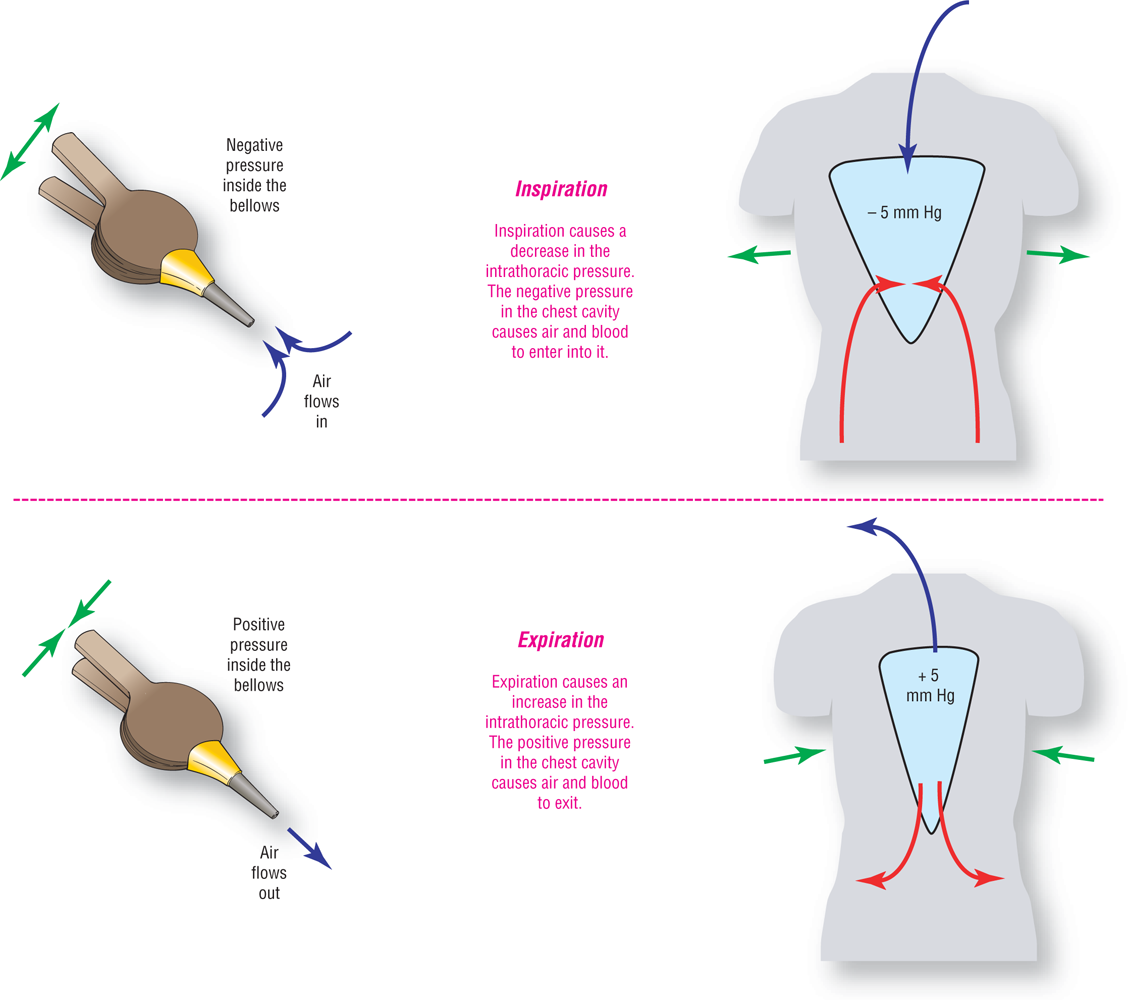
Figure 11-2 Inspiration and expiration.
© Jones & Bartlett Learning.
DescriptionWhen we breathe, our chest wall acts like the bellows that are used by blacksmiths (Figure 11-2). As the lungs expand with inspiration, the intrathoracic pressure (pressure inside the chest cavity) decreases. The laws of physics state that gases and fluids will always try to move from an area of higher pressure to an area of lower pressure. Therefore, air rushes into the lungs when we expand our chest wall because it is going from an area of higher pressure (the outside air) to an area of less pressure (the space within our lungs during inspiration). Notice that the air movement is passive, but the wall motion is active and controlled by the person. In addition to the air, blood from our extremities and abdomen also follows the pressure gradient and moves from our bodies to the right side of the heart.
