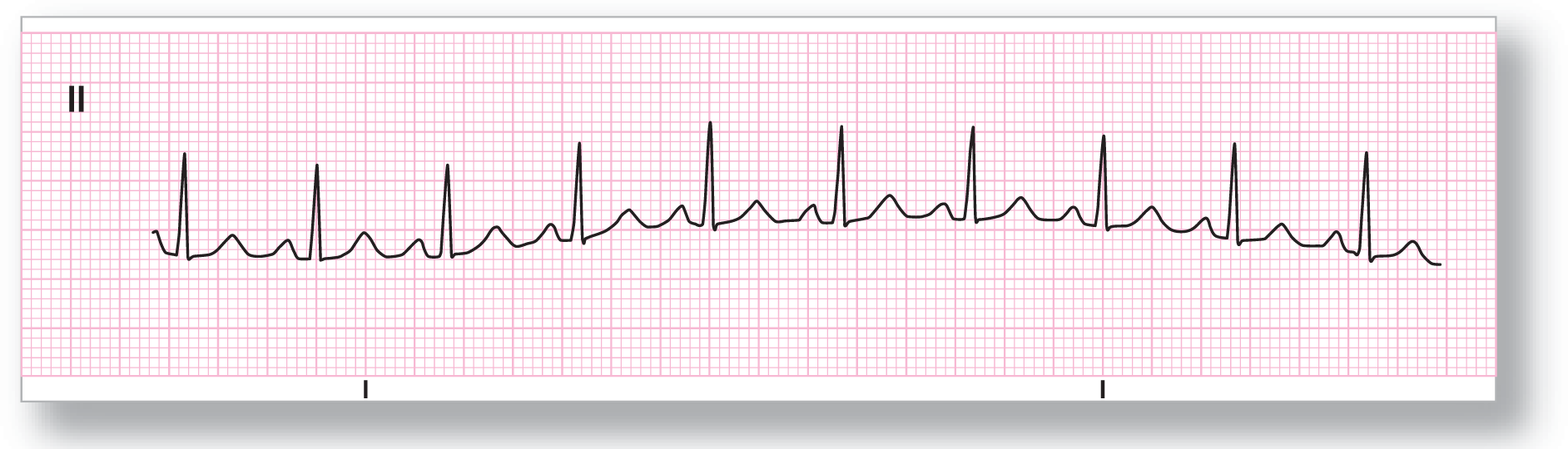
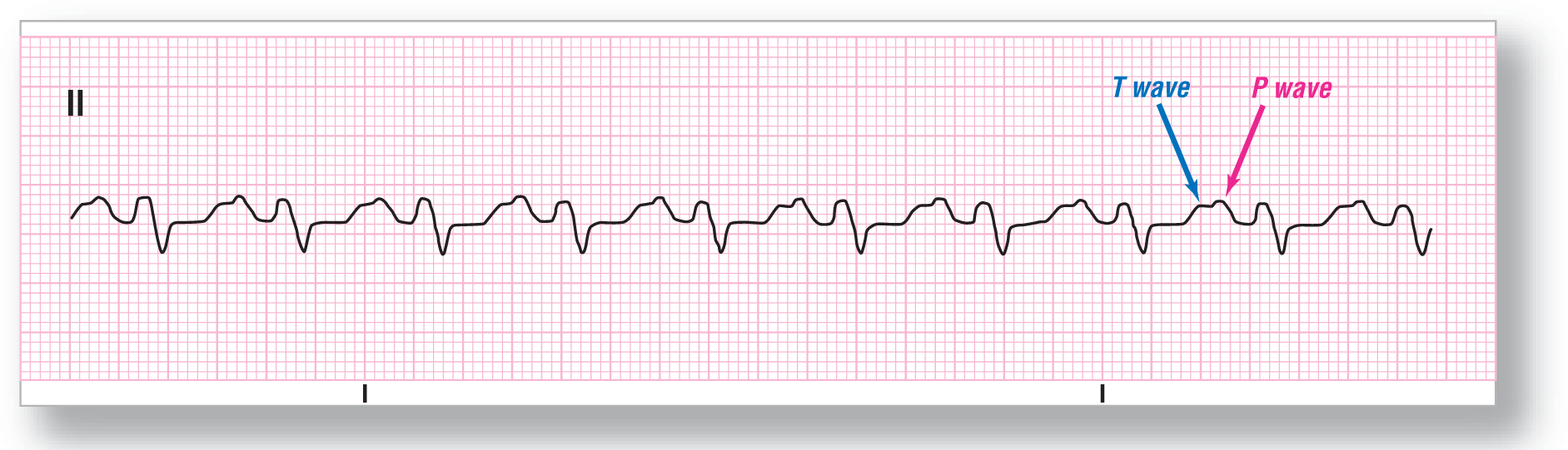
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 110 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present |
Rhythm: Sinus tachycardia |
Discussion:
ECG 10-1 has a wandering baseline, but the criteria are all present for the diagnosis of sinus tachycardia. Be careful not to confuse a wandering baseline for electrical alternans. Electrical alternans refers to a variation in the amplitude of the QRS complex. In a wandering baseline, the QRS complexes are all the same height.
