical conduction system to innervate both the atria and the ventricles sequentially.
An arrhythmia refers to a cardiac rhythm that is pathologic in nature, and is one that is created or transmitted differently than the normal process. It can begin somewhere outside the sinus node. It can travel through different pathways other than the normal electrical conduction system. It can occur at rates outside of the normal range. It can be hemodynamically stable or it can cause hemodynamic instability. It can be fast or slow, wide or narrow.
We also should understand the difference between a rhythm and a rhythm with an overlying cardiac event that momentarily alters the cadence of the underlying rhythm. Suppose you had a strip with a clearly visible, regular cadence on it. Suddenly another pacemaker in the heart became irritable and fired early. The cadence of the rhythm is altered by the event (Figure 6-7), but this is not a new arrhythmia. It is a normal rhythm with a premature complex. Always remember, an event is not a rhythm.

Figure 6-7
© Jones & Bartlett Learning.
Why the distinction? Usually novice clinicians will focus on the event and not the rhythm itself. It is usually the underlying arrhythmia that will cause the hemodynamic compromise, not the single event. Let’s use an analogy to think about this another way. In emergency medicine, we are involved in the care of trauma patients. For a trauma patient, one of the most impressive wounds, visually, is a scalp laceration. They normally cause small rivers of blood to drip down the face and can be quite dramatic. However, how many people actually die from a laceration to the scalp? Very, very few. On the other hand, a blunt liver laceration does not have an impressive visual presentation but is often a killer. The clinician needs to look past the dramatic presentation of the scalp laceration and concentrate on the blunt injury that can kill the patient. That same mentality is how you need to approach an arrhythmia; concentrate on the rhythm and just be aware of the single event.
The reason this fail-safe pacemaking system exists is so that if one pacemaker fails, there are other pacemakers to keep the heart going and the person does not die. In an escape complex, the pacemaker that is setting the main rhythm fails and the next one takes over. This can occur either for one complex, or for however long it is needed.
An escape rhythm occurs when the primary pacemaker fails for a prolonged time. Once again, the next pacemaker in succession will usually take over pacemaking function for the heart.