
Figure 28-6 Different types of conduction in a patient with Mobitz II second-degree AV block.
© Jones & Bartlett Learning.
DescriptionThe second-degree AV blocks are characterized by both the presence of P waves and intermittently dropped QRS complexes. Usually, there is only one dropped QRS complex for each grouping, but multiple dropped complexes can occasionally occur (especially in Mobitz II second-degree block). The nonconducted P waves occur because second-degree AV blocks work by an all-or-none kind of process. The conduction of the depolarization wave to the ventricles will either happen or it won’t. This is in sharp contrast to the simple delay that we saw when we looked at the first-degree AV blocks.
The dropped QRS complex in all types of second-degree AV blocks typically provides a natural barrier for the eye that gives the complexes the appearance of being grouped (Figure 28-6). In other words, the regular empty space created on the rhythm strip by the dropped QRS complex provides a natural break in the rhythm, which is very obvious to the naked eye. Since the dropped beats typically occur fairly frequently, the empty spaces make it look like the complexes come in groups. The presence of grouping is one of the major things that you need to look for when considering the possibility of a second-degree AV block.

Figure 28-6 Different types of conduction in a patient with Mobitz II second-degree AV block.
© Jones & Bartlett Learning.
DescriptionThere are two main types of second-degree AV block and two minor variations. The main types are known as Mobitz I second-degree AV block (also known as Wenckebach) and Mobitz II second-degree AV block. The differences between these two are related to the appearance of their PR intervals associated with the complexes and their most common sites of origin. The minor variations mentioned previously are the high-grade or advanced AV blocks and the 2:1 or untypable AV block, and we will discuss these separately.
Mobitz I Second-Degree AV Block or Wenckebach
Mobitz I second-degree AV block or Wenckebach is a very common rhythm abnormality that is usually clinically benign. It is characterized by the presence of P waves that appear with a progressive lengthening of their PR intervals until one of them fails to conduct. The process then typically begins all over again, with progressive lengthening of the PR interval until another QRS complex is dropped. The main criteria for the presence of a Mobitz I second-degree AV block are:
Additional Information
The Terminology of Conduction
When referring to the conduction ratios or sequences of the various groups in second-degree AV blocks, clinicians frequently use the words “conduction” and “block” interchangeably. This can lead to more confusion related to the word “block,” and can lead to some serious errors.
When we use the word conduction in discussing the conduction ratios in AV blocks, we refer to the ratio of P waves that conduct to the ventricles. For example, a 3:2 conduction means that in a grouping, there are three P waves, and two of those P waves conduct normally to create two QRS complexes. In other words, only one P wave has been blocked.
When we use the word block in reference to conduction ratios in groupings, we are comparing the number of P waves in the group and the number of P waves that have been blocked. For example, a 3:2 block means that for every three P waves, two get blocked and only one gets through to create a single QRS complex.
In order to avoid further problems with nomenclature, we suggest that you get used to using either “conduction” or “block” when referring to conduction ratios. We feel that “conduction” provides the maximal amount of information that is needed in clinical practice. In this text, the word “conduction” will be the terminology used exclusively.
The site where the block most commonly occurs is at the level of the AV node. However, in about a quarter of the cases, the block can occur below the AV nodes. The QRS complexes in Wenckebach are usually normal width unless there is a preexisting bundle branch block or there is aberrancy. An infra-Hisian site for the block may also be associated with a widening of the QRS complexes, although this is a rare occurrence.
1. PR interval progressively lengthens until a P wave is eventually blocked.
The Wenckebach phenomenon can occur with P waves that originate in either the sinus node, the ectopic atrial tissue, or the AV junction itself. In general, the P-P interval in Wenckebach is consistent, reflecting the cadence set by either the sinus node or the ectopic pacemaker.
In order for any second-degree AV block to develop, there needs to be a site of delay and eventually obstruction to the conduction of the supraventricular impulse to the ventricles. The delay and eventual obstruction occur as a result of any process that lengthens the refractory period and conduction rates of the obstructing site. For Wenckebach, this site is typically the AV node, but it can be anywhere along the electrical conduction system. For simplicity, we will limit this discussion to the AV node.
As the supraventricular impulses reach the AV node, the first complex after the pause finds the node normally or near normally ready to receive it (Figure 28-7). That first supraventricular impulse is conducted without difficulty because the node is set to receive it. As that first complex goes through, however, it leaves the node a little more refractory and a little less ready to receive the next impulse. This is reflected as a delay in transmitting the second impulse to the ventricles (Figure 28-8). In other words, the PR interval temporarily lengthens for this second complex.

Figure 28-7 This Figure represents three sinus waves that are approaching a slowly conducting or diseased AV node. In this figure, the wave labeled A reaches a rested, nonrefractory AV node. It easily makes it to the trigger zone and fires a ventricular depolarization wave.
© Jones & Bartlett Learning.

Figure 28-8 This Figure represents the second wave, labeled B, reaching a slower, more refractory AV node. Conduction is delayed and the PR interval appears to be prolonged. In this figure, the wave labeled B doesn’t penetrate the AV node as easily. It does, however, make it to the trigger zone and fires a ventricular depolarization wave.
© Jones & Bartlett Learning.
Now, as that second impulse goes through the node, it will in turn cause further refractoriness that will make the delay even longer for the third supraventricular impulse. This prolongs the PR interval even further during the third complex. This process of delay leading to further delay continues until, eventually, the refractoriness and delay in the AV node reach such a point that conduction completely fails (Figure 28-9). This will be represented on the ECG strip as a P wave with a dropped QRS complex. The time supplied by the blocked impulse allows the AV node to reset, and so the next P wave will begin the whole process all over again.
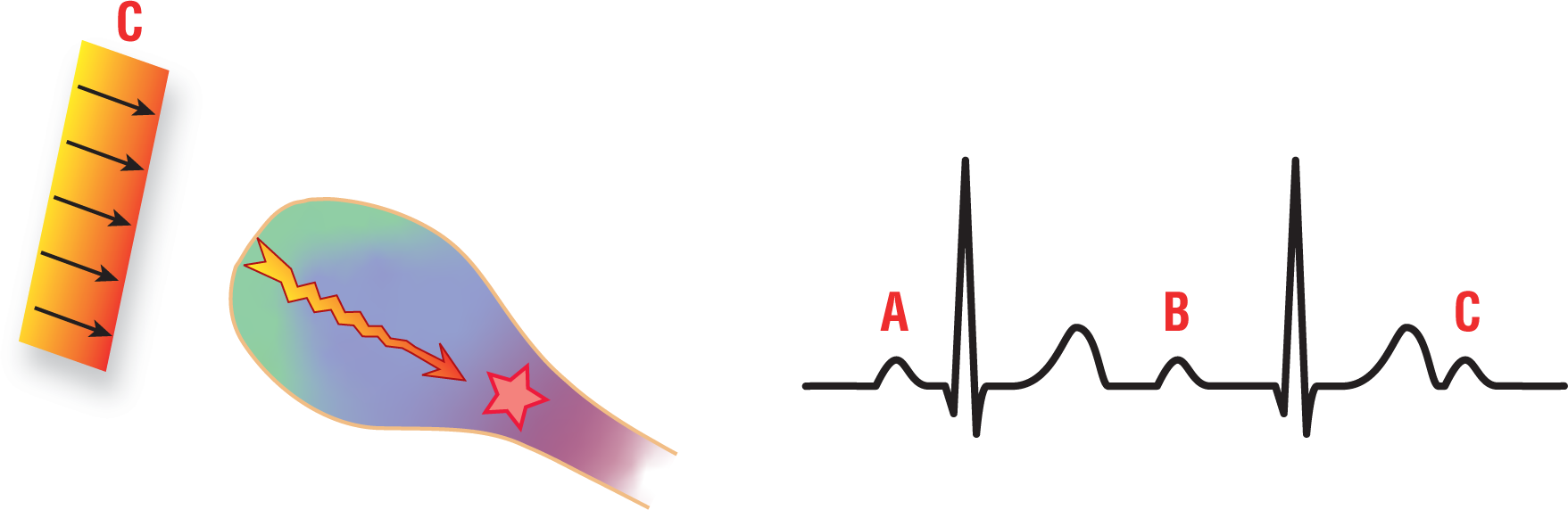
Figure 28-9 This Figure represents the third wave, labeled C, approaching the now very slowly conducting or heavily refractory AV node. In this figure, the wave labeled C hardly penetrates the AV node at all. It does not reach the trigger zone and does not fire a ventricular depolarization wave.
© Jones & Bartlett Learning.
