Figure 13-16 Action potential.
© Jones & Bartlett Learning.
DescriptionMany times during your career you will come face-to-face with a diagnostic dilemma. You will have a complex that has the features of one type of arrhythmia, but with some features that point directly toward another possibility. At times like these, you want to use every tool available to you to help you distinguish between the two possibilities. The type of pause that occurs immediately after a premature complex is just such a tool. Luckily, there are only two types of pauses that you need to worry about—the compensatory and noncompensatory pauses.
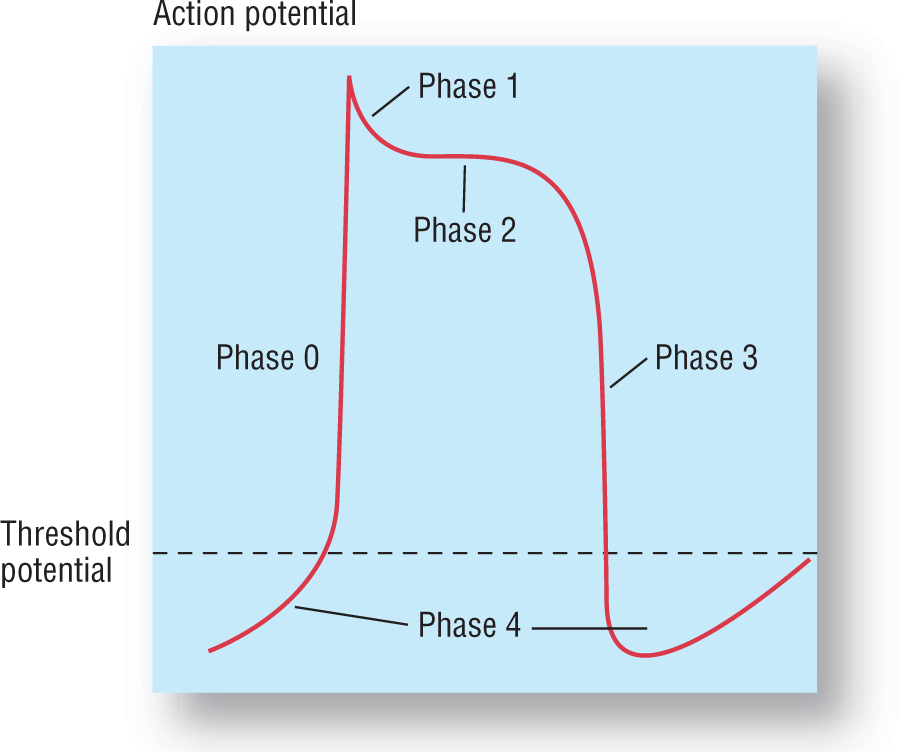
The key to understanding the two types of pauses is to understand the concept of phase 4 repolarization (Figure 13-16) and the resetting of the pacemaker. Recall from Chapter 2, Electrophysiology, that phase 4 repolarization refers to the slow influx of ions that cause a gradual depolarization of the cell toward the threshold potential. This is the basis of the pacemaking function of the cells of the heart. The rate of the ascent of phase 4 is individual to each type of cell found in the heart, and is responsible for the intrinsic pacing rate for each of those cell types (Figure 13-17).
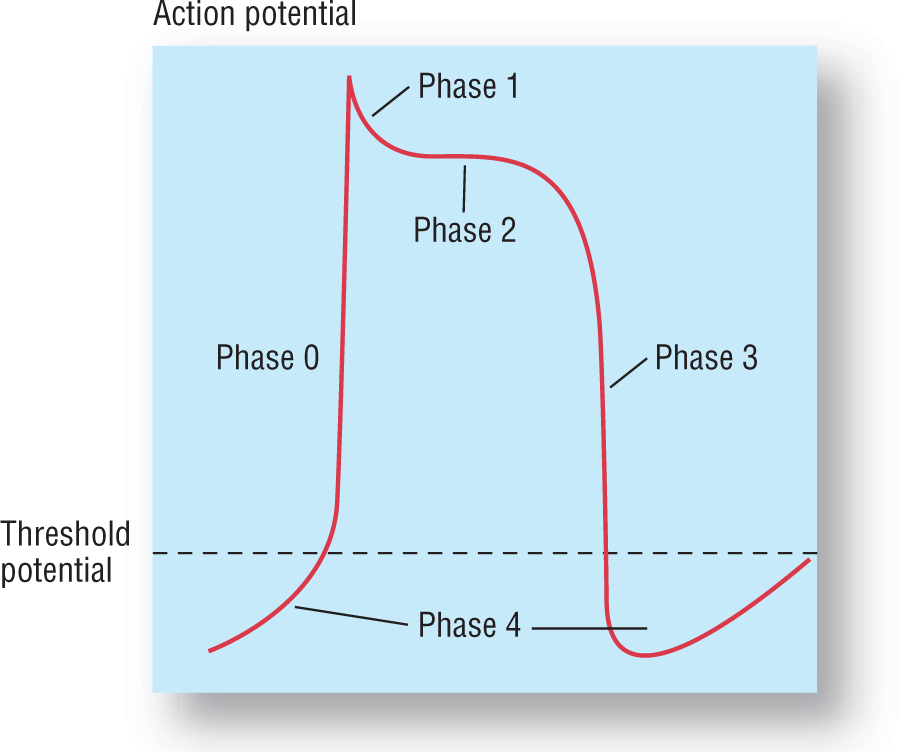
Figure 13-16 Action potential.
