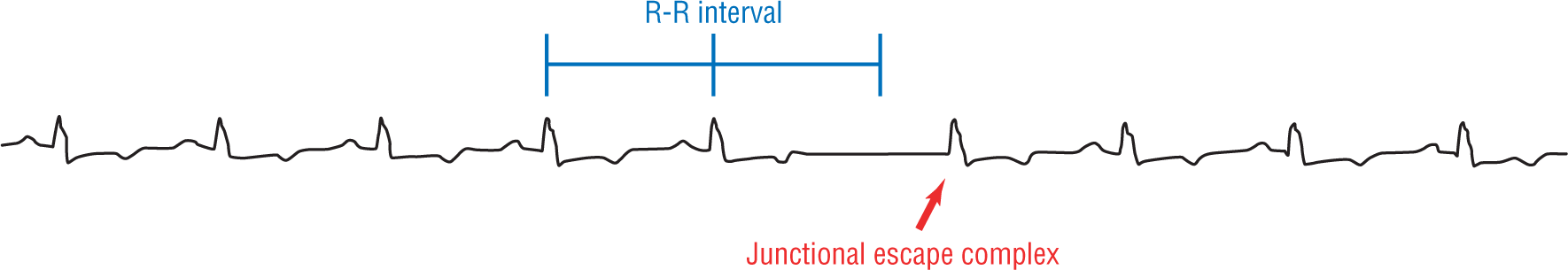
Figure 23-1 Sinus rhythm with a sinus pause leading to a junctional escape complex.
© Jones & Bartlett Learning.
DescriptionJunctional Escape Complexes and Rhythms
Remember in Chapter 1, Anatomy and Basic Physiology, we mentioned that the pacemaking function of all of the cardiac cells is occurring in all of the cells of the heart at the same time. The SA node, being the fastest, usually wins and sets the rate. Next in line would be the atrial myocardium itself. This ectopic pacemaker would give us an ectopic atrial rhythms. The next pacemaker in succession would be the AV node and the AV junctional area. In many cases, the atrial myocardium does not take over pacemaking function when the SA node fails and the pacing function skips right to the AV node directly.
Electrocardiographically, a junctional escape complex looks exactly like a sinus complex except that it doesn’t have a normal P wave, if it has any at all. Some minor variations may be present, but, in most cases, the QRS complex, the ST segments, and the T waves are identical to the normally conducted sinus complexes. Take a look at Figure 23-1. Notice how the sinus node suddenly fails to fire. An AV nodal pacemaker then fires, rescuing the ventricles from standstill. Then, the sinus node picks back up again continuing with a sinus rhythm. This is the usual presentation when there is a single solitary junctional escape complex.
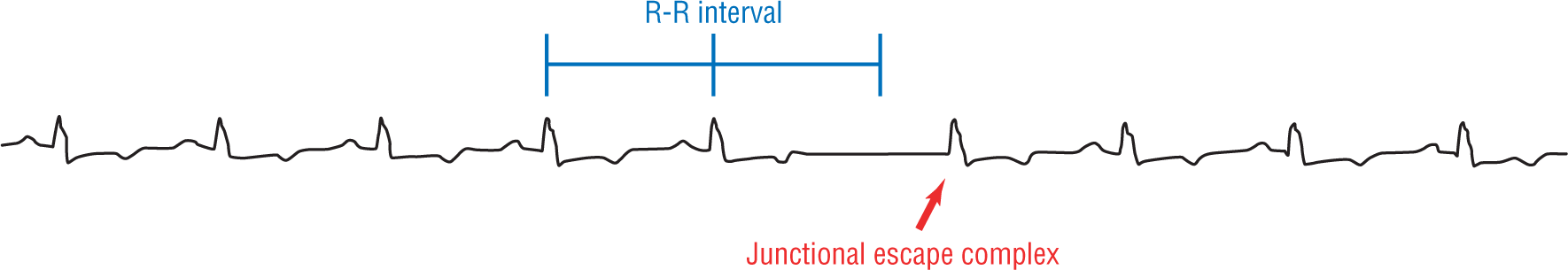
Figure 23-1 Sinus rhythm with a sinus pause leading to a junctional escape complex.