This repeating cycle of delay and eventual block is what gives Wenckebach its grouped appearance. The groupings can occur at many different conduction ratios. The groupings are, however, always found in a ratio of N:(N − 1). In other words, there will always be one less QRS complex than there are P waves. Examples of possible conduction ratios include 2:1, 3:2, 4:3, 5:4, . . . 10:9, . . . 17:16, . . . and so forth. The conduction ratios can also be variable within the same patient. Figure 28-10 shows some typical Mobitz II second-degree AV block conduction ratios.
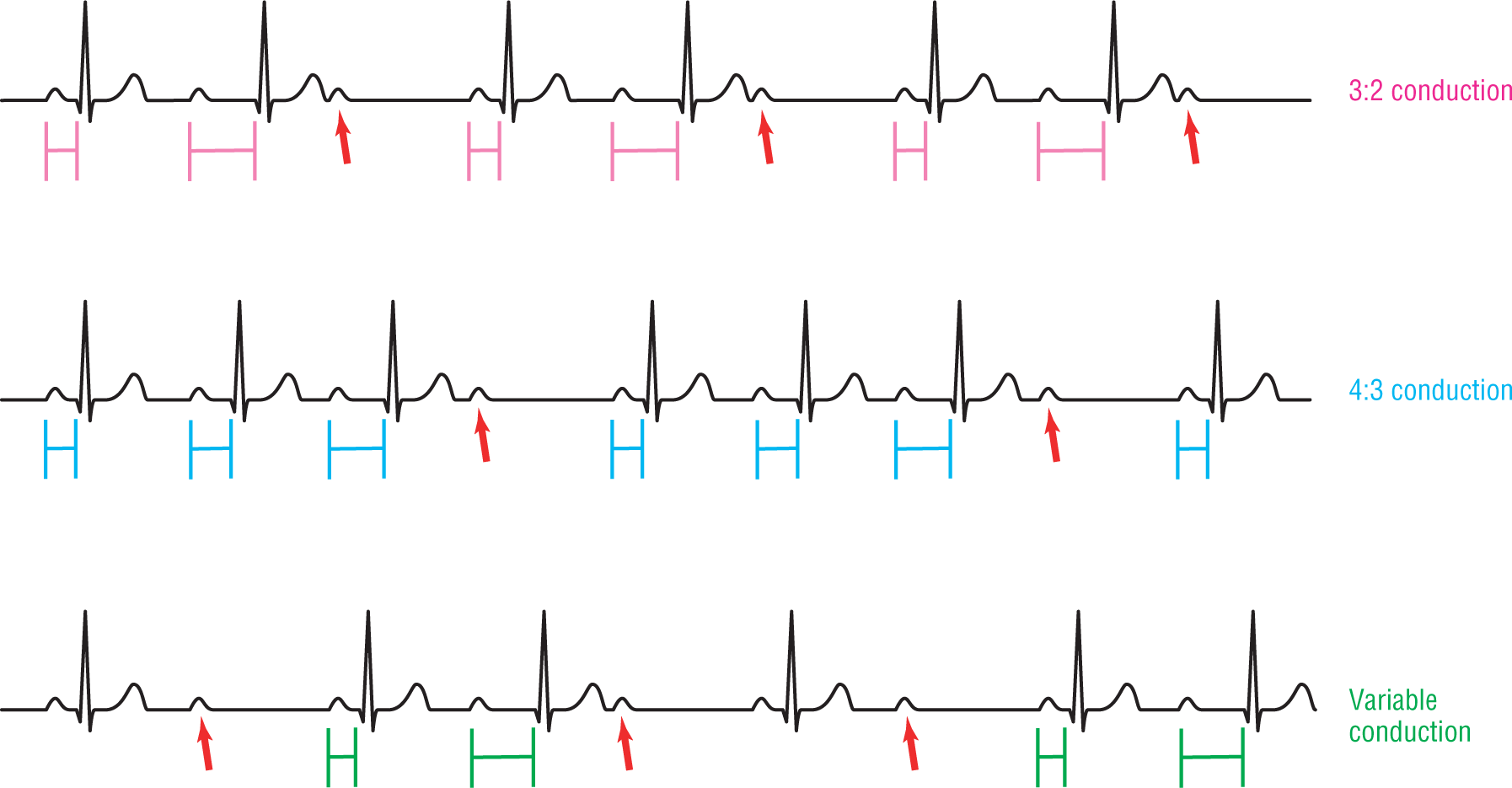
Figure 28-10 Different types of conduction in a patient with Mobitz I second-degree AV block. Note the progressive prolongation of the PR interval until one P wave fails to conduct (red arrows).
© Jones & Bartlett Learning.
a. The shortest PR interval is the one immediately following the dropped beat. As you saw from the previous discussion, the AV node is best able to receive a new impulse immediately after the dropped beat. This is because during the pause, the AV node had time to lose its refractoriness and to build up enough steam to conduct normally. Basically, the AV node can conduct this first P wave with minimal, if any, variation in the PR interval. Therefore, the first PR interval in any one group (the one that occurs immediately after the dropped beat) is always the shortest (Figure 28-11).
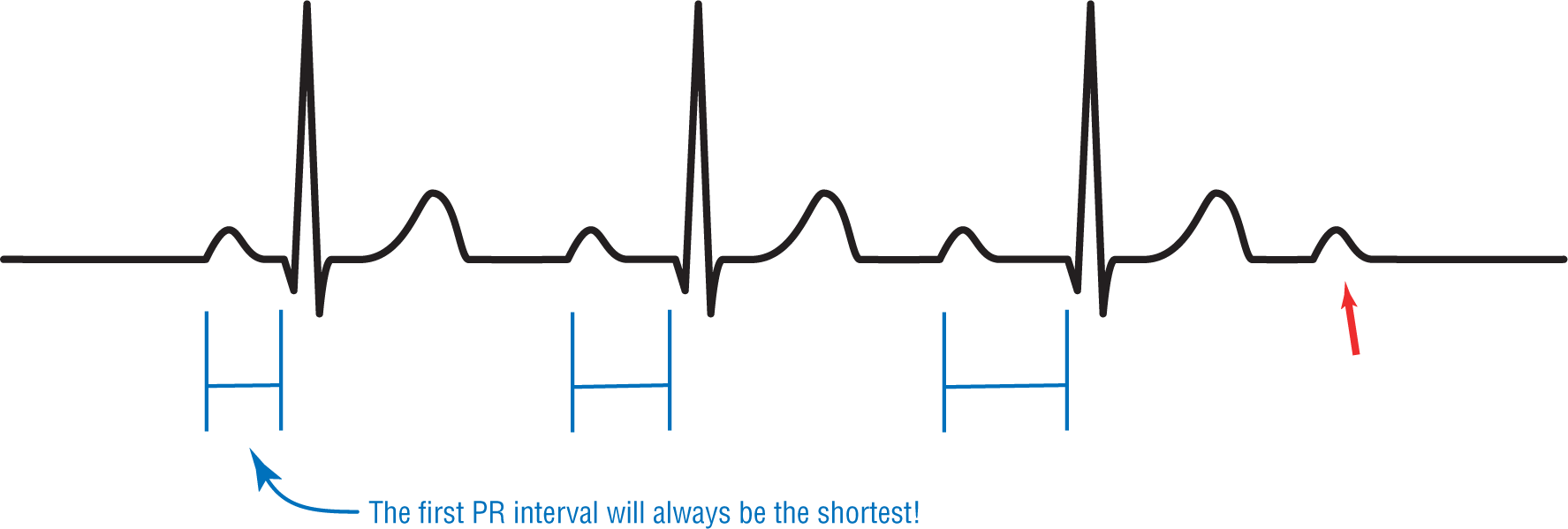
Figure 28-11 The shortest PR interval is always the first one after the dropped beat.
© Jones & Bartlett Learning.
b. The longest PR interval is the one immediately before the dropped beat. As we mentioned before, conduction through the electrical conduction system is an all-or-none phenomenon. Conduction will either occur or be blocked. Going back to our discussion on how the PR intervals become prolonged, we see that with every passing P wave, the PR interval lengthens as the AV node becomes more and more unable to transmit the impulse. Eventually, the delay becomes so great that the impulse fails to conduct to the ventricles. That last, nonconducted P wave does not have a PR interval at all. Therefore, the longest PR interval has to belong to the last P wave that was conducted and has a QRS wave. That lucky P wave reached the AV node before it completely gave out. It is the one with the maximal amount of delay but still conducted. That P wave gives rise to the last PR interval in a group (Figure 28-12).