© Jones & Bartlett Learning.
Description
Figure 13-17 Pacemaker rates for the various areas.
© Jones & Bartlett Learning.
DescriptionNow, for the sake of discussion, let’s take a look at one cell in the SA node as it is clipping along. The cell goes through a continuous series of phase 4 depolarizations and firing whenever the threshold potential is crossed (Figure 13-18). Suddenly, there is an unexpected depolarization wave that causes the cell to fire sooner than expected (e.g., a PAC, represented by the green star). As long as the cell is not in its absolute refractory phase, it will fire immediately. After the premature depolarization has occurred, the cell will continue with its phase 4 depolarization as before. But, notice that the regularity of the rhythm has been altered. The pacemaker was reset by the premature impulse. The new rate may be the same as before or it may be different (faster or slower).

Figure 13-18 Faster firing rate of a premature complex.
© Jones & Bartlett Learning.
To think about it another way, let’s consider a very common occurrence in our everyday lives. Have you ever been counting something, such as money, and someone calls out a different number? Suddenly, you are confused and can’t remember what number you were on. What is it that most of us do at this point? We start all over again. That is exactly what the SA node does. It is pacing and minding its own business, when suddenly a PAC comes along and confuses it with an early discharge. The SA node then resets and starts a new count (Figure 13-19).

Figure 13-19 The rushing depolarization wave from the PAC causes the SA node to immediately depolarize. This resets the pacemaker, which can either take up the same rate, go a little faster, or go a little slower than before.
© Jones & Bartlett Learning.
Electrocardiographically, the same thing is happening. First, we see a nice, regular sinus rhythm. Then a PAC occurs, which resets the pacer. A new sinus rate emerges. The pause that includes the PAC and the time immediately after the PAC is the diagnostic point that we will focus on in this section. Notice that if the SA node were depolarized and reset, the time frame during which the PAC and the pause occurred would not be an exact multiple of the normal P-P interval. That type of pause is known as a noncompensatory pause. If the SA node were not reset, the pause would be an exact multiple of the regular P-P interval, and then you know that the SA node was not reset. That type of pause is known as a compensatory pause.
First, let’s take a closer look at the noncompensatory pause. In a noncompensatory pause, the pause is not a multiple of the normal P-P interval (Figure 13-20). This is because the resetting of the SA node causes a variable time period to occur before it starts up again. The key to this type of pause is that the SA node was reset. The SA node is usually reset with a PAC. (PJCs and PVCs can also cause noncompensatory pauses if there is some retrograde conduction of the impulse back through the AV node to depolarize the atria. However, this doesn’t occur all the time.) The take-home message is that a noncompensatory pause usually points you in the direction of a PAC.
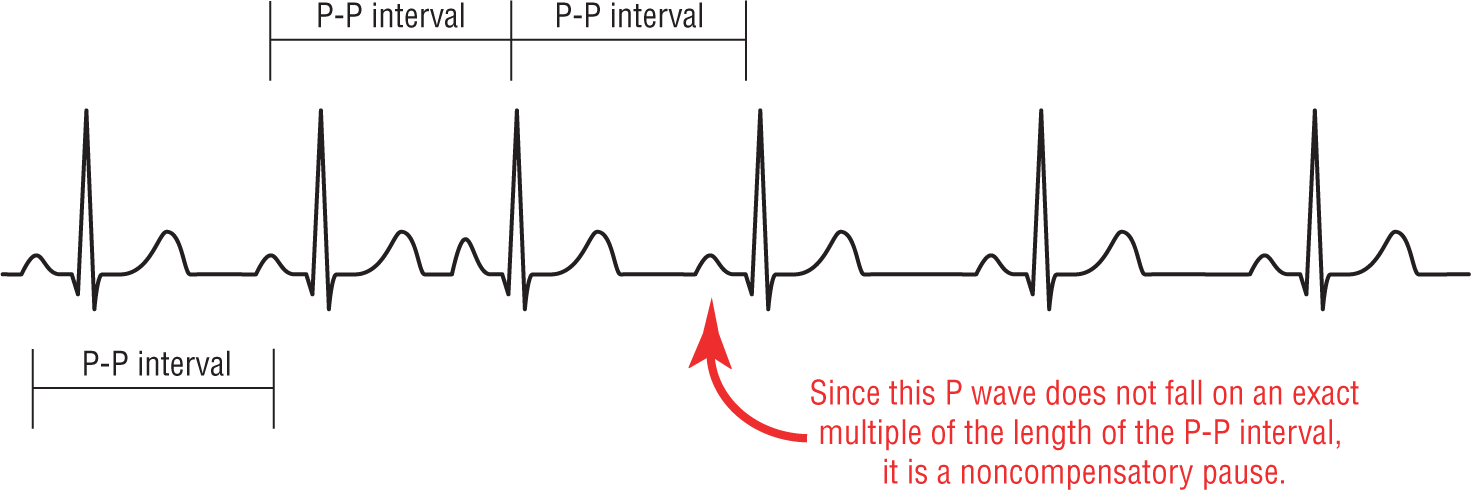
Figure 13-20 Noncompensatory pause.
