
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
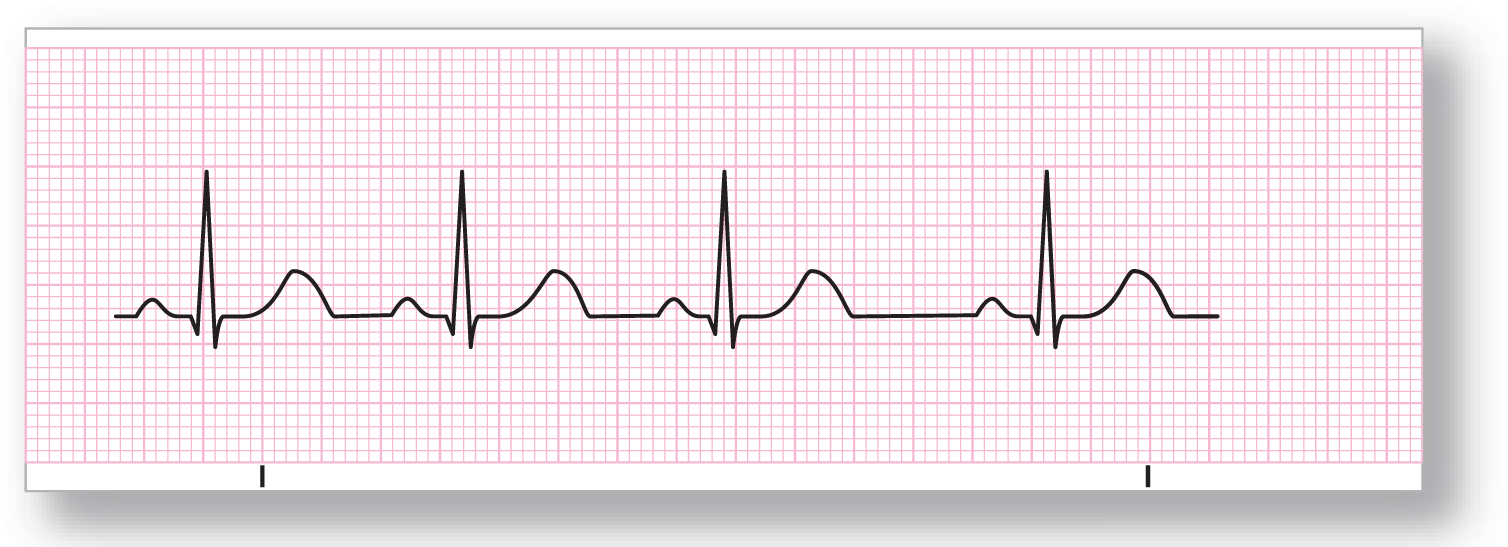
Normal Sinus Rhythm (NSR)

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: 60–100 BPM |
PR interval: Normal |
|
Regularity: Regular |
QRS width: Normal |
|
P wave: Present |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: None |
Putting it all together:
ECG 7-1 represents the normal state with the SA node functioning as the lead pacer. The intervals should all be consistent and within normal ranges. If the intervals are not within the normal rate but still sinus in origin, it is referred to as sinus rhythm.