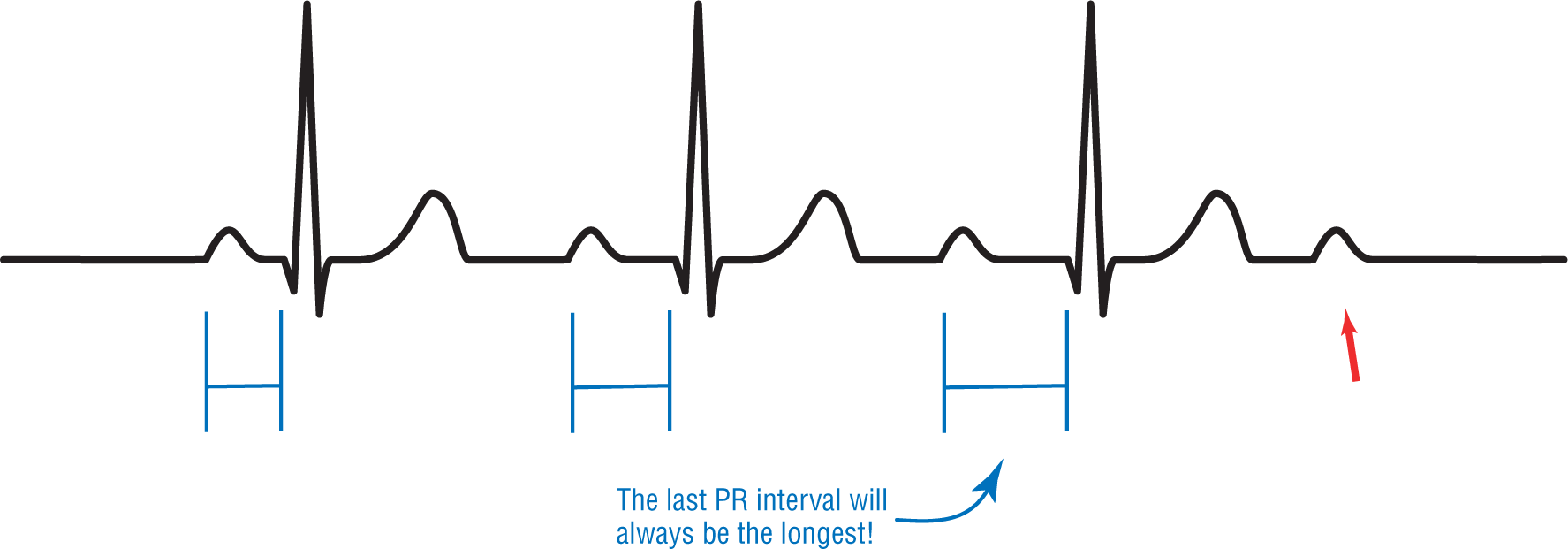
Figure 28-12 The longest PR interval is always the one right before the dropped P wave.
© Jones & Bartlett Learning.
So far, we have seen that Wenckebach or Mobitz I second-degree AV block is associated with a progressive prolongation of the PR interval until a P wave gets completely blocked. We have seen that the shortest PR interval is the first one in the grouping, and that the longest PR interval is the last one in a grouping. Now, we need to take a closer look at what happens in between the first and last PR intervals.
c. The largest incremental change in the PR interval occurs between the first and second PR intervals. We know that the first PR interval in a grouping is always the shortest. The next big diagnostic criterion that we are going to examine is that the largest incremental change in the PR interval occurs between the first and the second PR intervals (Figure 28-13).
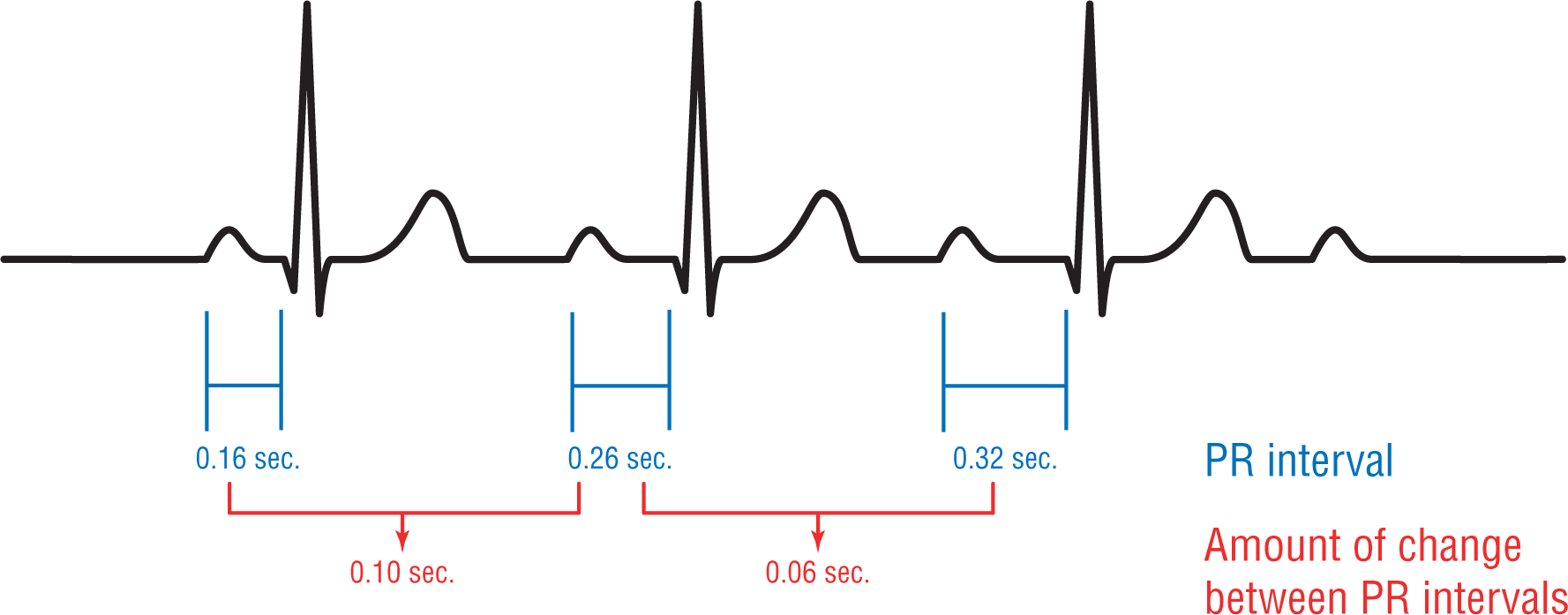
Figure 28-13 The biggest incremental change in the PR intervals occurs between the first and second PR intervals. In this example, the difference between the first and second PR intervals is 0.10 seconds. The difference between the second and third PR intervals is 0.06 seconds.
© Jones & Bartlett Learning.
Going back to our original progressive PR interval discussion, we see that right before the first P wave reaches the AV node, it is at its maximal amount of conductive potential. When the first P wave is conducted, the AV node remains somewhat refractory. This refractoriness leads to a delay in the conduction of the second P wave. The difference between maximal conductivity of the first P wave and the subsequent delay in the conduction of the second P wave signifies the largest amount of total change in conductivity in any one group.
Additional Information
Atypical Wenckebach or Mobitz I Second-Degree AV Block
What happens if you have a really long conduction group with Wenckebach, say 10:9? Does the progressive prolongation of the PR intervals and the amount of change between them continue throughout the strip? The answer is no. Eventually, the amount of change in the PR intervals becomes zero, if the strip is long enough before the dropped beat. What probably happens is that, after a while, the amount of delay continues to increase but at electrocardiographically unmeasureable amounts until the all-or-none phenomenon fails to conduct a P wave. This type of conduction defect is known as atypical Wenckebach or atypical Mobitz I second-degree AV block (Figure 28-14).

Figure 28-14 Atypical Wenckebach.
© Jones & Bartlett Learning.
DescriptionIn atypical Wenckebach, the first PR interval is still the shortest. The longest PR interval is still the last one. Finally, the largest amount of incremental change between the PR intervals is still between the first and second ones. The only difference is that the PR intervals do not continue to widen indefinitely. This can sometimes make the diagnosis of the AV block difficult. Always look closely at the interval with the dropped beat. If the PR interval before the dropped P wave is longer than the one immediately after the pause, you are probably dealing with an atypical Wenckebach.
The amount of additional delay that is added to each successive PR interval in a group is small in comparison to the delay between the first and second complexes. As you can see from Figure 28-13, the amount of prolongation seen between the subsequent PR intervals is smaller than between the first two.