© Jones & Bartlett Learning.
Now, let’s switch our attention over to a compensatory pause (Figure 13-21). In a compensatory pause, the SA node is not reset. It continues clipping along at its normal pace, oblivious to the premature impulse that occurred. It would be very unusual for an atrial depolarization wave to avoid the SA node entirely. However, an impulse that originated in the AV node or in the ventricles could have occurred with no retrograde conduction to the atria.
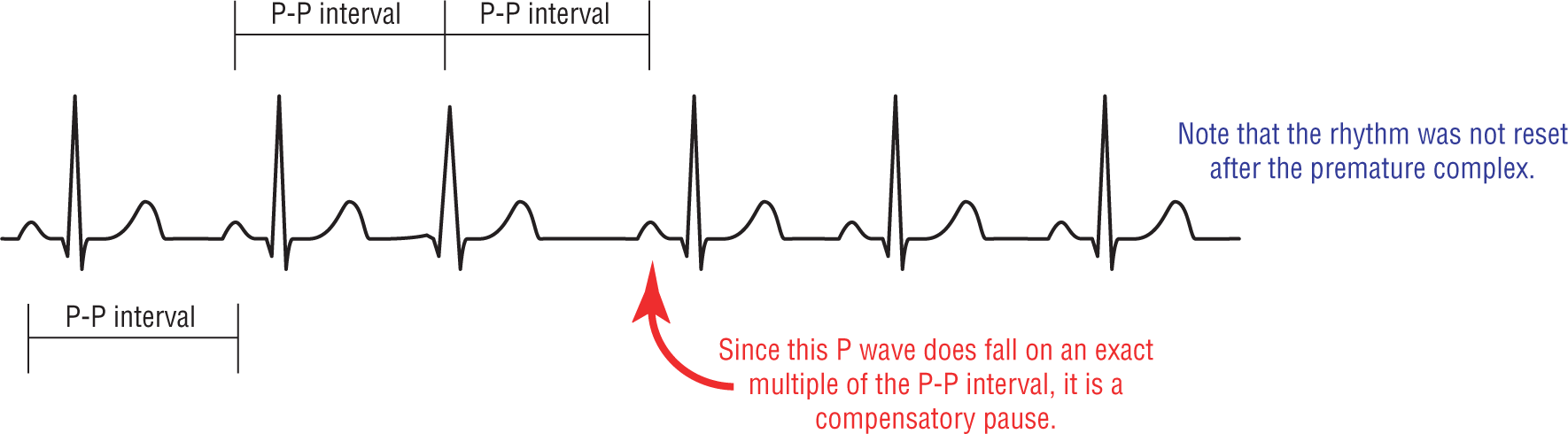
Figure 13-21 Compensatory pause.
© Jones & Bartlett Learning.
DescriptionIt is important to remember, when dealing with compensatory pauses, that the atria and the ventricles live in two different worlds with their only source of contact being the AV node. The AV node functions as a gatekeeper between the atria and the ventricles. As such, the AV node was created to allow antegrade conduction; it was not created to allow retrograde conduction. It allows impulses to pass easily to the ventricles. However, retrograde conduction back to the atria is a different matter. Retrograde conduction is only allowed to pass through once in awhile.
If the AV node does not allow a ventricular impulse to be spread retrogradely to the atria, then the atria would never know about it. Think of it as an event that occurred in another country. We would only be aware of it if we heard of it in the news. If you don’t hear about it, you can’t react to it. The same is true with the SA node. If it does not get depolarized by the impulse, it will not reset and will keep clipping along at its regular uninterrupted pace (Figure 13-22).

Figure 13-22 This is a strip isolating atrial activity only. Note that there is no break in the regularity of the rhythm. The premature complex, represented by the green star, did not influence the SA node in any way.
© Jones & Bartlett Learning.
A compensatory pause occurs when a premature impulse fails to reset the SA node. The time interval involving the premature impulse and the subsequent pause will, therefore, be a multiple of the normal P-P interval because the SA node was not reset. Frequently, you will see the sinus P marching through or fusing with the premature complex. Compensatory pauses usually occur with PJCs or PVCs, not with PACs. Not a bad diagnostic tool to have in your arsenal.