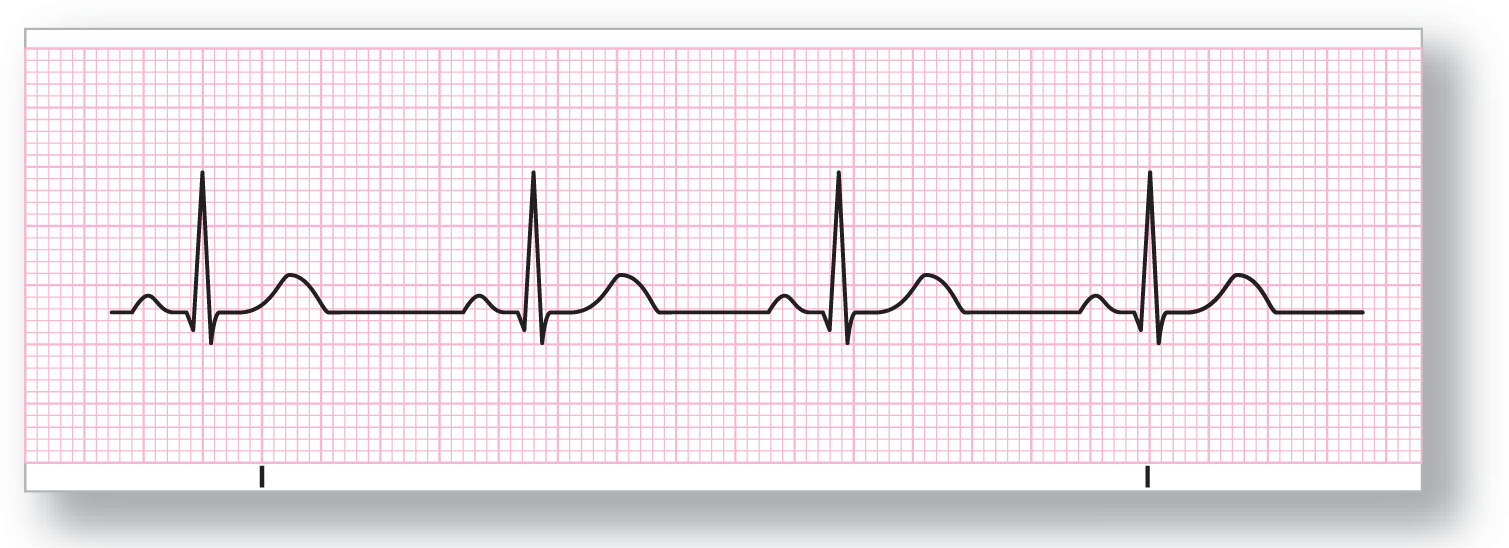
Sinus Arrhythmia
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: 60–100 BPM |
PR interval: Normal |
|
Regularity: Varies with respiration |
QRS width: Normal |
|
P wave: Normal |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: None |
Putting it all together:
ECG 7-2 represents the normal respiratory variation, becoming slower during exhalation and faster upon inhalation. This occurs because inhalation increases venous return by lowering intrathoracic pressure. Note that the PR intervals are the same; only the TP intervals (the interval from the end of the T wave of one complex to the beginning of the P wave of the next complex) vary with the respirations.
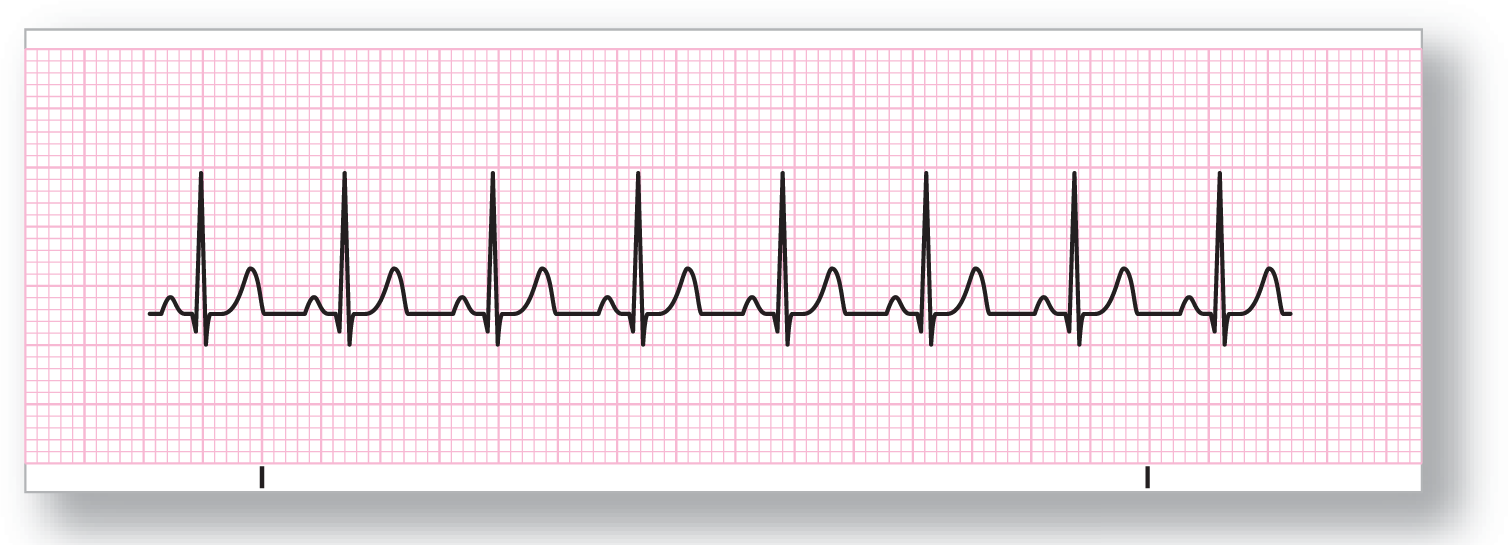
Sinus Bradycardia
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Less than 60 BPM |
PR interval: Normal to slightly prolonged |
|
Regularity: Regular |
QRS width: Normal to slightly prolonged |
|
P wave: Present |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: None |
Putting it all together:
In ECG 7-3, the sinus beats are slower than 60 BPM. The origin may be in the SA node or in an atrial pacemaker. This rhythm can be caused by vagal stimulation leading to nodal slowing, or by medicines such as beta blockers, and is normally found in some well-conditioned athletes. The QRS complex, and the PR and QTc intervals, may slightly widen as the rhythm slows below 60 BPM. However, they will not widen past the upper threshold of the normal range for that interval. For example, the PR interval may widen, but it should not widen over the upper range of 0.20 seconds.