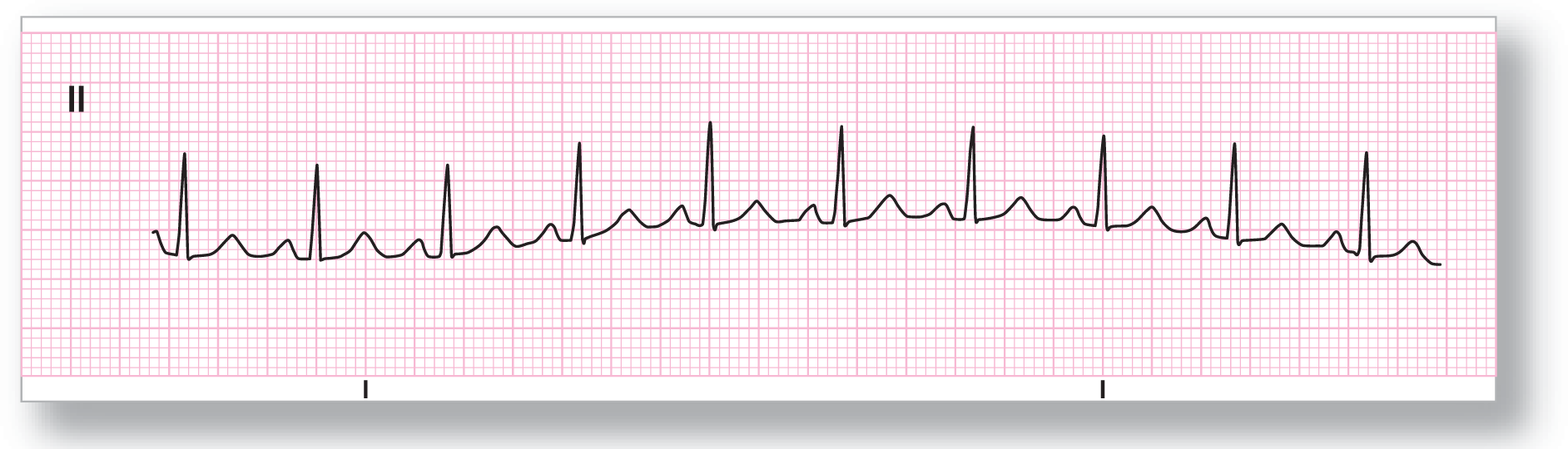
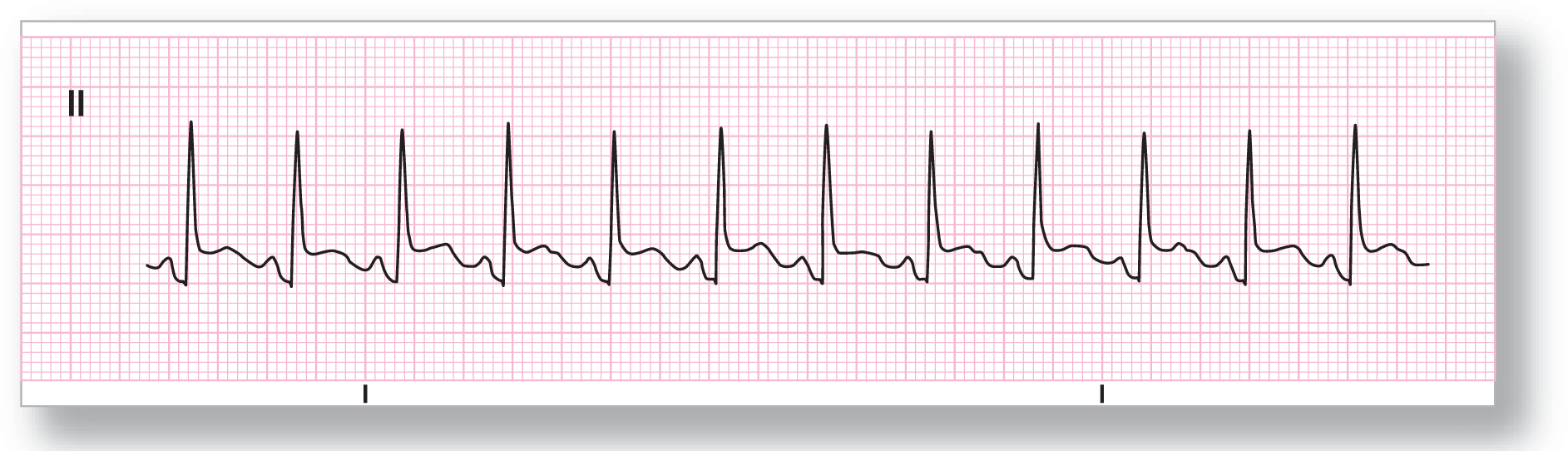
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 130 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present |
Rhythm: Sinus tachycardia |
Discussion:
ECG 10-2 is a classic example of sinus tachycardia. Note the slight depression of the ST segment. This could be due to the atrial repolarization wave or Tp wave, a slight amount of endocardial ischemia due to the tachycardia, or to some other cause. Whenever you see any significant abnormality on a rhythm strip, you should obtain an ECG to further evaluate the possible causes. In this case, the worst-case scenario could be that the ST depressions are due to reciprocal changes found in the inferior leads during a lateral AMI.