2. The R-R intervals progressively shorten until a QRS complex is dropped.
In Wenckebach, the R-R interval shortens progressively between each QRS complex. This is because the incremental change in the delay caused by the progressing PR interval becomes shorter.
The previous comments are counterintuitive until you really break it down by looking at a strip. Take a look at Figure 28-15. In this figure, you see that the P-P interval is a value of X seconds. Under normal circumstances, the P-P intervals and the R-R interval should be the same value. But, in Wenckebach we need to add the amount of incremental change caused by the PR interval getting longer (the delay) to the normal P-P interval of X in order to get the measurement of that R-R interval. In the case of the first two complexes, the value of the true R-R interval as X + 0.08 seconds. Using the same logic, the next R-R interval would now be X + 0.04 seconds. Notice that this is shorter than the first one. As you can see, as the incremental change between the PR intervals gets shorter, the R-R intervals have got to get shorter as well. This continues to occur until the dropped P wave, then the cycle begins all over again in the next group.

Figure 28-15 Decreasing R-R interval.
© Jones & Bartlett Learning.
DescriptionDon’t spend a lot of time trying to understand the math and why this occurs. Instead, just remember that the R-R intervals shorten between each complex in a group. This fact comes in handy in some tough diagnostic cases.
3. The interval including the blocked P wave is less than the sum of two P-P intervals.
The interval that includes the pause has got to be shorter than the sum of two P-P intervals (Figure 28-16). Why? Well, in a Mobitz I second-degree AV block, the P-P intervals are consistent; what is actually changing is the R-R interval. We mentioned that the shortest PR interval in a grouping is the first one. Therefore, it makes sense that the interval containing the narrowest PR interval would have to have its associated R waves the closest.
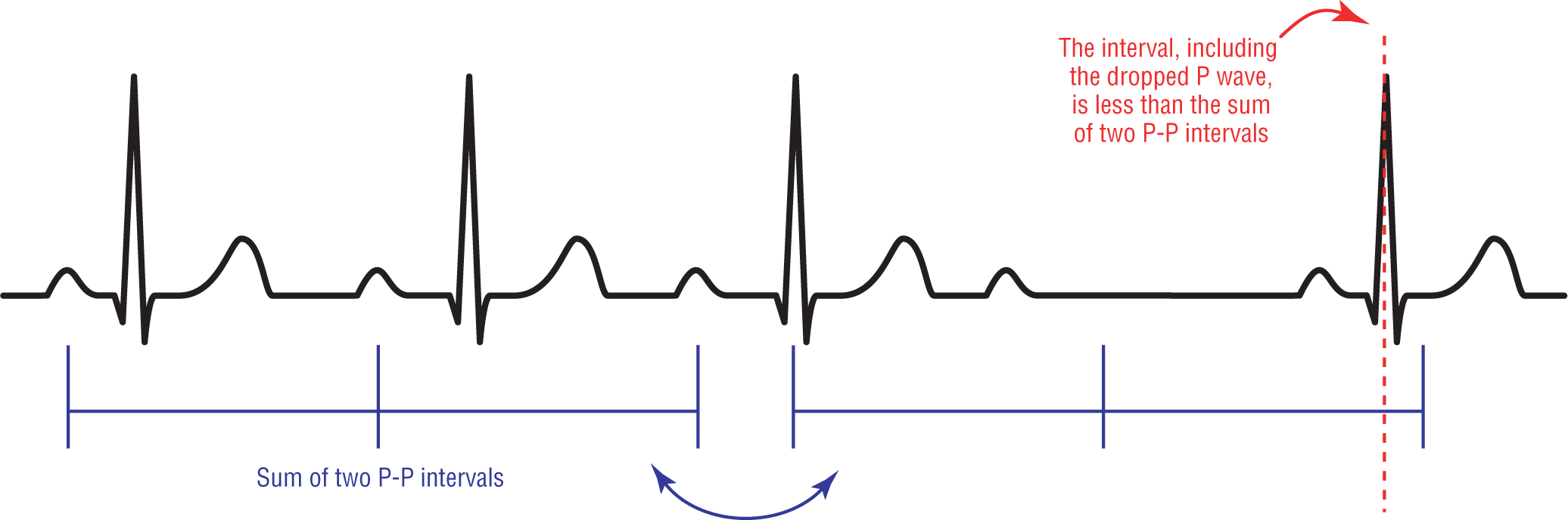
Figure 28-16 The distance of the pause.
© Jones & Bartlett Learning.
Mobitz I Second-Degree AV Block: A Final Word
Diagnosing Wenckebach or Mobitz I second-degree AV block is simple when the conduction ratios are 3:2 or 4:3. However, the longer conduction ratios make diagnosis more difficult. Atypical presentations abound that could easily throw you off track. The key is to note the progressive PR prolongation and the eventual dropped beat. A strip that only shows you progressive prolongation of the PR interval should steer you in the right direction, and you should think about getting a longer strip. The longer strip may show the dropped P wave and the typical changes seen around the pause.
The pause is the area of any strip where the changes of Wenckebach will be the most obvious. There you will see the longest PR interval in the beat before the dropped P. There you will see that the shortest PR interval will be the first PR interval in a group. There you will see that the largest incremental change in the PR intervals occurs between the first and second conducted complexes. Above all, remember that if you don’t think about the possibility, you will never make the diagnosis.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