Sinus Tachycardia
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: ≥ 100 BPM |
PR interval: Normal to slightly shortened |
|
Regularity: Regular |
QRS width: Normal to slightly shortened |
|
P wave: Present |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: None |
Putting it all together:
In ECG 7-4, the rhythm can be caused by medications or by conditions that require increased cardiac output, such as exercise, hypoxemia, hypovolemia, hemorrhage, and acidosis.
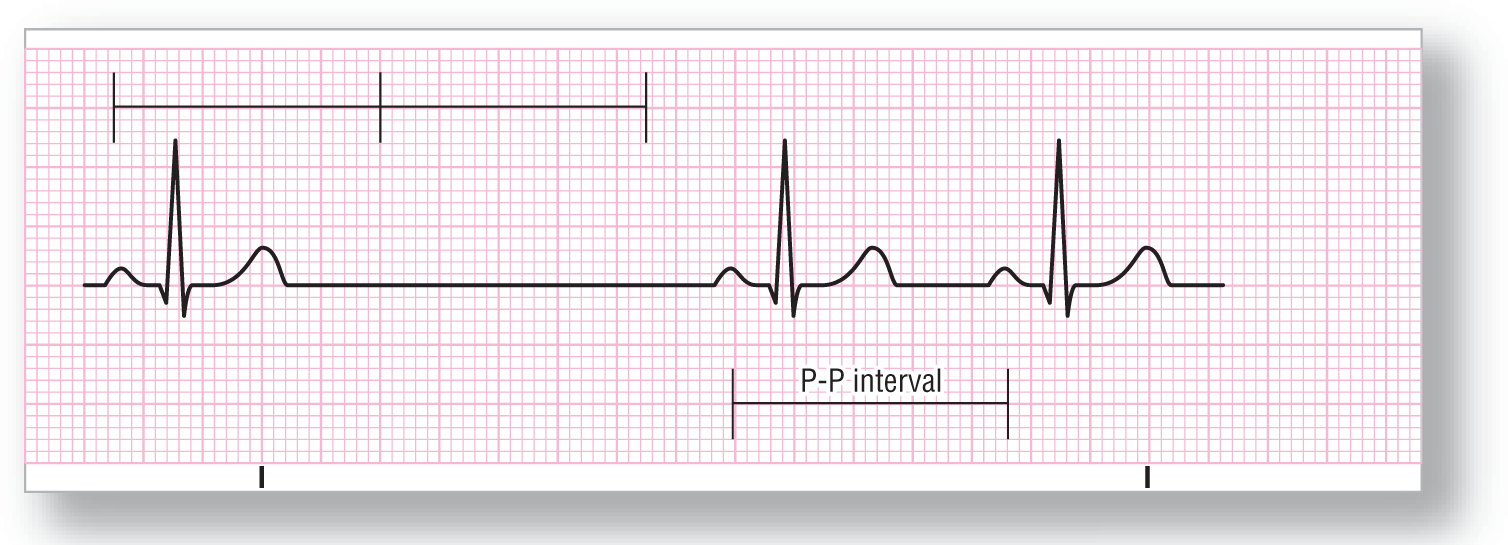
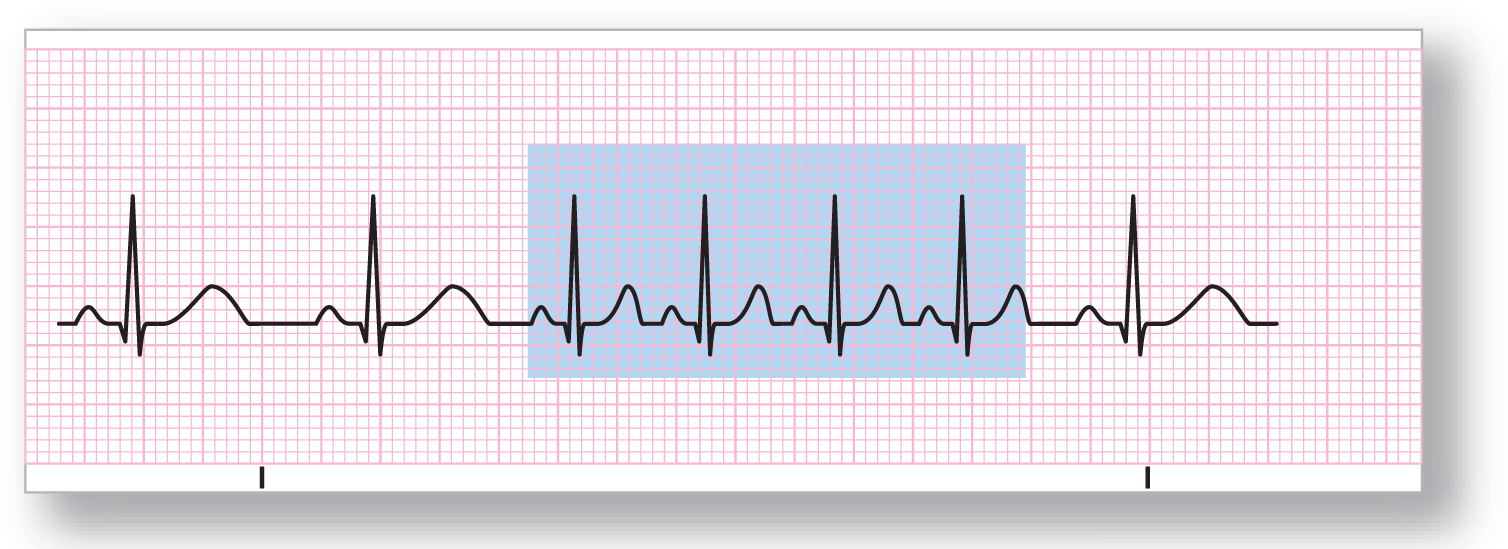
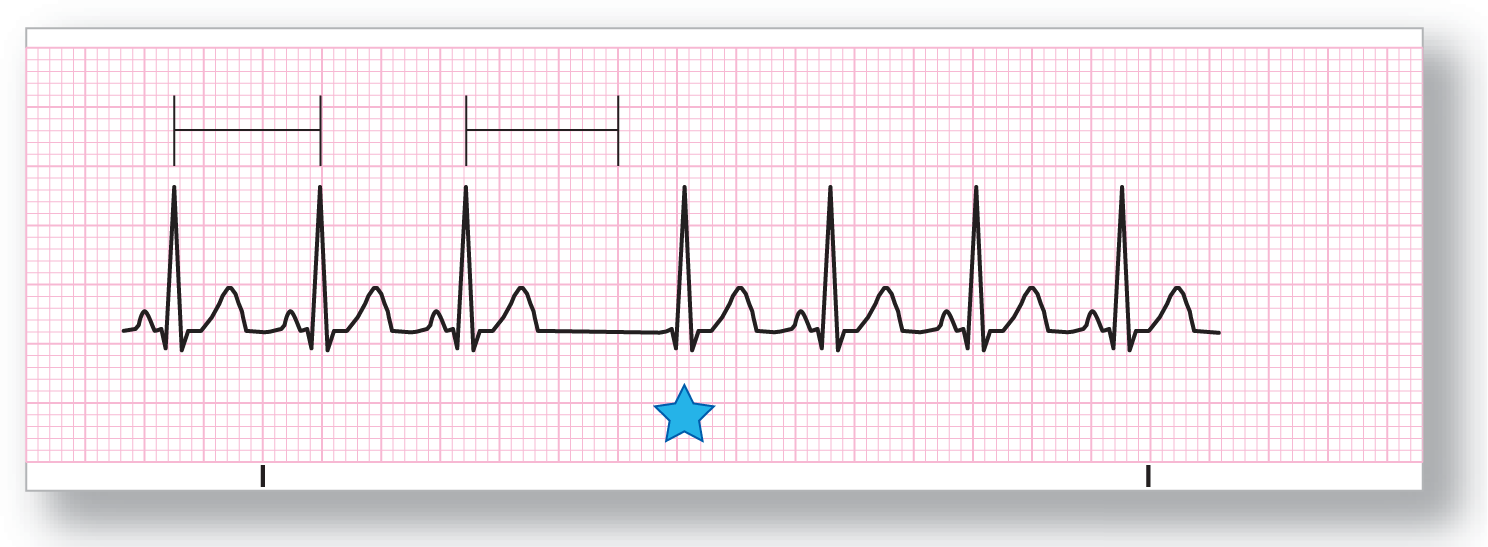
