Figure 25-17 Findings in AV nodal reentry tachycardia.
© Jones & Bartlett Learning.
DescriptionStep 3: Identifying the Arrhythmia
A supraventricular tachycardia is a rough, general term for a rapid rhythm that has its origin in the atrial and junctional areas of the heart (the areas above the ventricles). The supraventricular tachycardias include sinus tachycardia, focal atrial tachycardia and its variations, paroxysmal atrial tachycardia, atrial flutter, atrial fibrillation, junctional tachycardia, AV nodal reentry tachycardia, and AV reentry tachycardia. (The term supraventricular tachycardia is such an umbrella term that it should be used sparingly, if possible. It is more clinically useful to determine the actual rhythm and to use the appropriate term for the arrhythmia.)
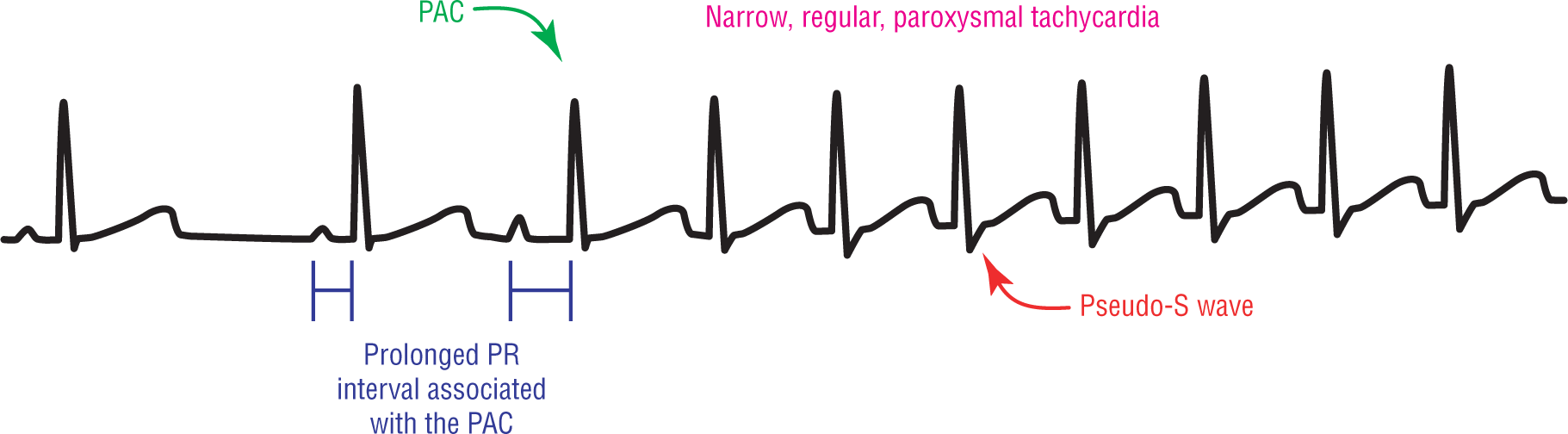
AVNRT is the most common regular paroxysmal supraventricular tachycardia found in clinical practice. Note the key words in that statement are the words “regular” and “paroxysmal.” AVNRT is a regular tachycardia that is caused by a reentry loop involving the AV junctional area. It is a paroxysmal (rapid onset, rapid termination) tachycardia that, as we saw, is usually triggered by a PAC (Figure 25-17). The PAC is usually associated with a prolonged PR interval because of transmission through the slow approach to the AV node.
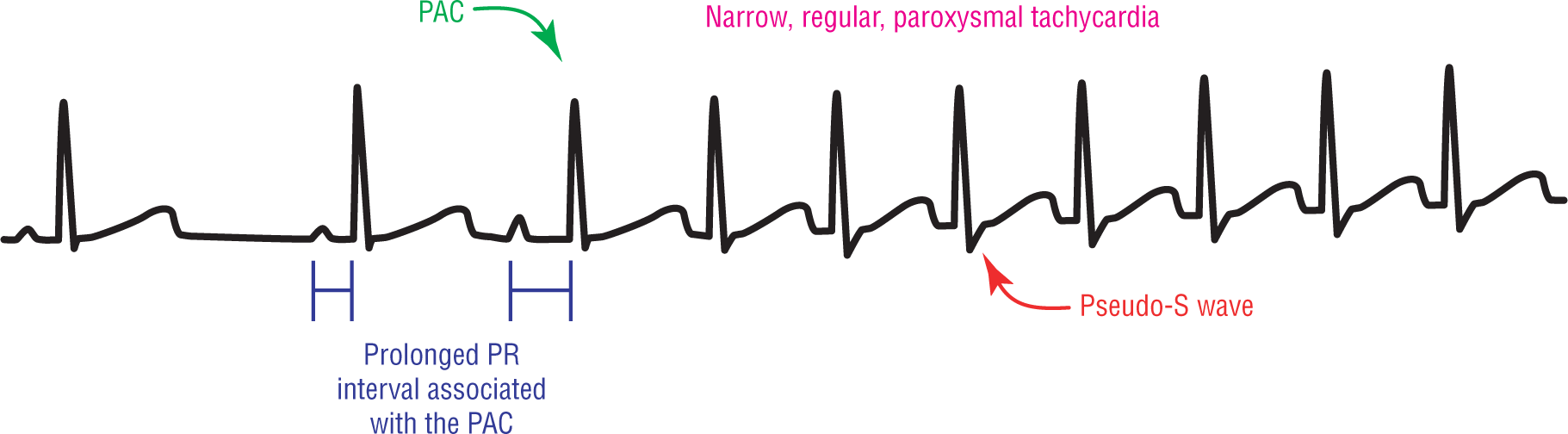
Figure 25-17 Findings in AV nodal reentry tachycardia.
