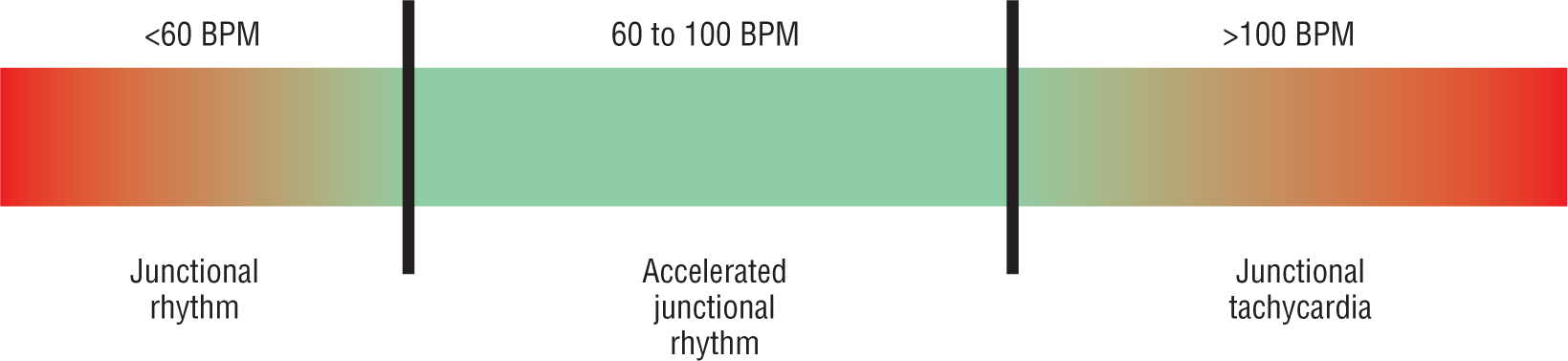
Figure 21-8 The spectrum of the junctional rhythms caused by increased intrinsic automaticity within the AV node and junctional area.
© Jones & Bartlett Learning.
DescriptionJunctional Rhythms: An Overview
As mentioned in Chapter 1, Anatomy and Basic Physiology, the intrinsic rate of the AV junctional area is between 40 and 50 BPM. However, we can clinically see junctional rhythms ranging from the 30s to over 300. Clinically, the junctional rhythms can be broken down into the intrinsic rhythms that originate somewhere in the AV junction and the reentrant tachycardias. The intrinsic rhythms include junctional escape complexes and rhythms, junctional premature complexes, accelerated junctional tachycardia, and junctional tachycardia. The two main reentrant tachycardias that we will cover include AV nodal reentry tachycardia and AV reentry tachycardia.
As a fail-safe or back-up pacemaker in case of sinus node malfunction, the junctional area performs its job admirably. For this reason, junctional escape complexes are quite common. Any slowing down of the atrial rate, for whatever reason, triggers a junctional escape complex. Many times the junctional escape complex depolarizes the SA node and causes a prolonged wait, which can stimulate another junctional escape, and so on. This type of cycle can easily stimulate a junctional escape rhythm, which is self-perpetuating and will persist until the SA node eventually speeds up. Generally, junctional escape rhythms will be between 40 and 60 BPM. They are easily spotted because of the rate and most importantly because of the presence of narrow, supraventricular QRS complexes with no observable P waves.
Increased automaticity will lead to junctional premature complexes and junctional rhythms that are above 60 BPM. Since this rate is above the intrinsic rate of the AV junction, these rhythms are known as accelerated junctional rhythms. If the rates of a junctional rhythm are above 100 BPM, they are referred to as junctional tachycardias. This spectrum is graphically represented by Figure 21-8.
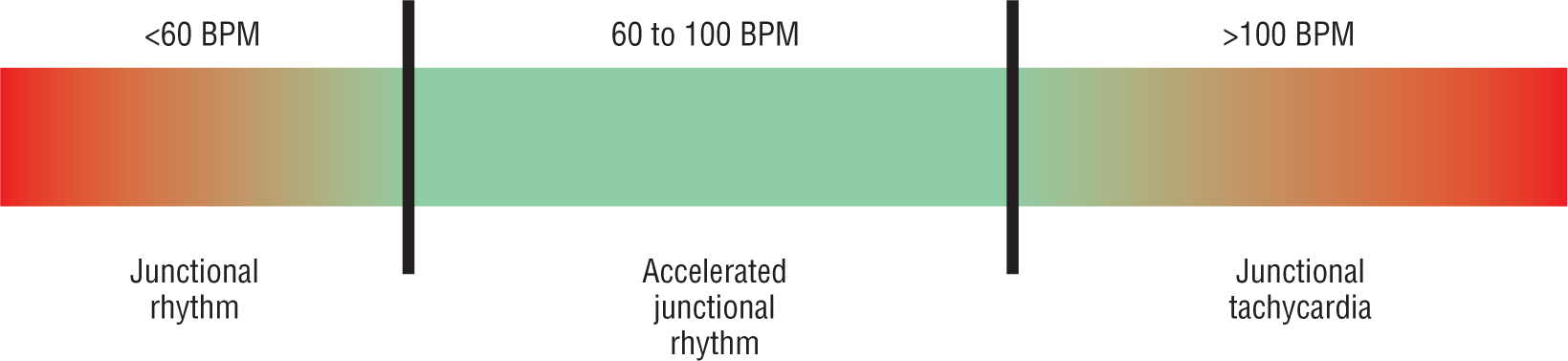
Figure 21-8 The spectrum of the junctional rhythms caused by increased intrinsic automaticity within the AV node and junctional area.
© Jones & Bartlett Learning.
DescriptionAs mentioned, the presence of narrow supraventricular complexes is important in identifying a junctional rhythm. There are some cases in which the complexes will be wide and aberrant. These include patients with preexisting bundle branch blocks, rate-related or ischemia-related aberrancy, and electrolyte abnormalities, to name a few. When wide supraventricular complexes are noted, it may be very difficult to differentiate the rhythm from a rhythm of ventricular origin such as ventricular tachycardia. If there is ever any question as to a possible ventricular origin of the complexes, they should be treated as if they are ventricular rhythms. Remember, the ventricles control the blood pressure. You should always treat for the worst-case scenario until proven otherwise!