Additional Information
1:1 Conduction
One of the most dangerous rhythms covered in this text is atrial flutter with 1:1 conduction. The problem with this conduction ratio is that, since the usual atrial rates are between 200 and 400 BPM, the ventricular rates will match the atrial rate. The net result is a catastrophic drop in blood pressure due to decreased stroke volume. As we saw in Chapter 1, Anatomy and Basic Physiology, the drop in stroke volume is due to the lack of ventricular filling and the loss of the atrial kick that typically occur in very rapid tachycardias.
When do we get 1:1 conduction of atrial flutter? The answer is variable. It can definitely occur with a normal AV node when the atrial rate is slow. During episodes of slow atrial beating, the AV node can transmit the impulse routinely and does not need to block any of the impulses. Sometimes drugs, like the catecholamines, can stimulate conduction through the AV node to the point that rapid tachycardias can ensue. The most common mechanism, however, is due to the presence of an accessory pathway. This information is a bit advanced, but the life-threatening quality of this complication and the frequency with which it is clinically found make review of this topic mandatory for all clinicians.
If you remember from Chapter 1, Anatomy and Basic Physiology, the only area of communication between the atria and the ventricles involves the AV node in almost all patients. There are, however, a certain few patients who have a second (or multiple) tract that traverses the AV septum (Figure 19-14). The result is that an electrical impulse can travel back and forth repeatedly through this bypass tract, avoiding the gatekeeping control of the AV node.
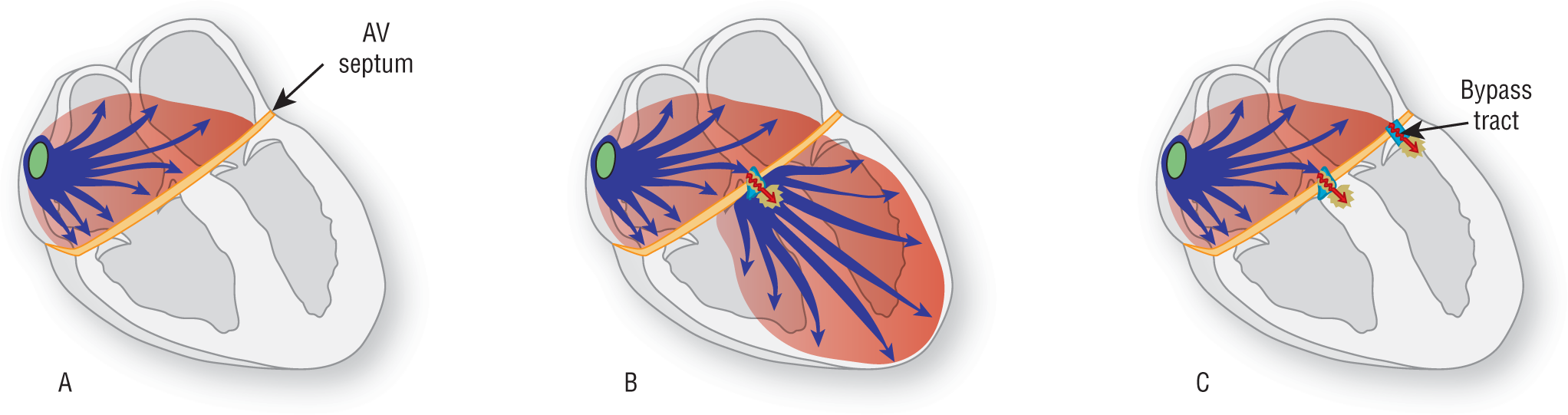
Figure 19-14 The AV septum represents a nonconductive wall between the atria and the ventricles. If the AV septum did not have any communication between the atria and the ventricles, the impulse would never reach the ventricles (A). The AV node provides a normal pathway through the AV septum and provides the gatekeeping function critically needed to maintain AV synchronization (B). An accessory pathway provides a bypass tract that allows an additional area of communication between the atria and the ventricles (C). The problem is that the bypass tract does not have a gatekeeping function and allows unlimited and unhindered communication between the atria and the ventricles. The result could be catastrophic arrhythmias, which could be life threatening in many cases.
© Jones & Bartlett Learning.
DescriptionThe net result of the loss of control created by these bypass tracts is that the atrial rates and the ventricular rates can be identical in these patients. If the atrial rate is 100 BPM, the bypass tract may or may not function. In either case, the net result is the same: The ventricular rate is 100 BPM. If the atrial rate is 300 BPM, the AV node functions as a gatekeeper but the bypass tract does not, and the net result is that the ventricular rate is 300 BPM. This same process can continue for even faster rates, including atrial fibrillation, which we will cover in the Atrial Fibrillation chapter. The lack of AV nodal control can lead to some very serious life-threatening tachycardias (Figure 19-15).
