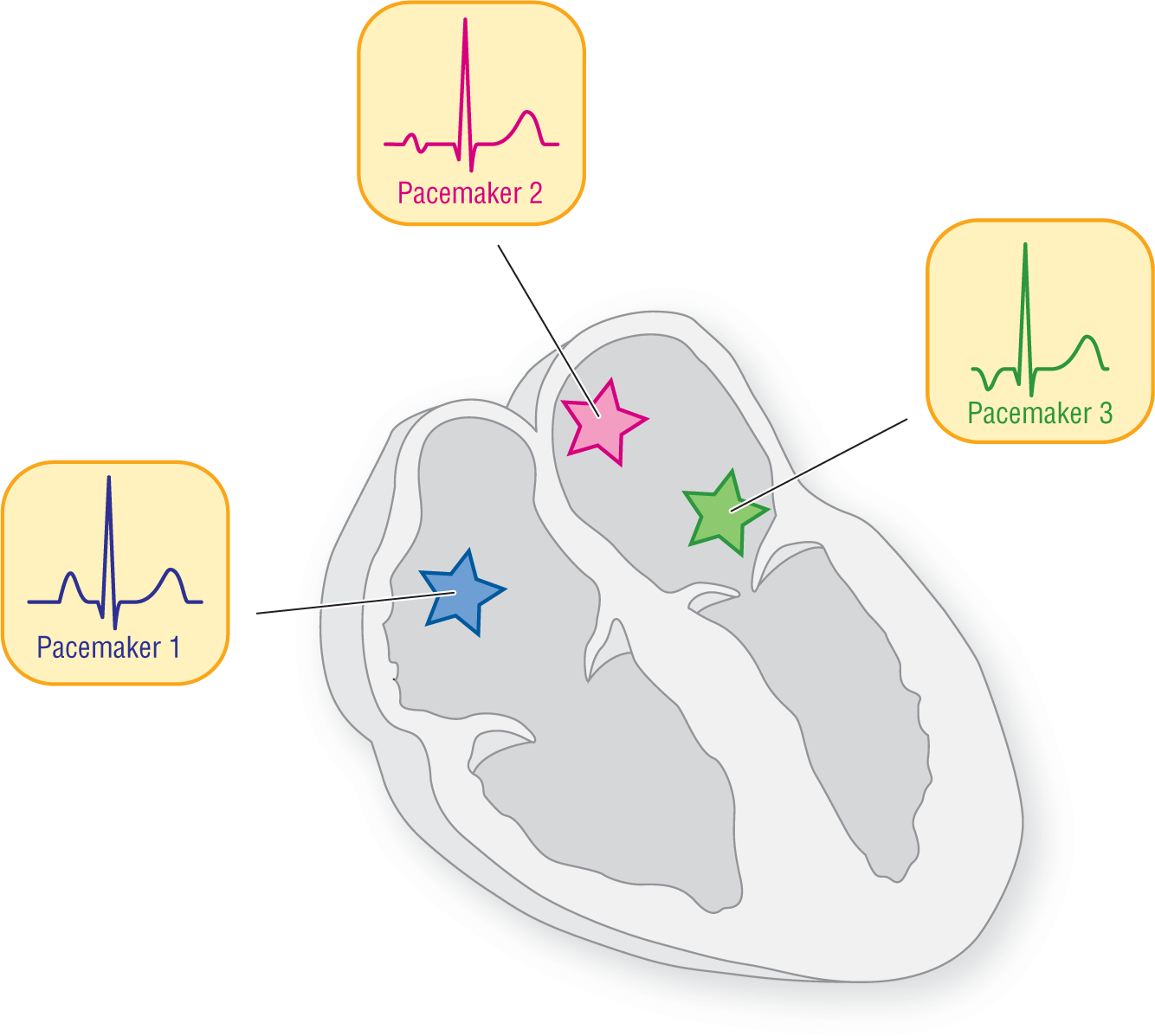
Figure 17-3 At least three individual pacemaker sites are at work in creating this presentation of wandering atrial pacemaker. Each site is associated with an individual P-wave morphology and PR interval.