© Jones & Bartlett Learning.
DescriptionThe rate criteria for AVNRT state that the rates should be between 150 and 250 beats per minute (BPM). As a side point, the most common rates seen clinically are actually in the 170- to 220-BPM zone (the midrange of the rate criteria). The P waves typically are buried within the QRS complex or are found immediately after the QRS complex. The P waves are rarely found in front of the QRS. The formation of pseudo-R' waves in lead V1 and pseudo-S waves in lead II is a common finding in AVNRT.
The QRS complexes are typically narrow complexes with a total QRS interval width of less than 0.12 seconds. Wider complexes are found when the patient has a preexisting bundle branch block, when the complexes are aberrantly conducted, and when there are significant electrolyte abnormalities. Care must be taken not to include the pseudo-R’ or pseudo-S wave interval in the calculation of the width of the QRS complex, as this causes a false widening of the QRS interval (Figure 25-18). Sometimes, an old strip or a section of sinus rhythm is needed to measure the true QRS interval. Other possible solutions include measuring the interval in a lead without the pseudo-waves or measuring the intervals once the rhythm is broken.
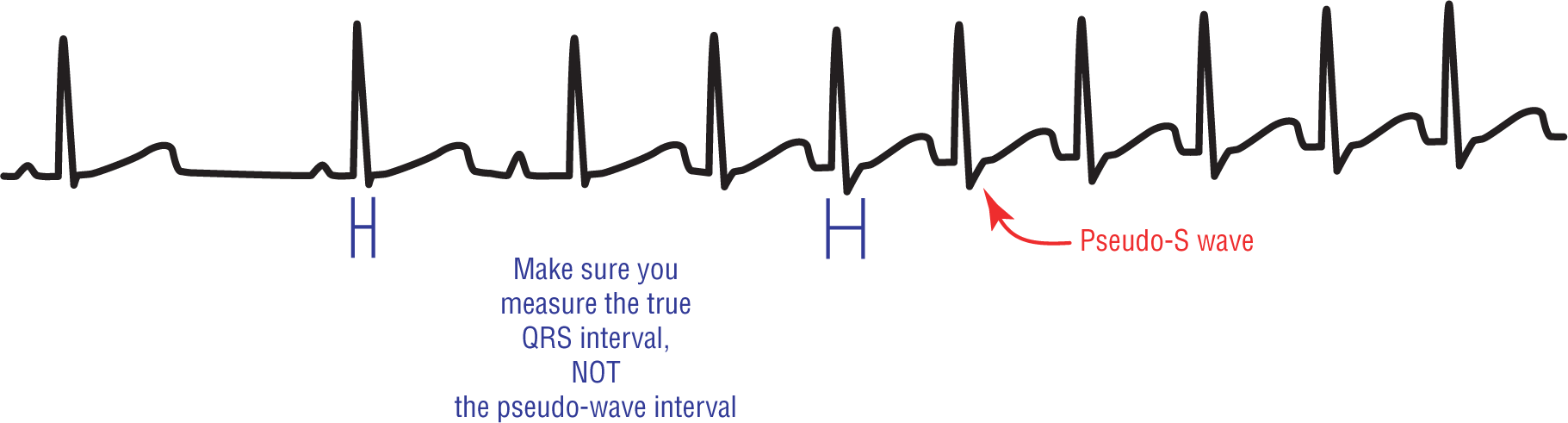
Figure 25-18 QRS interval in AVNRT. The thinner brackets are the true QRS interval. The wider brackets are the space being widened by the presence of a pseudo-S wave.
© Jones & Bartlett Learning.
DescriptionRemember when we first began discussing the anatomic importance of the fast and slow tracts fusing to form a common final pathway? We mentioned the importance of the fact that the looping of the impulses traveling down the tracts occurred before the AV node, and not inside of it. The presentation of only one impulse to the AV node for transmission allows the AV node to block fast rates for cardioprotection (for example because of a diseased or malfunctioning AV node), leading to 2:1, 3:1, or even variable conduction ratios. In other words, the two events (the circus movement formation and the AV blocks) could act independently of each other or could remain somewhat linked.