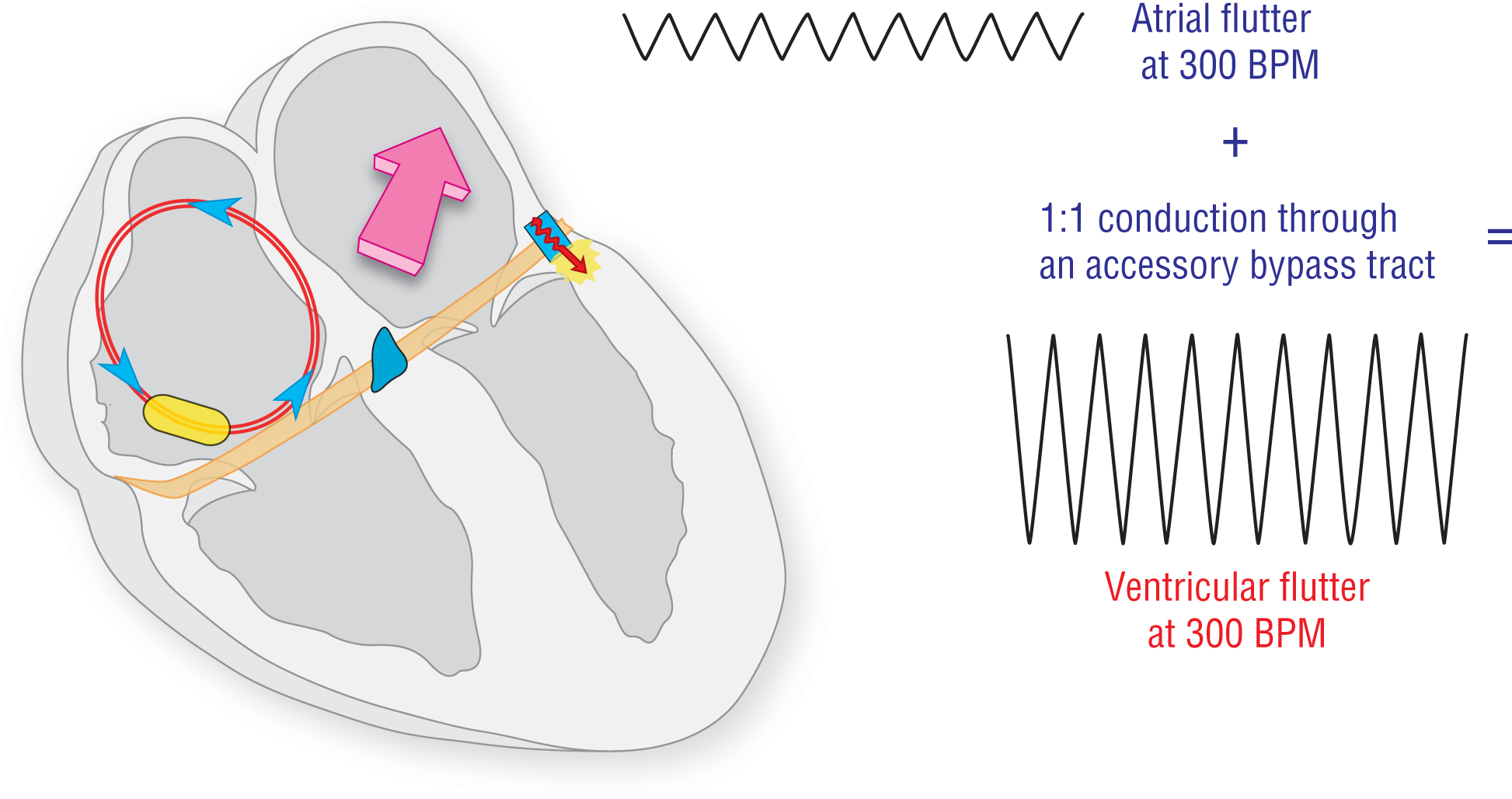
Figure 19-15 1:1 conduction.
© Jones & Bartlett Learning.
DescriptionSince the ventricular depolarizations occur through a bypass tract in these cases, the QRS complexes will be wide and aberrantly conducted. This occurs because the normal electrical conduction system is not used at all to transmit the impulse through the ventricles. Instead, the impulse is transmitted throughout the ventricles by the slow direct cell-to-cell transmission route. The morphology of the complexes will depend on the location of the bypass tract and the route taken by the depolarization wave as it makes its way throughout the ventricles.
A clinical pearl to remember is this: Think about a bypass tract on any strip or ECG with a ventricular rate over 250 BPM. These are very rapid rates and are well above the normal ranges for the standard electrical conduction system. The higher the rate, the greater the chance of an accessory pathway.