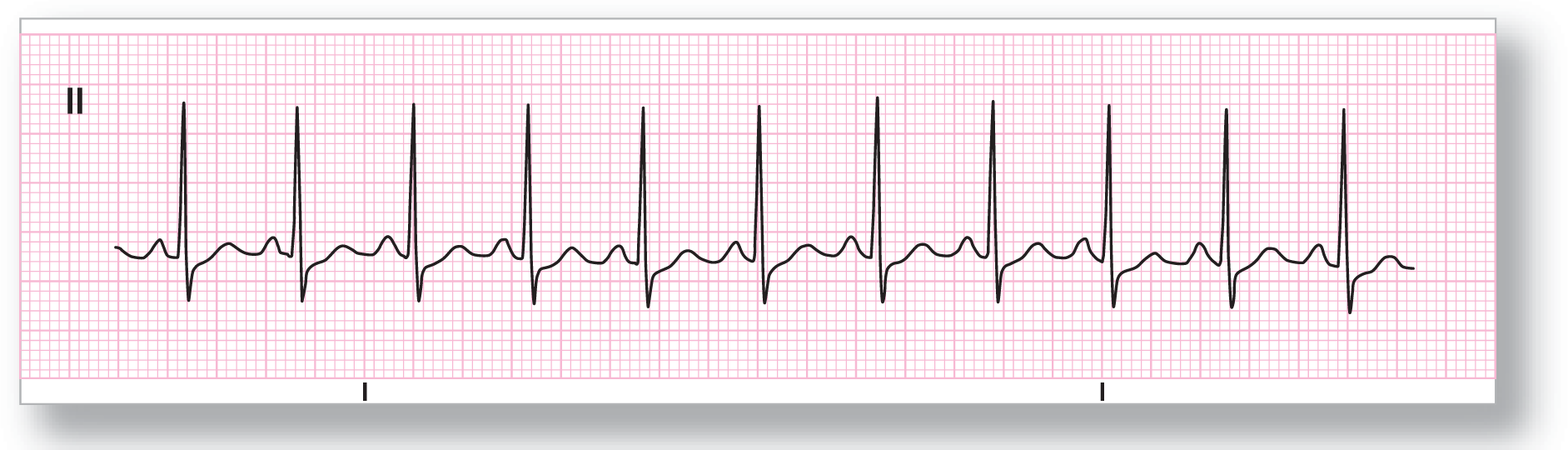
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 120 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present |
Rhythm: Sinus tachycardia |
Discussion:
ECG 10-3 is classic for sinus tachycardia. Note the easily identifiable P waves and the very slight irregularities in the morphology of the complexes. The irregularities are enough to be noticeable but not to the degree that you would expect from ectopic pacemakers.