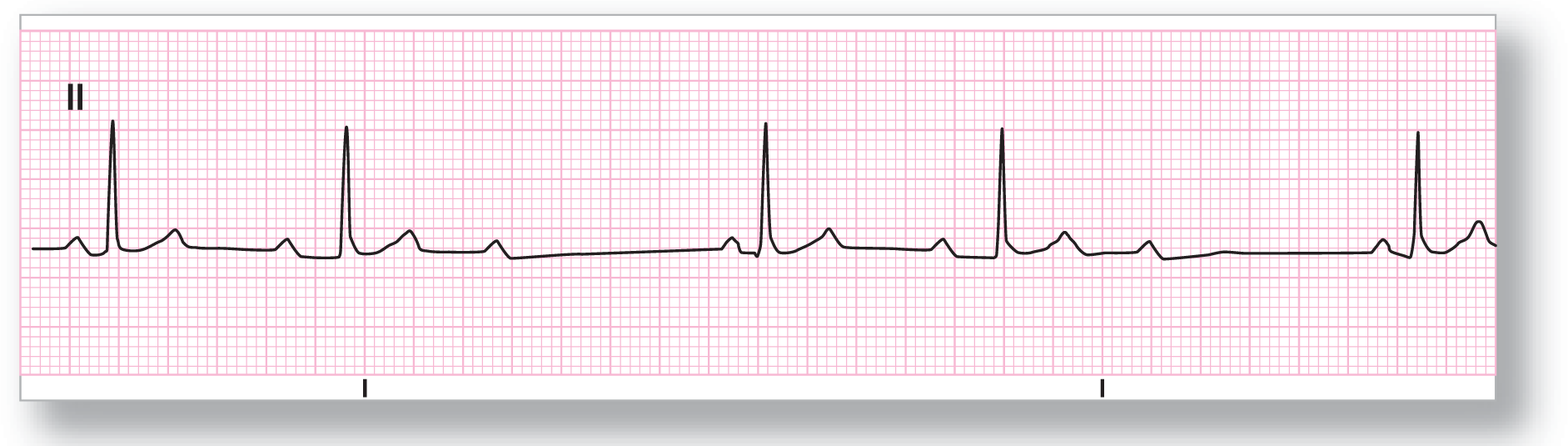
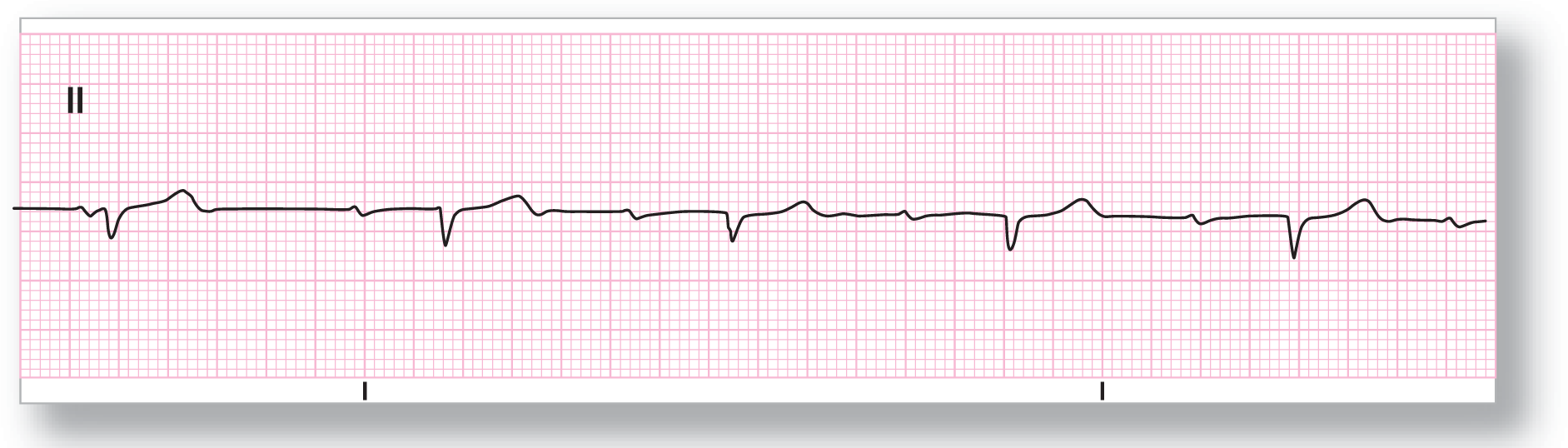
Rate: About 40 to 50 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 3:2 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
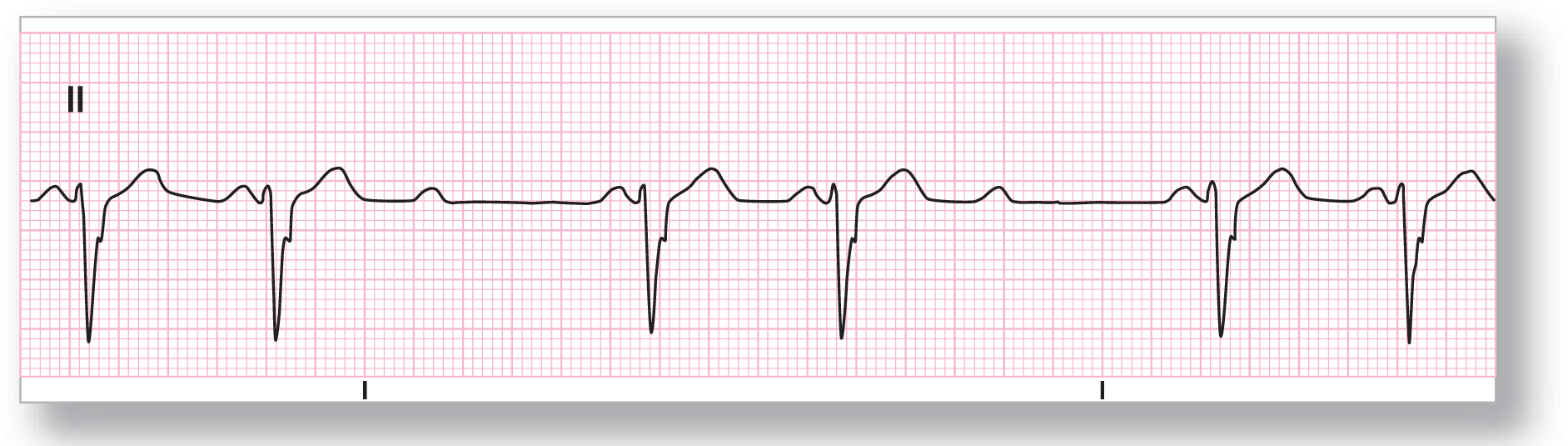
ECG 28-6 shows a grouped rhythm with a conduction ratio of 3:2. There is progressive widening of the PR interval between the first and second complexes and then there is a dropped P wave. The cycle then begins all over again in a recurrent pattern. This has all the earmarks of a Mobitz I second-degree AV block. Note that you cannot make a comment about shortening R-R intervals in this case because there is only one R-R interval per group.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 40 to 50 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Inverted Axis: Abnormal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 2:1 and 3:2 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
This patient starts off with two groupings that are conducted at a ratio of 2:1 (ECG 28-7). After these two groupings, we see a grouping that is made up of three P waves and two QRS complexes with progressive PR interval widening and then a dropped P wave. This is consistent with a Wenckebach or Mobitz I second-degree AV block. Note that the P waves are ectopic in nature as indicated by their inverted morphology in lead II. The QRS complexes are narrow and obviously supraventricular.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
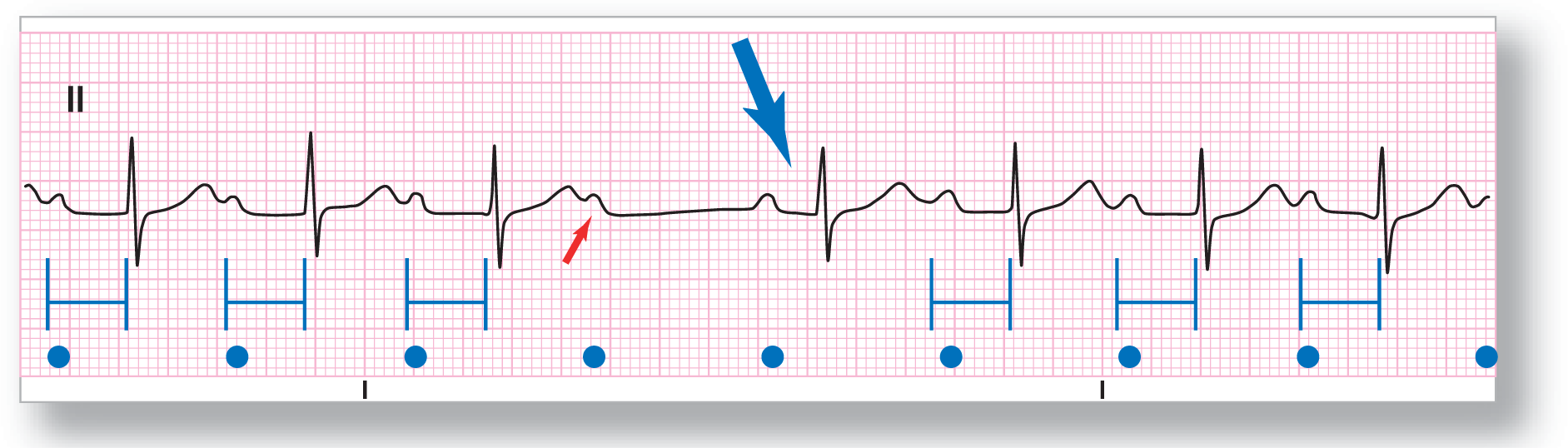
Description|
Rate: About 50 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 4:3 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
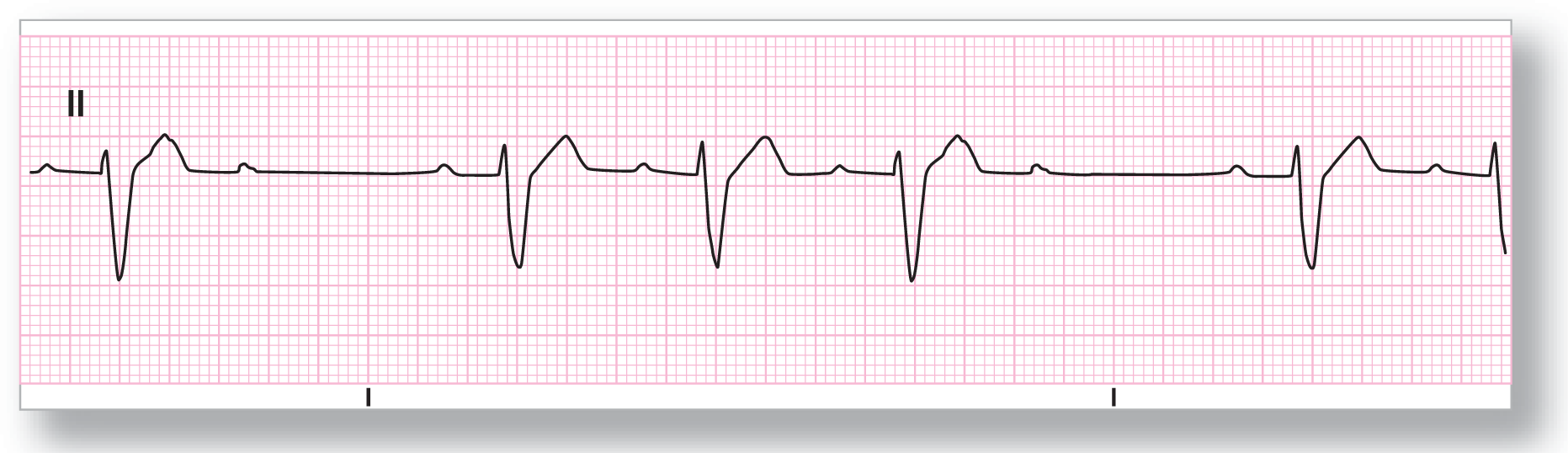
In ECG 28-8, we definitely see grouping, which would be clearer if we had a longer strip. The PR intervals progressively lengthen until there is a pause. The blocked P is not visible because it is buried in the T wave of the last complex (blue arrow). The incremental amount of the delay is definitely shorter between the second and third complexes than between the first and second complexes. However, since the third P is partially buried, the true measurement cannot be determined accurately.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
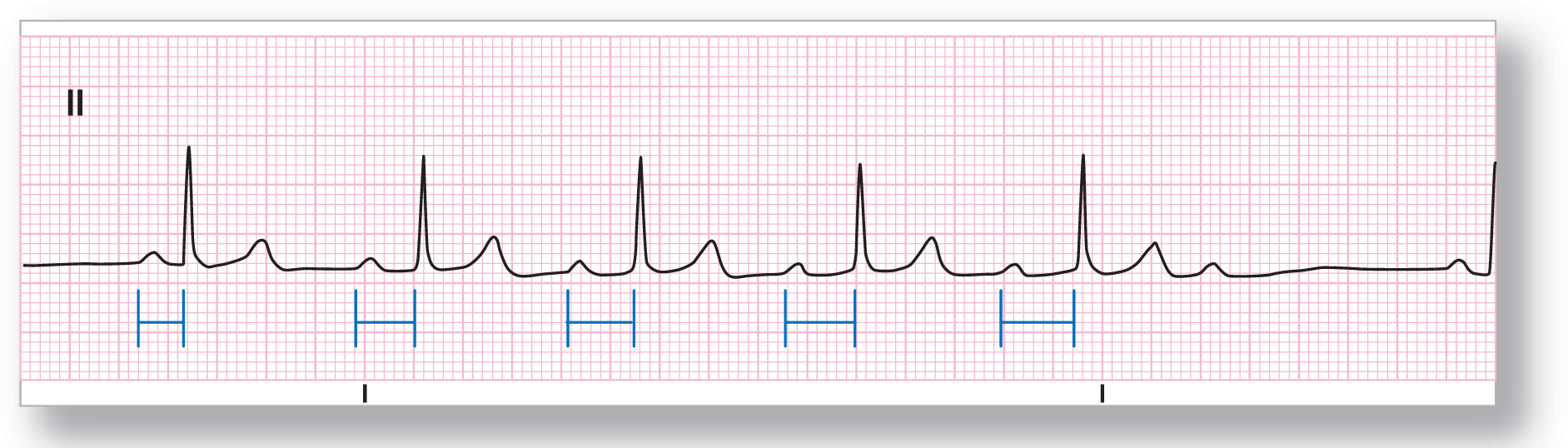
|
Rate: About 60 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 6:5 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
ECG 28-9 is classic for Wenckebach or Mobitz I second-degree AV block. We see a pause at the start and then a normal PR interval. The PR then begins to lengthen progressively throughout the rest of the group. Finally, the group terminates with a blocked P wave. The R-R interval shortens at the beginning of the group and then the shortening levels out, which is a bit atypical. The pause is less than the sum of two P-P intervals.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 50 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Normal Morphology: Biphasic Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 6:5 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