© Jones & Bartlett Learning.
DescriptionWandering Atrial Pacemaker: A Clinical Variation
In addition to the cases that meet the preceding traditional definition of WAP, there is another variation that occurs more commonly in everyday clinical medicine but has never, to our knowledge, been given an official title. Clinically, WAP also refers to an irregularly irregular rhythm created by multiple (three or more) ectopic atrial pacemakers each firing at its own rate. The resulting rhythm has no underlying regularity and is completely chaotic. Note, however, that the heart rate for WAP is always 100 BPM or less.
This entity or presentation is more common than previously thought because it is found in patients with enlarged atria and pulmonary disease (e.g., chronic obstructive pulmonary disease [COPD]). Because these clinical scenarios are relatively common in everyday practice, this rhythm abnormality is encountered more frequently. Since clinicians were forced to call this arrhythmia by some name, they chose to call it wandering atrial pacemaker.
How does this rhythm develop, and what does it look like on a rhythm strip? We went over some of the information already when we discussed regularity in Chapter 6, Electrocardiography and Arrhythmia Recognition, but it is worthwhile to review these concepts again.
This variation of WAP develops when at least three atrial pacemaking sites are involved in the production of the rhythm. As we saw in Chapter 13, Premature Atrial Contraction, each atrial pacemaker has its own intrinsic three-dimensional location on the atria. Because of this location, its P-wave morphology, and the PR interval associated with it, form an electrocardiographic pattern that is unique (Figure 17-3).
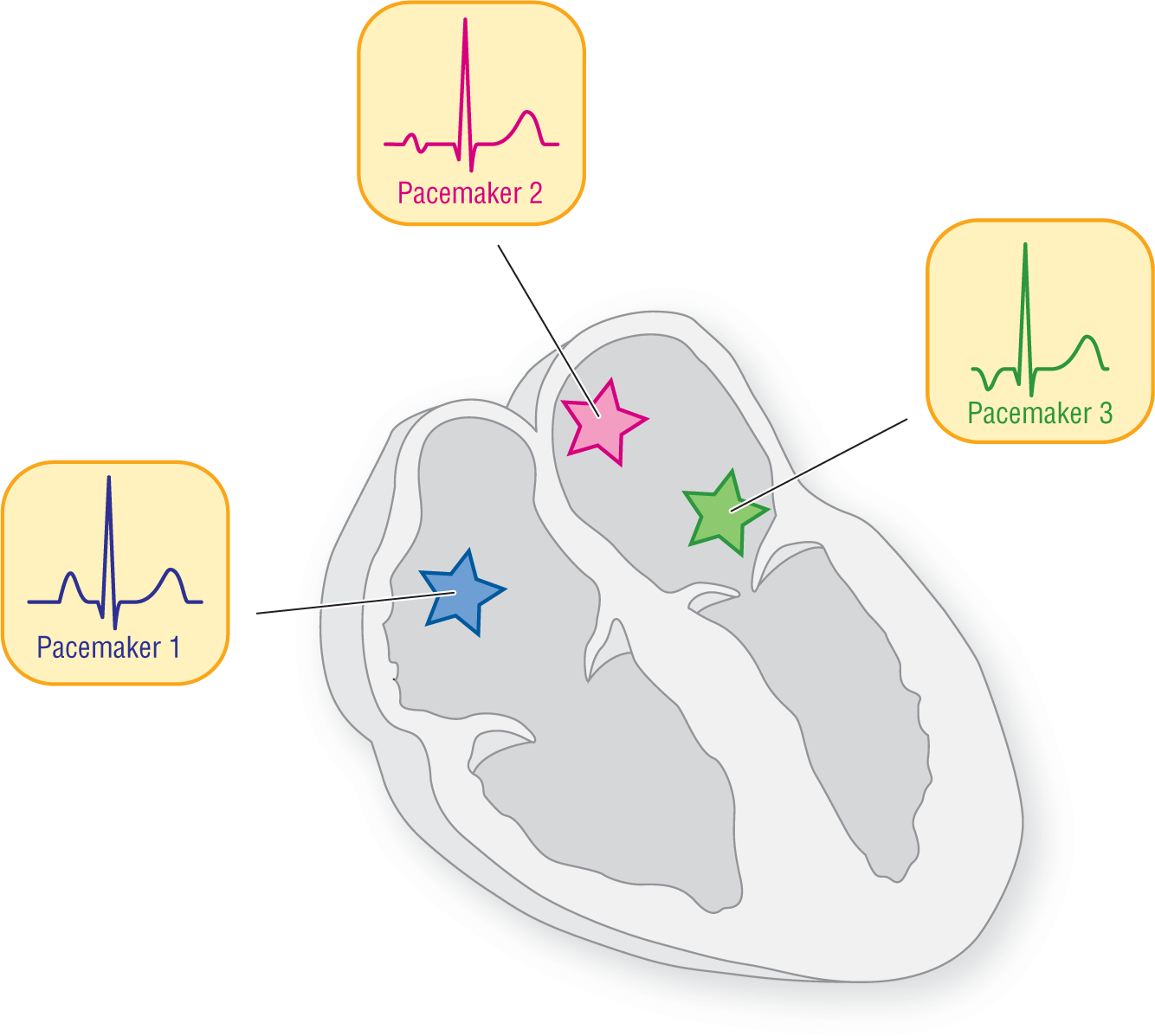
Figure 17-3 At least three individual pacemaker sites are at work in creating this presentation of wandering atrial pacemaker. Each site is associated with an individual P-wave morphology and PR interval.