Sinus Pause/Arrest
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Varies |
PR interval: Normal |
|
Regularity: Irregular |
QRS width: Normal |
|
P wave: Present except in areas of pause/arrest |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: Yes |
Putting it all together:
A sinus pause is a variable time period during which there is no sinus pacemaker working. The time interval is not a multiple of the normal P-P interval. (A dropped complex that is a multiple of the P-P interval is known as an SA block, discussed next.) A sinus arrest is a longer pause, though there is no clear-cut criterion for how long a pause has to last before it is called an arrest.
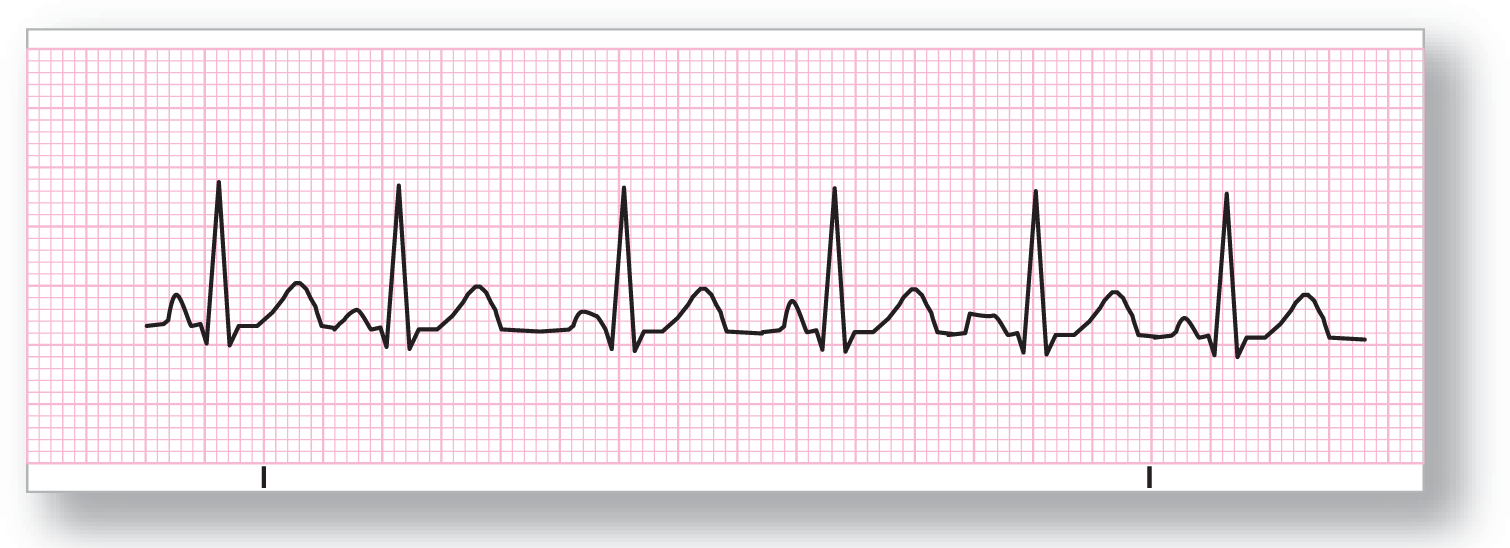
Sinoatrial Block

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Varies |
PR interval: Normal |
|
Regularity: Irregular |
QRS width: Normal |
|
P wave: Present except in areas of dropped beats |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: Yes |
Putting it all together:
In ECG 7-6, the block occurs in some multiple of the P-P interval. After the dropped beat, the cycles continue on time and as scheduled. The pathology involved is a nonconducted beat from the normal pacemaker.