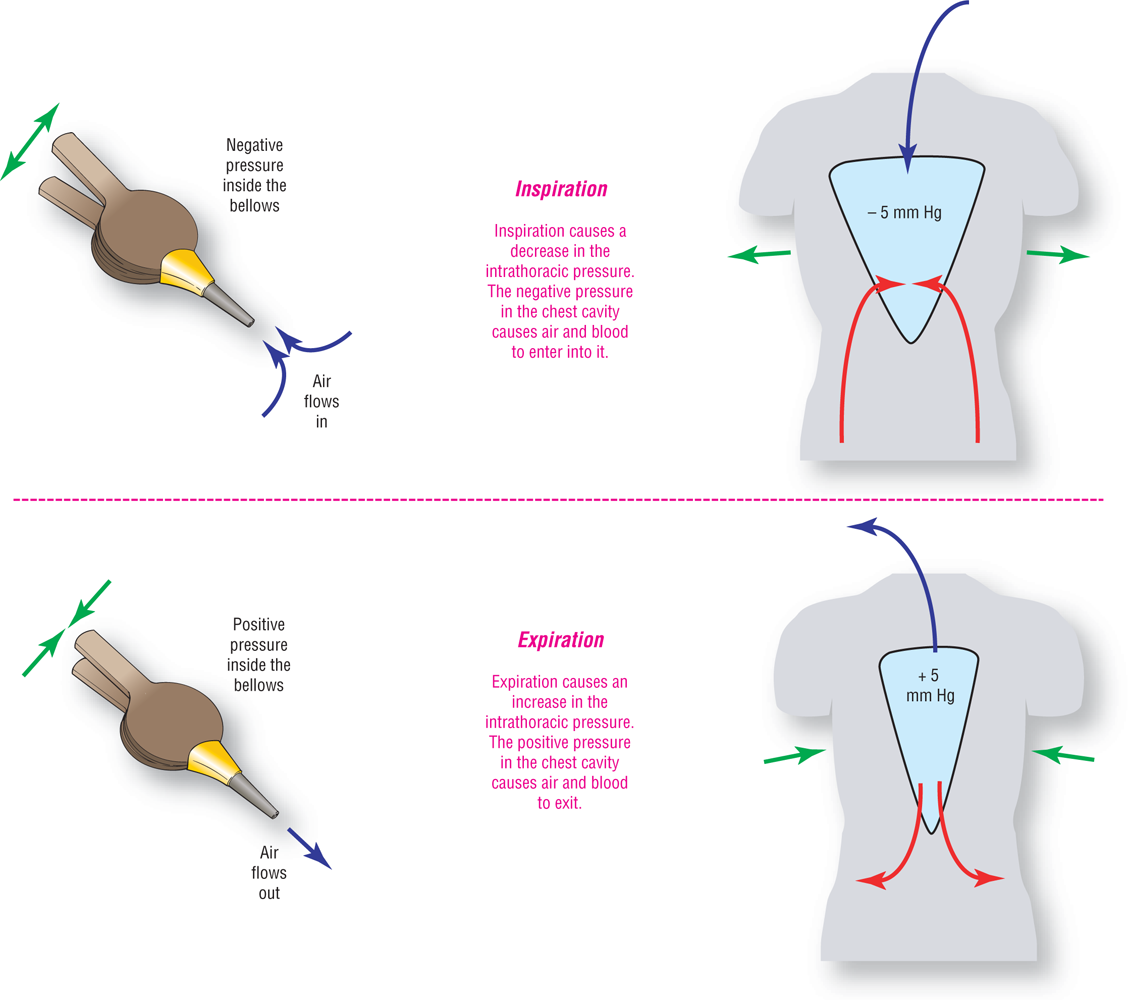
Figure 11-2 Inspiration and expiration.
© Jones & Bartlett Learning.
DescriptionThe increased amount of blood that comes into the thoracic cavity during inspiration causes the right atrium and ventricle to fill more efficiently. The increased blood flow to the right atria triggers some baroreceptors (receptors in the wall that measure distention and pressure in the chamber) that inhibit the normally-occurring vagal tone. The net result is that the heart rate increases slightly, helping move the excess blood from the intrathoracic space.
During expiration, the diaphragm relaxes and pushes upward into the chest, increasing the intrathoracic pressure. The pressure in the right atrium decreases and the baroreceptors do not exert their inhibitory stimulation on the vagal nerve, allowing it to behave normally. Vagal stimulation causes a transient slowing of the heart rate and a decrease in the amount of blood leaving the chest.
Note that we are mostly focusing on the right atrium. The left atrial response is partially muted because blood can pool within the lungs, as shown in the green areas of Figure 11-3.