© Jones & Bartlett Learning.
DescriptionIn addition to its appearance, each site also has a characteristic rate associated with it. Now, suppose we took a tracing from each of our three pacemakers individually. In Figure 17-4, each complex is represented by a small rectangle filled with its own individual color for simplicity. Notice how the three pacemakers each have an individual rate. But, in real time and in real life, the complexes would sometimes cancel each other out or fuse. The combined strip at the bottom of Figure 17-4 would be the result.

Figure 17-4 Individual rates of three ectopic pacemakers being electrocardiographically represented as one rhythm.
© Jones & Bartlett Learning.
DescriptionNotice that we have not even included two other factors that add to the complete chaos that is represented in this type of WAP: irritability and fusion. In addition to its own intrinsic pacemaking rate, the ectopic atrial foci in the clinical scenarios associated with this presentation are typically irritable. As we have seen, irritability leads to premature complexes, which could further alter the regularity of the rhythm. Fusion of the various components of the complexes or the complexes themselves also occurs, leading to frequent aberrancy and bizarre fused morphologies of the waves in WAP.
The final strip in Figure 17-5 shows the typical pattern of this presentation of WAP. For this type of presentation, therefore, the definition of WAP becomes: an irregularly irregular rhythm with a ventricular rate of 100 BPM or less, characterized by at least three different P-wave morphologies on the same strip, each associated with its own PR interval. Note that, contrary to a tracing with just frequent PACs, there is no underlying regular rhythm associated with it.