Premature Atrial Contraction (PAC)

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Depends on the underlying rate |
PR interval: Varies in the PAC, otherwise normal |
|
Regularity: Irregular |
QRS width: Normal |
|
P wave: Present; in the PAC, may be a different shape |
Grouping: Sometimes |
|
P:QRS ratio: 1:1 |
Dropped beats: No |
Putting it all together:
A premature atrial contraction (PAC) occurs when some other pacemaker cell in the atria fires at a rate faster than that of the SA node. The result is a complex that comes sooner than expected. Notice that the premature beat “resets” the SA node, and the pause after the PAC is not compensated; the underlying rhythm is disturbed and does not proceed at the same pace. This noncompensatory pause is less than twice the underlying normal P-P interval.
Focal Atrial Tachycardia
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: 100–200 BPM |
PR interval: Ectopic focus has a different interval |
|
Regularity: Regular |
QRS width: Normal, but can be aberrant at times |
|
P wave: Morphology of ectopic focus is different |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: None |
Putting it all together:
Focal atrial tachycardia occurs when an ectopic atrial focus fires more quickly than the underlying sinus rate. The P waves and PR intervals are different because the rhythm is caused by an ectopic atrial pacemaker (a pacemaker outside of the normal SA node). The episodes are usually not sustained for an extended period. Because of the accelerated rate, some ST- and T-wave abnormalities may be present transiently.
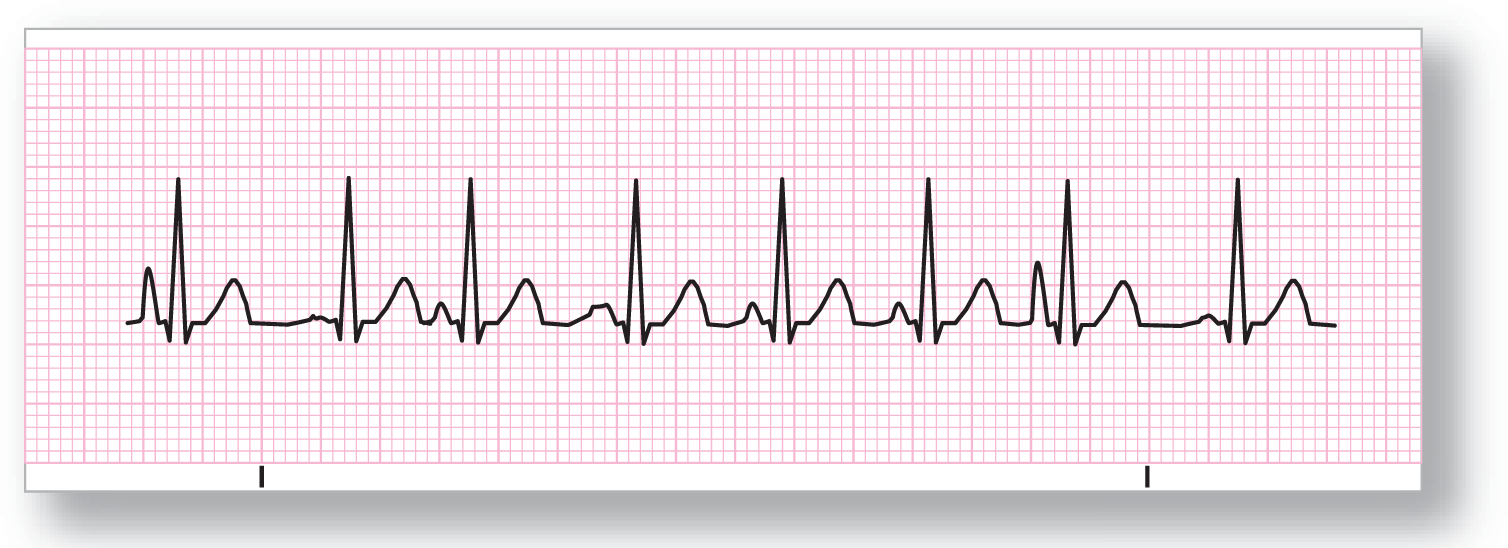
Wandering Atrial Pacemaker (WAP)
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: < 100 BPM |
PR interval: Variable depending on the focus |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P wave: At least three different morphologies |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: None |
Putting it all together:
Wandering atrial pacemaker (WAP) is an irregularly irregular rhythm created by multiple atrial pacemakers each firing at its own pace. The result is an ECG with at least three different P-wave morphologies with their own intrinsic PR intervals. Think of each pacer firing from a different distance, and with a different P-wave axis. The longer the distance, the longer the PR interval. The varying P-wave axis causes differences in the morphology of the P waves.