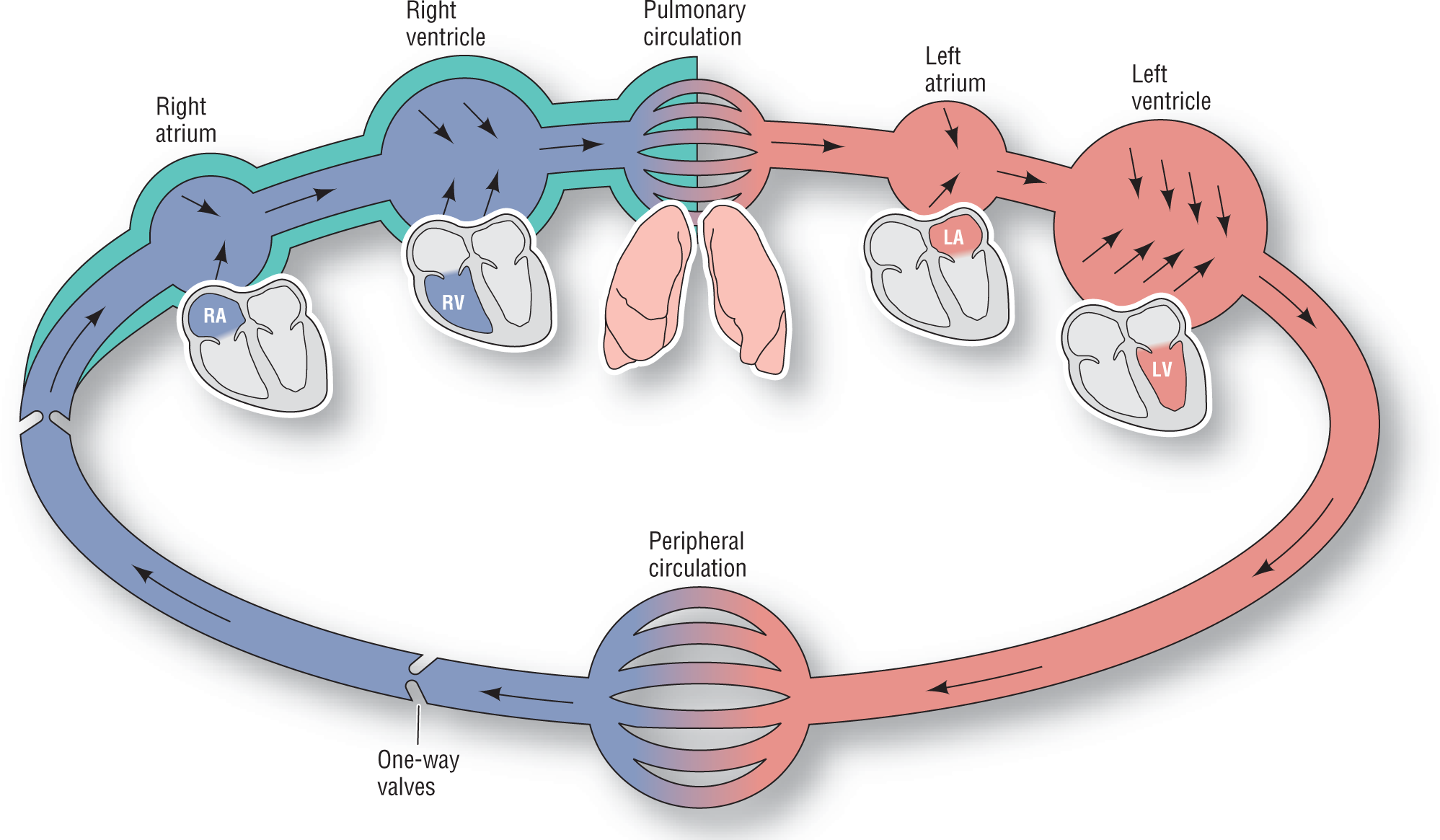
Figure 11-3 The green area represents the additional blood volume in the intrathoracic space due to inspiration. Note that the blood pools in the pulmonary circulation.
© Jones & Bartlett Learning.
DescriptionAll of the changes mentioned previously occur in seconds during the respiratory cycle. The transient increase in the heart rate that results from the vagal inhibition can be easily spotted on an ECG or a rhythm strip (Figure 11-4). This transient speeding up of the rate is especially evident when the underlying heart rate is bradycardic. That is why respiratory sinus arrhythmia is seen more commonly during slower heart rates and in athletes, since they usually have slower rates at baseline.
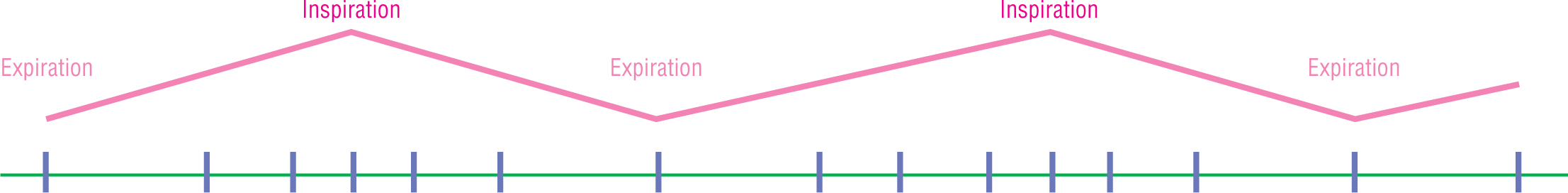
Figure 11-4 The green line represents a baseline on an ECG. The blue lines represent individual complexes. Note the gradual speeding up and slowing down of the heart rate with each respiratory cycle.
© Jones & Bartlett Learning.
Sinus arrhythmia is also very common in young children and disappears as they get older. In general, the rhythm also tends to disappear when the rate increases, as occurs, for example, with atropine or with exercise.
It is important to always remember that respiratory or phasic sinus arrhythmia is a variant of normal and is not a pathologic arrhythmia.