ECG 28-10 shows a partial grouping of a very long rhythm strip. The original, longer rhythm strip showed recurrent groupings that were identical to this strip. Nonetheless, this strip has many of the earmarks of Mobitz I second-degree AV block. The PR progressively widens throughout the group, while the subsequent incremental changes are minimal, which is a normal occurrence in longer strips. The incremental change in PR intervals is quite dramatic between the first one and the second one in the group, while the subsequent incremental changes are minimal, which is a normal occurrence in longer strips.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 90 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 4:3 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
ECG 28-11 also shows the classic changes for a Wenckebach or Mobitz I second-degree AV block. The PR interval starts off a bit prolonged and then continues to progressively increase throughout the strip. The groups end with a nonconducted P wave. Notice that the R-R intervals do not shorten on this strip, which is an atypical finding. The incremental change in the PR intervals is the largest between the first and second complex, as you would expect.
Mobitz II Second-Degree AV Block
Mobitz II second-degree AV block is a very simple rhythm to understand and identify compared with Mobitz I or Wenckebach. However, don’t let its simplicity fool you. The mechanisms behind a Mobitz II block are much more life-threatening, and misdiagnosis can be lethal.
Simply stated, Mobitz II second-degree AV block is diagnosed when you have either a single or multiple nonconducted P waves in the face of a rhythm with constant PR intervals (Figure 28-17). The PR interval can be either normal or prolonged, just as long as it is constant before the pause and constant after the pause. The P-P intervals are constant throughout the strip and the pause is exactly equal to two.

Figure 28-17 Mobitz II second-degree AV block.
© Jones & Bartlett Learning.
If you think about it, Mobitz II is the epitome of the all-or-none response. Almost all of the P waves will conduct normally. There is no delay associated with the P waves that are conducted. Occasionally, however, a P wave will simply fail to conduct.
In order to diagnose Mobitz II, you need to have at least two consecutive conducted P waves. This is important to be able to establish the consistency of the PR intervals. That said, the PR interval immediately after the pause may show some narrowing compared to the others (Figure 28-18). This can sometimes happen because of increased conduction through a well-rested conduction system. (This can sometimes lead to confusion and misdiagnosing the strip as a Mobitz I or Wenckebach.)
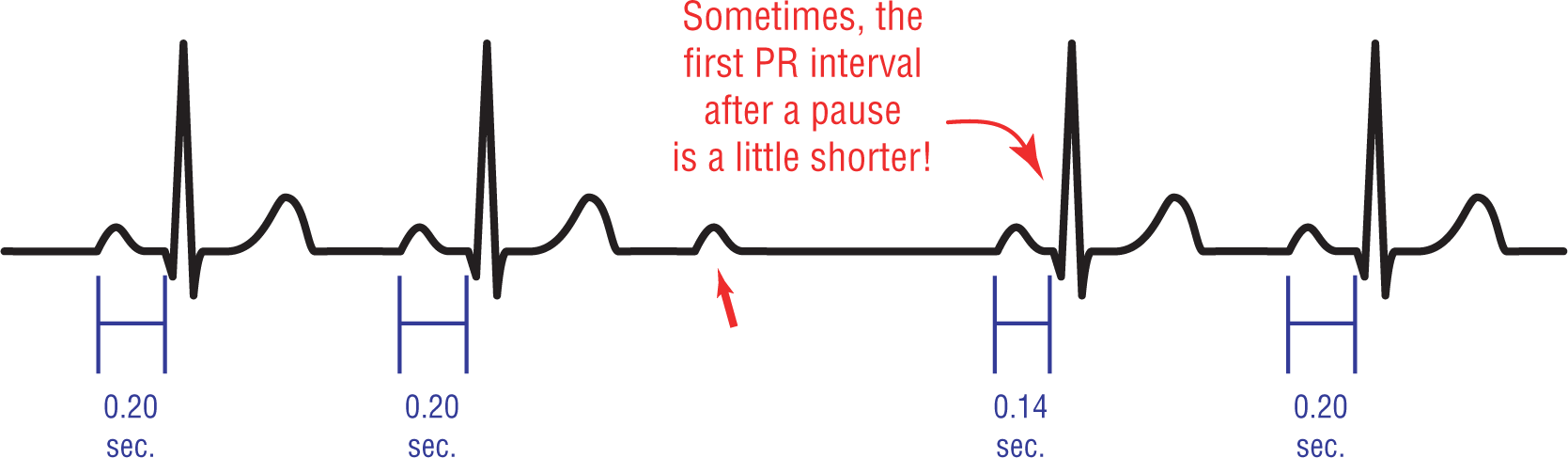
Figure 28-18 The first PR interval after a pause in Mobitz II second-degree AV block may be shorter.
© Jones & Bartlett Learning.
DescriptionThe conduction ratios of the Ps and QRSs can also vary in Mobitz II, just as they did in Mobitz I. Figure 28-19 is a graphical representation of various conduction ratios. The conduction ratios can also vary within the same patient at any one time.

Figure 28-19 Different types of conduction in a patient with Mobitz II second-degree AV block.
© Jones & Bartlett Learning.