Multifocal Atrial Tachycardia (MAT)
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: ≥ 100 BPM |
PR interval: Variable |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P wave: At least three different morphologies |
Grouping: None |
|
P:QRS ratio: 1:1 |
Dropped beats: None |
Putting it all together:
Multifocal atrial tachycardia (MAT) is merely a tachycardic WAP. Both MAT and WAP are commonly found in patients with severe lung disease. The tachycardia can cause cardiovascular instability at times, so it should be treated. Treatment is difficult and should be aimed at correcting the underlying problem.
Atrial Flutter
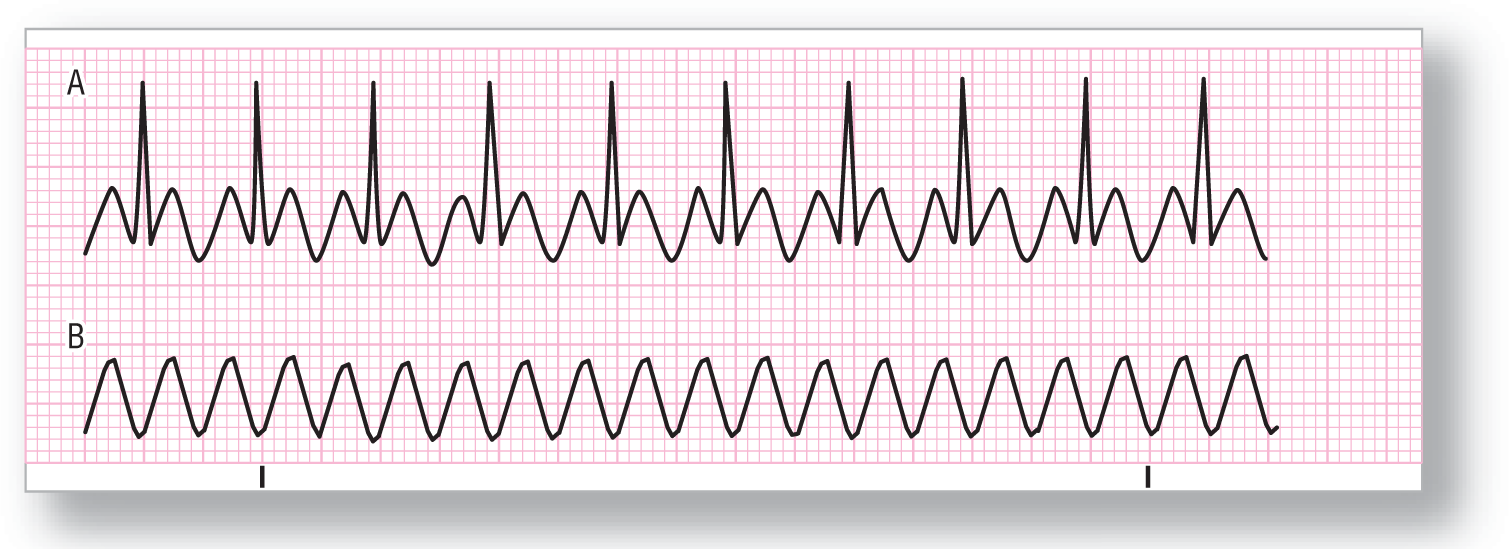
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial rate commonly 250–350 BPM |
PR interval: Variable |
|
Regularity: Usually regular, but may be variable |
QRS width: Normal |
|
P wave: Saw-toothed appearance, “F waves” |
Grouping: None |
|
P:QRS ratio: Variable, most commonly 2:1 |
Dropped beats: None |
Putting it all together:
The F waves appear in a saw-toothed pattern such as those in this ECG. (QRSs have been removed from strip B to reveal F-wave shape.) The QRS rate is usually regular and the complexes appear at some multiple of the P-P interval. The usual QRS response is 2:1 (this means that there are two F waves for each QRS complex). The ventricular response can also occur slower at rates of 3:1, 4:1, or higher. Sometimes the ventricular response will be irregular.