© Jones & Bartlett Learning.
DescriptionMany times, the rate or the rhythm immediately after the junctional escape complex is different than the one before it. A rate change is more commonly seen, but sometimes a different ectopic pacemaker may take over altogether.
Another common sequence is that the junctional escape complex depolarizes the SA node. The SA node then resets, taking a little longer to fire its next impulse. That extra time may be just long enough so that another junctional escape complex is triggered. This cycle is repeated over and over again, essentially creating a junctional escape rhythm or simply a junctional rhythm. When at least three consecutive complexes are junctional escape complexes, the rhythm is referred to as a junctional rhythm.
Figure 23-2 is an example of a junctional escape rhythm. The usual rate for a junctional rhythm is between 40 and 60 beats per minute (BPM). This rate is usually caused by an escape mechanism because it is too slow to be due to increased automaticity of a site (usually greater than 60 BPM). So, in general, even though a junctional rhythm is presumed to be due to escape, the word “escape” is usually presumed and the term shortened to junctional rhythm. The only time escape is explicitly used when describing a junctional rhythm is in the presence of an AV block.
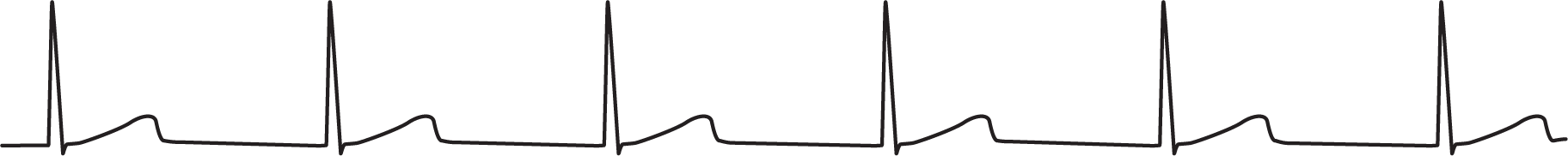
Figure 23-2 An example of a junctional rhythm.
© Jones & Bartlett Learning.
The baseline in a junctional rhythm can be completely flat, can have some minor irregularities, or as seen in Figure 23-3, can be completely erratic. The erratic baselines are usually caused by some sort of artifact. These sources of artifact can include tremors, outside electrical sources, moving lead wires, and so on.

Figure 23-3 The same junctional rhythm but with an erratic baseline.
© Jones & Bartlett Learning.
Cases with erratic baselines may be impossible to differentiate from atrial fibrillation with complete AV dissociation leading to a normalized junctional escape rhythm. It is difficult on a surface ECG to tell the difference between these two with any degree of certainty, and you need to maintain a high index of suspicion in these cases. Obtaining additional information, for example, by ruling out the possibility of digoxin toxicity, is critical. Remember, when interpreting any rhythm, always look at the company the rhythm keeps.
Junctional rhythms also commonly develop when there is no communication between the atria and ventricles. When this occurs, the atrial impulses die off before they ever reach the AV node and the ventricles. In these cases, the AV node takes over primary function as the pacemaker for the ventricles and, hence, a junctional rhythm is formed. We will be reviewing this occurrence in great detail in Chapter 28, Atrioventricular Blocks, when we talk about AV dissociation and complete heart block.
ARRHYTHMIA RECOGNITION
Junctional Rhythm
| Rate: | Between 40 and 60 BPM |
| Regularity: | Regular |
| P wave:
Morphology: Upright in II, III, and aVF: |
Absent or inverted
Abnormal No |
| P:QRS ratio: | Not applicable |
| PR interval: | Not applicable |
| QRS width: | Not applicable |
| Grouping: | None |
| Dropped beats: | None |
DIFFERENTIAL DIAGNOSIS
Junctional Rhythm
This list is not all-inclusive.