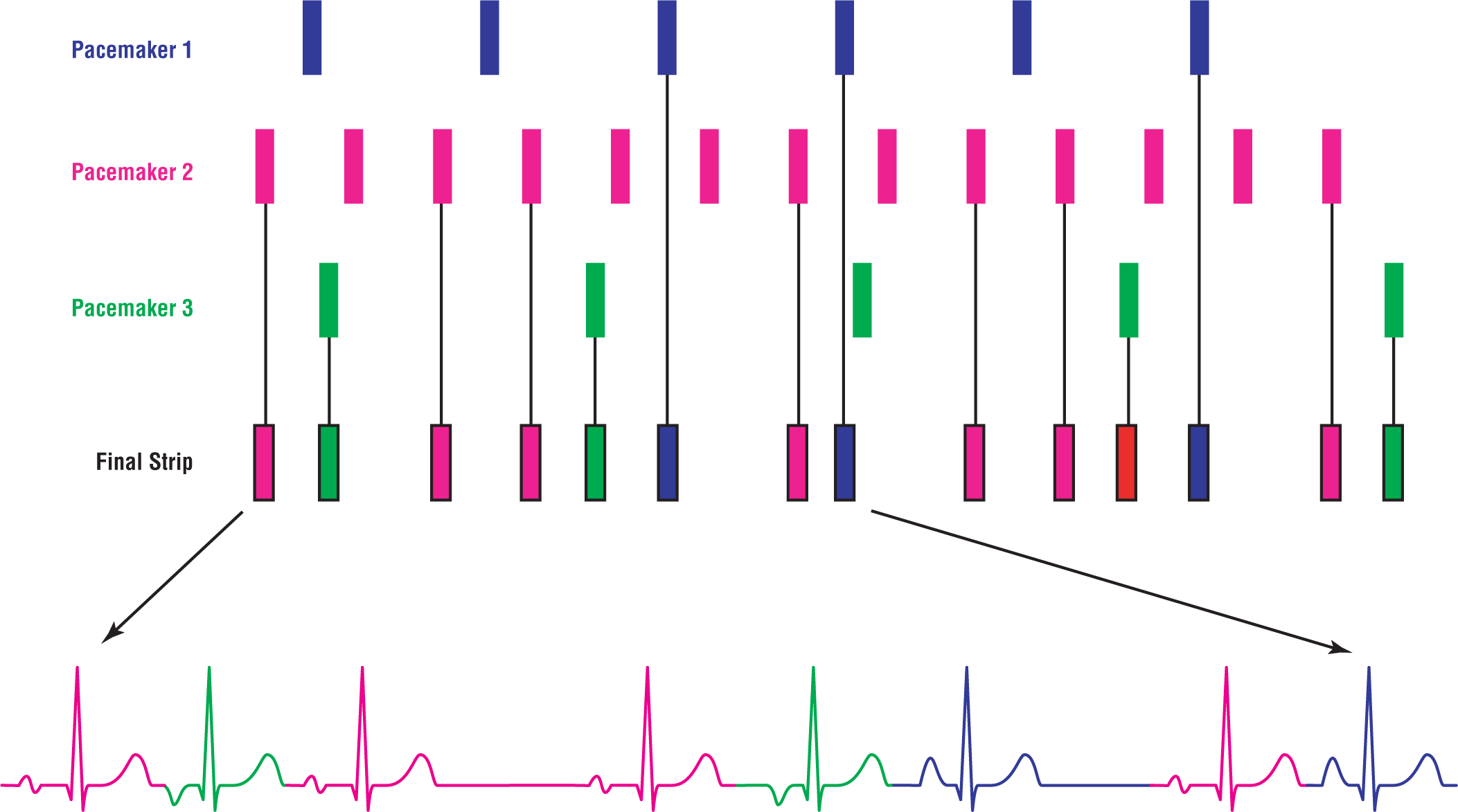
Figure 17-5 Note that there is no regularity to the rhythm. In real life, irritability and fused waves would further complicate the tracing.
© Jones & Bartlett Learning.
DescriptionARRHYTHMIA RECOGNITION
Wandering Atrial Pacemaker
| Rate: | 100 BPM or less |
| Regularity: | Irregularly irregular |
| P wave:
Morphology: Upright in II, III, and aVF: |
Present
Variable Sometimes |
| P:QRS ratio: | 1:1 |
| PR interval: | Variable |
| QRS width: | Normal or wide |
| Grouping: | None |
| Dropped beats: | Sometimes |
DIFFERENTIAL DIAGNOSIS
Wandering Atrial Pacemaker
This list is not all-inclusive.