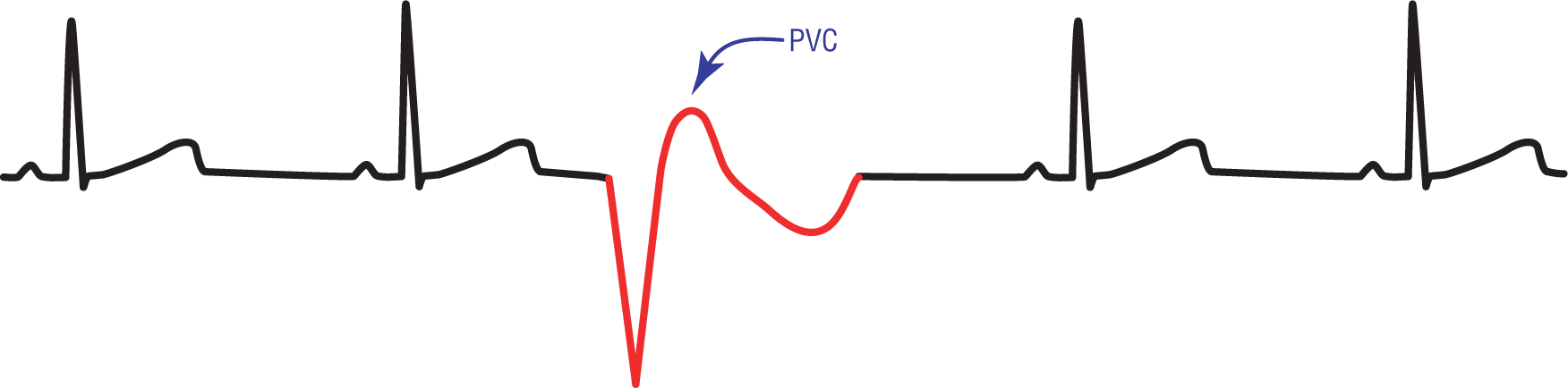
Figure 30-1 A premature ventricular contraction.
© Jones & Bartlett Learning.
Premature ventricular contractions (PVCs) can go by various names in the literature. They are known as ventricular premature depolarizations, ventricular premature contractions, and ventricular extrasystoles. Since there is no consensus in the literature about the correct terminology, we will stick to the tried and true nomenclature of PVCs that is very familiar to most clinicians.
A PVC is a depolarization wave that originates in a ventricular focus and that arrives prematurely when compared to the underlying rhythm. It has all of the qualities of a ventricular beat. The list of general characteristics of a PVC includes (Figure 30-1):
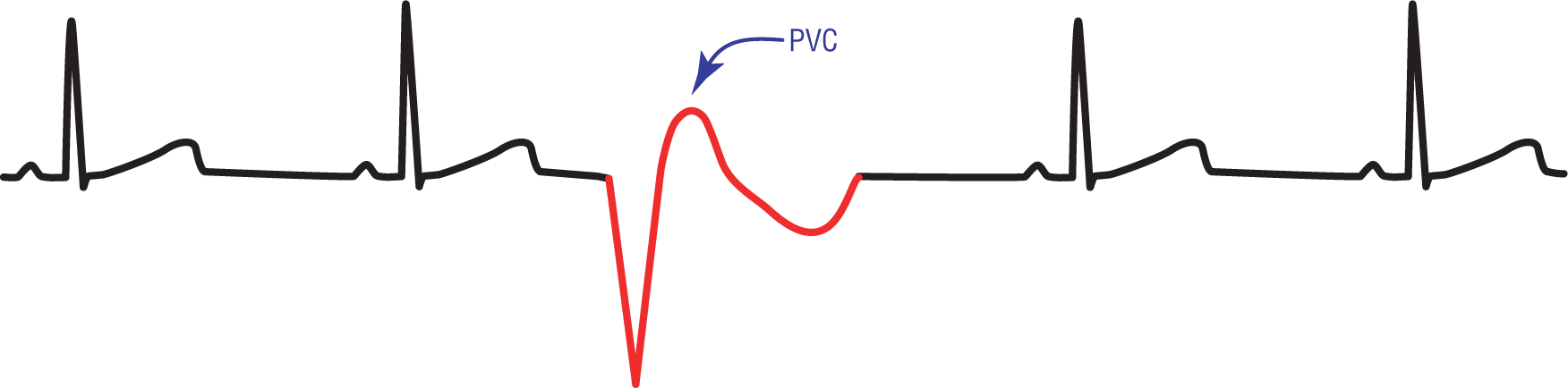
Figure 30-1 A premature ventricular contraction.
© Jones & Bartlett Learning.
PVCs are a very common occurrence and can occur in the normal population, as well as in patients with cardiac disease. In any one patient, the number of PVCs that occur can vary tremendously based on the time of day, medications, coffee, soda, or a hundred other variables. The PVCs usually cause no symptoms, and the patient will be completely unaware that they are occurring. Other times, the patient may just feel a slight skipping in the heart or a sense of palpitations.
In some cases, however, the unsynchronized contraction of the heart caused by a PVC may actually lead to a momentary stop in cardiac ejection. These patients may develop hemodynamic compromise if the frequency of PVCs is high enough. For example, a patient with a PVC occurring every other beat may have a monitored heart rate of 80 beats per minute (BPM), but the actual palpable heart rate in the peripheral arteries may be 40 BPM because every other beat is not having any form of effective contraction. As you know, a heart rate of 40 BPM may cause significant hemodynamic compromise in many patients.
NOTE
As we discussed in Chapter 6, Electrocardiography and Arrhythmia Recognition, there is a fine point in the cardiac nomenclature between a rhythm and an event. A rhythm is an intrinsic rate of the heart based on some cardiac pacemaker. An event is a single depolarization or an isolated set of depolarizations, either sinus or ectopic, that breaks up the regularity or cadence of an underlying rhythm. A PVC is an event. Two PVCs occurring sequentially, known as a couplet, is also an event. Many clinicians make the mistake of stating the couplet as the rhythm. The correct way of saying this is: The patient has a (fill in the rhythm) with a couplet.
A word about the treatment of PVCs: New treatment strategies and new pharmacologic agents are changing the clinical treatment spectrums of the various arrhythmias on an almost daily basis. We try to stay away from the treatment strategies of any rhythm abnormality whenever possible in order to try to keep this text current. However, there are some underlying treatment strategies related to PVCs that we feel are timeless and need to be presented here.
The drugs that we use to treat ventricular arrhythmias can be very dangerous in the wrong clinical setting. In many cases, these drugs can potentially initiate or propagate more serious, life-threatening arrhythmias in many patients. Therefore, when treating PVCs, remember to treat the patient and not the individual events. If the patient is asymptomatic from the PVCs, why would you want to give him or her a drug that could potentially be more harmful?