Rarely, you will have a truly variable ventricular response that does not fall on any multiple of the F-F interval. We call this an atrial flutter with a variable ventricular response.
In closing, keep in mind that the saw-toothed appearance may not be obvious in all 12 leads. Whenever you see a ventricular rate of 150 BPM, look for the buried F waves of an atrial flutter with 2:1 block!
Atrial Fibrillation

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Variable, ventricular response can be fast or slow |
PR interval: None |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P wave: None; chaotic atrial activity |
Grouping: None |
|
P:QRS ratio: None |
Dropped beats: None |
Putting it all together:
Atrial fibrillation is the chaotic firing of numerous atrial pacemaker cells in a totally haphazard fashion. The result is that there are no discernible P waves, and the QRS complexes are innervated haphazardly in an irregularly irregular pattern. The ventricular rate is guided by occasional activation from one of the pacemaking sources. Because the ventricles are not paced by any one site, the P-P intervals are completely random.
Premature Junctional Contraction (PJC)

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Depends on underlying rhythm |
PR interval: None, short, or retrograde; if present, does not represent atrial stimulation of the ventricles |
|
Regularity: Irregular |
QRS width: Normal |
|
P wave: Variable (none, antegrade, or retrograde) |
Grouping: Usually none, but can occur |
|
P:QRS ratio: None; or 1:1 if antegrade or retrograde |
Dropped beats: None |
Putting it all together:
A premature junctional contraction (PJC) is a beat that originates prematurely in the AV node. Because it travels down the normal electrical conduction system of the ventricles, the QRS complex is identical to the underlying QRSs. PJCs usually appear sporadically, but can occur in a regular, grouped pattern such as supraventricular bigeminy or trigeminy. There may be an antegrade or retrograde P wave associated with the complex. An antegrade P wave is one that appears before the QRS complex. The PR interval is very short in these cases, and the P-wave axis will be abnormal (inverted in leads II, III, and aVF; more on these types of P waves in Chapter 21, Introduction to Junctional Rhythms). A retrograde P is one that appears after the QRS complex.
Junctional Escape Beat
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Depends on underlying rhythm |
PR interval: None, short, or retrograde; if present, does not represent atrial stimulation of the ventricles |
|
Regularity: Irregular |
QRS width: Normal |
|
P wave: Variable (none, antegrade, or retrograde) |
Grouping: None |
|
P:QRS ratio: None; or 1:1 if antegrade or retrograde |
Dropped beats: Yes |
Putting it all together:
An escape beat occurs when the normal pacemaker fails to fire and the next available pacemaker in the conduction system fires in its place, as discussed in Chapter 1, Anatomy and Basic Physiology. The AV nodal pacer senses that the normal pacer did not fire. So, when its turn comes up and it reaches threshold potential, it fires. The distance of the escape beat from the preceding complex is always longer than the normal P-P interval.
Junctional Rhythm

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: 40–60 BPM |
PR interval: None, short, or retrograde; if present, does not represent atrial stimulation of the ventricles |
|
Regularity: Regular |
QRS width: Normal |
|
P wave: Variable (none, antegrade, retrograde) |
Grouping: None |
|
P:QRS ratio: None, or 1:1 if antegrade or retrograde |
Dropped beats: None |
Putting it all together:
A junctional rhythm arises as an escape rhythm when the normal pacemaking function of the atria and SA node is absent. It can also occur in the case of AV dissociation or third-degree AV block (more on this later).
Accelerated Junctional Rhythm

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: 60–100 BPM |
PR interval: None, short, or retrograde; if present, does not represent atrial stimulation of the ventricles |
|
Regularity: Regular |
QRS width: Normal |
|
P wave: Variable (none, antegrade, retrograde) |
Grouping: None |
|
P:QRS ratio: None, or 1:1 if antegrade or retrograde |
Dropped beats: None |
Putting it all together:
In ECG 7-16, the rhythm originates in a junctional pacemaker that, because it is firing faster than the normal pacemaker, takes over the pacing function. It is faster than expected for a normal junctional rhythm, pacing in the range of 60–100 BPM. If it exceeds 100 BPM, it is known as junctional tachycardia. As with other junctional pacers, the P waves can be absent or conducted in an antegrade or retrograde fashion.