DescriptionNotice in the strips that we have shown you so far of Mobitz II, all of the QRS complexes have been narrow. In Mobitz II, the QRS complexes can either be narrow or wide, depending on the location of the conduction block. If the block is in the AV node or in the bundle of His, the QRS complexes will be narrow. If the conduction block occurs below the bifurcation of the bundle of His, the QRS complexes will be wide.
The most common site for the conduction block in Mobitz II second-degree AV block is in the bundle branches. It is found there about 80% of the time. In the remaining 20% of the cases, the block occurs in the bundle of His. Mobitz II rarely occurs in the AV node. From these statistics we can say that, typically, the QRS complexes in Mobitz II will be wide.
The location of the conduction defect is also what makes these blocks so uncommon and so dangerous. Mobitz II is much less commonly found than Mobitz I. When it is found, it is indicative of fairly advanced conduction system disease. As a matter of fact, many of these patients have concomitant bundle branch blocks.
Clinically, Mobitz II is a permanent conduction defect and shows a great tendency to progress to higher degrees of block. Often it progresses to complete block.
Basically, that’s it. Diagnosing Mobitz II is fairly easy, and there are no variations except for an occasional narrowing of the first PR interval. When you do find it, be careful! Always have a pacemaker handy, because you are probably going to need it. This is especially true if the patient is having active ischemia or infarction.
Additional Information
Mobitz II vs. Blocked Premature Atrial Contraction (PAC)
There is one diagnostic problem that we would like to bring to your attention as we finish up Mobitz II second-degree AV block. Frequently, PACs are blocked from depolarizing the ventricles for whatever reason. The net result is that the P wave will be visible, but the QRS complex will not be. This resembles a Mobitz II block at first glance.
Close examination, however, will make a blocked PAC evident. First of all, a blocked PAC is still premature. The prematurity of the P wave of the PAC will be in stark contrast to the metronome regularity of the P waves in Mobitz II block. Remember, the P-P interval in Mobitz II is very, very regular. If you see a prematurely occurring P wave that is blocked, it should raise the suspicion of a blocked P wave from a PAC firmly in your mind.
Secondly, the morphology of the P wave in the PAC will be different from that of the rest of the complexes in the rhythm (Figure 28-20). In both Mobitz I and II, the morphology of ALL of the P waves are identical.
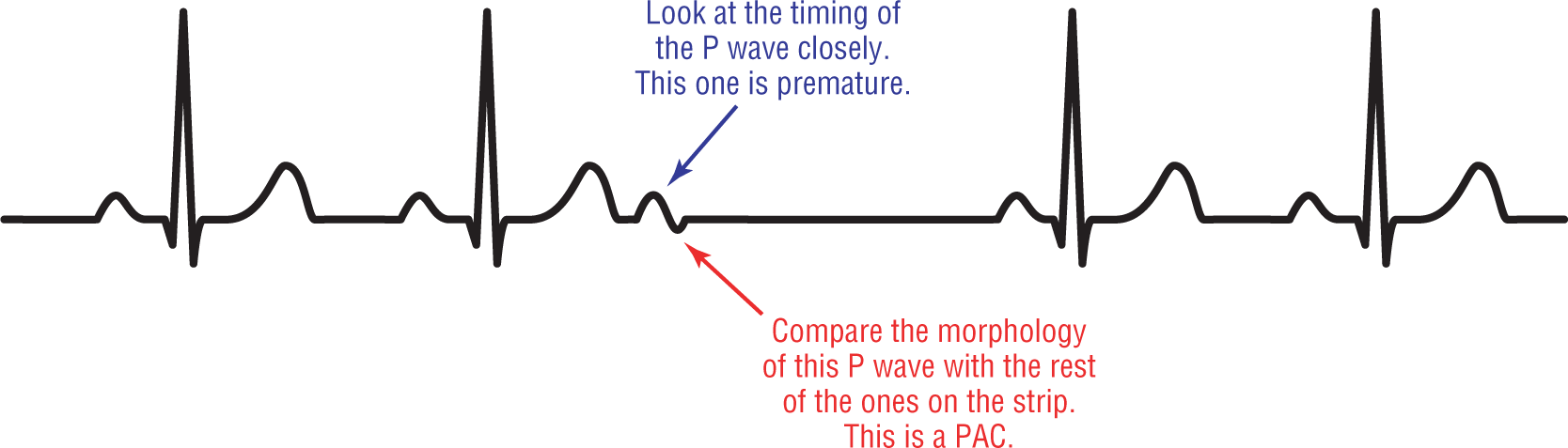
Figure 28-20 Blocked premature atrial contraction.
© Jones & Bartlett Learning.
Description
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 70 BPM |
PR intervals: Prolonged |
|
Regularity: Regularly irregular |
QRS width: Narrow |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Not present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 1:1 with one dropped beat |
Rhythm: Mobitz II second-degree AV block |
Discussion:
ECG 28-12 shows a long strip of complexes with prolonged but constant PR intervals. In the middle of the strip, there is a blocked P wave (red arrow). The blue arrow points out the first PR interval after the pause. Notice that this PR interval is a bit narrower than the others, which occurs occasionally in Mobitz II blocks. The second PR interval after the pause already is back to the constant PR interval found throughout the strip.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 60 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregularly |
QRS width: Wide |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 3:2 |
Rhythm: Mobitz II second-degree AV block |
Discussion:
ECG 28-13 shows a wide-complex regularly irregular rhythm with grouping. The groups are conducted in a ratio of 3:2. The important thing to note about the groups is that the PR interval remains constant throughout the strip. The P-P intervals are constant throughout, as you would expect in a Mobitz II block.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 50 BPM |
PR intervals: Constant |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 3:2 and 2:1 |
Rhythm: Mobitz II second-degree AV block |
Discussion:
ECG 28-14 shows a patient who is transiently wandering between 3:2 conduction to 2:1 conduction. Whenever you have an obvious Mobitz II second-degree AV block in any section of the strip and then you have an area of 2:1 conduction, the 2:1 block is assumed to be Mobitz II second-degree as well. The QRS complexes show a wide-complex morphology that is consistent with right bundle branch block in lead V1.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 55 BPM |
PR intervals: Constant |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 4:3 |
Rhythm: Mobitz II second-degree AV block |
Discussion:
ECG 28-15 shows a regularly irregular rhythm with dropped beats. The PR intervals are constant throughout the strip, and so are the P-P intervals. This is consistent with a Mobitz II second-degree AV block. The grouping that usually occurs in any second-degree AV block would be readily apparent if you had a longer strip. The QRS complex is wide and consistent with a left bundle branch block in this patient. Bundle branch blocks are often associated with Mobitz II.
Untypable or 2:1 Second-Degree AV Block
Take a look at Figure 28-21. What rhythm is it? Well, it could be a Mobitz I second-degree AV block being conducted at a 2:1 ratio. You don’t see the prolongation of the PR interval because the second P wave is the blocked P wave. But, it could also be Mobitz II second-degree AV block being conducted at a 2:1 ratio. If that were the case, you would have constant PR intervals. Once again, you could not see the constant PR intervals because the second P wave is the blocked P wave. As you can see, both possibilities could be right, and you have no way of telling.

Figure 28-21 It is unclear which type of block this strip represents.
© Jones & Bartlett Learning.
The answer is that this strip shows a 2:1 or untypable second-degree AV block. There is definitely evidence of a second-degree AV block, but you just don’t know which one. Why? Because in order to make the diagnosis of either Mobitz I or Mobitz II, you need to have at least two consecutive P waves that are conducted to the ventricles. This will allow you to establish the relationship of the PR intervals, and whether they are lengthening or staying constant. At a ratio of 2:1, you only have one conducted P wave in a group and there is no way of evaluating the relationship to the next PR interval. Since you can’t make the diagnosis, the block is simply called untypable. More commonly, the term 2:1 block is used and the lack of specificity is presumed to be understood.
However, that said, if you have a long enough rhythm strip or if you happen to be lucky enough to capture the first time a longer series occurs, you can state the type of second-degree block with a fair degree of certainty. That is because if you see a Mobitz I pattern anywhere, you can assume the complexes that are being conducted at 2:1 are also Wenckebach (Figure 28-22). Likewise, if you see a Mobitz II pattern anywhere, you can assume the complexes that are being conducted at 2:1 are Mobitz II. Remember, always look at “the company it keeps” and you will be able to make the diagnosis.

Figure 28-22 Mobitz I and Mobitz II 2:1 second-degree AV block.
© Jones & Bartlett Learning.