Additional Information
Atypical AVNRT
We have seen that the normal reentry loop occurs when the impulse enters the slow tract and then spreads retrogradely back via the fast tract. This is the most common type of AVNRT and is known as typical or common AVNRT. In addition to this type of AVNRT, there is also an uncommon or atypical form, which occurs in 5% to 10% of the cases. Atypical AVNRT occurs when the reentry loop is backward compared to the typical form. In the atypical form, the impulse enters the fast tract and then spreads retrogradely via the slow tract.
The big difference between these two types of AVNRT is the location of the P wave. The RP interval—the distance from the start of the QRS complex to the end of the P wave—is longer in the atypical form of AVNRT. This happens because the slow conduction time of the retrograde impulse through the slow tract, lengthens the total time to reach and spread through to the atria. In other words, slower conduction equals longer intervals (Figure 25-19).
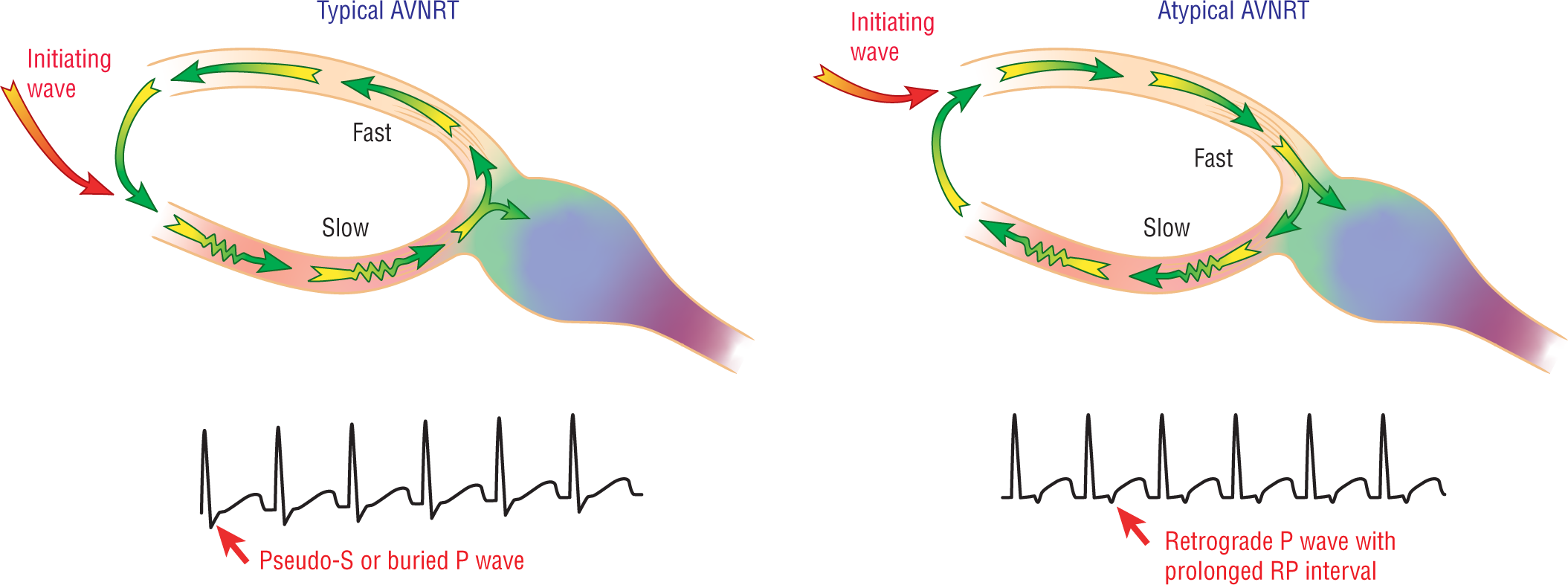
Figure 25-19 Typical and atypical AVNRT.
© Jones & Bartlett Learning.
DescriptionARRHYTHMIA RECOGNITION
AV Nodal Reentry Tachycardia
| Rate: | 150 to 250 BPM (ventricular) |
| Regularity: | Regular |
| P wave:
Morphology: Upright in II, III, and aVF: |
Inverted or buried
Inverted No |
| P:QRS ratio: | 1:1 (If P waves are present) |
| PR interval: | None or RP interval |
| QRS width: | Normal |
| Grouping: | None |
| Dropped beats: | None |
DIFFERENTIAL DIAGNOSIS
AV Nodal Reentry Tachycardia
AVNRT is caused because of the presence of a dual pathway approaching the AV junction. It is normally found in patients without other structural heart disease.