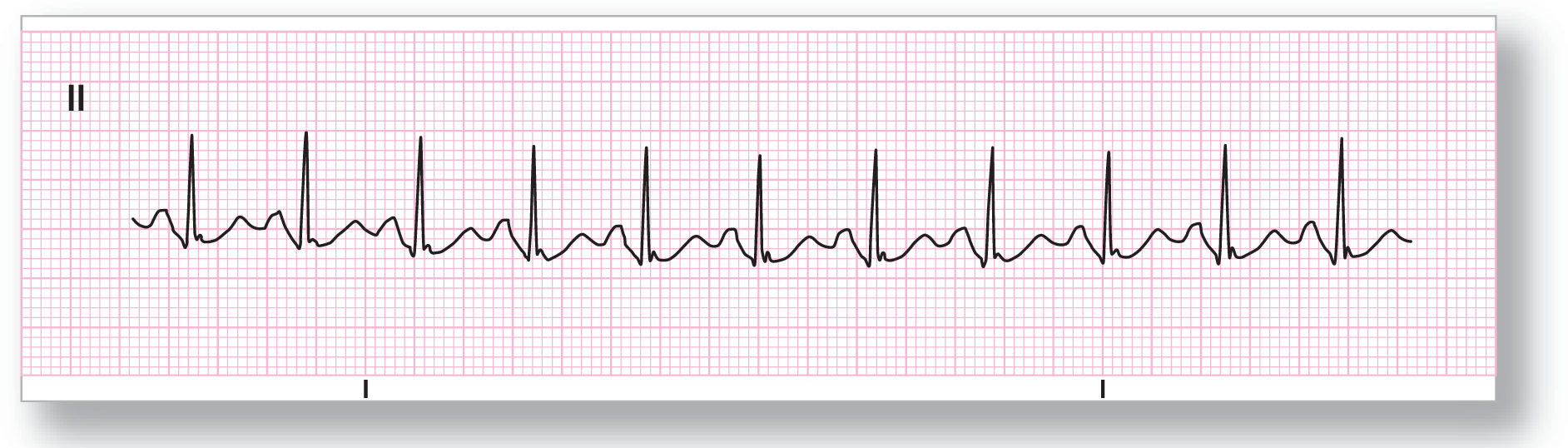
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 125 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present |
Rhythm: Sinus tachycardia |
Discussion:
ECG 10-4 is also fairly classic for sinus tachycardia. Note that the T waves and the P waves run into each other because the TP segment is nonexistent. In these cases, you need to use the base of the PR interval as the baseline for the strip. Using this as the baseline, the height of the P waves is dramatic. However, you cannot make the call of atrial enlargement on a rhythm strip—a full 12-lead ECG is needed to make that diagnosis.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 115 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present |
Rhythm: Sinus tachycardia |
Discussion:
ECG 10-5 is, once again, sinus tachycardia. Note the tall, prominent P waves, the flat ST segment, and the flipped T waves present on the complexes. The combination of flat ST segments and flipped T waves on an ECG would be consistent with ischemia. All you can say about them on a rhythm strip is that they are suggestive of ischemia, and a 12-lead ECG should be obtained for further evaluation. Always be suspicious and you won’t get burned!
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: A little over 100 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Widened ≥ 0.12 sec. |
|
P waves: Present |
Rhythm: Sinus tachycardia |
Discussion:
ECG 10-6 is a bit more problematic than the previous ones. There are a couple of reasons for this. First, the QRS complexes are wider than 0.12 seconds. This means you have to think about bundle branch blocks, aberrancy, or ventricular complexes as the source of the widened interval. Secondly, the T wave and the P waves run into each other to further complicate issues; however, with a P wave before each complex and a 1:1 ratio of P and QRS complexes, you can pretty well rule out ventricular complexes. A 12-lead ECG verified the fact that this was a patient with sinus tachycardia and a right bundle branch block.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: A little over 135 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present |
Rhythm: Sinus tachycardia |
Discussion:
ECG 10-7 has clear P waves before each QRS complex and the heart rate is over 100 BPM, making it consistent with sinus tachycardia. Once again, it is not a good idea to make a diagnosis about anything but the rhythm on a rhythm strip, but we can use it to justify some further investigation. Do you notice anything troubling about the strip above? What sticks out the most is the obvious ST-segment elevation that is present. Is this an AMI? Should we give thrombolytics? The answer to both of these questions is . . . we need to see a 12-lead ECG. The ST-segment elevation that is present could represent an AMI; however, it could also represent pericarditis. Giving thrombolytics to a patient with an AMI is definitely a good idea, provided there are no contraindications and the medication is clinically warranted. Giving thrombolytics to someone with pericarditis is not a very good idea. It would probably kill the patient by causing a hemorrhagic pericardial tamponade.
A 12-lead ECG, or at least additional leads, would be highly suggested and therapy should be based on the patient’s clinical history, physical examination, and ECG. This patient was indeed having an inferior wall MI. Quick and definitive action led to a good outcome.
The take-home point is that rhythm strips can be of more use than just a tool to recognize an arrhythmia. When you look at a rhythm strip, analyze the whole strip and remember that it represents one lead of a whole ECG. Then, put that information together with your history, physical, and other diagnostic tests to formulate your best clinical impression of the entire situation.