Description

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 42 BPM |
PR intervals: Prolonged |
|
Regularity: Regular |
QRS width: Narrow |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 2:1 |
Rhythm: 2:1 or untypable second-degree AV block |
Discussion:
ECG 28-16 was taken from a patient with a long episode of 2:1 block. There were never any obvious segments of either Mobitz I or Mobitz II. Since you cannot tell which of them it was, the rhythm is simply labeled 2:1 or untypable second-degree AV block. The prolonged PR interval does favor the diagnosis of Mobitz II, but this is not enough to make the call.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 35 BPM |
PR intervals: Constant |
|
Regularity: Regular |
QRS width: Narrow |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 2:1 |
Rhythm: 2:1 or untypable second-degree AV block |
Discussion:
ECG 28-17 shows a strip with 2:1 block and a ventricular rate of 35 BPM. The PR interval is normal and consistent when it conducts. This could be compatible with either Mobitz I or Mobitz II. Based on this strip, the diagnosis can only be 2:1 AV block.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 45 BPM |
PR intervals: Prolonged, constant |
|
Regularity: Regular |
QRS width: Narrow |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 2:1 |
Rhythm: 2:1 or untypable second-degree AV block |
Discussion:
ECG 28-18 shows another example of a typical 2:1 or untypable AV block. Even though you cannot officially make the call, there are a few things in this strip that favor Mobitz II. The prolonged PR interval is indicative of AV nodal dysfunction. In addition, the flat ST-segment elevation could easily represent an evolving inferior wall myocardial infarction (MI). A full 12-lead ECG is indicated for evaluation of a possible MI. A longer rhythm strip may resolve the issue of this block being either a Mobitz I or II.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 40 BPM |
PR intervals: Prolonged, constant |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: Present |
|
Dropped beats: Present |
|
|
P:QRS ratio: 2:1 |
Rhythm: 2:1 or untypable second-degree AV block |
Discussion:
Once again, you cannot make a decision on the type of second-degree AV block that this patient is experiencing based on ECG 28-19. Also once again, the presence of prolonged PR intervals and wide QRS complexes favor a Mobitz II block, but you simply cannot tell with any certainty. That is why the official diagnosis of the rhythm is 2:1 or untypable second-degree AV block.
High-Grade or Advanced AV Block
High-grade or advanced AV block is the term used to describe a conduction block that is somewhere between second-degree AV block and complete AV block. In order to meet the criteria for this type of block, at least two consecutive P waves need to be blocked due to an underlying conduction defect. Let’s look at these criteria a bit closer.
Figure 28-23 shows a typical example of a high-grade or advanced AV block. Note that the conduction ratio is roughly 3:1 (one P wave is buried in the T wave). This means that at least two consecutive P waves were blocked before the third one finally was conducted to the ventricles. The number of P waves that have to be blocked has to be two or greater in order to meet the criteria for this type of block. This is in comparison to Mobitz I or Mobitz II, which need only one P wave to be blocked.
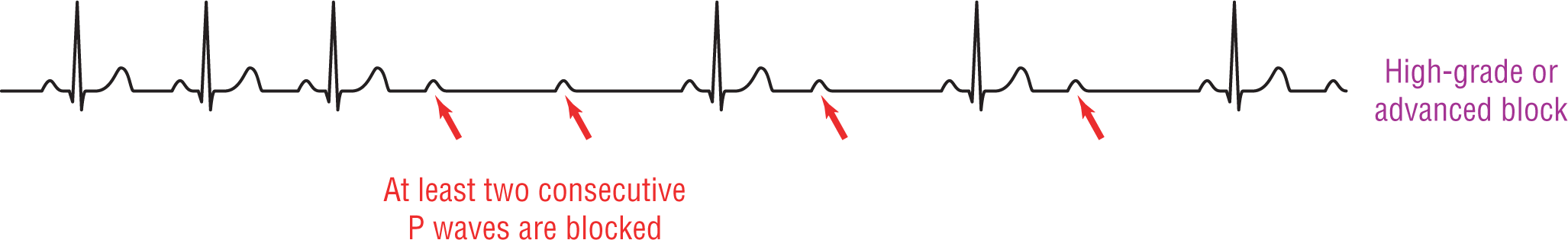
Figure 28-23 High-grade or advanced AV block.
© Jones & Bartlett Learning.
The second criterion is that the block has to be due to an underlying conduction defect and not simply be a normal physiologic response or block to a very rapid atrial rate. Let’s take for example a rapid atrial flutter that is stimulating the atria at about 300 BPM. The constant bombardment of the AV node by such a rapid rate will often cause a physiologic block to develop due to refractoriness of the node in either a 2:1, 3:1, or higher ratio. In this case, the block is not due to an underlying conduction defect but is a normal physiologic response to a very rapid atrial rate.
The term high-grade or advanced AV block has also been used to describe certain patients whose ECGs wander between blocked P waves and complete heart block. These patients do not typically fit into the category of Mobitz II or complete heart block.
As we hinted earlier, this category of AV block is meant to provide clinicians with a term for blocks that don’t really match any one pattern completely. As such, it is a nebulous term and there is a lot of confusion about it in the literature. In our research for this chapter, we found many different definitions and criteria for this type of block. You should be aware of the lack of consensus on this matter, and we will leave it here for now. Luckily, it is not a commonly found rhythm disturbance.

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 81 BPM |
PR intervals: Prolonged, constant |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: Present |
|
|
P:QRS ratio: Variable |
Rhythm: High-grade or advanced AV block |
Discussion:
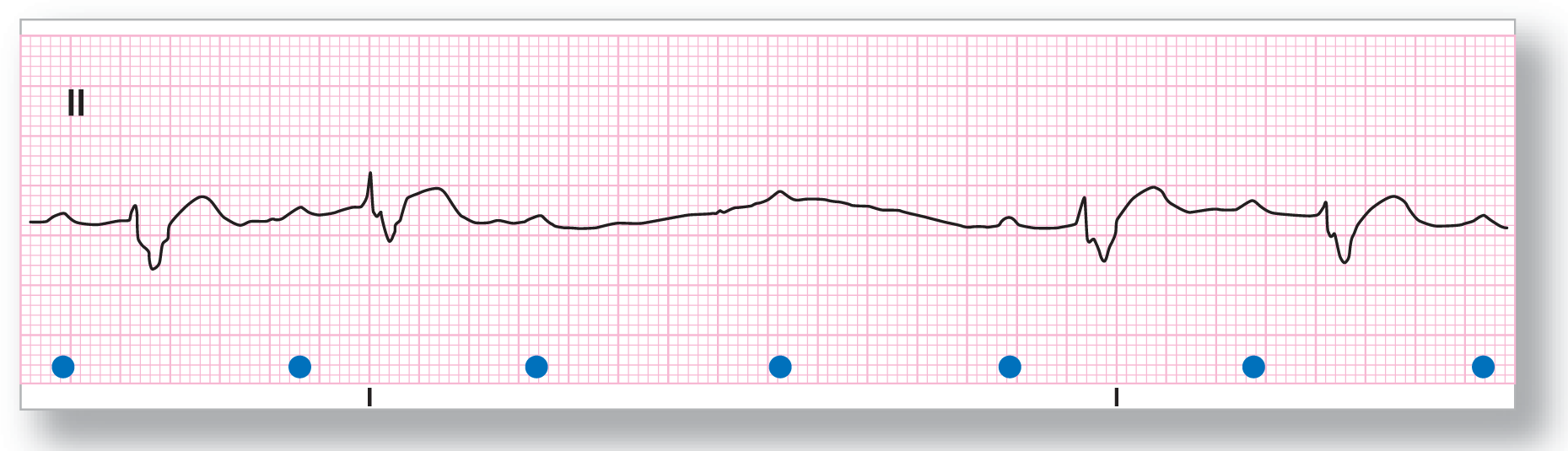
ECG 28-20 shows a prolonged PR interval that is constant throughout the conducted beats on this strip. There is evidence of Mobitz II block at the start of the strip where one QRS complex is dropped. In the middle of the strip, there are two consecutive QRS complexes dropped. The presence of the two dropped QRS complexes is indicative of a high-grade or advanced AV block. A 12-lead ECG revealed the presence of a right bundle branch block and an acute MI in this patient.
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 62 BPM |
PR intervals: Prolonged, constant |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Normal Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: Present |
|
|
P:QRS ratio: Variable |
Rhythm: High-grade or advanced AV block |
Discussion:
This patient has a strip with two consecutively blocked P waves (ECG 28-21). The PR interval is markedly prolonged, but constant throughout the conducted beats. The P-P interval remains fairly constant throughout the strip with only minimal variations that fluctuate slightly within acceptable limits, as usually happens in these patients. A 12-lead ECG was compatible with a left bundle branch block configuration in a patient having an acute MI.